
SAMPLE PROJECT PROPOSAL AND BUDGET
FOR REFERENCE ONLY
This document provides a sample project proposal and sample budget from a previous
year’s GME research grant program. Please note: These sample documents should be
used for reference ONLY.

Identification of Problem and Skill Assessment in Learning Neonatal Intubation: A Descriptive
Study Examining the Gaps in Procedural Proficiency
Introduction: Neonatal intubation is the most essential of all skills required by a health care
professional during neonatal resuscitation. The small size of the oral cavity in neonates makes
direct laryngoscopy (DL) challenging and difficult to learn and train. The difficulty in DL and
tracheal intubation further increases with prematurity, increasing the failure rate and increase
in the frequency of traumatic intubation. The data from a prospective observational study
collected from five level III POISE Network Neonatal Intensive Care Units (NICU) has shown
non-visualization of vocal cords accounting for as the cause responsible in 25% of intubation
failure Fig (1). It also shows that provider factors such as inability to visualize airway,
esophageal intubation, and prolonged duration accounted for the majority (55%) of failures (1)
(Figu r e 1) R e a sons f o r f ail u re (N I QI dat a f rom 5 l e vel I I I NICU i n POI SE netwo r k A to tal of 4 5 8
int u ba tion s w ere st udied )
Recent duty hour limitations and increased use of non-invasive ventilation have reduced trainee
exposure to intubation. The NIQI data suggests that house staff had the lowest success rates of
intubation among all health care workers and showed little improvement over the course of
training (Figure 2).
(Figure 2) Poor acquisition of neonatal intubation skills in pediatric house staff: Little improvement in intubation
success rate of pediatric residents (NIQI data) over 3 years of residency
Studies have shown that there are wide variation in the learning curves and the number of
attempts to achieve proficiency in performing medical and surgical procedures by novices and
new residents (2). Expertise literature stresses the importance of guided practice (3, 4) to avoid
the entrenchment of bad habits or the possibility of “laboring in vain” on tasks that are too easy
or too difficult to maximize the learning opportunity. (5) One of the most crucial aspects of
deliberate practice is the assessment of performance by an expert accompanied by immediate
feedback to allow for the correction of errors. (3, 4) Therefore it is necessary to determine
the specific types of problem areas that trainees experience when learning neonatal intubation
techniques and to determine the reliability with which expert teachers can identify these
difficulties in trainee performance.
Supervision of the non-expert intubator/operator traditionally has been provided by the
presence and verbal support of an expert provider (attending neonatologist, senior neonatal
fellow or practitioner), who is trusting observations verbally relayed from the operator, rather
than relying on their independent direct visual confirmation (6).
Direct laryngoscopy requires a line of sight along the blade to obtain a view to the glottis
opening. The viewing angle has been measured at 15 degree and is limited by oropharyngeal
structures (7). Limited space and small oral cavity obscures the view even more, especially in
premature neonates, making it near impossible to assess the skill closely and identify the
problem, required to train novices by deliberate practice.
A video camera at the tip of the blade can potentially provide an increased angle and a
magnified view of the glottis in the normal and difficult pediatric airway. Studies in adults have
shown efficacy of video laryngoscopy over DL, especially for teaching novice intubators (7). A
previous pediatric study done on children less than 4 years of age has found improved glottis
view compared to DL(8).
This study is designed to study the development of neonatal intubation skills by health care
workers frequently involved in neonatal resuscitation in a level III NICU. The study aims to
evaluate the procedure of neonatal intubation during training in the simulation lab in phase (I)
and in real patients (neonates in the NICU) in phase (II) of the study.
The Storz C-MAC video laryngoscope offers size 0 and 1 Miller blades as well as display and
recording capabilities via the fiberoptic camera in the light source at the tip of the blade (figure
3). The technique of placing an endotracheal tube is similar to the standard technique for direct
laryngoscopy that we currently employ and teach in the NICU. As the blade is straight, the view
on the screen is similar to what is seen when looking directly into the mouth (6, 9). Therefore,
the device can be used in the same manner as a traditional laryngoscope, or indirectly by
viewing the image on the screen. The video recorded can be later viewed by the trainers and
learners, and can serve as one of the unique tools for future research in skill acquisition,
competency assessment, and quality improvement in the neonatal intubation. The Food and
Drug Administration have approved the C-MAC for use in neonates.

