
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior authorization and step therapy coverage criteria
August 2024
= Prior Approval/Step Therapy may apply Page 1
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Blue Cross Blue Shield of Michigan and Blue Care Network work to make sure you get the safest, most effective and most reasonably priced prescription drugs. Our pharmacists do
this in many different ways. Prior authorization and step therapy are two of our tools.
What is prior authorization?
Blue Cross and BCN require a review of certain medications before your plan will cover them, which is called prior authorization. This ensures you’ve tried the preferred alternatives — drugs
with a proven track record that may be better tolerated, less expensive or less likely to cause interactions — and the drug is being prescribed appropriately. If your doctor doesn’t get prior
authorization when required, your drug may not be covered. You should consult with your doctor about an alternative therapy in those cases. Most approved prior authorizations last for a set
period of time, usually one year. Once they expire, your doctor must request prior authorization again for future coverage.
What is step therapy?
Step therapy requires that you try one or more preferred drugs before coverage for a more expensive alternative is approved. This ensures all clinically sound and cost-effective treatment
options are tried before more expensive medications. If your prescribed treatment doesn’t meet the step therapy criteria, it may not be covered. You should consult with your doctor about an
alternative therapy.
What kinds of drugs need prior authorization or step therapy?
Blue Cross and BCN may require prior authorization or step therapy for drugs that:
Have dangerous side effects or can be harmful when combined with other drugs
Should only be used for certain health conditions
Can be misused or abused
Are prescribed when there are preferred drugs available that are just as effective
The criteria for medications that need prior authorization or step therapy are based on current medical information and the recommendations of Blue Cross and BCN’s Pharmacy and
Therapeutics Committee, a group of physicians, pharmacists and other experts.
Coverage of drugs depends on your prescription drug plan. Not all drugs included in these prior authorization and step therapy guidelines are necessarily covered by your plan. Also, some
medications excluded from your prescription drug plan may be covered under your medical plan. Examples include medications that are generally administered in a physician’s office or
other sites of care, rather than at home by the patient. For drugs covered under commercial Blue Cross or BCN medical benefits, please see the Blue Cross and BCN Utilization
Management Medical Drug List. Requests for medications not covered by your prescription drug plan are reviewed by Blue Cross and BCN to determine if they are medically necessary for
you or if there are other equally effective treatments already covered by your drug plan. In rare cases, Blue Cross and BCN may approve medications that aren’t covered by your drug plan.

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 2
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Prior authorization and pharmacy programs listed in this guideline:
• BCN Custom Drug List
• BCBSM Custom Drug List
• BCBSM Clinical Drug List
• BCN Custom Select Drug List
• BCBSM Custom Select Drug List
• Lite Prior Authorization Program
• Preferred Therapy Program — This program encourages using more cost-effective drugs rather than higher-priced, brand-name drugs if a prescription for the brand-name drug
hasn’t been filled in the last 180 days.
• Off-Label and High-Cost Specialty program — Off-label means a drug is being used in a way that hasn’t been approved by the U.S. Food and Drug Administration. Drugs with
potential for off-label use and high-cost specialty drugs on this list require prior authorization for Blue Cross to cover them..
Questions?
Please call the Customer Service number on the back of your Blue Cross or BCN member ID card if you have questions about:
• Your drug plan’s coverage or how these pharmacy programs apply
• A drug claim
Electronic prior authorization for doctors and other health care providers
Your doctor can click here to request an electronic review of your covered drugs that require prior authorization or step therapy.

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 3
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
New coverage criteria for certain drugs
Drug name
Current
Blue Cross and BCN
coverage criteria
New
Blue Cross and BCN
coverage criteria
Publish
date
for the
new
coverage
criteria
Effective
date
for the
new
coverage
criteria
Cuvitru
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
Trial and failure or intolerance to Hizentra and Gammagard liquid
8/1/2024
10/1/2024
Cutaquig
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
Trial and failure or intolerance to Hizentra and Gammagard liquid
8/1/2024
10/1/2024
Gammaked
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
Trial and failure or intolerance to Hizentra and Gammagard liquid
8/1/2024
10/1/2024
Gamunex-C
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
Trial and failure or intolerance to Hizentra and Gammagard liquid
8/1/2024
10/1/2024
Hyqvia
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
Trial and failure or intolerance to Hizentra and Gammagard liquid
8/1/2024
10/1/2024
Xembify
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
Trial and failure or intolerance to Hizentra and Gammagard liquid
8/1/2024
10/1/2024
Qulipta
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
1. For preventive treatment of migraine headaches
2. Age ≥ 18 years old
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
5. Not to be used in combination with other CGRP antagonists for migraine prevention
8/1/2024
10/1/2024
Ajovy
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
1. Age ≥ 18 years old
2. Being used for preventive treatment of migraine headaches
3. Member has history of ≥ 4 headache days per month
8/1/2024
10/1/2024
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 4
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug name
Current
Blue Cross and BCN
coverage criteria
New
Blue Cross and BCN
coverage criteria
Publish
date
for the
new
coverage
criteria
Effective
date
for the
new
coverage
criteria
4. Trial of two medications from two different classes for the prevention of migraines
5. Trial and treatment failure of Aimovig and Emgality
6. Not to be used in combination with other CGRP antagonists for migraine prevention
Nurtec
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
1. For preventive treatment of migraine headaches
2. Age ≥ 18 years old
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
5. Not to be used in combination with other CGRP antagonists for migraine prevention
8/1/2024
10/1/2024
Aimovig
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
1. For preventive treatment of migraine headaches
2. Age ≥ 18 years old
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
5. Not to be used in combination with other CGRP antagonists for migraine prevention
8/1/2024
10/1/2024
Emgality 120
mg/ml
(For full coverage criteria, please see drug entry below)
Current criteria as listed in drug entry below and:
1. For preventive treatment of migraine headaches
2. Age ≥ 18 years old
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
5. Not to be used in combination with other CGRP antagonists for migraine prevention
8/1/2024
10/1/2024

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 5
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Accrufer
Coverage requires the following:
1. Diagnosis of iron deficiency
2. Age ≥ 18 years old
3. Trial and failure or intolerance to two over-the-counter iron products
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 6
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Actemra SC
Coverage requires the following:
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of one Disease-Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
( examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
4. Trial and treatment failure of two of the following Enbrel, Humira, Cimzia, Simponi, Rinvoq, or Xeljanz/XR
OR
1. Diagnosis of Polyarticular Juvenile Idiopathic Arthritis
2. Age ≥ 2 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, leflunomide)
4. Trial and treatment failure of two of the following Enbrel, Humira, or Xeljanz
OR
1. Diagnosis of Still’s disease, including adult-onset Still’s disease (AOSD) and systemic juvenile idiopathic arthritis
(sJIA)
2. Age ≥ 2 years old
3. Trial and treatment failure of one of the following therapies: glucocorticoids or NSAIDs
OR
1. Diagnosis of giant cell arteritis
2. Age ≥ 18 years old
OR
1. Diagnosis of systemic sclerosis-associated interstitial lung disease (SSc-ILD)
2. Inadequate response to (as evidenced by disease progression - (e.g. worsening of pulmonary function) or not a
candidate for either mycophenolate mofetil OR cyclophosphamide
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 7
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Acthar Gel
Coverage is provided for the treatment of infantile spasms (West Syndrome) for children less than 2 years old
Approval: 60 days
NC
NC
adapalene/benzoyl
peroxide
(Epiduo
Forte)
Coverage requires the following:
1. Diagnosis of acne
2. Trial and failure, contraindication, or intolerance to three generic or preferred topical agents for the treatment of
acne, one of which must be benzoyl peroxide and another must be adapalene
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Adbry
Coverage requires the following:
1. Diagnosis of moderate to severe atopic dermatitis (AD)
2. Age ≥ 12 years old
3. Trial and treatment failure of one of the following: high potency topical corticosteroid, tacrolimus, pimecrolimus,
cyclosporine, methotrexate, azathioprine, or mycophenolate mofetil
4. Cannot be used in combination with other biologic agents indicated for atopic dermatitis
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 8
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Addyi
Coverage requires the following:
1. Premenopausal female ≥ 18 years old
2. Diagnosis of acquired, generalized hypoactive sexual desire disorder (HSDD) that has been ongoing for more than
6 months
3. Other causes (such as relationship difficulty, substance abuse, medication side effects) of HSDD must be ruled out
Initial approval: 60 days
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Adempas
Coverage requires the following:
1. Diagnosis of persistent/recurrent Chronic Thromboembolic Pulmonary Hypertension (CTEPH) (WHO Group 4) after
surgical treatment or inoperable CTEPH
OR
1. Diagnosis of Pulmonary Arterial Hypertension (PAH)(WHO Group 1)
Adlarity
Coverage requires the following:
1. Diagnosis of mild, moderate, and severe dementia of Alzheimer’s type
2. Trial and failure or intolerance to generic oral donepezil
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 9
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Adzenys ER,
amphetamine
suspension
Coverage requires the following:
1. Diagnosis of Attention Deficit Hyperactivity Disorder
2. Age ≥ 6 years old
3. Treatment failure or intolerance to both a generic methylphenidate and a generic amphetamine product, one of
which must be a long-acting formulation
OR
3. Member cannot swallow tablets/capsules and has tried and failed one of the agents that can be opened and
sprinkled on applesauce (methylphenidate ER, Adderall XR)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Adzenys
XR-ODT
Coverage requires the following:
1. Diagnosis of Attention Deficit Hyperactivity Disorder
2. Age ≥ 6 years old
3. Treatment failure or intolerance to both a generic methylphenidate and a generic amphetamine product, one of
which must be a long-acting formulation
OR
3. Member cannot swallow tablets/capsules and has tried and failed one of the agents that can be opened and
sprinkled on applesauce (methylphenidate ER, Adderall XR)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 10
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Afrezza
Coverage is provided when the member has experienced treatment failure or intolerance to Novolog
NC
NC
Agamree
Coverage requires the following:
1. Diagnosis of Duchenne Muscular Dystrophy (DMD)
2. Age ≥ 2 years old
3. Trial and failure, contraindication, or intolerance to adequate doses (0.75 mg/kg/day) of generic prednisone or
generic prednisolone
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Aimovig
Coverage requires the following:
1. Age ≥ 18 years old
2. Being used for preventive treatment of migraine headaches
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 11
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ajovy
Coverage requires the following:
1. Age ≥ 18 years old
2. Being used for preventive treatment of migraine headaches
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
5. Trial and treatment failure of Aimovig and Emgality
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Akeega
Coverage requires the following:
1. Age ≥ 18 years old
2. For the treatment of deleterious or suspected deleterious BRCA mutated (BRCAm) metastatic castration-resistant
prostate cancer (mCRPC)
3. Using in combination with prednisone
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 12
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Akynzeo
Coverage is provided for the prevention of chemotherapy-induced nausea/vomiting (CINV) and after a trial of all of the
following:
1. Generic 5HT3 antagonist (ex. generic Zofran, generic Kytril)
2. Preferred NK1 antagonist (ex. Emend).
3. Glucocorticoid (dexamethasone)
Initial approval: 1 year
Renewal requires continuation of chemotherapy
Alecensa
Coverage requires the following:
1. Diagnosis of anaplastic lymphoma kinase (ALK) positive, metastatic non-small cell lung cancer
OR
1. Diagnosis of anaplastic lymphoma kinase (ALK) positive non-small cell lung cancer (tumors ≥ 4 cm or node
positive)
2. Using as adjuvant treatment following tumor resection
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 13
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Alkindi Sprinkle
Coverage requires the following:
1. Diagnosis of adrenocortical insufficiency
2. Age ≤ 6 years old
OR
2. Member cannot swallow tablets/capsules
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
almotriptan
(Axert)
Coverage requires trial of 2 of the following generic triptans: Imitrex, Maxalt, Amerge or Zomig/ZMT
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Alunbrig
Coverage requires the following:
Diagnosis of anaplastic lymphoma kinase (ALK)-positive metastatic non-small cell lung cancer (NSCLC) as detected by an
FDA-approved test
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
ambrisentan
(Letairis)
Coverage is provided for the treatment of pulmonary arterial hypertension (WHO Group 1)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 14
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
amphetamine sulfate
(Evekeo)
Coverage is provided when one of the following have been met. (1, 2 or 3):
1. Narcolepsy:
a. ≥ 6 years of age
b. Trial and treatment failure or intolerance to generic Adderall IR and a generic methylphenidate product
2. ADHD: (Attention deficit hyperactivity disorder)
a. 3-6 years of age
i. Trial and treatment failure or intolerance to generic amphetamine product or
b. ≥ 6 years of age
i. Trial and treatment failure or intolerance to of generic amphetamine and generic methylphenidate
product
3. Obesity:
a. ≥ 12 years of age
b. BMI ≥ 30 kg/m2
c. Current weight (within 30 days) must be submitted to the plan for review
d. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR
active participation for a minimum of 6 months in an alternative concurrent lifestyle modification program (e.g.
recent food diaries, exercise logs, program receipts, app participation, etc.) if member does not have access to
a covered BCBSM/BCN program
e. Previous trials of weight loss therapies (examples include: repeated diets, group programs, or other weight
loss medications)
Approval (Obesity): 60 days
Initial approval (Narcolepsy and ADHD): 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 15
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
anastrozole
(Arimidex)
Coverage for $0 copayment will be provided when:
1. The member is a woman at least 35 years of age
2. The medication is being used for prevention of primary breast cancer
3. Members is classified as high risk
4. Does not have a history of breast cancer
5. Member is currently post-menopausal
Aptiom
Coverage requires the following:
1. Treatment of seizures in patients with epilepsy
2. Treatment failure or intolerance to at least 3 generic alternatives for the treatment of seizures
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 16
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Arcalyst
Coverage requires the following:
1. Treatment of Cryopyrin-Associated Periodic Syndromes (CAPS), including Familial Cold Autoinflammatory
Syndrome (FCAS) and Muckle-Wells Syndrome (MWS)
2. Age ≥ 12 years old
3. Laboratory evidence of a genetic mutation OR elevated inflammatory markers plus at least two of six typical CAPS
manifestations: (urticaria-like rash, cold-triggered episodes, hearing loss, musculoskeletal symptoms, chronic
aseptic meningitis, or skeletal abnormalities)
OR
1. Diagnosis of deficiency of interleukin-1 receptor antagonist (DIRA)
2. Laboratory evidence of homozygous genetic mutations of IL1RN
3. Weight ≥ 10 kg
4. Trial and failure, contraindication, or intolerance to Kineret
OR
1. Diagnosis of recurrent pericarditis (RP)
2. Age ≥ 12 years old
3. Trial and treatment failure or intolerance to nonsteroidal anti-inflammatory drugs (NSAIDs) in combination with
colchicine
4. Trial and treatment failure or intolerance to Kineret
5. Must not be used in combination with other biologic medications used for recurrent pericarditis, such as Kineret
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 17
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Arikayce
Coverage requires the following:
1. Diagnosis of mycobacterium avium complex (MAC)
2. Age ≥ 18 years old
Initial approval: 1 year
Augtyro
Coverage requires the following:
1. Diagnosis of locally advanced or metastatic ROS1-positive non-small cell lung cancer (NSCLC)
2. Age ≥ 18 years old
OR
1. For the treatment of solid tumors that:
a. Have a neurotrophic tyrosine receptor kinase (NTRK) gene fusion AND
b. Are locally advanced or metastatic or where surgical resection is likely to result in severe morbidity AND
c. Progressed following treatment or have no satisfactory alternative therapy
2. Age ≥ 12 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Auvelity
Coverage requires trial and failure of at least three antidepressant agents
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 18
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Austedo
Coverage requires the following:
1. Diagnosis of chorea associated with Huntington’s disease
2. Trial and failure or intolerance to Xenazine
OR
1. Diagnosis of Tardive Dyskinesia
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Austedo XR
Coverage requires the following:
1. Diagnosis of chorea associated with Huntington’s disease (HD)
2. Age ≥ 18 years old
3. Trial and failure, contraindication, or intolerance to generic Xenazine (tetrabenazine)
OR
1. Diagnosis of tardive dyskinesia
2. Age≥ 18 years old
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 19
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ayvakit
Coverage requires the following:
1. Treatment of unresectable or metastatic gastrointestinal stromal tumor harboring a PDGFRA exon 18 mutation
2. Age ≥ 18 years old
OR
1. Diagnosis of advanced systemic mastocytosis (advSM)
2. Age ≥ 18 years old
OR
1. Diagnosis of indolent systemic mastocytosis (ISM)
2. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Azstarys
Coverage requires the following:
1. Diagnosis of attention deficit hyperactivity disorder (ADHD)
2. Age ≥ 6 years old
3. Trial and treatment failure or intolerance to one generic stimulant, such as a generic amphetamine product or a
generic methylphenidate product
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 20
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
baclofen suspension
(Fleqsuvy)
Coverage requires the following:
1. Diagnosis of spasticity
2. Trial and failure or intolerance to baclofen tablets OR member is unable to swallow tablets
3. Trial and failure or intolerance to Lyvispah
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Balversa
Coverage requires the following:
1. Diagnosis of locally advanced or metastatic urothelial carcinoma with susceptible FGFR3 genetic alterations
2. Disease progression during or following at least one line of prior systemic therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Beconase AQ
Coverage requires trial and failure/intolerance of 2 of the following intranasal steroids: generic fluticasone (Flonase), generic
flunisolide (Nasalide), or generic triamcinolone (Nasacort AQ)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 21
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Belsomra
Coverage requires treatment failure of ONE of the following: immediate-release zolpidem (Ambien), eszopiclone (Lunesta),
zaleplon (Sonata), trazodone (Desyrel), or doxepin (Silenor)
Coverage will not be approved for combination therapy with other sedative hypnotics
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Benlysta
Coverage requires the following:
1. Age ≥ 5 years old
2. Diagnosis of systemic lupus erythematosus (SLE)
3. Patients have tested positive for serum antibodies at 2 independent time points
4. If patient has lupus nephritis ONLY and no other symptoms of SLE, patient must have active disease of the kidney
confirmed on biopsy
5. Does not have severe active CNS lupus
6. Previous treatment courses of at least 12 weeks each with 2 or more of the following have been ineffective:
hydroxychloroquine, methotrexate, azathioprine, cyclophosphamide or mycophenolate, unless all are
contraindicated or not tolerated
7. Patient is currently receiving, and will continue to receive standard of care regimen (examples include
antimalarials, corticosteroids, and non-biologic immunosuppressants)
8. Not to be used in combination with other biologics, B-cell targeted therapies
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 22
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Besremi
Coverage requires the following:
1. Treatment of polycythemia vera (PV)
2. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
bexarotene capsule
(Targretin)
Coverage requires the following:
1. Diagnosis of cutaneous T-cell lymphoma (CTCL)
2. Treatment failure or intolerance to at least one systemic therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
bexarotene gel
(Targretin)
Coverage requires the following:
1. Diagnosis of Cutaneous T-cell lymphoma
2. Topical treatment of cutaneous lesions

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 23
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Binosto
Coverage requires trial and treatment failure or intolerance to two of the following:
1. Actonel (risedronate)
2. Boniva (ibandronate)
3. Fosamax (alendronate)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Bonjesta
Coverage requires the following:
1. Treatment of nausea and vomiting of pregnancy
2. Trial and treatment failure of the individual agents (doxylamine and pyridoxine) in combination
Approval length: 9 months
NC
NC
bosentan
(Tracleer)
Coverage is provided for the treatment of pulmonary arterial hypertension (WHO Group 1)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 24
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Bosulif
Coverage requires the following:
1. Diagnosis of chronic phase Philadelphia chromosome-positive (PH+) chronic myelogenous leukemia (CML)
OR
1. Diagnosis of chronic, accelerated, or blast phase PH+ CML with resistance or intolerance to prior therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Braftovi
Coverage requires the following:
1. Diagnosis of unresectable or metastatic melanoma with a BRAF V600E or V600K mutation as detected by an FDA-
approved test
2. Using in combination with Mektovi
OR
1. Diagnosis of metastatic colorectal cancer with a BRAF V600E mutation as detected by an FDA approved test
2. Using in combination with Erbitux
3. Treatment failure or intolerance to prior therapy
OR
1. Diagnosis of metastatic non-small cell lung cancer (NSCLC) with a BRAF V600E mutation as detected by an FDA
approved test
2. Using in comination with Mektovi
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 25
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Brexafemme
Coverage requires the following:
1. Treatment of acute vulvovaginal candidiasis (VVC) or recurrent vulvovaginal candidiasis (RVVC)
2. Trial and failure, contraindication, or intolerance to generic oral fluconazole alone
Approval: 6 months
Bronchitol
Coverage requires the following:
1. Using as add-on maintenance therapy to improve pulmonary function in patients with cystic fibrosis (CF)
2. Age ≥ 18 years old
3. Must have passed the Bronchitol Tolerance Test
4. Member will be taking a short-acting bronchodilator 5-15 minutes before every dose of Bronchitol
5. Trial and failure, contraindication, or intolerance to nebulized hypertonic saline
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Briviact
oral solution + tablet
Coverage requires the following:
1. Treatment of seizure disorder/epilepsy
2. Treatment failure or intolerance to 3 generic preferred alternatives
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 26
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Brukinsa
Coverage requires the following:
1. Diagnosis of mantle cell lymphoma (MCL)
2. Treatment failure or intolerance to Calquence
OR
1. Diagnosis of Waldenström’s macroglobulinemia (WM)
2. Trial and failure or intolerance to Imbruvica
OR
1. Diagnosis of marginal zone lymphoma (MZL)
2. Treatment failure or intolerance to one or more rounds of therapy with a CD20 inhibiting antibody
OR
1. Diagnosis of chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL)
2. Treatment failure or intolerance to Calquence or Imbruvica
OR
1. Diagnosis of relapsed or refractory follicular lymphoma (FL)
2. Using in combination with obinutuzumab
3. Treatment failure of two or more lines of systemic therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 27
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
buprenorphine hcl
(Belbuca)
Coverage requires the following:
1. Diagnosis of moderate to severe chronic pain requiring around the clock opioid analgesia for an extended period of
time
2. Trial and failure or intolerance to two long-acting opioids, one of which must be buprenorphine transdermal patch
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Note: Coverage will not be provided if the patient is on more than one long acting opioid concurrently
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 28
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Bylvay
Coverage requires the following:
1. For the treatment of pruritus in patients with a diagnosis of progressive familial intrahepatic cholestasis (PFIC)
2. Age ≥ 3 months old
3. Genetic testing does not show presence of the ABCB11 variants resulting in a nonfunctional or complete absence
of the bile salt export pump protein (BSEP-3).
4. No history of liver transplant or planned future liver transplant
5. No clinical evidence of decompensated cirrhosis
6. Trial and failure, contraindication, or intolerance to generic ursodiol
OR
1. For the treatment of cholestatic pruritus in patients with a diagnosis of Alagille syndrome (ALGS)
2. Diagnosis is confirmed by documentation of 1 of the following:
a. Genetic testing shows presence of the JAG1 or NOTCH2 genetic mutation
b. Liver biopsy shows bile duct scarcity
c. Involvement of 3 of 7 of the main organ systems affected in ALGS: hepatic, ocular, skeletal, vascular,
facial, cardiac, or renal involvement
3. Age ≥ 12 months old
4. No history of liver transplant or planned future liver transplant
5. No clinical evidence of decompensated cirrhosis
6. Trial and failure, contraindication, or intolerance to generic ursodiol
Initial approval: 6 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 29
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Cablivi
Coverage requires the following:
1. Diagnosis of acquired aTTP
2. Administered in addition to plasma exchange and immunosuppressive therapy
3. Continued 30 days after discontinuation of plasma exchange
Approval: 60 days
Cabometyx
Coverage requires the following:
1. Diagnosis of advanced renal cell carcinoma
2. Age ≥ 18 years old
3. Using as a single agent or in combination with Opdivo (nivolumab)
OR
1. Diagnosis of hepatocellular carcinoma (HCC)
2. Previous treatment with sorafenib
3. Age ≥ 18 years old
OR
1. Diagnosis of locally advanced or metastatic differentiated thyroid cancer (DTC), radioactive iodine-refractory or
ineligible
2. Previous treatment with VEGFR-targeted therapy
3. Age ≥ 12 years old
Initial approval: 1 year
Continuation of treatment requires of a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 30
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Calquence
Coverage requires the following:
1. Diagnosis of mantle cell lymphoma (MCL)
2. Treatment failure or intolerance to at least one prior therapy
OR
1. Diagnosis of chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL)
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Camzyos
Coverage requires the following:
1. Diagnosis of symptomatic obstructive hypertrophic cardiomyopathy (HCM)
2. New York Heart Association (NYHA) class II-III
3. Age ≥ 18 years old
4. Left ventricular ejection fraction (LVEF) > 55%
5. Trial and failure, contraindication, or intolerance to a beta blocker or calcium channel blocker
Initial approval: 1 year
Renewal requires that the medication is providing clinical benefit and that LVEF is ≥ 50%
Caprelsa
Coverage will be provided for the treatment of patients with metastatic or unresectable locally advanced medullary thyroid
cancer
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 31
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Caplyta
Coverage requires the following:
Trial and failure, contraindication, or intolerance to two preferred second generation antipsychotics (examples include:
aripiprazole, clozapine, risperidone, quetiapine, olanzapine, ziprasidone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
carglumic acid
(Carbaglu)
Coverage requires the following:
1. Adjunctive and maintenance therapy for the treatment of hyperammonemia due to NAGSD, a deficiency of the
hepatic enzyme N-acetylglutamate synthase (NAGS)
2. Deficiency must be confirmed by enzyme or DNA mutation analysis
Initial approval for NAGSD: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
OR
1. Adjunctive treatment of acute hyperammonemia due to propionic acidemia (PA) or methylmalonic acidemia (MMA)
2. Diagnosis must be confirmed by analysis of organic acids in urine and assessment of the acylcarnitine profile in
blood
Approval for PA or MMA: 60 days
Caverject
May be covered for the diagnosis of erectile dysfunction dependent on the plan’s benefit with quantity limit restrictions
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 32
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Cayston
Coverage is provided for the treatment of Pseudomonas aeruginosa infection in members with cystic fibrosis
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Cerdelga
Coverage requires the following:
1. Age ≥ 18 years old
2. For the long-term treatment of Gaucher disease type 1 (GD1)
3. Confirmation of diagnosis by biochemical assay showing decreased glucocerebrosidase activity in white blood
cells or skin fibroblasts AND genotyping revealing two pathogenic mutations of the glucocerebrosidase gene
4. Two symptomatic manifestations of the disease are present, such as anemia, thrombocytopenia, bone disease,
hepatomegaly, or splenomegaly
5. CYP2D6 genotyping by an FDA-cleared test reveals an extensive metabolizer (EM), intermediate metabolizer (IM),
or poor metabolizer (PM)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
cetrorelix
(Cetrotide)
Coverage requires the following:
1. It is being prescribed to treat infertility in accordance with generally accepted medical practice
2. The members benefit provides for coverage for infertility medications
3. Will not be covered if being used as part of assisted reproductive treatment (ART)
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 33
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Chenodal
Coverage requires the following:
1. Treatment of gallstones
2. Ineligible for surgery
3. Treatment failure or intolerance to Actigall (ursodiol)
Coverage is limited to 24 months
Cholbam
Coverage requires the following:
1. Prescribed by or in consultation with hepatologist or gastroenterologist
2. Treatment of bile acid synthesis disorder due to single enzyme defects (SEDs)
OR
1. Adjunctive treatment of peroxisomal disorders (PDs) including Zellweger spectrum disorders in patients who exhibit
manifestation of liver disease, steatorrhea or complications from decreased fat-soluble vitamin deficiency
2. Prescribed by or in consultation with a hepatologist or gastroenterologist

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 34
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
chorionic
gonadotropin (HCG)
(Novarel)
Coverage requires the following:
1. It is being prescribed to treat infertility in accordance with generally accepted medical practice.
2. The members benefit provides for coverage for infertility medications
3. Coverage may be provided in accordance with your medical fertility benefit
OR
For the diagnosis of:
1. Hypogonadotrophic hypogonadism secondary to a pituitary deficiency in males
OR
1. Prepubertal cryptorchidism not caused by anatomic obstruction
NC
NC
Cibinqo
Coverage requires the following:
1. Diagnosis of moderate to severe atopic dermatitis (AD)
2. Age ≥ 12 years old
3. Trial and treatment failure of one of the following: high potency topical corticosteroid, tacrolimus, pimecrolimus,
cyclosporine, methotrexate, azathioprine, or mycophenolate mofetil
4. Cannot be used in combination with other biologic agents indicated for severe atopic dermatitis
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 35
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Cimzia
Coverage requires the following:
1. Diagnosis of Crohn’s Disease
2. Age ≥ 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
OR
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, leflunomide, hydroxychloroquine, sulfasalazine)
OR
1. Diagnosis of Ankylosing Spondylitis
2. Age ≥ 18 years old
OR
1. Diagnosis of Psoriatic Arthritis
2. Age ≥ 18 years old
OR
1. Diagnosis of Psoriasis
2. Age ≥ 18 years old
3. Trial and treatment failure of one topical steroid
OR
1. Diagnosis of active Non-Radiographic Axial Spondyloarthritis with objective signs of inflammation
2. Age > 18 years old
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 36
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Cometriq
Coverage is provided for the treatment of patients with progressive, metastatic medullary thyroid cancer. Therapy is
considered investigational for all other conditions
Continuation of treatment requires a lack of disease progression
Compounds
Coverage requires the following:
1. The compound is medically necessary for the member’s condition
2. The compound contains only FDA-approved drugs
3. There are no appropriate FDA-approved commercial formulations of the compound available
4. There is medical literature to support the safety, effectiveness and route of administration of the compound

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 37
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Continuous Glucose
Monitors
Dexcom G6
Dexcom G7
Freestyle Libre 14 day
Freestyle Libre 2 14 day
Freestyle Libre 3
Coverage requires the following:
1. Member is insulin-requiring
OR
1. Member has a diagnosis of diabetes and history of problematic hypoglycemia with at least one of the following:
a. Recurrent (more than one) level 2 hypoglycemia events (glucose < 54 mg/dL (3.0mmol/L) that persist
despite multiple (more than one) attempts to adjust medication(s) and/or modify the diabetes treatment
plan
b. A history of one level 3 hypoglycemia event (glucose < 54 mg/dL (3.0mmol/L)) characterized by altered
mental and/or physical state requiring third-party assistance for treatment of hypoglycemia
OR
1. Member has a diagnosis of diabetes and is currently pregnant and experiencing post prandial hyperglycemia
OR
1. Physician attests to active participation in the Michigan Collaborative for Type 2 Diabetes (MCT2D) Collaborative
Quality Initiative (CQI)
OR
1. Physician attests to active participation in the Provider Delivered Care Management (PDCM) program AND attests
that the member has a diagnosis of diabetes (Type 1 or Type 2)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 38
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Contraceptives
Coverage for $0 copayment will be provided when:
1. Used for the prevention of pregnancy
2. Trial and treatment failure or intolerance to at least three generic contraceptive medications
Contrave
Coverage requires the following:
1. Age ≥ 18 years old
2. BMI ≥ 30, or ≥ 27 with one weight related comorbid condition
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active
participation for a minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food
diaries, exercise logs, program receipts, app participation, etc.) if member does not have access to a covered
BCBSM/BCN program
5. Not to be used in combination with other weight loss products
Initial approval: 6 months
Continued coverage will be reviewed annually and may be provided if the member has maintained a 5% weight loss from
baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30 days) and BMI ≥
18.5 kg/m2 must be submitted to the plan for review
NC
NC
Copiktra
Coverage requires the following:
1. Diagnosis of relapsed or refractory chronic lymphocytic leukemia (CLL or small lymphocytic lymphoma (SLL)) after
at least two prior therapies

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 39
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Cotellic
Coverage requires the following:
1. Diagnosis of unresectable or metastatic melanoma with a BRAF V600E or V600K mutation
2. Using in combination with Zelboraf
OR
1. Diagnosis of histiocytic neoplasms
Initial approval: 1 year
Continuation of coverage requires a lack of disease progression
Crinone 8%
Coverage requires the following:
1. It is being prescribed to treat infertility in accordance with generally accepted medical practice
2. The members benefit provides for coverage for infertility medications
3. Will not be covered if being used as part of assisted reproductive treatment (ART)
NC
NC
Cutaquig
Requires appropriate diagnosis for coverage, subcutaneous administration and other criteria may apply depending on
diagnosis. Dosing must be based on ideal body weight (IBW) unless the patient’s BMI is greater than 30. If the patient’s BMI
is greater than 30 or if actual body weight is 20-30% greater than IBW, adjusted body weight must be used
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Cuvitru
Requires appropriate diagnosis for coverage, subcutaneous administration and other criteria may apply depending on
diagnosis. Dosing must be based on ideal body weight (IBW) unless the patient’s BMI is greater than 30. If the patient’s BMI
is greater than 30 or if actual body weight is 20-30% greater than IBW, adjusted body weight must be used
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 40
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Cystadrops
Coverage is provided for the treatment of corneal cystine crystal accumulation in patients with cystinosis, when taking in
combination with oral Cystagon.
Cystaran
Coverage is provided for the treatment of corneal cystine crystal accumulation in patients with cystinosis, when taking in
combination with oral Cystagon
Daurismo
Coverage requires the following:
Treatment of newly diagnosed acute myeloid leukemia (in combination with low-dose cytarabine) in adult patients who are ≥
75 years of age or who have comorbidities that preclude use of intensive induction chemotherapy
Limitations of use: Has not been studied in patients with severe renal impairment or moderate to severe hepatic impairment
Daybue
Coverage requires the following:
1. Diagnosis of classic Rett syndrome consistent with the RettSearch Consortium diagnostic criteria
2. Does not have atypical or variant Rett syndrome
3. Age ≥ 2 years old
Initial approval: 6 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 41
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Dayvigo
Coverage requires treatment failure of ONE of the following: immediate-release zolpidem (Ambien), eszopiclone (Lunesta),
zaleplon (Sonata), trazodone (Desyrel), or doxepin (Silenor)
Coverage will not be approved for combination therapy with other sedative hypnotics
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
deferasirox
(Exjade)
Coverage requires the following:
1. Chronic iron overload due to transfusions
2. ≥ 2 years of age
OR
1. Chronic iron overload in nontransfusion-dependent thalassemia syndromes
2. ≥ 10 years of age
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 42
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
deferasirox
(Jadenu)
Coverage requires the following:
1. Chronic iron overload due to transfusions:
a. ≥ 2 years of age
OR
2. Chronic iron overload in nontransfusion-dependent thalassemia syndromes:
a. ≥ 10 years of age
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
deferiprone tablets
(Ferriprox)
Coverage requires the following:
1. Age ≥ 8 years old
2. Diagnosis of transfusional iron overload due to thalassemia syndromes when current chelation therapy is
inadequate
3. Treatment failure or intolerance to generic Jadenu or generic Exjade
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 43
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
deferiprone solution
(Ferriprox)
Coverage requires the following:
1. Age ≥ 3 years old
2. Diagnosis of transfusional iron overload due to thalassemia syndromes when current chelation therapy is
inadequate
3. Treatment failure or intolerance to generic Jadenu or generic Exjade
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
deflazacort
(Emflaza)
Coverage requires the following:
1. Diagnosis of Duchenne Muscular Dystrophy (DMD)
2. Age ≥ 2 years old
3. Trial and treatment failure, contraindication, or intolerance to adequate doses (0.75 mg/kg/day) of generic of
prednisone or prednisolone
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 44
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Descovy
Coverage with $0 copayment will be provided when:
1. Using for pre exposure prophylaxis (PrEP) for HIV
2. Negative HIV test within the past 3 months
3. Trial and intolerance or contraindication to generic Truvada 200mg/300mg
OR
1. Coverage will be provided for the treatment of HIV infection
Initial approval: 2 years
Renewal requires that current criteria are met, and that the medication is providing clinical benefit AND documentation of a
negative HIV test result within the past 3 months
Desvenlafaxine ER
Coverage requires trial and failure of at least three antidepressant agents
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Dexilant /
dexlansoprazole
Coverage requires failure of or intolerance to four of the following generic alternatives: omeprazole (Prilosec),
esomeprazole (Nexium), pantoprazole (Protonix), lansoprazole (Prevacid/Prevacid Solutab), and rabeprazole (Aciphex)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 45
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Diacomit
Coverage requires the following:
1. Diagnosis of Dravet Syndrome
2. Trial and failure, contraindication, or intolerance to 2 of the following generic options: valproic acid, clobazam, or
topiramate
3. Using in combination with clobazam
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
dichlorphenamide
(Keveyis)
Coverage requires the following:
1. Diagnosis of primary hyperkalemic periodic paralysis, primary hypokalemic periodic paralysis and related variants
as confirmed by a genetic test or positive family history
2. Trial and failure of lifestyle modifications such as diet (potassium intake alterations) and exercise modifications
3. Trial and treatment failure of acetazolamide
diclofenac 2%
external solution
(Pennsaid 2%)
Coverage requires the following:
1. Diagnosis of osteoarthritis of the knee
2. Trial of or intolerance to generic oral diclofenac and at least two other oral, traditional NSAIDs
3. Trial of generic Pennsaid 1.5% topical solution
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Please note: Coverage will not be provided in the presence of concurrent therapy with oral NSAIDs
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 46
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
diclofenac
potassium
(Zipsor)
Coverage requires the following:
1. Age ≥ 12 years old
2. Diagnosis of acute pain
3. Trial and failure of oral diclofenac
4. Trial and failure of two other preferred oral NSAIDs
Initial approval: 3 months
NC
NC
diclofenac sodium
3% gel
(Solaraze)
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of actinic keratosis
3. Trial and failure or intolerance to cryotherapy or phototherapy
4. Trial and treatment failure or intolerance to a generic or preferred topical fluorouracil
5. Trial and treatment failure or intolerance to generic imiquimod 5%
Initial approval: 3 months
Renewal requires recurrence and/or new lesions
Dojolvi
Coverage requires the following:
1. Treatment of molecularly confirmed long-chain fatty acid oxidation disorders
2. Following low fat/high carbohydrate diet and avoiding fasting
3. Trial of medium chain triglycerides at a maximally tolerated dose
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 47
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Doptelet
Coverage requires the following:
1. Diagnosis of thrombocytopenia in chronic liver disease
a. Age > 18 years old
b. Platelet count < 50,000/mcL
c. Scheduled to undergo a procedure
OR
2. Diagnosis of chronic immune thrombocytopenia (ITP) and persistent thrombocytopenia (platelet count <
100,000/mcL) for ≥ 3 months and requires all of the following:
a. Age > 18 years old
b. Current platelet count is < 20,000/mcL or < 30,000/mcL and has symptoms of active bleeding
c. Diagnosis confirmed by, or in consultation with a hematologist
d. Inadequate response to (e.g. unable to maintain platelet count ≥ 30,000/mcL) OR are not candidates for
therapy with corticosteroids, immunoglobulins, or splenectomy with an insufficient response to previous
treatment
Initial approval for diagnosis of thrombocytopenia in chronic liver disease: 60 days
Initial approval for diagnosis of chronic ITP: 3 months
Renewal requires a recent platelet count between 50,000 and 200,000/mcL
Doryx MPC
Coverage requires the following:
Trial and treatment failure or intolerance to generic doxycycline monohydrate (Monodox) AND generic doxycycline hyclate
immediate release (Vibramycin)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 48
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Doxepin
topical cream
Coverage requires the following:
1. Diagnosis of atopic pruritis or lichen simplex chronicus
2. Trial and treatment failure of two topical steroids, one of which must be a medium or high potency product
3. Trial and treatment failure to one preferred topical calcineurin inhibitor (tacrolimus, pimecrolimus)
OR
1. Diagnosis of peripheral neuropathic pain
2. Trial and treatment failure of two over-the-counter topical analgesics
3. Trial and treatment failure of one preferred topical non-steroidal anti-inflammatory drug (NSAID)
Approval: 60 days
doxycycline hyclate
(Doryx)
Coverage requires the following:
Trial and treatment failure or intolerance to generic doxycycline monohydrate (Monodox) AND generic doxycycline hyclate
immediate release (Vibramycin)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
doxycycline
monohydrate
(Adoxa
/ Adoxa Pak)
Coverage requires the following:
Trial and treatment failure or intolerance to generic doxycycline monohydrate (Monodox) AND generic doxycycline hyclate
immediate release (Vibramycin)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 49
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
droxidopa
(Northera)
Coverage requires the following:
1. Diagnosis of orthostatic hypotension
2. Age ≥18 years old
3. Trial and treatment failure of midodrine
4. Trial and treatment failure of fludrocortisone
NC
NC
Duopa
Coverage requires the following:
1. Diagnosis of advanced Parkinson’s disease
2. Member has a feeding tube

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 50
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Dupixent
Coverage requires the following:
1. Diagnosis of moderate to severe atopic dermatitis
2. Age ≥ 6 months old
3. Trial and treatment failure of one of the following: high potency topical corticosteroid, tacroliumus, pimecrolimus,
cyclosporine, methotrexate, azathioprine, or mycophenolate mofetil
4. Cannot be used in combination with other biologic agents indicated for severe atopic dermatitis
OR
1. Diagnosis of eosinophilic asthma
2. Age ≥ 6 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. Eosinophil count ≥ 150 cells/microliter at initiation of treatment
5. Failure to maintain adequate control after at least a 3 month trial of daily oral corticosteroids or high dose inhaled
corticosteroids in combination with:
a. LABA (long acting inhaled β2 agonist)
OR
b. Leukotriene modifier
OR
c. LAMA (long acting muscarininc antagonist) in adults and children ≥ 12 years old
6. Cannot be used in combination with other biologic agents indicated for asthma
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 51
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Dupixent
(continued)
OR
1. Diagnosis of oral corticosteroid dependent asthma
2. Age ≥ 6 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. Failure to maintain adequate control after at least a 3 month trial of daily oral corticosteroids AND high dose
inhaled corticosteroids in combination with:
a. LABA (long acting inhaled β2 agonist)
OR
b. Leukotriene modifier
OR
c. LAMA (long acting muscarininc antagonist) in adults and children ≥ 12 years old
5. Cannot be used in combination with other biologic agents indicated for asthma
OR
1. Diagnosis of chronic rhinosinusitis with nasal polyposis (CRSwNP)
2. Age > 18 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. CRSwNP is recurring despite previous treatment with intranasal corticosteroids
5. Cannot be used in combination with other biologic agents indicated for CRSwNP
OR
1. Diagnosis of eosinophilic esophagitis (EoE)
2. Age ≥ 1 year old
3. Weight ≥ 15 killograms
4. Trial and treatment failure of a proton pump inhibitor (PPI)
OR
4. Trial and treatment failure of a swallowed topical glucocorticoid
OR
1. Diagnosis of Prurigo Nodularis (PN)
2. Age ≥ 18 years old
3. Trial and treatment failure with topical steroids or topical calcineurin inhibitors
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 52
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Duvyzat
Coverage requires the following:
1. Age ≥ 6 years old
2. Diagnosis of Duchenne muscular dystrophy (DMD), confirmed by genetic testing demonstrating a mutation of the
DMD gene
3. Must be on a stable dose of systemic corticosteroids prior to starting therapy with Duvyzat
4. Must be ambulatory prior to starting therapy with Duvyzat
Initial approval: 1 year
Renewal requires that current criteria are met and that the medication is providing clinical benefit
Dyanavel XR
Coverage requires the following:
1. Diagnosis of Attention Deficit Hyperactivity Disorder
2. Age ≥ 6 years old
3. Treatment failure or intolerance to both a generic methylphenidate and a generic amphetamine product, one of
which must be a long-acting formulation
OR
3. Member cannot swallow tablets/capsules and has tried and failed one of the agents that can be opened and
sprinkled on applesauce (methylphenidate ER, Adderall XR)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 53
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ecoza
Coverage requires the following:
1. Diagnosis of tinea pedis
2. Treatment failure of 2 topical over-the-counter antifungal agents
3. Treatment failure of two oral generic antifungal agents (fluconazole, itraconazole or terbinafine)
NC
NC
Edarbi
Coverage requires that the member has experienced treatment failure or intolerance to two generic Angiotensin II Receptor
Blockers (ARB)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Edarbyclor
Coverage requires that the member has experienced treatment failure or intolerance to two generic Angiotensin II Receptor
Blockers (ARB)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Edex
May be covered for the diagnosis of erectile dysfunction dependent on the plan’s benefit with quantity limit restrictions
NC
NC
Edluar
Coverage requires treatment failure of 3 of the following: immediate-release zolpidem (Ambien), eszopiclone (Lunesta),
zaleplon (Sonata), trazodone (Desyrel), or doxepin (Silenor), one of which must be generic Ambien
Coverage will not be approved for combination therapy with other sedative hypnotics
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 54
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Egrifta
Coverage requires the following:
1. Diagnosis of HIV
2. Currently receiving antiretroviral therapy (ART)
3. Medical complication caused by excess abdominal fat
4. Medical complication due to excess abdominal fat is not responsive to conventional therapy
Initial approval: 6 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Elepsia XR
Coverage requires the following:
1. Treatment of seizure disorder/epilepsy
2. Treatment failure or intolerance to three generic or preferred alternatives, one of which must be generic Keppra
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
eletriptan
(Relpax)
Coverage requires trial of 2 of the following generic triptans: Imitrex, Maxalt, Amerge, or Zomig/ZMT
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 55
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Emgality 100mg/ml
Coverage requires the following:
1. For the treatment of episodic cluster headache
2. Age ≥18 years old
Initial approval: 6 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Emgality 120mg/ml
Coverage requires the following:
1. Age ≥ 18 years old
2. For preventive treatment of migraine headaches
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 56
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Empaveli
Coverage requires the following:
1. Diagnosis of paroxysmal nocturnal hemoglobinuria (PNH)
2. Age ≥ 18 years old
3. Flow cytometric confirmation of PNH type III red cells
4. Had at least 1 transfusion in 12 months preceding Empaveli
OR
4. History of major adverse thrombotic vascular events from thromboembolism
OR
4. Patient has high disease activity defined as a lactic dehydrogenase (LDH) level ≥ 1.5 times the upper limit of
normal with one of the following symptoms:
i. Weakness
ii. Fatigue
iii. Hemoglobinuria
iv. Abdominal pain
v. Dyspnea
vi. Hemoglobin < 10 g/dL
vii. A major vascular event
viii. Dysphagia
ix. Erectile dysfunction
5. Must not be used in combination with Soliris®, Ultomiris®, or other medications used to treat PNH
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 57
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Emsam
Coverage requires the following:
1. Treatment of major depressive disorder
2. Age > 18 years old
3. Member has experienced treatment failure or intolerance to at least three different generic antidepressants
emtricitabine
200mg-tenofovir
300mg
(Truvada)
Coverage for $0 copayment will be provided when:
1. For prevention of HIV infection in members who are at a high risk of getting HIV
2. Member is not taking concomitant antiretroviral therapy