(Figure 3) Karl Storz C-Mac Video Laryngoscope
Over the past decade, there have been an increasing number of studies evaluating the
effectiveness of simulation as educational tool (13) Simulation-based educational interventions
increase retention of knowledge for resuscitation, trauma care, airway management, procedural
skills team-training, and disaster management (14)
The intubation studies in the past have focused on the effectiveness of video laryngoscopy over
direct laryngoscopy and the use of video laryngoscope for difficult intubations. However no
studies have been done in order to identify the reason(s) behind variation in the training curve
of novices and learners including pediatric residents. The question of why some learners require
more time and more number of neonatal intubations to achieve proficiency is still unanswered.
Objective: To identify the specific problems in learning neonatal intubation by novices, by
assessment of their intubation skill in a neonatal manikin (phase I) and real neonates in NICU
(phase II) with the help of video laryngoscopy (Karl Storz C-MAC Video Laryngoscope).
Specific Aim:
1. Define novice vs. expert in neonatal intubation from procedural steps prospective, by
studying video recording of learners’ performing the procedure. Performance will be
evaluated from two perspectives: external to the intubation head and inside the oral
cavity using video laryngoscopy.
2. Identification of problem areas in learning neonatal intubation (e.g. anatomy,
equipment, patient position)
Purpose:
1. Defining the steps required in achieving mastery in the procedure of neonatal intubation.
2. Development of the most effective and efficient training module of neonatal intubation.
Method: The study is planned in 2 phases which can occur in tandem,
Phase I: Evaluation of performance in the simulated setting
Phase II: Evaluation of performance in the clinical setting
Participants are practicing health care workers performing neonatal intubations as well as novice
providers performing neonatal intubation. The participants will include Attending
Neonatologists, Neonatal Fellows, Neonatal Nurse Practitioners, and Respiratory Therapists,
pediatric residents, novice pediatric residents and interns. The participants (subjects) will be
grouped in the following 3 categories according to their proficiency in performing neonatal
intubations:
1. Experts: Neonatologists (attending physicians), senior neonatology fellows, NICU
transport nurses, and experienced mid-level providers
2. Advance providers: Nurse Practitioners (ARNP), Respiratory therapists (RT) and
Neonatology Fellows
3. Novices: Pediatric interns and residents, and other trainees (transport RN, NNP students)
We plan to study 20 intubations from each group of participants in both the phases.
A total of 60 intubations will be studied in phase I and 60 intubations in phase II. The process of
evaluating the procedural elements of the novice learners as compared to experts will be
evaluated by cognitive task analysis (CTA). CTA has replaced traditional task analysis techniques
to generate task demands as an input to training system design for many complex tasks. (15)
The study method will include following steps:
1. Pre-procedure assessment
All participants will be instructed to watch the New England Journal of Medicine Videos in
Clinical Medicine on Orotracheal Intubation (16) to allow for an introduction to the airway
anatomy and baseline understanding of the procedural technique. The details of the instrument
and the neonatal manikin will be explained to each participant before performing the procedure.
The participant will complete a self assessment questionnaire (Pre procedure subject form) form
no.1 to assess their knowledge and expertise in neonatal intubation
2. Procedural data collection
Phase I: Each participant will perform 2 intubations using Storz C-MAC by direct laryngoscopy,
(not visualizing the video) in a neonatal manikin (for phase I) in the presence of a direct observer
and an external video camera (recording the procedure). Video captured will be scored to
characterize novice proceduralists for comparison to video of experts performing intubation on
the same manikin.
Phase II: Trainees will perform neonatal intubations using Storz C-MAC by direct laryngoscopy,
(performance will be recorded using the Storz device) in the NICU of Tampa General Hospital in
the presence of a direct observer. Intubation procedure methods (patient choice, patient
monitoring, supervision and assistance, and patient tolerance of procedure attempts) will not
differ from current standard of care. In addition, the proceduralist’s discipline and level of
training will be documented. Recordings of successful and failed attempts will be evaluated for
validation of novice and expert procedural technique determined in the simulation environment.
The video images will not be available to the participant, but all the attempts will be recorded in
order to describe the intubation process by the investigator.
Post-procedure assessment
Each participant will answer a self-assessment (post procedure subject form) form no.2 to test
and assess view of glottis during intubation attempt(s) and success of procedure.
In the simulation setting (Phase I), form no.3 will be competed describing the intubation
attempts including handling of equipment, time to intubate and no. of attempts
In the clinical setting (Phase 2), form No.4 will be completed describing the details of the event
in the live neonate, which will include the vital signs, patient characteristics and details of
stabilization.