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 58
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Enbrel
Coverage requires the following:
1. Diagnosis Psoriatic Arthritis
2. Age ≥ 2 years old
OR
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
OR
1. Diagnosis of Ankylosing Spondylitis
2. Age ≥ 18 years old
OR
1. Diagnosis of Psoriasis
2. Age ≥ 4 years old
3. Trial and treatment failure of one topical steroid
OR
1. Diagnosis of Juvenile Idiopathic Arthritis (JIA)
2. Age ≥ 2 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, leflunomide)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 59
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Endari
Coverage requires the following:
1. Diagnosis of sickle cell disease
2. Age ≥ 5 years old
3. Prescribed by or in consultation with a hematologist
4. Patient has experienced 2 or more sickle cell-related crises in the past 12 months
5. Trial and treatment failure for at least 6 months, contraindication, or intolerance to hydroxyurea
6. Trial and failure of over-the-counter (OTC) L-glutamine
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Endometrin
Coverage requires the following:
1. It is being prescribed in accordance with generally accepted medical practice
2. Requires a previous trial of Crinone
3. The members benefit provides coverage for infertility medications
Coverage is provided in accordance with your medical fertility benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 60
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Enspryng
Coverage requires the following:
1. Diagnosis of neuromyelitis optica spectrum disorder (NMOSD) in adult patients who are anti-aquaporin-4 (AQP4)
antibody positive
Enspryng will not be approved for use in combination with Soliris or Uplizna
Initial approval: 1 year
Continuation of treatment requires of a lack of disease progression
Enstilar
Coverage requires the following:
1. Diagnosis of psoriasis
2. Trial and treatment failure with a high potency topical steroid in combination with generic Dovonex
3. Trial and treatment failure with generic Taclonex
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 61
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Eohilia
Coverage requires the following:
1. Diagnosis of of eosinophilic esophagitis (EoE)
2. Age ≥ 11 years old
3. Trial and failure, contraindication, or intolerance to a proton pump inhibitor (PPI)
OR
3. Trial and failure, contraindication, or intolerance to a swallowed topical glucocorticoid such as inhaled budesonide
Approval: 12 weeks
Epclusa /
Sofosbuvir +
Velpatasvir
Coverage requires the following:
1. Age ≥ 3 years old or weight ≥ 17kg
2. Diagnosis of chronic hepatitis C genotype 1, 2, 3, 4, 5, or 6
3. If treatment experienced, documentation of previous treatment experience for Hepatitis C
4. If cirrhosis is present: documentation of decompensated or compensated cirrhosis
Drug will be reviewed based on a case by case basis utilizing AASLD guidelines and FDA approved package labeling

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 62
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Epidiolex
Coverage requires the following:
1. Diagnosis of Lennox-Gastaut syndrome
2. Trial and failure, contraindication, OR intolerance to at least 2 generic alternatives for the treatment of seizures
OR
1. Diagnosis of Dravet syndrome
2. Trial and failure, contraindication, OR intolerance to 2 of the following generic options: valproic acid, clobazam, or
topiramate
OR
1. Treatment of seizures associated with tuberous sclerosis complex
2. Trial and failure, contraindication, OR intolerance to 3 generic alternatives for the treatment of seizures
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 63
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Eprontia
Coverage requires the following:
1. Treatment of seizure disorder/epilepsy
2. Treatment failure or intolerance to at least 3 generic alternatives, one of which must be generic topiramate
(Topamax)
OR
2. Member is unable to swallow tablets/capsules
OR
1. Diagnosis of Lennox-Gastaut Syndrome
2. Treatment failure or intolerance to at least 2 generic alternatives, one of which must be generic topiramate
(Topamax)
OR
2. Member is unable to swallow tablets/capsules
OR
1. For preventative treatment of migraine headaches
2. Age ≥ 12 years old
3. Treatment failure or intolerance to 3 generic alternatives for the prevention of migraines, one of which must be
generic topiramate (Topamax)
OR
3. Member is unable to swallow tablets/capsules
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 64
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Erivedge
Coverage requires the following:
1. Diagnosis of locally advanced basal cell carcinoma
2. Carcinoma occurred again following surgery OR the member not able to have surgery
3. Not a candidate for radiation
OR
1. Diagnosis of metastatic basal cell carcinoma
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Erleada
Coverage requires the following:
1. Metastatic castration-sensitive prostate cancer
OR
1. Non-metastatic castration-resistant prostate cancer
erlotinib
(Tarceva)
Coverage is provided for the treatment of the FDA approved indications
Eucrisa
Coverage requires trial and treatment failure of one of the following: a topical steroid, generic Protopic, or generic Elidel
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 65
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Eulexin
Coverage requires the following:
1. Diagnosis of locally confined or metastatic carcinoma of the prostate
2. Age ≥ 18 years old
3. Using in combination with luteinizing hormone-releasing hormone (LHRH)-agonists
4. Trial and failure, contraindication, or intolerance to generic Casodex (bicalutamide)
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 66
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
everolimus
(Afinitor)
Coverage requires the following:
1. Diagnosis of HR-positive, HER-2 negative advanced breast cancer (in combination with exemestane)
2. Previous treatment failure with letrozole or anastrozole
OR
1. Treatment of progressive pancreatic neuroendocrine tumors in patients with unresectable, locally advanced or
metastatic disease
OR
1. Treatment of progressive, well-differentiated nonfunctional gastrointestinal or lung neuroendocrine tumors in
patients with unresectable, locally advanced or metastatic disease
OR
1. Treatment of advanced renal cell carcinoma after Sutent (sunitinib) or Nexavar (sorafenib) failure
OR
1. Treatment of renal angiomyolipoma with tuberous sclerosis complex (TSC) not requiring immediate surgery
OR
1. Treatment of subependymal giant cell astrocytoma (SEGA) associated with TSC that requires therapeutic
intervention but cannot be curatively resected
2. Age > 1 year old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 67
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
everolimus
(Afinitor
Disperz)
Coverage requires the following:
1. Adjunctive treatment of partial-onset seizures associated with tuberous sclerosis complex (TSC)
2. Age ≥ 2 years old
OR
1. Treatment of subependymal giant cell astrocytoma (SEGA) associated with TSC that requires therapeutic
intervention but cannot be curatively resected
2. Age ≥ 1 year old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 68
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Evrysdi
Coverage requires the following:
Diagnosis of type 1, 2, or 3 Spinal Muscular Atrophy (SMA) confirmed by genetic testing AND
1. Prescribed by or in consultation with a neurologist specializing in neuromuscular disorders
2. Submission of a baseline, age appropriate exam to establish baseline motor function and ability
3. Patient is not currently taking SMN2-targeting antisense oligonucleotide or SMN2 splicing modifier AND patient has
not had gene therapy treatment for SMA (or being considered for treatment with any other gene therapy for SMA)
4. Patient is not requiring invasive ventilation or tracheostomy
5. The requesting physician attests to providing clinical outcome information within the Audaire Health™ provider
portal as requested by BCBSM
Initial approval: 1 year
Continuation of treatment requires submission of repeat motor ability assessment and documentation of response to
therapy defined as a clinically significant improvement in SMA-associated motor milestones and motor function (for
example, progression, stabilization, or decreased functional motor decline) compared to predicted natural history and
progression
exemestane
(Aromasin)
Coverage for $0 copayment will be provided when:
1. The member is a woman at least 35 years of age
2. The medication is being used for prevention of primary breast cancer
3. Members classified as high risk
4. Does not have a history of breast cancer
5. Member is currently post-menopausal
6. Member is not taking any estrogen containing products

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 69
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Exservan
Coverage requires the following:
1. Diagnosis of Amyotrophic Lateral Sclerosis (ALS)
2. Trial of generic riluzole tablets
OR
2. Difficulty swallowing
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 70
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Fabhalta
Coverage requires the following:
1. Diagnosis of paroxysmal nocturnal hemoglobinuria (PNH)
2. Age ≥ 18 years old
3. Flow cytometric confirmation of PNH type III red cells
4. Had at least 1 transfusion in 6 months preceding Fabhalta
OR
4. Documented history of major adverse thrombotic vascular events from thromboembolism
OR
4. Patient has high disease activity defined as a lactic dehydrogenase (LDH) level ≥ 1.5 times the upper limit of
normal with one of the following symptoms:
a. Weakness
b. Fatigue
c. Hemoglobinuria
d. Abdominal pain
e. Dyspnea
f. Hemoglobin < 10 g/dL
g. A major vascular event
h. Dysphagia
i. Erectile dysfunction
5. Must not be used in combination with Soliris, Ultomiris, or other medications to treat PNH
6. Trial and failure, contraindication, or intolerance to Empaveli
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 71
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Fabior
Coverage requires the following:
Trial and failure, contraindication, or intolerance to both generic adapalene (Differin) and generic tretinoin (Retin-A, Avita)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Fanapt
Coverage requires the following:
Trial and failure, contraindication, or intolerance to two preferred second generation antipsychotics (examples include:
aripiprazole, clozapine, risperidone, quetiapine, olanzapine, ziprasidone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 72
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Fasenra pen
Coverage requires the following:
1. Diagnosis of severe uncontrolled eosinophilic asthma
2. Age ≥ 6 years old
3. Patient is currently receiving and will continue to receive standard of care regimen
4. Severe eosinophilic asthma identified by:
a. Blood eosinophils greater than or equal to 150 cells/microliter at initiation of treatment
AND
b. Failure to maintain adequate control after at least a 3 month trial of daily oral corticosteroids or high
dose inhaled corticosteroids in combination with:
i. LABA (long acting inhaled β2 agonist)
OR
ii. Leukotriene modifier
OR
iii. LAMA (long acting muscarinic antagonist) in adults and children ≥ 12 years old
5. Cannot be used in combination with other biologic agents indicated for uncontrolled eosinophilic asthma
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 73
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
fentanyl citrate
buccal lollipop
(Actiq)
Coverage requires the following:
1. Medication is being used for the treatment of breakthrough cancer pain
2. Member is tolerant to high dose opioids
3. Currently receiving a long acting opioid
4. Treatment failure or intolerance to oral immediate release opioids (examples include, but not limited to: morphine,
oxycodone, or hydrocodone containing products)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Fentora;
fentanyl citrate
buccal tablet
Coverage requires the following:
1. Medication is being used for the treatment of breakthrough cancer pain
2. Member is tolerant to high dose opioids
3. Currently receiving a long acting opioid
4. Treatment failure or intolerance to oral immediate release opioids (examples include, but not limited to: morphine,
oxycodone, or hydrocodone containing products)
5. Treatment failure or intolerance to generic Actiq
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Fetzima
Coverage requires trial and failure of at least three antidepressant agents
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 74
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Filspari
Coverage requires the following:
1. To reduce proteinuria in adults with primary immunoglobulin A nephropathy (IgAN) at risk of rapid disease
progression
2. Age ≥ 18 years old
3. Trial and failure to maximally tolerated dose of angiotensin converting enzyme (ACE) inhibitor or angiotensin
receptor blocker (ARB) therapy unless contraindicated
4. Trial and failure, contraindication, or intolerance to generic methylprednisolone, prednisolone, or prednisone
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Filsuvez
Coverage requires the following:
1. For the treatment of wounds associated with dystrophic epidermolysis bullosa (DEB) and junctional epidermolysis
bullosa (JEB)
2. Age ≥ 6 months old
3. Open wounds requiring treatment
4. Must not have current evidence or a history of malignancy (e.g., basal cell carcinoma, squamous cell carcinoma),
or active infection in the area undergoing treatment
5. Must not have undergone stem cell transplant or gene therapy for the treatment of inhereited epidermolysis bullosa
Initial approval: 6 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 75
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Finacea foam
Coverage requires the following:
1. Trial and failure, contraindication, or intolerance to generic topical metronidazole
2. Trial and failure, contraindication, or intolerance to generic oral tetracycline, generic doxycycline or generic
minocycline
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Fintepla
Coverage requires the following:
1. Treatment of seizures associated with Dravet syndrome
2. Age ≥ 2 years old
3. Trial and treatment failure of two of the following: valproic acid, clobazam, topiramate
OR
1. Treatment of seizures associated with Lennox-Gastaut syndrome
2. Age ≥ 2 years old
3. Trial and treatment failure of 2 generic alternatives for the treatment of seizures
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 76
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Firazyr
Coverage requires the following:
1. Treatment of acute attacks of hereditary angioedema (HAE)
2. Diagnosis confirmed by genetic testing or with the following laboratory findings:
i. C4 level below the limits of the laboratory’s normal reference range (normal range = 16-58 mg/dL)
ii. C1INH (antigenic or function) below the limits of the laboratory’s normal reference range (normal range ≥ 41%)
3. Prescribed by an immunologist, allergist or hematologist
4. Trial and treatment failure of generic Firazyr (icatibant)
5. Not to be used in combination with other products indicated for acute HAE attacks
Initial approval: 1 year
Renewal requires objective data documenting at least 50% improvement in time to relief of symptoms of acute attacks
and maintenance of improvement of symptoms
Firdapse
Coverage requires the following:
1. Treatment of Lambert-Eaton myasthenic syndrome
2. Age ≥ 6 years old
3. Prescribed by a neurologist
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 77
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Flector,
Diclofenac
Epolamine 1.3%
patch
Coverage requires the following:
1. Diagnosis of acute pain due to minor strains, sprains or contusions
2. Trial of or intolerance to generic oral diclofenac and at least two other oral, traditional NSAIDs
Initial approval: 3 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Please note: Coverage will not be provided in the presence of concurrent therapy with oral NSAIDs
NC
NC
Follistim AQ
Coverage requires the following:
1. It is being prescribed to treat infertility in accordance with generally accepted medical practice
2. Requires a previous trial of Gonal-f or Gonal-f RFF
3. The members benefit provides for coverage for infertility medications
Coverage is provided in accordance with your medical fertility benefit
Fosamax Plus D
Coverage requires trial and treatment failure or intolerance to two of the following:
1. Actonel (risedronate)
2. Boniva (ibandronate)
3. Fosamax (alendronate)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 78
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Fotivda
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of relapsed or refractory advanced renal cell carcinoma (RCC)
3. Received at least 2 prior systemic therapies
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
frovatriptan
(Frova)
Coverage requires trial of 2 of the following generic triptans: Imitrex, Maxalt, Amerge, or Zomig/ZMT
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Fruzaqla
Coverage requires the following:
1. Diagnosis of metastatic colorectal cancer (mCRC), previously treated with fluoropyrimidine-, oxaliplatin-, and
irinotecan-based chemotherapy, an anti-vascular endothelial growth factor (VEGF) therapy, and, if RAS wild-type
and medically appropriate, an anti-epidermal growth factor receptor (EGFR) therapy
2. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Fulphila
Coverage requires trial and failure or intolerance to Neulasta and Ziextenzo