The investigator will score the video recording of the procedure technique (recorded using
external camera). The video recording of each intubation attempt will show the procedure from
inside the oropharynx. The investigator will now complete the (Investigator Video Form/ form
no.5) based on video recordings from Storz C-MAC describing position of blade of laryngoscope
and laryngeal anatomy visible during procedure.
Statistics and descriptive analysis
The data from all the forms will be collected and will be used for a descriptive analysis of the
neonatal intubation by different health care workers. Sixty participants (20 from each group - 20
experts, 20 advanced learners and 20 novices) will be included in each phase I and phase II. It
will require the capture of more than 60 intubations in the clinical setting to assure the proper
distribution of experience in providers. The results from both the phase (I and II) will be used to
identify the reason behind the variations in the learning curve of novices and differentiating
experts from novices based on real time video recording of the procedure. Raters will score
procedural performance using videotaped examples of the neonatal intubation (external and via
video laryngoscope in the simulation lab; via video laryngoscope in the NICU). We will assess
rater agreement using agreement statistics corrected by Cohn’s kappa for unequal base rates,
considering 0.75 kappa to be acceptable agreement.
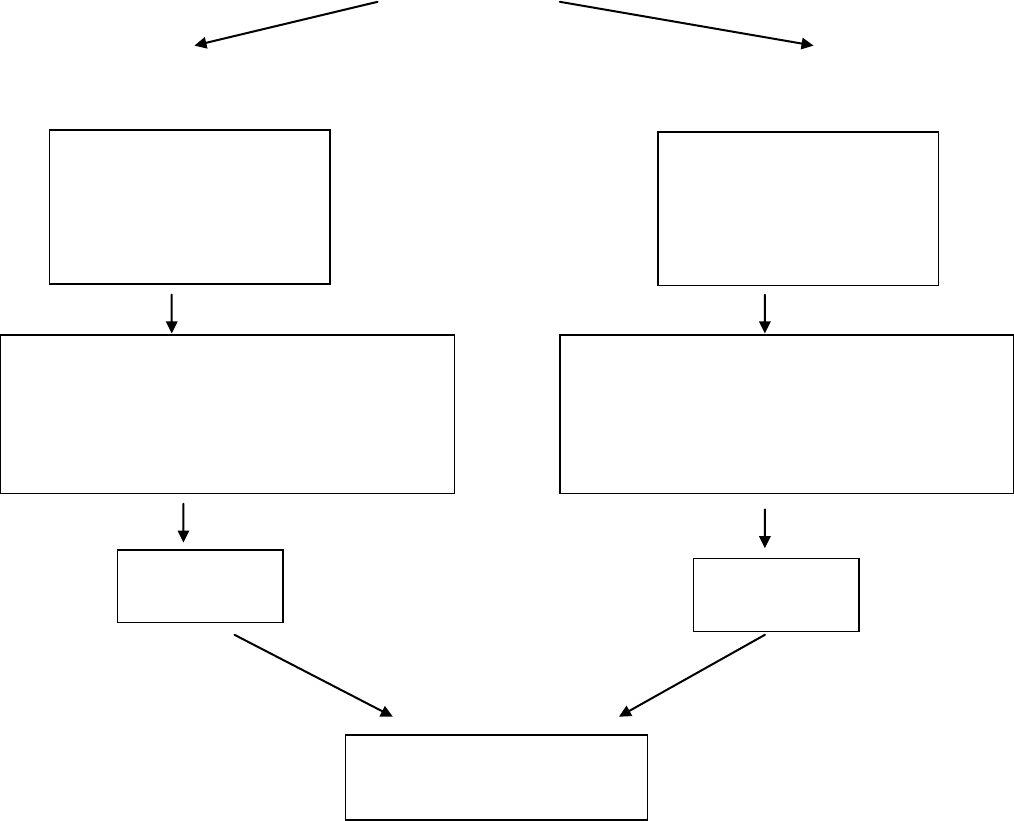
Study Design
PHASE I in neonatal manikin Phase II in neonates in
Sim lab (CAMLS) NICU & Delivery room
20 Experts
20 Advanced Learners
20 Novices
Total subjects = 60
20 Experts
20 Advanced Learners
20 Novices
Total intubations = 60
1. Preprocedure self assessment (Form 1)
2. Post procedure subject Form (Form2 )
3. Observer Form (Form 3)
4. Research video form (Form 5)
1. Preprocedure self assessment (Form 1)
2. Post procedure subject Form (Form2 )
3. Nurse Observer Form (Form 4)
4. Research video form (Form 5)
Results
Phase I
Results
Phase II
Combined final Result
from Phase I and Phase II

References:
1. Tatum P, Haubner L, Auerbach M, Soghier L, Barry J, Johnston L, White MJ. Pediatric
Resident Neonatal Intubation Success Rates Do Not Improve with Current Airway Education
Methods: An Examination of Baseline Data for a Simulation-based Educational Intervention.