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 79
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Furoscix
Coverage requires the following:
1. Diagnosis of New York Heart Association (NYHA) Class II or Class III chronic heart failure
2. Age ≥ 18 years old
3. Patient is experiencing an increase in signs and symptoms of congestion due to fluid overload
4. Established on background therapy with a loop diuretic
5. Patient is stable and does not require emergency care or hospitalization for heart failure, acute pulmonary edema,
or other conditions
Approval: 60 days
gabapentin
(Gralise)
Coverage requires the following:
Diagnosis of post-herpetic neuralgia (PHN)
AND
1. ≤ 65 years of age
2. Trial of generic Neurontin (gabapentin)
3. Trial of generic tricyclic antidepressant (ex: amitriptyline, desipramine, imipramine)
OR
1. ≥ 65 years of age
2. Trial of generic Neurontin (gabapentin)
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 80
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Galafold
Coverage requires the following:
1. Diagnosis of Fabry’s disease confirmed by genetic testing showing an amenable mutation in the GLA gene
a. In addition for males: serum assay of enzyme α-galactosidase showing decreased activity in plasma and/or
leukocytes
2. Age ≥ 18 years old
3. Prescribed by or in consultation with a geneticist or metabolic specialist
4. Initiation of therapy should begin as follows:
a. Males with classic disease: at time of diagnosis
b. Females and males with atypical disease: once patient is showing symptoms of Fabry’s disease
Galafold will not be approved for use in combination or with any other molecular chaperone or enzyme replacement therapy
for Fabry’s disease
Gammagard,
Gammaked,
Gamunex-C
Requires appropriate diagnosis for coverage, subcutaneous administration and other criteria may apply depending on
diagnosis. Dosing must be based on ideal body weight (IBW) unless the patient’s BMI is greater than 30. If the patient’s BMI
is greater than 30 or if actual body weight is 20-30% greater than IBW, adjusted body weight must be used.
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
ganirelix Acetate
(generic only)
Coverage requires the following:
1. It is being prescribed to treat infertility in accordance with generally accepted medical practice
2. The members benefit provides for coverage for infertility medications
3. Will not be covered if being used as part of assisted reproductive treatment (ART)
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 81
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Gattex
Coverage requires the following:
1. Diagnosis of Short Bowel Syndrome (SBS)
2. Dependent on parenteral support ≥ 12 months
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit, defined as a reduction in
≥ 20% of weekly parenteral nutrition volume or intravenous fluid volume
Gavreto
Coverage requires the following:
1. Age > 18 years old
2. Treatment of metastatic RET fusion-positive non-small cell lung cancer (NSCLC) as detected by an FDA-approved
test
OR
1. Age > 12 years old
2. Treatment of advanced or metastatic RET fusion-positive thyroid cancer that requires systemic therapy and who
are radioactive iodine-refractory (if radioactive iodine is appropriate)
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Gelnique
Coverage requires treatment failure or intolerance to at least 2 generic OAB (Overactive Bladder) therapies
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 82
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Gemtesa
Coverage requires the following:
1. Trial and treatment failure or intolerance to two preferred therapies for overactive bladder (OAB)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
gefitinib
(Iressa)
Coverage requires the following:
1. Diagnosis of metastatic non-small cell lung cancer (NSCLC)
2. Epidermal growth factor (EGFR) exon 19 deletions or exon 21 (l858R) substitution mutations as detected by an
FDA-approved test
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Gilotrif
Coverage requires the following:
1. Diagnosis of metastatic non-small cell lung cancer (NSCLC) whose tumors have non-resistant epidermal growth
factor receptor (EGFR) mutations as detected by an FDA-approved test
OR
2. Diagnosis of metastatic squamous NSCLC that has progressed following platinum-based chemotherapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 83
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Glassia
Coverage requires the following:
1. Age > 18 years old
2. Must be a nonsmoker
3. Member must have pre-treatment serum levels of alpha-1 antitrypsin (AAT) that are less than 11 micromol/L
measured by ELISA (less than 80 mg/dlL measured by radial immunodiffusion or less than 57 mg/dL measured by
nephelometry) consistent with phenotypes PiZZ, PiZ (null), or Pi (null, null) of AAT
a. Phenotype/genotype testing may be requested for additional support of alpha-1 antitrypsin deficiency
diagnosis
4. Member must have symptoms with their emphysema
5. Member must have deteriorating lung function, as demonstrated by a decline in the FEV1 (35-60% of predictive
value)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Gonal-f,
Gonal-f RFF
Coverage requires the following:
1. It is being prescribed to treat infertility in accordance with generally accepted medical practice
2. The members benefit provides for coverage for infertility medications
Coverage is provided in accordance with your medical fertility benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 84
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Grastek
Coverage requires the following:
1. Age 5 through 65 years old
2. Diagnosis of grass pollen-induced allergic rhinitis, confirmed by positive skin test or in vitro testing for pollen-
specific IgE antibodies for Timothy grass or cross-reactive grass pollens
3. Trial of one agent from each of the following classes:
a. Intranasal corticosteroid
b. Oral or intranasal antihistamine
Initial approval: 3 years
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 85
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Growth Hormone
(adults)
Preferred
Genotropin
Norditropin
Non-preferred
Humatrope
Ngenla
Nutropin
Nutropin AQ
Omnitrope
Saizen
Sogroya
Zomacton
Coverage requires the following:
1. Documentation of at least one known cause for pituitary disease or condition affecting pituitary function (i.e.
pituitary tumor, traumatic brain injury, surgical damage, hypothalamic disease, irradiation, trauma, history of
childhood growth hormone deficiency, or infiltrative disease), with one of the following (A, B, C, or D):
A. Failed at least one clinically validated, clearly documented growth hormone stimulation test
i. IGF-1 level below age and BMI-corrected lower limit of reference labs normal range
ii. For suspected growth hormone deficiency due to traumatic brain injury, GH stimulation test must be
administered at least one-year post brain injury
iii. For history of childhood growth hormone deficiency, GH stimulation test to be done after growth hormone
has been discontinued for at least one month
OR
B. Failed at least one clearly documented, clinically validated growth hormone stimulation test
i. IGF -1 level below age and BMI-corrected lower limit of reference labs normal range
ii. Documentation of two additional pituitary hormone deficiencies clearly of pituitary origin (other than growth
hormone) requiring hormone replacement
OR
C. Documentation of three pituitary hormone deficiencies clearly of pituitary origin (other than growth hormone)
requiring hormone replacement
i. IGF-1 level below age and BMI-corrected lower limit of reference labs normal range
OR
D. Failed at least two clearly documented, clinically validated GH stimulation tests
i. IGF-1 level below age and BMI-corrected lower limit of reference lab’s normal range
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 86
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Growth Hormone
(adults)
(continued)
OR
1. Diagnosis of AIDS wasting cachexia
2. Unexplained weight loss > 10% of baseline
3. Concomitant anti-viral therapy for the duration of treatment
OR
1. Diagnosis of short bowel syndrome
2. Receiving specialized nutritional support, which may include dietary adjustments, enteral feedings, parenteral
nutrition, fluid and micronutrient supplements
Authorization period for short bowel syndrome: 4 weeks of treatment
Coverage for a non-preferred medication requires treatment failure to ALL preferred medications (Genotropin and
Norditropin)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 87
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Growth Hormone
(pediatrics)
Preferred
Genotropin
Norditropin
Non-preferred
Humatrope
Nutropin
Nutropin AQ
Omnitrope
Saizen
Skytrofa
Sogroya
Zomacton
Coverage requires the following:
1. Diagnosis of Growth Hormone Deficiency with ONE of the following:
a. 2 subnormal growth hormone stimulation tests, or
b. 1 subnormal growth hormone stimulation test AND IGF-1 and IGFBP3 levels below normal for children of
the same age and gender, or
c. Documentation of a hypothalamic pituitary defect (such as a major congenital malformation, tumor,
surgery, irradiation, or trauma) AND a deficiency in at least one additional pituitary hormone
AND
2. Initial height measurements < 5
th
percentile for age and gender
3. Abnormal growth velocity for at least 6 months
4. Open epiphyses
OR
1. Diagnosis of Growth Hormone Deficiency due to congenital hypopituitarism in a newborn
2. Documentation of hypoglycemia with associated with growth hormone levels <5 mcg/L
AND
a. Documentation of deficiency of at least one additional pituitary hormone, or
b. Imaging to support a pituitary defect (such as ectopic posterior pituitary and pituitary hypoplasia with
abnormal stalk
OR
1. Diagnosis of Turners Syndrome, SHOX deficiency, or Noonan Syndrome
2. Initial height measurements < 5
th
percentile for age and gender
3. Abnormal growth velocity for at least 6 months
4. Open epiphyses
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 88
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Growth Hormone
(pediatrics)
(continued)
OR
1. Chronic Renal Insufficiency
2. Initial height measurements < 5
th
percentile for age and gender
3. Abnormal growth velocity for at least 6 months
4. Open epiphyses
5. If post-transplant – persistent growth failure without spontaneous catch up one year post-transplant and in whom
steroid-free immunosuppression is not feasible
OR
1. Small for Gestational Age (SGA)
2. Birth weight and/or length at least 2 standard deviations below the mean for gestational age
3. Fails to manifest catch-up growth by 2 years of age
4. Open epiphyses
Authorization period: Approved until 18
th
birthday
OR
1. Diagnosis of Prader-Willi Syndrome
OR
1. Pediatric Burn
2. Burns over at least 40% of total body surface area
Initial approval: 1 year
Coverage for a non-preferred medication requires treatment failure to ALL preferred medications (Genotropin and
Norditropin)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 89
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Haegarda
Coverage requires the following:
1. Diagnosis of hereditary angioedema (HAE)
2. Diagnosis confirmed by genetic testing or with the following laboratory findings:
i. C4 level below the limits of the laboratory’s normal reference range (normal range = 16-58 mg/dL)
ii. C1INH (antigenic or function) below the limits of the laboratory’s normal reference range (normal
range ≥ 41%)
3. History of at least 2 HAE attacks per month OR a history of attacks that are considered severe with swelling of the
face, throat or gastrointestinal tract
4. Prescribed by an immunologist, allergist or hematologist
5. Not to be used in combination with other products indicated for HAE prophylaxis
Initial approval: 1 year
Renewal requires improvement in HAE demonstrated by a 50% reduction in the number of attacks OR that the severity of
HAE attacks was reduced by 50% or more
Harvoni / Ledipasvir
+Sofosbuvir
Coverage requires the following:
1. Age 3 years or older
2. Diagnosis of chronic hepatitis C genotype 1,4,5 or 6
3. If treatment experienced, documentation of previous treatment experience for Hepatitis C
4. Trial of preferred medication: Zepatier for genotypes 1 and 4 OR Epclusa for genotypes 1,4,5 and 6 in adult
patients
5. If cirrhosis is present: documentation of decompensated or compensated cirrhosis
Drug will be reviewed on a case by case basis utilizing AASLD guidelines and FDA approved package labeling and trial and
failure of Epclusa or Zepatier
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 90
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Harvoni oral pellets
Coverage requires the following:
1. Age 3 years or older
2. Diagnosis of chronic hepatitis C genotype 1,4,5 or 6
3. If treatment experienced, documentation of previous treatment experience for Hepatitis C
4. Trial of preferred medication: Zepatier for genotypes 1 and 4 OR Epclusa for genotypes 1,4,5 and 6 in adult
patients
5. If cirrhosis is present: documentation of decompensated or compensated cirrhosis
Drug will be reviewed on a case by case basis utilizing AASLD guidelines and FDA approved package labeling and trial and
failure of Epclusa or Zepatier

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 91
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Hemlibra
Coverage requires the following:
1. For prophylaxis of bleeding episodes in patients diagnosed with congenital hemophilia A with inhibitors
a. Prescribed and dispensed by a specialist that works in a hemophilia treatment center
b. Documentation of a historical or current high titer for factor VIII inhibitors measuring > 5 Bethesda Units per
milliliter (BU/mL)
c. Will not be used in combination with Immune Tolerance Induction (ITI)
d. Medication is dispensed by a treatment center associated with hemophilia that provides high quality
hemophilia care with outcome based results (ie: hemophilia treatment centers)
OR
2. For prophylaxis of spontaneous bleeding episodes in patients diagnosed with congenital hemophilia A without
inhibitors
a. Prescribed and dispensed by a specialist that works in a hemophilia treatment center
b. Documentation of severe hemophilia A with factor VIII level <1% OR moderate hemophilia A with factor VIII
level between 1%-5%
c. Documentation of optimally dosed prophylactic factor VIII product is ineffective for the prevention of
spontaneous bleeding events (such as: continuing to have bleeding events or arthroscopic changes within a
target joint)
d. Documentation of the number of bleeds experienced within the past 12 months
e. Medication is dispensed by a treatment center associated with hemophilia that provides high quality
hemophilia care with outcome based results (ie: hemophilia treatment centers)
Initial approval: 1 year
Continuation of coverage will be provided when treatment has been proven successful through a decrease in the number of
bleeds and absence of anti-drug antibodies that impact the clearance or efficacy of Hemlibra

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 92
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Hetlioz LQ
Coverage requires the following:
1. Age 3 to 15 years old
2. Diagnosis of nighttime sleep disturbances in Smith-Magenis Syndrome (SMS) confirmed by genetic testing
showing deletion of chromosome 17p11.2 OR mutation in the retinoic acid-induced 1 (RAI1) gene
a. Trial and failure, contraindication, or intolerance to over-the-counter melatonin AND acebutolol
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Hizentra
Requires appropriate diagnosis for coverage, subcutaneous administration and other criteria may apply depending on
diagnosis. Dosing must be based on ideal body weight (IBW) unless the patient’s BMI is greater than 30. If the patient’s BMI
is greater than 30 or if actual body weight is 20-30% greater than IBW, adjusted body weight must be used.
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 93
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Horizant
Coverage requires the following:
1. Diagnosis of Restless Leg Syndrome (RLS)
2. Trial and treatment failure of generic Mirapex (pramipexole)
3. Trial and treatment failure of generic Requip/XL (ropinirole)
4. Trial and treatment failure of generic Neurontin (gabapentin)
OR
1. Diagnosis of post-herpetic neuralgia (PHN)
2. ≤ 65 years of age
3. Trial of generic Neurontin (gabapentin)
4. Trial of generic tricyclic antidepressant (ex: amitriptyline, desipramine, imipramine)
OR
1. Diagnosis of post-herpetic neuralgia (PHN)
2. ≥ 65 years of age
3. Trial of generic Neurontin (gabapentin)
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 94
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Humira
Coverage requires the following:
1. Diagnosis of Psoriatic Arthritis
2. Age > 18 years old
OR
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
OR
1. Diagnosis of Juvenile Idiopathic Arthritis (JIA)
2. Age > 2 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, leflunomide)
OR
1. Diagnosis of Ankylosing Spondylitis
2. Age ≥ 18 years old
OR
1. Diagnosis of Psoriasis
2. Age ≥ 18 years old
3. Trial and treatment failure of one topical steroid
OR
1. Diagnosis of Crohn’s Disease
2. Age > 6 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
(criteria continued next page)
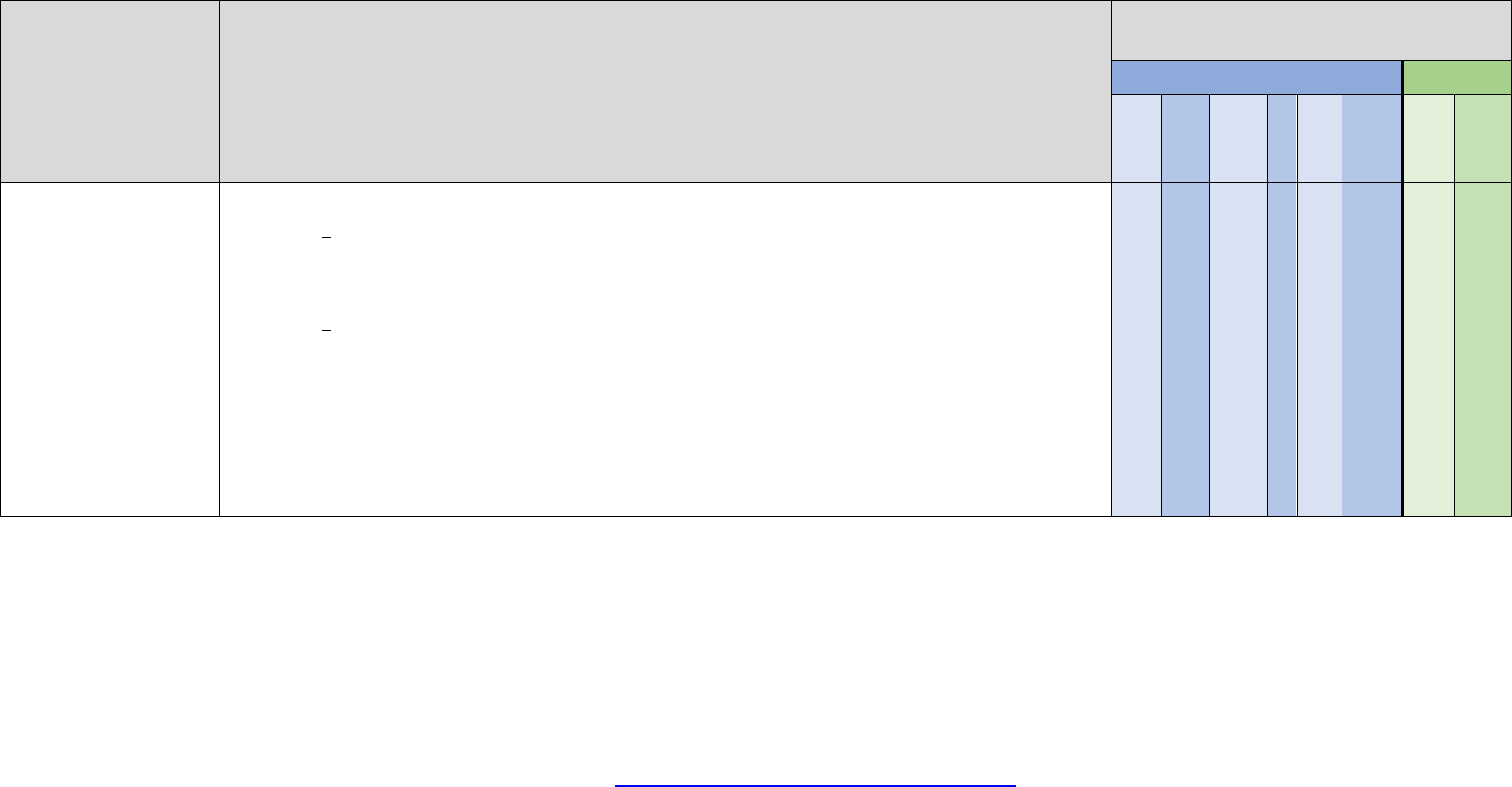
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 95
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Humira
(continued)
OR
1. Diagnosis of Ulcerative Colitis
2. Age > 5 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
OR
1. Diagnosis of Hidradenitis Suppurativa
2. Age > 12 years old
3. Previous 3-month trial of oral antibiotics
OR
1. Diagnosis of Noninfectious Uveitis
2. Age ≥ 2 years old
3. Trial of an oral corticosteroid
4. Trial of an oral immunomodulatory agent (examples include methotrexate, azathioprine, cyclosporine)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 96
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
hydrocodone
bitartrate
(Hysingla
ER)
Coverage requires the following:
1. Diagnosis of moderate to severe chronic pain requiring around the clock opioid analgesia for an extended period of
time
2. Trial and failure or intolerance to three generic long-acting opioids (examples include, but not limited to:
buprenorphine transdermal patch, tramadol, morphine, fentanyl, and methadone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Note: Coverage will not be provided if the patient is on more than one long acting opioid concurrently
NC
NC
hydrocodone
bitartrate
(Zohydro ER)
Coverage requires the following:
1. Diagnosis of moderate to severe chronic pain requiring around the clock opioid analgesia for an extended period of
time
2. Trial and failure or intolerance to three generic long-acting opioids (examples include, but not limited to:
buprenorphine transdermal patch, tramadol, morphine, fentanyl, and methadone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit.
Note: Coverage will not be provided if the patient is on more than one long acting opioid concurrently

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 97
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
hydromorphone
(Exalgo)
Coverage requires the following:
1. Diagnosis of moderate to severe chronic pain requiring around the clock opioid analgesia for an extended period of
time
2. Trial and failure or intolerance to three generic long-acting opioids (examples include, but not limited to:
buprenorphine transdermal patch, tramadol, morphine, fentanyl, and methadone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Note: Coverage will not be provided if the patient is on more than one long acting opioid concurrently.
NC
NC
Hyftor
Coverage requires the following:
1. Diagnosis of facial angiofibroma associated with tuberous sclerosis
2. Age ≥ 6 years old
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
HyQvia
Requires appropriate diagnosis for coverage, subcutaneous administration and other criteria may apply depending on
diagnosis. Dosing must be based on ideal body weight (IBW) unless the patient’s BMI is greater than 30. If the patient’s BMI
is greater than 30 or if actual body weight is 20-30% greater than IBW, adjusted body weight must be used
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 98
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ibrance
Coverage requires the following:
1. Initial therapy for the diagnosis of HR-positive, HER-2 negative advanced or metastic breast cancer
2. Using in combination with an aromatase inhibitor
OR
1. Diagnosis of HR-positive, HER-2 negative advanced or metastatic breast cancer in patients with disease
progression following endocrine therapy
2. Using in combination with fulvestrant
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Ibsrela
Coverage requires the following:
1. Trial and treatment failure or intolerance to lactulose or polyethylene glycol
2. Trial and treatment failure or intolerance to Linzess
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 99
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
icatibant
(Firazyr)
Coverage requires the following:
1. Treatment of acute attacks of hereditary angioedema (HAE)
2. Diagnosis confirmed by genetic testing or with the following laboratory findings:
i. C4 level below the limits of the laboratory’s normal reference range (normal range = 16-58 mg/dL)
ii. C1INH (antigenic or function) below the limits of the laboratory’s normal reference range (normal range ≥ 41%)
3. Prescribed by an immunologist, allergist or hematologist
4. Not to be used in combination with other products indicated for acute HAE attacks
Initial approval: 1 year
Renewal requires objective data documenting at least 50% improvement in time to relief of symptoms of acute attacks
and maintenance of improvement of symptoms

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 100
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Iclusig
Coverage requires the following:
1. Age ≥18 years old
2. Diagnosis of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ALL) for whom no other
tyrosine kinase inhibitor therapy is indicated or who are T315l-positive
OR
1. Age ≥ 18 years old
2. New diagnosis of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ALL)
3. Using in combination with chemotherapy
OR
2. Treatment of chronic phase, accelerated phase, or blast phase chronic myeloid leukemia (CML) for whom no other
tyrosine kinase inhibitor therapy is indicated or who are T315l-positive
OR
2. Treatment of chronic phase (CP) chronic myeloid leukemia (CML) with resistance or intolerance to at least two
prior kinase inhibitors
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Idhifa
Coverage requires the following:
1. Treatment of relapsed or refractory acute myeloid leukemia (AML)
2. Isocitrate dehydrogenase-2 (IDH2) mutation
Initial approval: 1 year.
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 101
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Imbruvica
Coverage requires treatment of FDA approved indications
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 102
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Imcivree
Coverage requires the following:
1. Age ≥ 6 years old
2. Diagnosis of proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin
receptor (LEPR) deficiency confirmed by genetic testing
3. Genetic testing must demonstrate that the variants in POMC, PCSK1, or LEPR genes are interpreted as
pathogenic, likely pathogenic, or of uncertain significance
4. Current weight and BMI (within 30 days) must be submitted to the plan for review
5. Patient has obesity defined as:
a. Adult patients: BMI ≥ 30 kg/m
2
b. Pediatric patients: BMI ≥ 95
th
percentile for children and teens of the same age and sex
OR
1. Age ≥ 6 years old
2. Diagnosis of Bardet-Biedl syndrome (BBS)
3. Current weight and BMI (within 30 days) must be submitted to the plan for review
4. Patient has obesity defined as:
a. Adult patients: BMI ≥ 30 kg/m
2
b. Pediatric patients: BMI ≥ 95
th
percentile for children and teens of the same age and sex
Initial approval for POMC, PCSK1, or LEPR deficiency: 4 months
Initial approval for BBS: 1 year
Continued coverage will be reviewed annually and may be provided if the member has maintained at least a 5% reduction
in baseline body weight OR at least a 5% reduction in baseline BMI for patients with continued growth potential

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 103
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
imiquimod
(Zyclara)
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of actinic keratosis
3. Trial and failure or intolerance to cryotherapy or phototherapy
4. Trial and treatment failure or intolerance to a generic or preferred topical fluorouracil
5. Trial and treatment failure or intolerance to generic imiquimod 5%
OR
1. Age ≥ 12 years old
2. Diagnosis of genital or perianal warts
Initial approval: 60 days
Renewal requires recurrence and or new lesions
NC
NC
Inbrija
Coverage requires the following:
1. Treatment of intermittent OFF episodes in patients with Parkinson’s Disease
2. Currently experiencing “off” episodes while taking carbidopa/levodopa
3. Using in combination with carbidopa/levodopa
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 104
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Increlex
Coverage requires the following:
1. Diagnosis of one of the following:
a. Severe primary IGF-1 deficiency
b. Growth hormone gene deletion
c. Genetic mutation of growth hormone receptor (Laron Syndrome)
2. Current height measurement greater than or equal to 3 standard deviations below normal for age and sex
3. IGF-1 level greater than or equal to 3 standard deviations below normal for age and sex
4. Normal or elevated growth hormone levels based on at least one growth hormone stimulation test
5. Open epiphyses
Initial approval: 1 year
Continued coverage requires documentation of growth velocity of > 2 cm/year and open epiphyses
Ingrezza
Coverage requires the following:
1. Diagnosis of tardive dyskinesia
2. Age ≥ 18 years old
OR
1. Diagnosis of chorea associated with Huntington’s disease
2. Age ≥ 18 years old
3. Trial and failure, contraindication or intolerance to generic Xenazine (tetrabenazine)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 105
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Inlyta
Coverage requires the following:
1. Diagnosis of advanced Renal Cell Carcinoma (RCC)
AND
2. Used in combination with Bavencio (avelumab) as first-line treatment
OR
2. Used in combination with Keytruda (pembrolizumab) as first-line treatment
OR
2. After treatment failure of one prior therapy
Inqovi
Coverage requires the following:
1. Diagnosis of myelodysplastic syndromes
2. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Inrebic
Coverage requires the following:
1. Treatment of patients with intermediate-2 or high-risk primary or secondary myelofibrosis (MF).
2. Age ≥ 18 years old
3. Trial or treatment failure to Jakafi

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 106
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Isturisa
Coverage requires the following:
1. Diagnosis of Cushing’s disease
2. Pituitary surgery is not an option
3. Treatment failure to one of the following ketoconazole, mitotane, or cabergoline
ivermectin 1% cream
(Soolantra)
Coverage requires the following:
1. Trial and failure, contraindication, or intolerance to generic topical metronidazole
2. Trial and failure, contraindication, or intolerance to generic oral tetracycline, generic doxycycline or generic
minocycline
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Iwilfin
Coverage requires the following:
1. To reduce te risk of relapse for the diagnosis of high-risk neuroblastoma (HRNB)
2. Previously demonstrated at least a partial response to prior multiagent, multimodality therapy including anti-GD2
immunotherapy
3. Age ≥ 4 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 107
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Iyuzeh
Coverage requires the following:
1. For the reduction of elevated intraocular pressure (IOP)
2. Age ≥ 18 years old
3. Trial and failure of two preferred or generic benzalkonium chloride-free medications for the treatment of glaucoma
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Jakafi
Coverage requires the following:
1. Diagnosis of intermediate or high risk myelofibrosis
2. Prescribing physician is an oncologist/hematologist
OR
1. Diagnosis of polycythemia vera
2. Trial of hydroxyurea
3. Prescribing physician is an oncologist or hematologist
OR
1. Diagnosis of acute graft-versus-host disease (GVHD)
2. Trial and failure, contraindication, or intolerance to systemic glucocorticoids
3. Age ≥ 12 years old
OR
1. Diagnosis of chronic graft-versus-host disease (cGVHD)
2. Trial and failure, or intolerance to one or two lines of systemic therapy
3. Age ≥ 12 years old
Initial approval: 6 months
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 108
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Jatenzo
Coverage requires the following:
1. Diagnosis of male hypogonadism
2. Two signs and symptoms specific to testosterone deficiency
3. Trial and failure, contraindication or intolerance to one generic or preferred testosterone product (examples include
generic Androgel, Androderm, and generic Depo-Testosterone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Jaypirca
Coverage requires the following:
1. Diagnosis of relapsed or refractory mantle cell lymphoma (MCL)
2. Age ≥ 18 years old
3. Failure of least two lines of systemic therapy, including a Bruton tyrosine kinase (BTK) inhibitor
OR
1. Diagnosis of chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL)
2. Age ≥ 18 years old
3. Failure of at least two prior lines of therapy, including a BTK inhibitor and a BCL-2 inhibitor
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 109
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Joenja
Coverage requires the following:
1. Diagnosis of activated phosphoinositide 3-kinase delta (PI3Kδ) syndrome (APDS) with an associated PI3Kδ
mutation
a. Documented variant in either PIK3CD or PIK3R1
2. Documented symptoms associated with APDS such as:
a. Nodal and/or extranodal lymphoproliferation, history of repeated oto-sino-pulmonary infections and/or organ
dysfunction (e.g. lung, liver)
3. Age ≥ 12 years old
4. Member will not use concurrently with an immunosuppressive medication
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Jornay PM
Coverage requires the following:
1. Diagnosis of attention deficit hyperactivity disorder (ADHD)
2. Age ≥ 6 years old
3. Trial and treatment failure or intolerance to one generic stimulant, such as a generic amphetamine product or a
generic methylphenidate product
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 110
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Juxtapid
Coverage requires the following:
1. Diagnosis of homozygous familial hypercholesterolemia (HoFH)
2. Receiving optimal adjunctive therapies including a low-fat diet and other lipid-lowering treatments
3. Trial and treatment failure of Repatha
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Jynarque
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of autosomal dominant polycystic kidney disease (ADPKD)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Kalydeco
Coverage requires the following:
1. Diagnosis of Cystic Fibrosis (CF)
2. FDA approved gene mutation confirmed by genetic testing
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Karbinal ER
Coverage requires trial and treatment failure to generic carbinoxamine and two other generic antihistamines
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 111
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Kerendia
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of chronic kidney disease associated with type 2 diabetes
3. Being used to reduce the risk of renal function decline, end-stage kidney disease, cardiovascular death, non-fatal
myocardial infarction, and hospitalization for heart failure
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Ketoprofen 25mg
Coverage requires the following:
1. Diagnosis of osteoarthritis
OR
1. Diagnosis of pain
OR
1. Diagnosis of primary dysmenorrhea
OR
1. Diagnosis of rheumatoid arthritis

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 112
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Kevzara
Coverage requires the following:
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure with one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month
trial (examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
4. Trial and treatment failure of two of the following: Enbrel, Humira, Rinvoq, Cimzia, Simponi, or Xeljanz/XR
5. Trial and treatment failure of Actemra and Orencia
OR
1. Diagnosis of polymyalgia rheumatica
2. Age ≥ 18 years old
3. History of treatment with corticosteroids at a dose of > 10 mg per day prednisone equivalent for at least 8 weeks
4. Inadequate response or intolerance to corticosteroids as demonstrated by a disease flare during corticosteroid
taper
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 113
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Kineret
Coverage requires the following:
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
4. Trial and treatment failure of two of the following: Enbrel, Humira, Cimzia, Simponi, Rinvoq, or Xeljanz/XR
5. Trial and treatment failure of Actemra and Orencia
OR
1. Diagnosis of Cryopyrin-Associated Periodic Syndromes (CAPS) with phenotype: Neonatal-onset multisystem
inflammatory disease (NOMID)
2. Laboratory evidence of a genetic mutation OR elevated inflammatory markers plus at least two of six typical CAPS
manifestations: (urticaria-like rash, cold-triggered episodes, hearing loss, musculoskeletal symptoms, chronic
aseptic meningitis, or skeletal abnormalities)
OR
1. Diagnosis of Still’s disease: including adult onset Still’s disease (AOSD) and systemic juvenile idiopathic arthritis
(sJIA)
2. Trial and treatment failure of one of the following therapies: glucocorticoids or NSAIDs
OR
1. Diagnosis of deficiency of interleukin-1 receptor antagonist (DIRA)
2. Laboratory evidence of homozygous genetic mutations of IL1RN
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 114
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Kineret
(continued)
OR
1. Diagnosis of recurrent pericarditis (RP)
2. Age ≥ 12 years old
3. Trial and treatment failure or intolerance to nonsteroidal anti-inflammatory drugs (NSAIDs) in combination with
colchicine
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Kisqali
Coverage requires the diagnosis of HR-positive, HER-2 negative advanced or metastatic breast cancer and ONE of the
following:
a) Using in combination with an aromatase inhibitor as initial endocrine-based therapy
OR
b) Using in combination with fulvestrant as initial endocrine-based therapy in postmenopausal women or in men
OR
c) Using in combination with fulvestrant following disease progression on endocrine therapy in postmenopausal
women or in men
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 115
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Kisqali Femara
Co-
pack
Coverage requires the following:
1. Treatment of FDA approved indications
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Klisyri
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of actinic keratosis (AK) on the face or scalp
3. Trial and treatment failure or intolerance to cryotherapy or phototherapy
4. Trial and treatment failure or intolerance to a generic or preferred topical fluorouracil
5. Trial and treatment failure or intolerance to generic imiquimod 5%
Initial approval: 60 days
Renewal requires lesion recurrence and/or the presence of new lesions

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 116
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Koselugo
Coverage requires the following:
1. Age ≥ 2 years old
2. Diagnosis of Neurofibromatosis Type 1 (NF1)
3. Diagnosis made using either genetic testing or diagnostic criteria established by the National Institutes of Health
(NIH)
OR
3. Receiving treatment by or in consultation with a neurofibromatosis clinic
Initial approval: 6 months
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 117
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Krazati
Coverage requires the following:
1. Diagnosis of KRAS G12C-mutated locally advanced or metastatic non-small cell lung cancer (NSCLC), as
determined by an FDA approved test
2. Age ≥ 18 years old
3. Received at least one prior systemic therapy
OR
1. Diagnosis of KRAS G12-C-mutated locally advanced or metastatic colorectal cancer (CRC), as determined by an
FDA-approved test
2. Age ≥ 18 years old
3. Using in combination with cetuximab
4. Previously treated with fluoropyrimidine-, oxaliplatin-, and irinotecan-based chemotherapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Kyzatrex
Coverage requires the following:
1. Diagnosis of male hypogonadism
2. Two signs and symptoms specific to testosterone deficiency
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 118
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
lapatinib
(Tykerb)
Coverage is provided for the treatment of the FDA approved indications
Lenvima
Coverage requires the following:
1. Diagnosis of locally recurrent or metastatic, progressive differentiated thyroid cancer (DTC)
a. Progression of disease after treatment with standard therapy
OR
1. Diagnosis of advanced renal cell carcinoma
a. Using as first-line treatment in combination with pembrolizumab
OR
b. Treatment failure to one prior anti-angiogenic therapy AND using in combination with everolimus
OR
1. Diagnosis of unresectable hepatocellular carcinoma
OR
1. Diagnosis of advanced endometrial carcinoma
a. Progression of disease after prior systemic therapy
b. Not a candidate for curative surgery or radiation
c. Using in combination with pembrolizumab
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 119
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Levorphanol
Coverage requires the following:
1. When used for as needed pain: Treatment failure or intolerance to three generic immediate release opioids
(examples include, but not limited to: tramadol, morphine, hydrocodone, and oxycodone containing products)
OR
1. When used for chronic pain requiring around-the-clock analgesia: Treatment failure or intolerance to three generic
long-acting opioids. Examples include but are not limited to: buprenorphine transdermal patch, tramadol extended
release, morphine extended release, fentanyl, methadone.
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Note: Coverage will not be provided if the patient is on more than one long acting opioid concurrently

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 120
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Litfulo
Coverage requires the following:
1. Diagnosis of severe Alopecia Areata (AA), defined as ≥ 50% scalp hair loss OR 21-49% scalp hair loss with at least
one of the following:
a. Significant impact on psychosocial functioning resulting from AA
b. Eyebrow or eyelash involvement
c. Inadequate response to previous treatment after at least 6 months
d. Diffuse (multifocal) positive hair pull test consistent with rapidly progressive AA
2. Age ≥ 12 years old
3. Cannot be used in combination with other biologic agents or targeted DMARDs indicated for AA
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 121
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Livmarli
Coverage requires the following:
1. Treatment of cholestatic pruritus in patients with a diagnosis Alagille syndrome (ALGS) confirmed by
documentation of ONE of the following:
a. Genetic testing shows presence of the JAG1 or NOTCH2 genetic mutation
b. Liver biopsy shows bile duct scarcity
c. Involvement of 3 of 7 of the main organ systems affected in ALGS: hepatic, ocular, skeletal, vascular,
facial, cardiac, or renal involvement
2. Age ≥ 3 months old
3. No history of liver transplant or planned future transplant
4. No clinical evidence of decompensated cirrhosis
5. Trial and failure, contraindication, or intolerance to generic ursodiol\
OR
1. Treatment of cholestatic pruritis in patients with progressive familial intrahepatic cholestasis (PFIC)
i. Genetic testing does NOT show the presence of the ABCB11 variants resulting in a nonfunctional or
complete absence of the bile salt export pump protein (BSEP-3)
2. Age ≥ 5 years old
3. No history of liver transplant or planned future transplant
4. No clinical evidence of decompensated cirrhosis
5. Trial and failure, contraindication, or intolerance to generic ursodiol
Initial approval: 6 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 122
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Livtencity
Coverage requires the following:
1. Diagnosis of post-transplant cytomegalovirus (CMV) infection/disease
2. Age ≥ 12 years old and weight ≥ 35 kg
3. Trial and treatment failure of one of the following: ganciclovir, valganciclovir, cidofovir or foscarnet
Initial approval: 3 months
Lonsurf
Coverage requires the following:
1. Diagnosis of metastatic colorectal cancer
2. Previous treatment with
a. fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy
b. anti-VEGF biological therapy
3. Test results showing RAS wild type have received treatment with an anti-EGFR therapy
4. Using alone or in combination with bevacizumab
OR
1. Diagnosis of metastatic gastric or gastroesophageal junction adenocarcinoma
2. Previous treatment with at least 2 lines of chemotherapy prior systemic therapies which included a fluoropyrimidine,
a platinum, either a taxane or irinotecan, and a HER2/neu-targeted therapy (if appropriate)
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 123
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Lorbrena
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of metastatic non-small cell lung cancer (NSCLC) whose tumors are anaplastic lymphoma kinase (ALK)-
positive as detected by an FDA-approved test
luliconazole
Coverage requires the following:
1. Diagnosis of tinea pedis, tinea cruris or tinea corporis
2. Treatment failure of 2 topical over-the-counter antifungal agents
3. Treatment failure of two oral generic antifungal agents (fluconazole, itraconazole or terbinafine)
NC
NC
Lumakras
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of KRAS G12C-mutated locally advanced or metastatic non-small cell lung cancer (NSCLC), as
determinedby an FDA-approved test
3. Received at least one prior systemic therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 124
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Lumryz
Coverage requires the following:
1. Diagnosis of narcolepsy and cataplexy
2. Age ≥ 18 years old
3. Trial and failure, contraindication, or intolerance to Wakix
OR
1. Diagnosis of narcolepsy and excessive daytime sleepiness
2. Age ≥ 18 years old
3. Trial and failure, contraindication, or intolerance to at least one generic or preferred treatment such as
methylphenidate or dextroamphetamine
4. Trial and failure, contraindication, or intolerance to modafinil or armodafinil, AND Sunosi, AND Wakix
Lumryz will not be approved if patient is being treated with sedative hypnotic agents, other central nervous system (CNS)
depressants or using alcohol
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 125
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Lupkynis
Coverage requires the following:
1. Age ≥ 18 years old
2. Treatment of active lupus nephritis (LN) in combination with a background immunosuppressive therapy regimen
3. Must have active disease of the kidney confirmed on biopsy
4. Previous treatment courses of the following have been ineffective unless contraindicated or not tolerated:
cyclophosphamide plus glucocorticoids OR mycophenolate mofetil plus glucocorticoids
5. Trial and failure, contraindication, or intolerance to Benlysta
Initial approval: 6 months
Initial renewal requires that the member is experiencing clinical benefit (for example, a stabilization or improvement in
glomerular filtration rate (GFR) or at least a 50% reduction in proteinuria)
Renewal approval: 1 year
Subsequent renewal requires that the member has not yet reached complete clinical response defined as proteinuria less
than 0.5–0.7 g/24 hours
Lynparza
Coverage requires the treatment of FDA approved indications
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 126
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Lybalvi
Coverage requires the following:
Trial and failure, contraindication, or intolerance to two preferred second generation antipsychotics (examples include:
aripiprazole, clozapine, risperidone, quetiapine, olanzapine, ziprasidone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Lytgobi
Coverage requires the following:
1. Diagnosis of previously treated, unresectable, locally advanced or metastatic intrahepatic cholangiocarcinoma
harboring fibroblast growth factor receptor 2 (FGFR2) gene fusions or other rearrangements
2. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Lyvispah
Coverage requires the following:
1. Diagnosis of spasticity
2. Trial of baclofen tablets
OR
2. Member is unable to swallow tablets
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 127
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Mavenclad
Coverage requires trial and failure or intolerance to one generic or preferred medication for the treatment of multiple
sclerosis (MS) such as Avonex, Bafiertam, Betaseron, Copaxone, Kesimpta, or Vumerity
Initial approval: 2 years
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Mavyret
Coverage requires the following:
1. Age ≥ 3 years old
2. Diagnosis of chronic hepatitis C genotype 1, 2, 3, 4, 5, or 6
3. If treatment experienced, documentation of previous treatment experience for Hepatitis C
4. Trial of the preferred medication: Epclusa or Zepatier
5. Patients with HCV genotype 1 who have previously been treated with regimens containing an NS5A (nonstructural
protein 5A) inhibitor or an NS3/4A protease inhibitor, but not both
6. If cirrhosis is present: documentation of decompensated or compensated cirrhosis
Drug will be reviewed on a case by case basis utilizing AASLD guidelines and FDA approved package labeling and trial and
failure to Epclusa or Zepatier

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 128
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Mekinist
Coverage requires the following:
1. Diagnosis of melanoma
2. Presence of BRAF V600E or V600K mutation
3. Using as a single agent or in combination with Tafinlar (dabrafenib)
OR
1. Diagnosis of metastatic non-small cell lung cancer or advanced or metastatic anaplastic thyroid cancer
2. Presence of BRAF V600 E mutation
3. Using in combination with Tafinlar (dabrafenib)
OR
1. Age ≥ 1 year old
2. Diagnosis of unresectable or metastatic solid tumors who have progressed following prior treatment and have no
satisfactory alternative treatment options
3. Presence of with BRAF V600E mutation
4. Using in combination with Tafinlar (dabrafenib)
OR
1. Age ≥ 1 year old
2. Diagnosis of low-grade glioma (LGG) with a BRAF V600E mutation requiring systemic therapy
3. Using in combination with Tafinlar
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 129
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Mektovi
Coverage requires the following:
1. Diagnosis of unresectable or metastatic melanoma with a BRAF V600E or V600K mutation as detected by an FDA-
approved test
2. Using in combination with Braftovi
OR
1. Diagnosis of metastatic non-small cell lung cancer (NSCLC) with a BRAF V600E mutation as detected by an FDA
approved test
2. Using in comination with Braftovi
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
meloxicam capsule
(Vivlodex)
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of osteoarthritis
3. Trial and failure of generic Mobic (meloxicam tablet)
4. Trial and failure of two other preferred oral NSAIDs
Initial approval: 1 year
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 130
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
metformin hcl
extended release
(Fortamet)
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of type 2 diabetes mellitus
3. Trial and treatment failure or intolerance to generic Glucophage XR (metformin extended release)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 131
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
methylergonovine
(Methergine)
Coverage requires the following:
1. Management of uterine atony, hemorrhage, and subinvolution of the uterus following delivery of the placenta or
control of uterine hemorrhage following delivery of the anterior shoulder in the second stage of labor
OR
1. Being used for the prevention of migraine headaches
2. Member has persistent history of recurring debilitating headaches (4 or more headache days per month with
migraine headache lasting for 4 hours per day or longer)
3. Trial and treatment failure after a minimum of 2 month trial, contraindication, or intolerance to three of the following:
a. Anticonvulsants
b. ACE inhibitors or angiotensin receptor blockers
c. Beta blockers
d. Calcium channel blockers
e. Antidepressants
f. Botulinum toxin
4. Trial and treatment failure after a minimum 2 month trial, contraindication, or intolerance to at least one calcitonin
gene related peptide (CGRP) antagonist (such as: Aimovig, Ajovy, Emgality, or Vyepti)
OR
1. Being used for the treatment of episodic or chronic cluster headache
2. Trial and failure, contraindication, or intolerance to at least three of the following: suboccipital steroid injection,
verapamil, lithium, melatonin, frovatriptan, prednisone, or topiramate
3. Trial and failure, contraindication, or intolerance to Emgality
Initial approval: 6 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
For headache indications, member must have at least a 1 month drug holiday after 3-6 months of therapy has occurred
prior to restarting methylergonovine

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 132
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
mifepristone
(Korlym)
Coverage requires the following:
1. Member is ≥ 18 years of age
2. Diagnosis of hypercortisolism as a result of endogenous Cushing’s Syndrome
3. Diagnosis of type II diabetes mellitus (DM) or glucose intolerance secondary to hypercortisolism.
4. Surgical treatment has been ineffective or not a candidate for surgery
5. Treatment failure or intolerance to a steroidogenesis inhibitor (such as ketoconazole, mitotane, or cabergoline),
unless contraindicated
6. Failure to achieve adequate blood glucose control with maximally titrated therapy with an antidiabetic agent given
for at least 3 months and which does not include metformin
7. Documentation of baseline 2 – hour glucose tolerance test if diagnosis is glucose intolerance.
8. HbA1c is required if diagnosis is type II DM
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 133
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
miglustat
(Zavesca, Yargesa)
Coverage requires the following:
1. Age ≥ 18 years old
2. For the treatment of mild to moderate Gaucher disease type 1 (GD1)
3. Confirmation of diagnosis by biochemical assay showing decreased glucocerebrosidase activity in white blood cells
or skin fibroblasts AND genotyping revealing two pathogenic mutations of the glucocerebrosidase gene
4. Two symptomatic manifestations of the disease are present, such as anemia, thrombocytopenia, bone disease,
hepatomegaly, or splenomegaly
5. Trial and failure, contraindication, or intolerance to enzyme replacement therapy (ERT)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
mirabegron ER
tablets
(Myrbetriq)
Coverage requires the following:
1. Diagnosis of overactive bladder (OAB)
2. Age ≥ 18 years old
3. Trial and treatment failure or intolerance to two preferred therapies for OAB
OR
1. Diagnosis of neurogenic detrusor overactivity (NDO)
2. Weight ≥ 35 kg
3. Trial and treatment failure or intolerance to two generic anticholinergic agents for the treatment of NDO
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 134
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Mounjaro
Coverage requires the following:
1. For the treatment of Type 2 Diabetes or trial of one generic or preferred medication for the treatment of Type 2
Diabetes
2. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist-containing products
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Motegrity
Coverage requires the following:
1. Trial and treatment failure or intolerance to lactulose or polyethylene glycol
2. Trial and treatment failure or intolerance to Linzess
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Motpoly XR
Coverage requires the following:
1. Treatment of seizure disorder/epilepsy
2. Weight ≥ 50 kg
3. Trial and failure, contraindication, OR intolerance to TWO generic alternatives for the treatment of seizures
4. Trial and failure, contraindication, OR intolerance to generic Vimpat tablet or solution
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 135
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Muse
May be covered for the diagnosis of erectile dysfunction dependent on the plan’s benefit with quantity limit restrictions
NC
NC
Myalept
Coverage requires the following:
1. Replacement therapy to treat the complications of leptin deficiency, in addition to diet, in patients with congenital or
acquired generalized lipodystrophy.
2. Optimally treated with insulin
3. Optimally treated with a statin (examples include atorvastatin, simvastatin)
Mycapssa
Coverage requires the following:
1. Diagnosis of acromegaly
2. Previously tried, responded to, and tolerated generic immediate-release octreotide or lanreotide
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 136
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Myfembree
Coverage requires the following:
1. Management of heavy menstrual bleeding associated with uterine leiomyomas (fibroids) in premenopausal women
2. Age ≥ 18 years old
3. Trial of two hormone related therapies
OR
1. Treatment of pain associated with endometriosis in premenopausal women
2. Age ≥ 18 years old
3. Trial of two hormone related therapies
Myfembree will be approved for a maximum of two years
Myrbetriq granules
Coverage requires the following:
1. Diagnosis of neurogenic detrusor overactivity (NDO)
2. Age ≥ 3 years old
3. Trial and treatment failure or intolerance to two generic anticholinergic agents for the treatment of NDO
OR
3. Member cannot swallow tablets/capsules AND has tried and failed an anticholinergic medication available as a
solution
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Mytesi
Coverage is provided for the symptomatic relief of noninfectious diarrhea in patients with HIV/AIDS and on antiretroviral
therapy