Poster Presentation at the International Pediatric Simulation Symposia and Workshops,
Toulouse, France 10/26/2011.
2. Dalal PG, Dalal GB, Pott L, Bezinover D, Prozesky J, Bosseau Murray W. Learning curves of
novice anesthesiology residents performing simulated fibreoptic upper airway endoscopy.Can J
Anaesth. 2011 Sep;58(9):802-9.
3. Ericsson KA. The Road to Excellence: The Acquisition of Expert Performance in the Arts
and Sciences, Sports, and Games. Mahwah, NJ: Erlbaum; 1996.
4. Ericsson KA. Deliberate practice and the acquisition and maintenance of expert
performance in medicine and related domains. Acad Med. 2004;79(10 suppl):S70–S81.
5. Nelson TO, Leonesio RJ. Allocation of selfpaced study time and the labor-in-vain effect. J
Exp Psychol Learn Mem Cogn. 1988;14: 676–686.
6. Vanderhal AL, Berci G, Simmons CF et al.A videolaryngoscopy technique for the
intubation of the newborn. Pediatrics 2009; 124:e339–e346.
7. Low D, Healy D, Rasburn N. The use of the BERCI DCI Video Laryngoscope for teaching
novices direct laryngoscopy and tracheal intubation. Anaesthesia. 2008 Feb;63(2):195-201
8. Vlatten A, Aucoin S, Litz S, Macmanus B, Soder C. A comparison of the STORZ video
laryngoscope and standard direct laryngoscopy for intubation in the Pediatric airway--a
randomized clinical trial. Paediatr Anaesth. 2009 Nov;19(11):1102-7.
9. Holm-Knudsen R. The difficult pediatric airway--a review of new devices for indirect
laryngoscopy in children younger than two years of age. Paediatr Anaesth. 2011 Feb;21(2):98-
103.
10. Hackell RS, Held LD, Stricker PA, Fiadjoe JE. Management of the difficult infant airway
with the Storz Video Laryngoscope: a case series. Anesth Analg. 2009 Sep;109(3):763-6.
11. Wald SH, Keyes M, Brown A. Pediatric video laryngoscope rescue for a difficult neonatal
intubation. Paediatr Anaesth. 2008 Aug;18(8):790-2.
12. Fiadjoe JE, Stricker PA, Hackell RS, Salam A, Gurnaney H, Rehman MA, Litman RS.The
Efficacy of the Storz Miller 1 Video Laryngoscope in a Simulated Infant Difficult Intubation.
Anesth Analg 2009;108:1783-1786.
13. Issenberg SB, McGaghie WC, Petrusa ER, et al. Features and uses of high-fidelity medical
simulations that lead to effective learning: a BEME systematic review. Med Teach 2005; 27:10–
28.
14. Weinberg ER, Auerbach MA, Shah NB. The use of simulation for pediatric training and
assessment. Curr Opin Pediatr. 2009 Jun;21(3):282-7.
15. Fackler JC, Watts C, Grome A, Miller T, Crandall B, Pronovost P. Critical care physician
cognitive task analysis: an exploratory study. Crit Care. 2009; 13(2):R33.
16. Christopher Kabrhel, M.D., Todd W. Thomsen, M.D., Gary S. Setnik, M.D., and Ron M.
Walls, M.D. Orotracheal Intubation. N Engl J Med 2007; 356:e15, April 26, 2007.
http://www.nejm.org/doi/full/10.1056/NEJMvcm063574
SAMPLE BUDGETS

Examples of Prior Grantee’s Sample Budget Per Type of Research
Basic/ Translational Science
Immunohistochemical Characterization of Anaplastic Large Cell Lymphoma
Disclaimer: Max grant allotment is $5,000
Disparity Projects:
Alleviating Burden of Chronic Disease (ABCD) among the Uninsured of Tampa Bay: USF Diabetes
Intervention

Quality Improvement Projects:
Who is on my team? Using baseball cards to improve patients' satisfaction through recognition
and communication with their physician staff.
Clinical Trials
Concurrent Hypertonic saline For Congestive heart failure Patients with and without Renal
Syndrome I (CHF CPRS I)
Disclaimer: Max grant allotment is $5,000