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 137
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Naftifine gel
(Naftin)
Coverage requires the following:
1. Diagnosis of tinea pedis, tinea cruris or tinea corporis
2. Treatment failure to two topical over-the-counter antifungal agents
3. Treatment failure to two oral generic antifungal agents
Namzaric
Coverage requires the following:
Already stable on memantine (Namenda) and donepezil (Aricept)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Natesto
Coverage requires the following:
1. Diagnosis of male hypogonadism
2. Two signs and symptoms specific to testosterone deficiency
3. Trial and failure, contraindication or intolerance to one generic or preferred testosterone product (examples include
generic Androgel, Androderm, and generic Depo-Testosterone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Natpara
Coverage requires the following:
1. Using as an adjunct to calcium and Vitamin D to control hypocalcemia in patients with hypoparathyroidism
2. Currently on calcium and Vitamin D and hypocalcemia is not well controlled

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 138
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nerlynx
Coverage requires the following:
1. Diagnosis of early stage HER2 positive breast cancer
2. Previous treatment with trastuzumab (Herceptin)-based therapy
OR
1. Diagnosis of advanced or metastatic HER2 positive breast cancer
2. Previous treatment with two or more anti-HER2 based regimens
3. Using in combination with capecitabine
Neupro
Coverage requires the following:
1. Diagnosis of Parkinson’s disease
2. Treatment failure or intolerance to generic Mirapex (pramipexole) and generic Requip (ropinirole)
OR
1. Diagnosis of Restless legs syndrome
2. Treatment failure or intolerance to generic Mirapex (pramipexole), generic Requip (ropinirole) and generic
Neurontin (gabapentin)
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 139
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nexletol
Coverage requires the following:
1. Diagnosis of established cardiovascular disease (CVD), high risk for a CVD event but without established CVD,
primary hyperlipidemia, or heterozygous familial hypercholesterolemia (HeFH)
2. Age ≥ 18 years old
AND
3. Trial with one high intensity statin at maximum tolerated dose
OR
3. History of statin intolerance (skeletal muscle related symptoms) after a trial of two generic statins (examples
include: Crestor, Lescol, Lipitor, Livalo, Mevacor, Pravachol, Zocor)
OR
3. History of rhabdomyolysis after a trial of one statin (Examples include: Crestor, Lescol, Lipitor, Livalo, Mevacor,
Pravachol, Zocor)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 140
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nexlizet
Coverage requires the following:
1. Diagnosis of established cardiovascular disease (CVD), high risk for a CVD event but without established CVD,
primary hyperlipidemia, or heterozygous familial hypercholesterolemia (HeFH)
2. Age ≥ 18 years old
AND
3. Trial with one high intensity statin at maximum tolerated dose
OR
3. History of statin intolerance (skeletal muscle related symptoms) after a trial of two generic statins (examples
include: Crestor, Lescol, Lipitor, Livalo, Mevacor, Pravachol, Zocor)
OR
3. History of rhabdomyolysis after a trial of one statin (examples include: Crestor, Lescol, Lipitor, Livalo, Mevacor,
Pravachol, Zocor)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Nicotrol,
Nicotrol NS
Coverage for $0 copayment will require trial and failure of 2 preferred agents such as generic bupropion extended release
(Zyban), nicotine patch, nicotrine gum, nicotine lozenge
nilutamide
(Nilandron)
Coverage requires the following:
1. Treatment of metastatic prostate cancer in combination with surgical castration
2. Trial and failure, contraindication, or intolerance to generic Casodex (bicalutamide)
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 141
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ninlaro
Coverage requires the following:
1. Diagnosis of multiple myeloma
2. Using in combination with lenalidomide and dexamethasone
3. Have received at least one prior therapy
nitisinone
(Orfadin)
Coverage requires the following:
1. Diagnosis of hereditary tyrosinemia type 1
2. Using along with dietary restriction of tyrosine and phenylalanine
Nityr
Coverage requires the following:
1. Diagnosis of hereditary tyrosinemia type 1
2. Using along with dietary restriction of tyrosine and phenylalanine
Nocdurna
Coverage requires the following:
1. Diagnosis of nocturnal polyuria
2. Lifestyle changes have been tried (including limiting fluids, elevation of legs)
3. Treatment failure or intolerance to one generic medication for overactive bladder (OAB)
4. Trial of generic oral desmopressin
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 142
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Noctiva
Coverage requires the following:
1. Diagnosis of nocturnal polyuria
2. Age ≥ 50 years old
3. Lifestyle changes have been tried (including limiting fluids such as water, alcohol and caffeine, elevation of legs)
4. Treatment failure or intolerance to one generic medication for over active bladder (OAB) (examples tolterodine,
oxybutynin)
5. Trial of generic oral desmopressin
NC
NC
Nourianz
Coverage requires the following:
1. Treatment of intermittent OFF episodes in patients with Parkinson’s Disease
2. Currently experiencing “off” episodes while taking carbidopa/levodopa
3. Using in combination with carbidopa/levodopa
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 143
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nubeqa
Coverage requires the following:
1. Treatment of nonmetastatic castration-resistant prostate cancer
OR
1. Treatment of metastatic hormone sensitive prostate cancer
2. Using in combination with docetaxel
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 144
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nucala
Coverage requires the following:
1. Diagnosis of severe uncontrolled eosinophilic asthma
2. Age ≥ 6 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. Severe eosinophilic asthma identified by:
a. Blood eosinophils greater than or equal to 150 cells/microliter at initiation of treatment
AND
b. Failure to maintain adequate control after at least a 3 month trial of daily oral corticosteroids or high dose
inhaled corticosteroids in combination with:
i. LABA (long acting inhaled β2 agonist)
OR
ii. or leukotriene modifier
OR
iii. LAMA (long acting muscarininc antagonist) in adults and children ≥ 12 years old
5. Cannot be used in combination with other biologic agents indicated for uncontrolled eosinophilic asthma
OR
1. Diagnosis of eosinophilic granulomatosis with polyangiitis (EGPA)
2. Age ≥18 years old
3. Consult with an allergist/immunologist prior to initiation of Nucala therapy
4. History or presence of asthma
5. Presence of at least 2 of the following criteria that are typical of EGPA: histopathological evidence of eosinophilic
vasculitis, perivascular eosinophilic infiltration, or eosinophil-rich granulomatous inflammation, neuropathy,
pulmonary infiltrates, allergic rhinitis and nasal polyps, cardiomyopathy, glomerulonephritis, alveolar hemorrhage,
palpable purpura, or antineutrophil cytoplasmic antibody (ANCA) positivity
6. Cannot be used in combination with other biologic agents indicated for EGPA
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 145
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nucala
(continued)
OR
1. Diagnosis of hypereosinophilic syndrome (HES)
2. Age ≥ 12 years old
3. At least 2 HES flares within the past 12 months (defined as HES-related worsening of clinical symptoms or blood
eosinophil counts requiring an escalation in therapy
4. Stable on HES therapy for at least 4 weeks (examples include: oral corticosteroids, immunosuppressive or
cytotoxic therapy)
5. Eosinophil counts of 1,000 cells/microL or higher at initiation of therapy
6. Member does not have eosinophilia of unknown clinical significance, non-hematologic secondary HES (drug
hypersensitivity, parasitic helminth infection, HIV infection, non-hematologic malignancy), or F1P1L1-PDGFRa
kinase-positive HES
7. Cannot be used in combination with other biologic agents indicated for HES
OR
1. Diagnosis of chronic rhinosinusitis with nasal polyposis (CRSwNP)
2. Age > 18 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. CRSwNP is recurring despite previous treatment with intranasal corticosteroids
5. Cannot be used in combination with other biologic agents indicated for CRSwNP
Approval length: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 146
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nucynta
Coverage requires the following:
1. Diagnosis of acute pain
2. Age ≥ 6 years old and weight ≥ 16kg
3. Treatment failure or intolerance to three generic immediate release opioids (examples include, but not limited to:
tramadol, morphine, hydrocodone, and oxycodone containing products)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 147
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nucynta ER
Coverage requires the following:
1. Diagnosis of moderate to severe chronic pain requiring around the clock opioid analgesia for an extended period of
time
2. Trial and failure or intolerance to three generic long-acting opioids (examples include, but not limited to:
buprenorphine transdermal patch, tramadol, morphine, fentanyl, and methadone)
3. Trial and failure or intolerance to Xtampza ER
OR
1. Diagnosis of Diabetic Peripheral Neuropathy (DPN)
AND
2. If the member is equal to or greater than 65 years of age: Trial and failure of generic gabapentin (Neurontin) AND
generic duloxetine (Cymbalta)
OR
3. If the member is less than 65 years of age: Trial and failure of generic gabapentin (Neurontin) and generic
duloxetine (Cymbalta) and a tricyclic antidepressant such as amitriptyline, desipramine, nortriptyline or imipramine
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Note: Coverage will not be provided if the patient is on more than one long acting opioid concurrently
Nuedexta
Coverage requires the following:
1. Diagnosis of pseudobulbar affect (PBA)
2. Presence of an underlying neurological condition causing symptoms of PBA (ex. Multiple Sclerosis, amyotrophic
lateral sclerosis, Parkinson’s Disease, stroke, traumatic brain injury)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 148
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Nuplazid
Coverage requires the following:
1. Diagnosis of Parkinson’s disease psychosis
Initial approval: 1 year
Renewal requires clinically significant improvement in psychosis symptoms
Nurtec ODT
Coverage requires the following:
1. For acute treatment of migraine
2. Age ≥ 18 years old
3. Treatment failure or contraindication with 2 generic triptan medications
OR
1. For preventive treatment of migraine headaches
2. Age ≥ 18 years old
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Nyvepria
Coverage requires trial and failure or intolerance to Neulasta and Ziextenzo

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 149
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ocaliva
Coverage requires the following:
1. Diagnosis of primary biliary cholangtis (PBC) confirmed by 2 of the 3 following American Association for the Study
of Liver Diseases criteria: a positive test for antimitochondrial antibodies, elevated serum levels of alkaline
phosphatase (ALP), histologic evidence of PBC based on liver biopsy
2. If cirrhosis is present: documentation of no evidence of portal hypertension
3. Inadequate response to ursodeoxycholic acid (UDCA) such as Actigall (ursodiol) after at least one year at a dose
of 13-15mg/kg/day or inability to tolerate UDCA
4. Treatment plan must include UDCA unless unable to tolerate it
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Odactra
Coverage requires the following:
1. 12 to 65 years of age
2. Diagnosis of house dust mite (HDM)-induced allergic rhinitis confirmed by a positive skin test or in vitro testing for
IgE antibodies to house dust mites
3. Trial of one agent from each of the following classes:
a. Intranasal corticosteroid
b. Oral or intranasal antihistamine
Initial approval: 3 years
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 150
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Odomzo
Coverage requires the following:
1. Diagnosis of locally advanced basal cell carcinoma
2. Carcinoma occurred again following surgery or radiation therapy OR member is not able to receive treatment with
surgery or radiation therapy
Ofev
Coverage requires the following:
1. Treatment of idiopathic pulmonary fibrosis (IPF)
OR
1. Treatment of declining pulmonary function in patients with systemic sclerosis-associated interstitial lung disease
OR
1. Treatment of chronic fibrosing interstitial lung diseases (ILDs) with a progressive phenotype
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Ogsiveo
Coverage requires the following:
1. Diagnosis of progressing desmoid tumors requiring systemic treatment
2. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 151
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ojemda
Coverage requires the following:
1. Diagnosis or relapsed or refractory low-grade glioma (LGG) harboring a BRAF fusion or rearrangement, or BRAF
V600 mutation
2. Age ≥ 6 months old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Ojjaara
Coverage requires the following:
1. Age ≥ 18 years old
2. For the treatment of intermediate or high-risk myelofibrosis (MF), including primary MF or secondary MF [post-
polycythemia vera (PV) and post-essential thrombocythemia (ET)], with anemia
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Olpruva
Coverage requires the following:
1. Diagnosis of urea cycle disorder
2. Will be used as adjunctive therapy to dietary management (such as dietary protein restriction and/or amino acid
supplementation)
3. Trial and treatment failure of Buphenyl® (sodium phenylbutyrate)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 152
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Olumiant
Coverage requires the following:
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
4. Trial and treatment failure of two of the following: Enbrel, Humira, Cimzia, Simponi, Rinvoq, or Xeljanz/XR
5. Trial and treatment failure of Actemra and Orencia
OR
1. Diagnosis of severe Alopecia Areata (AA), defined as ≥ 50% scalp hair loss OR 21-49% scalp hair loss with at least
one of the following:
i. Significant impact on psychosocial functioning resulting from AA
ii. Eyebrow or eyelash involvement
iii. Inadequate response to previous treatment after at least 6 months
iv. Diffuse (multifocal) positive hair pull test consistent with rapidly progressive AA
2. Age ≥ 18 years old
3. Cannot be used in combination with other biologic agents or targeted DMARDs indicated for AA
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 153
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Omnaris
Coverage requires trial and failure or intolerance of 2 of the following intranasal steroids:
1. Generic fluticasone (Flonase)
2. Generic flunisolide (Nasalide)
3. Nasacort (over-the-counter)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
NC
Ongentys
Coverage requires the following:
1. Age ≥ 18 years old
2. For treatment of patients with Parkinson’s disease (PD) experiencing “OFF” episodes
3. Taking with carbidopa/levodopa
4. Trial and failure or contraindication to generic COMT-inhibitor such as generic Comtan (entacapone) or generic
Tasmar (tolcapone)
Onureg
Coverage requires the following:
Maintenance treatment of acute myeloid leukemia (AML) in adults who achieved first complete remission (CR) or complete
remission with incomplete blood count recovery (Cri) following intensive induction chemotherapy and are not able to
complete intensive curative therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 154
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Onzetra Xsail
Coverage requires the following:
1. Treatment failure or intolerance to generic Imitrex (sumatriptan) nasal spray and one other generic triptan
(examples include: generic Maxalt (rizatriptan), generic Amerge (naratriptan), generic Zomig/ZMT(zolmitriptan))
OR
1. Age 12-17 years old
2. Treatment failure or intolerance to generic Maxalt (rizatriptan)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Opsumit
Coverage is provided for the treatment of pulmonary arterial hypertension (WHO Group 1)
Opsynvi
Coverage requires the following:
1. Diagnosis of pulmonary arterial hypertension (PAH, WHO Group I)
2. WHO functional class (FC) II-III
3. Age ≥ 18 years old
4. Trial and failure, intolerance, or contraindication to ALL of the following:
i. Generic sildenafil or tadalafil
ii. Generic ambrisentan AND bosentan
OR
4. Member is currently stable on individual components of Opsynvi being used in combination
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
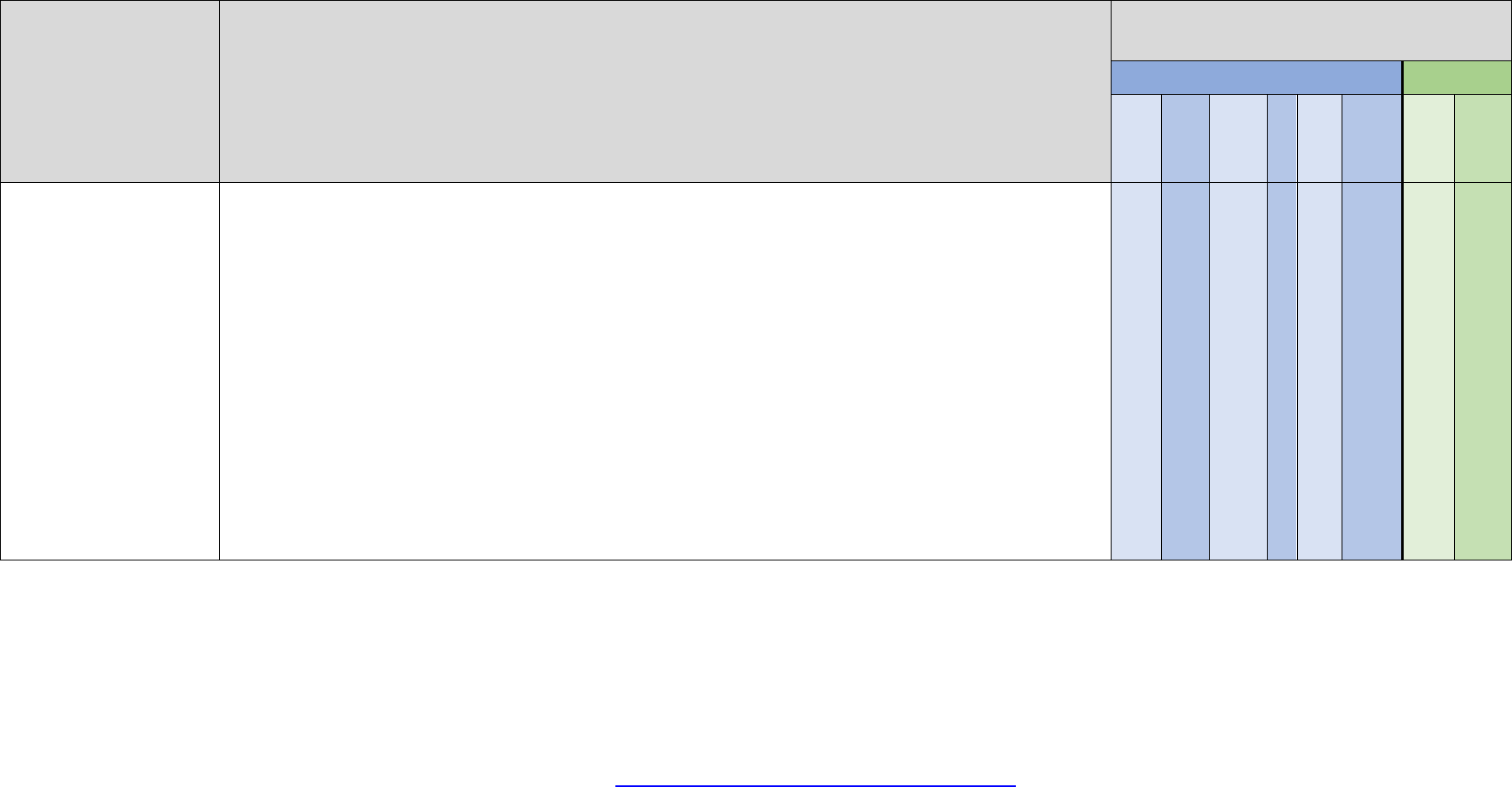
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 155
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Opzelura
Coverage requires the following:
1. Diagnosis of atopic dermatitis (AD)
2. Age ≥ 12 years old
3. Trial and treatment failure with one topical steroid
4. Trial and treatment failure with generic Protopic (tacrolimus) or generic Elidel (pimecrolimus)
5. Trial and treatment failure with Eucrisa
6. Cannot be used in combination with therapeutic biologics, other JAK inhibitors or potent immunosuppressants such
as azathioprine or cyclosporine
OR
1. Diagnosis vitiligo
2. Age ≥ 12 years old
3. Trial and treatment failure of one topical steroid
4. Trial and treatment failure with generic Protopic (tacrolimus) or generic Elidel (pimecrolimus)
5. Not to be used in combination with therapeutic biologics, other JAK inhibitors, or potent immunosuppressants such
as azathioprine or cyclosporine
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 156
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Oralair
Coverage requires the following:
1. Age 5 through 65 years old
2. Diagnosis of grass pollen-induced allergic rhinitis, confirmed by positive skin test or in vitro testing for pollen-
specific IgE antibodies for any of the 5 grass species contained in this product
3. Trial of one agent from each of the following classes:
a. Intranasal corticosteroid
b. Oral or intranasal antihistamine
Initial approval: 3 years
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Oracea, doxycycline
IR DR
Coverage requires the following:
Trial and treatment failure or intolerance to generic doxycycline monohydrate (Monodox) AND generic doxycycline hyclate
immediate release (Vibramycin)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 157
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Orencia SC
Coverage requires the following:
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
4. Trial and treatment failure of two of the following: Enbrel, Humira, Cimzia, Simponi, Rinvoq, or Xeljanz/XR
OR
1. Diagnosis of Juvenile Idiopathic Arthritis (JIA)
2. Age ≥ 2 years old
3. Trial and treatment failure of one DMARD after a minimum 3-month trial (examples include methotrexate,
leflunomide)
4. Trial and treatment failure of two of the following: Enbrel, Humira, or Xeljanz
OR
1. Diagnosis of Psoriatic Arthritis
2. Age 2 to 5 years old
3. Trial and treatment failure of Enbrel
OR
2. Age 6 to 17 years old
3. Trial and treatment failure of Enbrel or Stelara
OR
2. Age ≥ 18 years old
3. Trial and treatment failure of two of the following: Enbrel, Humira, Cimzia, Simponi, Stelara, Rinvoq, Skyrizi,
Tremfya, or Xeljanz/XR
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 158
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Orenitram
Coverage requires the following:
1. Diagnosis of pulmonary arterial hypertension (WHO Group 1)
2. Trial and treatment failure of sildenafil or tadalafil AND ambrisentan or bosentan
Orgovyx
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of advanced prostate cancer
3. Trial and failure, contraindication, OR intolerance to Firmagon (covered under medical benefit)
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Oriahnn
Coverage requires the following:
1. Management of heavy menstrual bleeding associated with uterine leiomyomas (fibroids) in premenopausal women
2. Age ≥18 years old
3. Trial of two hormone related therapies
4. Trial of Myfembree
Oriahnn will be approved for a maximum of two years

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 159
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Orilissa
Coverage requires the following:
1. Treatment of pain associated with endometriosis
2. Trial of two hormone related therapies
3. Age ≥ 18 years old.
150mg: Approval length 2 years
200mg: Approval length 6 months
Orkambi
Coverage requires the following:
1. Age ≥ 1 year old
2. Diagnosis of cystic fibrosis (CF)
3. Presence of two copies of the F508del mutation confirmed by genetic test
Initial approval: 6 months
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 160
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Orladeyo
Coverage requires the following:
1. Age ≥ 12 years old
2. Diagnosis of hereditary angioedema (HAE)
3. Diagnosis confirmed by genetic testing or with the following laboratory findings:
i. C4 level below the limits of the laboratory’s normal reference range (normal range = 16-58 mg/dL)
ii. C1INH (antigenic or function) below the limits of the laboratory’s normal referencerange (normal range ≥
41%)
4. History of at least 2 HAE attacks per month OR a history of attacks that are considered severe with swelling of the
face, throat or gastrointestinal tract
5. Prescribed by an immunologist, allergist or hematologist
6. Trial and failure, contraindication, OR intolerance to Haegarda AND Takhzyro (if appropriate per age)
7. Not to be used in combination with other products indicated for HAE prophylaxis
Initial approval: 1 year
Renewal requires improvement in HAE demonstrated by a 50% reduction in the number of attacks OR the severity of HAE
attacks was reduced by 50% or more

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 161
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
orlistat
(Xenical)
Coverage requires the following:
1. Age ≥ 18 years old
2. BMI ≥ 30 kg/m2 or ≥ 27 kg/m2 with one related comorbid condition
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active
participation for a minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food
diaries, exercise logs, program receipts, app participation, etc.) if member does not have access to a covered
BCBSM/BCN program
5. Not to be used in combination with other weight loss products
Initial approval: 6 months
Continued coverage will be reviewed annually and may be provided if the member has maintained at least a 5% weight loss
from baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30 days) and
BMI ≥ 18.5 kg/m2 must be submitted to the plan for review
NC
NC
orphenadrine/aspirin
/caffeine
(Norgesic)
Coverage requires the following:
1. Treatment of acute pain
2. Age ≥ 12 years old
3. Trial and failure or intolerance to at least 3 preferred generic skeletal muscle relaxants, one of which must be
generic Norflex (orphenadrine)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 162
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Orserdu
Coverage requires the following:
1. Diagnosis of estrogen receptor (ER)-positive, human epidermal growth factor receptor 2 (HER2)-negative, estrogen
receptor 1 (ESR1)-mutated advanced or metastatic breast cancer in postmenopausal women or men
2. Age ≥ 18 years old
3. Disease progression following at least one line of endocrine therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Otezla
Coverage requires the following:
1. Diagnosis of Psoriatic Arthritis
2. Age ≥ 18 years old
OR
1. Diagnosis of Psoriasis
2. Age ≥ 6 years old with weight at least 20 kg
3. Trial and treatment failure of one topical steroid
OR
1. Diagnosis of oral ulcers associated with Behcet disease
2. Age ≥ 18 years old
3. Trial and treatment failure to one topical steroid for oral ulcers such as triamcinolone paste
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 163
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Otrexup
Coverage requires the following:
1. Diagnosis of rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, or psoriasis
2. Trial and treatment failure of oral methotrexate
3. Trial and treatment failure of injectable methotrexate
NC
NC
Ovidrel
Coverage requires the following:
1. It is being prescribed to treat infertility in accordance with generally accepted medical practice
2. The members benefit provides for coverage for infertility medications
Coverage is provided in accordance with your medical fertility benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 164
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Oxbryta
Coverage requires the following:
1. Diagnosis of sickle cell disease
2. Age ≥ 4 years old
3. Hemoglobin ≤ 10.5 g/dl
4. Not receiving long-term red blood cell transfusion therapy
5. Trial and failure after a minimum 6 month trial, contraindication, OR intolerance to hydroxyurea
OR
5. If requesting tablets for suspension, member cannot swallow tablets/capsules AND has tried and failed after
aminimum 6-month trial, a contraindication, or intolerance to Siklos (hydroxyurea)
Initial approval: 1 year
Renewal requires improved sickle cell disease control (including, but not limited to: improvement in hemoglobin, symptoms
improvement, or reduction in vaso-occlusive crises, and not receiving regular transfusion therapy)
Oxervate
Coverage requires the following:
Diagnosis of neurotrophic keratitis that has progressed to stage 2 or 3
Approval: 60 days
oxiconazole
(Oxistat)
Coverage requires the following:
1. Diagnosis of tinea pedis, tinea cruris or tinea corporis
2. Treatment failure to two topical over-the-counter antifungal agents
3. Treatment failure to two oral generic antifungal agents

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 165
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Oxtellar XR
Coverage requires the following:
1. Treatment of seizures in patients with epilepsy
2. Treatment failure or intolerance to at least 3 generic alternatives, one of which must be generic oxcarbazepine
(Trileptal)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
oxymorphone HCl
ER
(Opana ER)
Coverage requires the following:
1. Diagnosis of moderate to severe chronic pain requiring around the clock opioid analgesia for an extended period of
time
2. Trial and failure or intolerance to three generic long-acting opioids (examples include, but not limited to:
buprenorphine transdermal patch, tramadol, morphine, fentanyl, and methadone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Note: Coverage will not be provided if the patient is on more than one long acting opioid concurrently

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 166
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ozempic
Coverage requires the following:
1. For the treatment of Type 2 Diabetes or trial of one generic or preferred medication for the treatment of Type 2
Diabetes
2. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist-containing products
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Ozobax / baclofen
Coverage requires the following:
1. Diagnosis of spasticity
2. Trial and failure or intolerance to baclofen tablets OR member is unable to swallow tablets
3. Trial and failure or intolerance to Lyvispah
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Palforzia
Coverage for maintenance treatment requires the following:
1. FDA approved indication
2. Completion of all dose levels of up-dosing before starting maintenance
OR
1. Stable on maintenance dose
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 167
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Palynziq
Coverage requires the following:
1. Diagnosis of phenylketonuria
2. Age ≥ 18 years old
3. Following a phenylalanine-restricted diet
4. Phenylalanine concentration ≥ 600 umol/liter
5. Trial and failure of Kuvan (Requires prior authorization)
Initial approval: 1 year
Renewal requires current phenylalanine concentration < 600 µmol/L or at least a 20% reduction from baseline
Pancreaze
Coverage requires trial and treatment failure of Creon and Zenpep
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
pazopanib
(Votrient)
Coverage is provided for the treatment of FDA approved indications

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 168
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Pemazyre
Coverage requires the following:
1. Age ≥ 18 years old
2. For the treatment of previously treated, unresectable locally advanced or metastatic cholangiocarcinoma
3. Presence of fibroblast growth factor receptor 2 fusion or other rearragement (as detected by an FDA-approved
test)
OR
1. Age ≥ 18 years old
2. For the treatment of relapsed or refractory myeloid/lymphoid neoplasms (MLNs)
3. Presence of fibroblast growth factor receptor 1 (FGFR1) rearrangement
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Pertzye
Coverage requires trial and treatment failure of Creon and Zenpep
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 169
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Pheburane
Coverage requires the following:
1. Diagnosis of urea cycle disorder
2. Will be used as adjunctive therapy to dietary management (such as dietary protein restriction and/or amino acid
supplementation)
3. Trial and treatment failure of Buphenyl (sodium phenylbutyrate)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
phenoxy-benzamine
HCl
(Dibenzyline)
Coverage is provided for the treatment of hypertension and sweating episodes due to pheochromocytoma:
Age ≥ 18 years old
Preoperative treatment: for members who have experienced treatment failure of or intolerance to a preferred selective
alpha1-adrenergic receptor blocker (such as Cardura (doxazosin)) in combination with a preferred calcium channel blocker
(such as Norvasc (amlodipine))
Approval: 60 days
Non-preoperative treatment: for members who have experienced treatment failure of or intolerance to TWO selective
alpha1-adrenergic receptor blockers (such as Cardura (doxazosin)) where both are used in combination with a preferred
calcium channel blocker (such as Norvasc (amlodipine))
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 170
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
pirfenidone
(Esbriet)
Coverage is provided for the treatment of idiopathic pulmonary fibrosis (IPF)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Piqray
Coverage requires the following:
1. Treatment of hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2) negative,
advanced or metastatic breast cancer
2. Used in combination with fulvestrant
3. PIK3CA-mutation confirmed by FDA approved test
4. Progression of cancer after an endocrine-based regimen such as anastrozole (Arimidex), exemestane (Aromasin),
and letrozole (Femara)
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
OR for Piqray 250 mg tablet strength:
1. Diagnosis of PIK3CA‐Related Overgrowth Spectrum (PROS) confirmed by detection of a PIK3CA mutation or
based on clinical features suspected of PROS
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 171
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
pitavastatin (Livalo)
Coverage requires treatment failure or intolerance to at least two generic statins (examples include atorvastatin,
rosuvastatin, simvastatin)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Pomalyst
Coverage requires the following:
1. Diagnosis of Multiple myeloma
2. Used in combination with dexamethasone
3. Received at least 2 prior therapies including an immunomodulatory agent (ex. Thalidomide, lenalidomide) and a
proteasome inhibitor (ex. Bortezomib)
4. Disease progression within 60 days of completion of last therapy
OR
1. Diagnosis of AIDS-related Kaposi Sarcoma after failure of highly active antiretroviral therapy (HAART)
2. Used in combination with HAART
OR
1. Diagnosis of Kaposi Sarcoma in patients who are HIV-negative
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 172
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Pregnyl
Coverage requires the following:
1. It is being prescribed to treat infertility in accordance with generally accepted medical practice.
2. The member’s benefit provides for coverage for infertility medications
3. Coverage may be provided in accordance with your medical fertility benefit
For the diagnosis of:
1. Hypogonadotrophic hypogonadism secondary to a pituitary deficiency in males
OR
2. Prepubertal cryptorchidism not caused by anatomic obstruction
Procysbi
Coverage requires the following:
1. Treatment of nephropathic cystinosis
2. Has had a positive response to oral cysteamine (Cystagon) but has experienced intolerable side effects
NC
NC
Prodigy Voice
Glucose Meter
Coverage is provided when the member is visually impaired
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 173
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Promacta
Coverage requires the following:
1. Diagnosis of chronic immune thrombocytopenia (ITP) and persistent thrombocytopenia (platelet count < 100,000
mcL) for ≥ 3 months and requires all of the following:
a. Age ≥ 1 year of age
b. Inadequate response or patient must not be a candidate for corticosteroids, immunoglobulins or
splenectomy
c. Current platelet count is < 20,000 mcL or <30,000 mcL and has symptoms of active bleeding
d. Dose does not exceed 75mg/day
OR
2. Diagnosis of thrombocytopenia with chronic hepatitis C and requires all of the following:
a. ≥18 years of age
b. Platelets <75,000 mcL
c. Dose does not exceed 100mg/day
OR
3. Diagnosis of severe aplastic anemia and requires all of the following:
a. ≥ 2 years of age
b. Current platelets ≤ 30,000/mcL
c. Insufficient response to antithymocyte globulin based immunosuppressive therapy
OR
c. Using in combination with standard immunosuppressive therapy as first line treatment
d. Dose does not exceed 150mg/day
Initial approval: 3 months
Renewal of therapy requires ALL the following to be met:
1. Recent platelet count between 50,000 and 200,000/mcL OR for platelet counts outside this range, dosage has
been adjusted accordingly to FDA labeled recommendations
2. Dose does not exceed recommended maximum for indication

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 174
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Pulmozyme
Coverage requires a diagnosis of cystic fibrosis
pyrimethamine
(Daraprim)
Coverage is provided for the treatment of toxoplasmosis when used conjointly with a sulfonamide
Pyrukynd
Coverage requires the following:
1. Diagnosis of hemolytic anemia with pyruvate kinase (PK) deficiency
2. Age ≥ 18 years old
3. Must have clinical manifestations of disease, including, but not limited to, decreased hemoglobin (Hgb), increased
reticulocytes, bilirubin, and/or lactate dehydrogenase (LDH) levels AND either one of the following:
i. Serum assay showing a decrease of pyruvate kinase activity OR
ii. Genetic testing showing at least 2 variant alleles in the pyruvate kinase liver and red blood cell (PKLR)
gene
Initial approval: 6 months
Renewal requires improvement in pyruvate kinase (PK) deficiency, including, but not limited to, improvement in Hgb,
hemolysis laboratory results, and transfusion requirements
Qbrexza
Coverage requires the following:
1. Treatment of primary axillary hyperhidrosis
2. Age ≥ 9 years of age
3. Trial of Drysol
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 175
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Qelbree
Coverage requires the following:
1. Diagnosis of attention deficit hyperactivity disorder (ADHD)
2. Age ≥ 6 years old
3. Trial and treatment failure or intolerance to TWO generic or preferred products for the treatment of ADHD, at least
one of which must be a nonstimulant
OR
3. Member cannot swallow tablets/capsules
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Qinlock
Coverage requires the following:
1. Age ≥ 18 years old
2. For the treatment of advanced gastrointestinal stromal tumor (GIST)
3. Received prior treatment with 3 or more kinase inhibitors, including imatinib
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 176
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Qnasl
Coverage requires trial and failure or intolerance of 2 of the following intranasal steroids:
1. Generic fluticasone (Flonase)
2. Generic flunisolide (Nasalide)
3. Nasacort (over-the-counter)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
NC
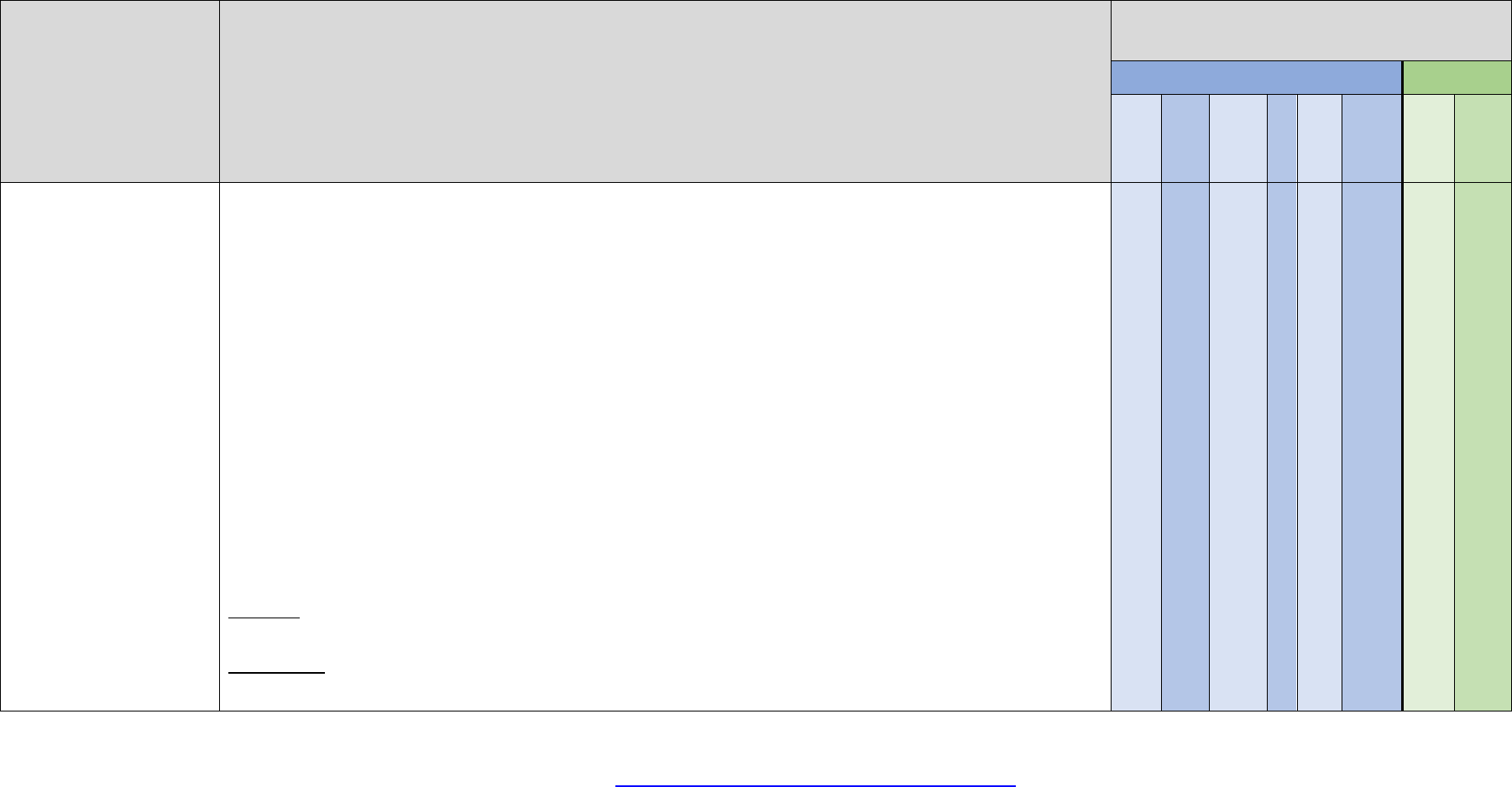
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 177
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Qsymia
Coverage requires the following:
1. Age ≥ 18 years old
2. BMI ≥ 30, or ≥ 27 with one weight related comorbid condition
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active
participation for a minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food
diaries, exercise logs, program receipts, app participation, etc.) if member does not have access to a covered
BCBSM/BCN program
5. Not to be used in combination with other weight loss products
OR
1. 12 to 17 years of age
2. BMI ≥ 95th percentile, standardized for age and sex
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active
participation for a minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food
diaries, exercise logs, program receipts, app participation, etc.) if member does not have access to a covered
BCBSM/BCN program
5. Not to be used in combination with other weight loss products
Initial approval: 6 months
For adults, continued coverage will be reviewed annually and may be provided if the member has maintained at least a 5%
weight loss from baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30
days) and BMI ≥ 18.5 kg/m2 must be submitted to the plan for review
For pediatrics, continued coverage will be reviewed annually and may be provided if the member has maintained at least a
3% reduction in BMI from baseline AND requires continued participation in a lifestyle modification program. Current weight
(within 30 days) and BMI-for-age percentile ≥ 5th percentile must be submitted to the plan for review
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 178
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Quillichew ER
Coverage requires the following:
1. The member is ≥ 6 years of age and diagnosed with ADHD or ADD
2. And has tried and failed both a generic methylphenidate and a generic amphetamine product, one of which must
be a generic long acting formulation
OR
2. Member cannot swallow tablets/capsules and has tried and failed one of the agents that can be opened and
sprinkled on applesauce, methylphenidate ER or generic amphetamine-dextroamphetamine (Adderall XR)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Quillivant XR
Coverage requires the following:
1. The member is ≥ 6 years of age and diagnosed with ADHD or ADD
2. And has tried and failed both a generic methylphenidate and a generic amphetamine product, one of which must
be a generic long acting formulation
OR
2. Member cannot swallow tablets/capsules and has tried and failed one of the agents that can be opened and
sprinkled on applesauce, methylphenidate ER or generic amphetamine-dextroamphetamine (Adderall XR)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 179
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Qulipta
Coverage requires the following:
1. For preventive treatment of migraine headaches
2. Age ≥ 18 years old
3. Member has history of ≥ 4 headache days per month
4. Trial of two medications from two different classes for the prevention of migraines
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Quviviq
Coverage requires treatment failure of 3 of the following: immediate-release zolpidem (Ambien), eszopiclone (Lunesta),
zaleplon (Sonata), trazodone (Desyrel), or doxepin (Silenor)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 180
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Radicava ORS
Coverage requires the following:
1. Diagnosis of Amyotrophic Lateral Sclerosis (ALS)
2. Prescribed by or in consultation with a neurologist
3. Start of treatment is within 2 years of diagnosis with amyotrophic lateral sclerosis (ALS)
OR
3. After 2 years of diagnosis, with a percent predicted vital capacity value of ≥ 80%
4. Submission of a baseline metrics from the ALSFRS-R (Revised ALS Functional Rating Scale)
5. Currently receiving treatment and will continue to receive treatment with Riluzole, if tolerated
Initial approval: 1 year
Renewal requires submission of patient assessments using the ALSFRS-R or other clinical documentation, to determine if
Radicava is slowing the progression of ALS
Ragwitek
Coverage requires the following:
1. Age 5 through 65 years old
2. Diagnosis of short ragweed pollen induced allergic rhinitis, confirmed by positive skin test or in vitro testing for
pollen-specific IgE antibodies for short ragweed pollen
3. Trial of one agent from each of the following classes:
a. Intranasal corticosteroid
b. Oral or intranasal antihistamine
Initial approval: 3 years
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 181
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
raloxifene
(Evista)
Coverage for $0 copayment will be provided when:
1. The member is a woman, at least 35 years of age and post-menopausal
2. The medication is being used for prevention of primary breast cancer in members classified as high risk
3. Cost share will not be waived for members with a history of breast cancer or venous thrombotic event (VTE)
Rasuvo
Coverage requires the following:
1. Diagnosis of rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, or psoriasis
2. Trial and treatment failure of oral methotrexate
3. Trial and treatment failure of injectable methotrexate
NC
NC
Ravicti
Coverage requires the following:
1. Diagnosis of urea cycle disorder
2. Will be used as adjunctive therapy to dietary management (such as dietary protein restriction and/or amino acid
supplementation)
3. Trial and treatment failure of Buphenyl (sodium phenylbutyrate)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 182
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Rayos
Coverage requires the following:
1. Diagnosis of rheumatoid arthritis
2. Trial or intolerance of two systemically absorbed generic oral corticosteroids, one of which must be prednisone
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Rebif
Coverage requires trial and failure or intolerance to two generic or preferred medications for the treatment of multiple
sclerosis (examples include: Avonex, Bafiertam, Betaseron, Copaxone, Kesimpta, and Vumerity)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Recorlev
Coverage requires the following:
1. Treatment of endogenous hypercortisolemia in patients with Cushing’s syndrome for whom surgery is not an option
or has not been curative
2. Age ≥ 18 years old
3. Trial and treatment failure, contraindication, or intolerance to ketoconazole, mitotane, or cabergoline
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 183
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Repatha
Coverage requires the following:
1. Diagnosis of primary hyperlipidemia, or prevention of cardiovascular events in patients with established cardiovascular
disease
a. Age ≥ 18 years old
b. Trial and failure of one high intensity statin
OR
b. History of statin intolerance (skeletal muscle related symptoms) after a trial of two generic statins (Examples include:
Crestor, Lescol, Lipitor, Livalo, Mevacor, Pravachol, Zocor)
OR
b. History of rhabdomyolysis after a trial of one statin (Examples include: Crestor, Lescol, Lipitor, Livalo, Mevacor,
Pravachol, Zocor)
c. Not to be used in combination with other PCSK9 inhibitors
OR
2. Diagnosis of homozygous familial hypercholesterolemia or heterozygoius familial hypercholesterolemia
a. Age ≥ 10 years old
b. Trial and treatment failure with one high intensity statin
OR
b. History of statin intolerance (skeletal muscle related symptoms) after a trial of two generic statins (Examples include:
Crestor, Lescol, Lipitor, Livalo, Mevacor, Pravachol, Zocor)
OR
b. History of rhabdomyolysis after a trial of one statin (Examples include: Crestor, Lescol, Lipitor, Livalo, Mevacor,
Pravachol, Zocor)
c. Not to be used in combination with other PCSK9 inhibitors
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 184
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Retevmo
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of Metastatic RET Fusion-Positive Non-Small Cell Lung Cancer
OR
1. Age ≥ 2 years old
2. Diagnosis of RET-Mutant Medullary Thyroid Cancer
OR
1. Age ≥ 2 years old
2. Diagnosis of RET Fusion-Positive Thyroid Cancer Refractory to radioactive iodine (if radioactive iodine is
appropriate)
OR
1. Age ≥ 2 years old
2. Diagnosis of RET Fusion-Positive solid tumor
3. Disease progression following prior systemic treatment OR there are no satisfactory alternative treatment options
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 185
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Revcovi
Coverage requires the following:
1. Diagnosis of adenosine deaminase (ADA) deficiency in patients with severe combined immunodeficiency disease
(SCID)
2. Prescribed by or in consultation with an immunologist
3. Confirmation of diagnosis by serum assay showing a decrease of adenosine deaminase activity followed by
genetic testing showing a mutation in the adenosine deaminase gene
4. Treatment failure of or not a suitable candidate for a bone marrow transplant
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Rexulti
Coverage requires the following:
1. Treatment of schizophrenia
2. Trial and failure, contraindication, or intolerance to two preferred second generation antipsychotics (examples
include: aripiprazole, clozapine, risperidone, quetiapine, olanzapine, ziprasidone)
OR
1. Treatment of agitation associated with dementia due to Alzheimer’s disease
OR
1. Adjunctive treatment of major depressive disorder (MDD)
2. Trial and failure, contraindication, or intolerance to two preferred second generation antipsychotics (examples
include: aripiprazole, clozapine, risperidone, quetiapine, olanzapine, ziprasidone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
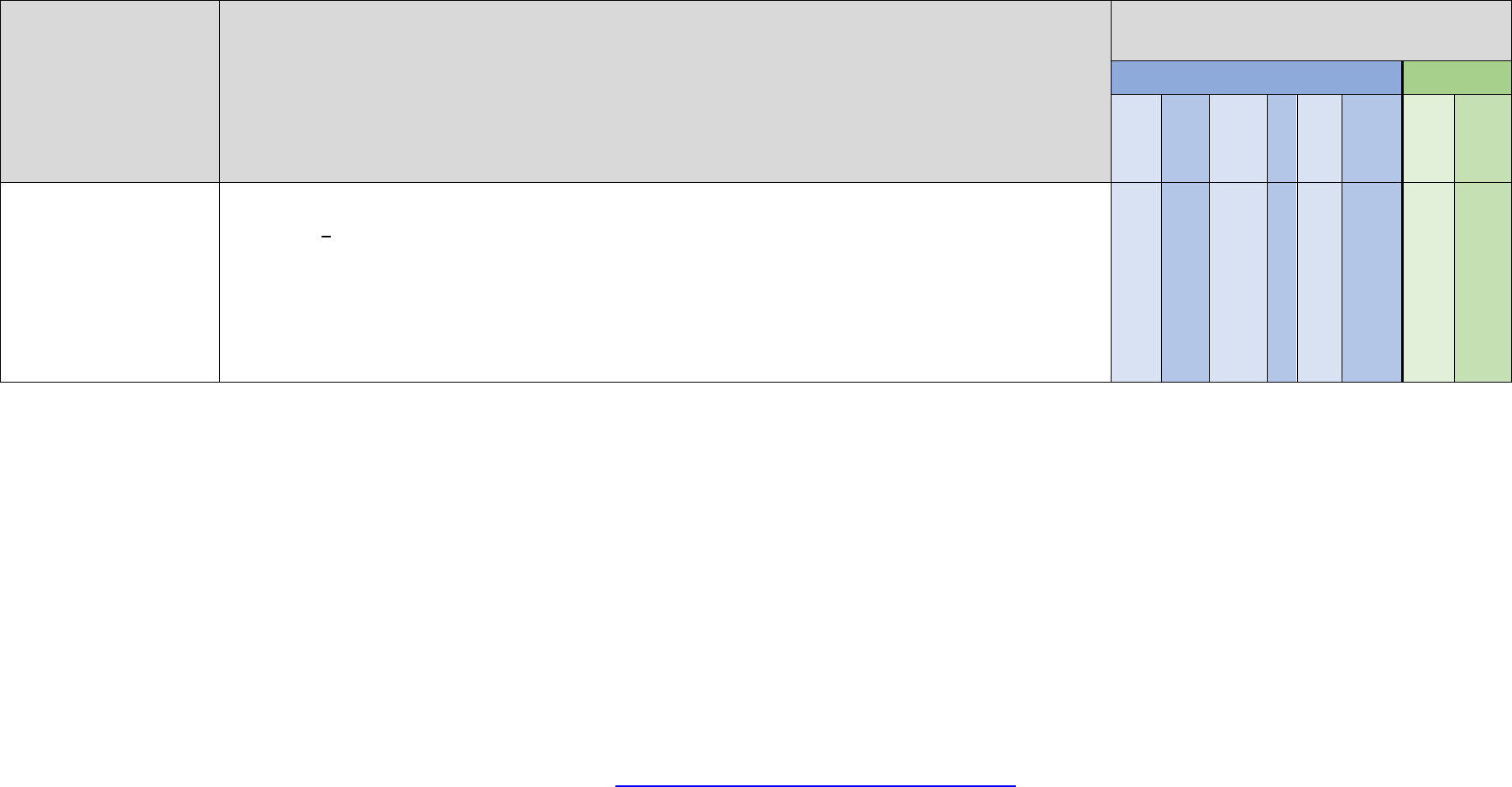
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 186
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Reyvow
Coverage requires the following:
1. Age > 18 years old
2. For the acute treatment of migraines
3. Trial and treatment failure, contraindication, or intolerance to 2 generic triptan medications
4. Trial and treatment failure, contraindication, or intolerance to Ubrelvy and Nurtec ODT
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 187
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Rezdiffra
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of noncirrhotic nonalcoholic steatohepatitis (NASH)
3. Presence of advanced liver fibrosis (stage F2 to F3) verified by FibroScan or other imaging-based non-invasive
liver disease assessment
4. Using in conjunction with diet and exercise
5. For members with BMI >27 kg/m2, documentation of active participation for a minimum of 3 months in a lifestyle
modification program
6. Member does not drink alcohol
Initial approval: 1 year
Renewal requires that current criteria are met AND
• Member has not progressed to cirrhosis AND
• That the medication is providing clinical benefit demonstrated by ONE of the following:
o NASH resolution and no worsening of fibrosis
o Improvement in fibrosis by ≥ 1 stage with no worsening of NASH or that the medication is providing clinical
benefit
o Improvement or stabilization of NASH demonstrated by imaging or blood based non-invasive liver disease
assessment

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 188
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Rezlidhia
Coverage requires the following:
1. Diagnosis of relapsed or refractory acute myeloid leukemia (AML) with a susceptible isocitrate dehydrogenase-1
(IDH1) mutation as detected by an FDA-approved test
2. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Rezurock
Coverage requires the following:
1. Age ≥ 12 years old
2. Diagnosis of chronic graft versus‐host disease (cGVHD) after failure of at least two prior lines of systemic therapy
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Please note: For quantity requests greater than one tablet per day due to concomitant proton pump inhibitor therapy, use of
a H2-receptor antagonist is recommended
Rhopressa
Coverage requires the following:
1. Trial of one generic medication, such as generic Xalatan, generic Lumigan, timolol
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 189
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Rinvoq tablet
Coverage requires the following:
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Psoriatic Arthritis
2. Age ≥ 2 years old
3. Weight ≥ 30kg
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Polyarticular Juvenile Idiopathic Arthritis
2. Age ≥ 2 years old
3. Weight ≥ 30 kg
4. Trial and failure of at least 3 months of one DMARD unless contraindicated or not tolerated.
Examples include methotrexate and leflunomide
5. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of moderate to severe Atopic Dermatitis
2. Age ≥ 12 years old
3. Weight ≥ 40 kg
4. Trial and treatment failure of one of the following: high potency topical corticosteroid, tacrolimus, pimecrolimus,
cyclosporine, methotrexate, azathioprine, or mycophenolate mofetil
5. Cannot be used in combination with other biologic agents indicated for severe atopic dermatitis
OR
1. Diagnosis of Ulcerative Colitis
2. Age ≥ 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
4. Trial and treatment failure to one or more tumor necrosis factor (TNF) inhibitor(s)
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 190
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Rinvoq tablet
(continued)
OR
1. Diagnosis of Crohn’s Disease
2. Age ≥ 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of ankylosing spondylitis
2. Age ≥ 18 years old
3. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Non-Radiographic Axial Spondyloarthritis with objective signs of inflammation
2. Age ≥ 18 years old
3. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 191
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Rinvoq LQ
Coverage requires the following:
1. Diagnosis of Psoriatic Arthritis
2. Age ≥ 2 years old
3. Weight ≥ 10 kg
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Polyarticular Juvenile Idiopathic Arthritis
2. Age ≥ 2 years old
3. Weight ≥ 10 kg
4. Trial and failure of at least 3 months of one DMARD unless contraindicated or not tolerated. Examples include
methotrexate and leflunomide
5. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
risedronate DR
(Atelvia)
Coverage requires trial and treatment failure or intolerance to two of the following:
1. Actonel (risedronate)
2. Boniva (ibandronate)
3. Fosamax (alendronate)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 192
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Rivfloza
Coverage requires the following:
1. Diagnosis of primary hyperoxaluria type 1 (PH1) confirmed by genetic testing of the AGXT mutation
2. Age ≥ 9 years old
3. Patient has an estimated glomerular filtration rate (eGFR) ≥ 30 ml/min/1.73 m2
4. Patient does not have a history of kidney or liver transplant
5. Trial and failure (for at least 3 months), contraindication, OR intolerance to a course of high-dose vitamin B-6
therapy
6. Will not be used in combination with Oxlumo
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Rocklatan
Coverage requires the following:
1. Trial of one generic medication, such as generic Xalatan, generic Lumigan, timolol
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Rolvedon
Coverage requires trial and failure or intolerance to Neulasta and Ziextenzo
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 193
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Rozlytrek
Coverage requires the following:
1. Treatment of metastatic non-small cell lung cancer in adults whose tumors are ROS1-positive, as detected by an
FDA-approved test
2. Age ≥ 18 years old
OR
1. Treatment of solid tumors that have a neurotrophic tyrosine receptor kinase (NTRK) gene fusion as detected by an
FDA-approved test without a known acquired resistance mutation
2. Age ≥ 1 month old
3. Tumor is metastatic or where surgical resection is not an option
4. Tumor has progressed following treatment or there is no alternative therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 194
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ruconest
Coverage requires the following:
1. Treatment of acute attacks of hereditary angioedema (HAE)
2. Diagnosis confirmed by genetic testing or with the following laboratory findings:
i. C4 level below the limits of the laboratory’s normal reference range (normal range = 16-58 mg/dL)
ii. C1INH (antigenic or function) below the limits of the laboratory’s normal reference range (normal range
≥ 41%)
3. Prescribed by an immunologist, allergist or hematologist
4. Trial and treatment failure of generic Firazyr (icatibant)
5. Not to be used in combination with other products indicated for acute HAE attacks
Initial approval: 1 year
Renewal requires objective data documenting at least 50% improvement in time to relief of symptoms of acute attacks
and maintenance of improvement of symptoms
rufinamide tablet
(Banzel)
Coverage requires the following:
1. Treatment of seizures associated with Lennox-Gastaut syndrome
2. Age ≥ 1 year old
3. Trial and failure, contraindication, OR intolerance to two generic alternatives for the treatment of Lennox-Gastaut
Syndrome
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 195
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ryaltris
Coverage requires trial and failure or intolerance to 1 generic intranasal steroid product after a minimum 3-month trial
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
NC
Rybelsus
Coverage requires the following:
1. For the treatment of Type 2 Diabetes or trial of one generic or preferred medication for the treatment of Type 2
Diabetes
2. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist-containing products
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Rydapt
Coverage requires the following:
1. Diagnosis of acute myeloid leukemia (AML) that is FLT3 mutation-positive as detected by an FDA-approved test.
2. Using in combination with cytarabine and daunorubicin induction and cytarabine consolidation
OR
1. Diagnosis of mast cell leukemia (MCL)
OR
1. Diagnosis of aggressive systemic mastocytosis or systemic mastocytosis with associated hematological neoplasm
(SM-AHN)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 196
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Rytary
Coverage requires trial and treatment failure of generic Sinemet CR
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Sancuso
Coverage requires the following:
1. Using for prevention and/or treatment of nausea/vomiting associated with chemotherapy and/or radiation therapy
2. Treatment/failure with generic ondansetron (Zofran)/ODT and generic granisetron (Kytril)
Initial approval: 1 year
Renewal requires continuation of chemotherapy
sapropterin
(Kuvan, Javygtor)
Coverage requires the following:
1. Treatment of phenylketonuria (PKU)
2. Following a phenylalanine-restricted diet

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 197
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Savella
Coverage requires the following
1. Diagnosis of fibromyalgia
2. Treatment failure or intolerance to gabapentin
3. Treatment failure or intolerance to 3 of the following:
a. Tricyclic antidepressant
b. Selective serotonin reuptake inhibitor (SSRI)
c. Serotonin norepinephrine reuptake inhibitor (SNRI)
d. Cyclobenzaprine (Flexeril)
e. Tramadol (Ultram)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 198
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Saxenda
Coverage criteria is determined by group benefit and requires one of the following:
1. Age ≥ 18 years old
2. BMI ≥ 30, or ≥ 27 with one weight related comorbid condition
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active participation for a
minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food diaries, exercise logs, program
receipts, app participation, etc.) if member does not have access to a covered BCBSM/BCN program
5. Not to be used in combination with other weight loss products
6. Cannot be used in combination with other glucagon-like peptide-1(GLP-1) agonist containing products
OR
1. 12 to 17 years of age
2. BMI corresponding to 30 or greater for adults
3. Current weight (within 30 days) above 132 lb (60 kg) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active participation for a
minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food diaries, exercise logs, program
receipts, app participation, etc.) if member does not have access to a covered BCBSM/BCN program
5. Not to be used in combination with other weight loss products
6. Cannot be used in combination with other glucagon-like peptide-1(GLP-1) agonist containing products
Initial approval: 6 months
For adults, continued coverage will be reviewed annually and may be provided if the member has maintained at least a 4% weight loss from
baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30 days) and BMI ≥ 18.5kg/m2 must be
submitted to the plan for review. Saxenda cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products
For pediatrics, continued coverage will be reviewed annually and may be provided if the member has maintained at least a 1% reduction in BMI
from baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30 days) and BMI-for-age percentile ≥
5th percentile must be submitted to the plan for review. Saxenda cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist
containing products
OR
1. Age ≥ 18 years old
2. Body mass index (BMI) ≥ 35 kg/m2
3. Documentation of current (within 30 days) baseline weight
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 199
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Saxenda
(continued)
4. Documentation of active participation for a minimum of 6 months in a lifestyle modification program and documentation of current active
participation in Teladoc Health Weight Management Program** must be submitted to the plan
5. Must be prescribed by a PCP or provider who has an established relationship with the member that the member has seen in-person
6. Not to be used in combination with other weight loss products
7. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products
8. Will not be covered for members with Type 2 Diabetes Mellitus
OR
1. 12 to 17 years of age
2. BMI corresponding to 30 or greater for adults
3. Current weight (within 30 days) above 132 lb (60 kg) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active participation for a
minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food diaries, exercise logs, program
receipts, app participation, etc.) if member does not have access to a covered BCBSM/BCN program
5. Not to be used in combination with other weight loss products
6. Cannot be used in combination with other glucagon-like peptide-1(GLP-1) agonist containing products
Initial approval: 6 months
Continued coverage for adults may be provided if the member has maintained at least a 5% weight loss from baseline AND
1. Documentation of active participation for a minimum of 6 months in a lifestyle modification program and documentation of current active
participation in Teladoc Health Weight Management Program** must be submitted to the plan AND
2. Must be prescribed by a PCP or provider, with an established relationship with the member, that the member has seen in-person AND
3. Current weight (within 30 days) must be submitted to the plan for review AND
4. Patient's BMI was ≥ 35 kg/m2 prior to starting treatment, current BMI ≥ 18.5kg/m2 AND
5. Patient must have a proportion of days covered ≥ 80% AND
6. Not to be used in combination with other weight loss products AND
7. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products AND
8. Will not be covered for members with Type 2 Diabetes Mellitus
Continued coverage for pediatrics will be reviewed annually and may be provided if the member has maintained at least a 1% reduction in BMI
from baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30 days) and BMI-for-age percentile ≥
5th percentile must be submitted to the plan for review. Saxenda cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist
containing products
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 200
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Saxenda
(continued)
**Proof of active engagement requires at a minimum: documentation that the member has met with a Teladoc weight management coach and the
member has a plan of action
NC
NC
Scemblix
Coverage requires the following:
1. Treatment of philadelphia chromosome‐positive chronic myeloid leukemia (Ph+ CML) in chronic phase (CP)
2. Previously treated with two or more tyrosine kinase inhibitors (TKIs)
3. Age ≥ 18 years old
OR
1. Treatmentt of philadelphia chromosome‐positive chronic myeloid leukemia (Ph+ CML) in chronic phase (CP)
2. Presence of T315I mutation
3. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Secuado
Coverage requires the following:
Trial and failure, contraindication, or intolerance to two preferred second generation antipsychotics (examples include:
aripiprazole, clozapine, risperidone, quetiapine, olanzapine, ziprasidone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 201
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Serostim
Coverage requires the following:
1. Diagnosis of AIDS wasting cachexia
2. Age > 18 years old
3. Unexplained weight loss > 10% of baseline
4. Concomitant anti-viral therapy for the duration of treatment
sertraline HCl
capsule
Coverage requires that the member has been stable on generic sertraline tablets at a dose of 150 mg or 200 mg daily for at
least 3 months
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Signifor
Coverage requires the following:
1. Treatment of hypercortisolism as a result of endogenous Cushing’s syndrome
2. Surgical treatment has not been effective or is not an option
3. Treatment failure or intolerance to ketoconazole, mitotane, or cabergoline, unless contraindicated
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 202
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Siklos
Coverage requires the following:
1. Diagnosis of sickle cell anemia
2. Age ≥ 2 years old
3. Unable to swallow capsules
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
sildenafil citrate
suspension
(Revatio)
Coverage is provided for the treatment of pulmonary arterial hypertension (WHO Group 1) when the member is unable to
swallow tablets/capsules
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
sildenafil citrate
tablet
(Revatio)
Coverage is provided for the treatment of pulmonary arterial hypertension (WHO Group 1)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
sildenafil
(Viagra)
May be covered for the diagnosis of erectile dysfunction dependent on the plan’s benefit with quantity limit restrictions
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 203
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Simponi
Coverage requires the following:
1. Diagnosis of Ankylosing Spondylitis
2. Age ≥ 18 years old
OR
1. Diagnosis of Rheumatoid Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure to one Disease Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
OR
1. Diagnosis of Psoriatic Arthritis
2. Age ≥ 18 years old
OR
1. Diagnosis of Ulcerative Colitis
2. Age ≥ 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Sirturo
Coverage requires the following:
1. Age > 5 years old and weighting at least 15 kg
2. Treatment of pulmonary multi-drug resistant tuberculosis (MDR-TB)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 204
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Skyclarys
Coverage requires the following:
1. Diagnosis of Friedreich’s ataxia
2. Age ≥ 16 years old
3. Confirmation of diagnosis via genetic testing revealing two pathogenic mutations of the frataxin (FXN) gene
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Skyrizi
Coverage requires the following:
1. Diagnosis of Psoriasis
2. Age ≥ 18 years old
3. Trial and treatment failure of one topical steroid
OR
1. Diagnosis of Psoriatic Arthritis
2. Age ≥ 18 years old
OR
1. Diagnosis of Crohn’s Disease
2. Age ≥ 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 205
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
sodium oxybate
(Xyrem)
Coverage requires a diagnosis of narcolepsy AND:
1. Age ≥ 7 years of age
2. Cataplexy
3. For adults only - Trial and failure, contraindication, or intolerance to Wakix
OR
2. Excessive daytime sleepiness, AND
3. Trial and failure, contraindication, or intolerance to at least one generic or preferred treatment such as
methylphenidate or dextroamphetamine
4. For adults only - Trial and failure, contraindication, or intolerance to modafinil or armodafinil, AND Sunosi, AND
Wakix
Xyrem will not be approved if patient is being treated with sedative hypnotic agents, other CNS depressants or using
alcohol
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Sohonos
Coverage requires the following:
1. Age ≥ 8 years old for females OR age ≥ 10 years old for males
2. Diagnosis of fibrodysplasia ossificans progressiva (FOP) confirmed by genetic testing showing an ACVR1
mutation, for the reduction in the volume of new heterotopic ossification (HO)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 206
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Somavert
Coverage requires diagnosis of acromegaly in patients who have had an inadequate response to surgery and/or for whom
surgery is not an option
sorafenib
(Nexavar)
Coverage is provided for the treatment of the FDA approved indications
Sotyktu
Coverage requires the following:
1. Diagnosis of Psoriasis
2. Age ≥ 18 years old
3. Trial and treatment failure of one topical steroid
4. Trial and treatment failure of two of the following: Cimzia, Enbrel, Humira, Otezla, Skyrizi, Stelara, or Tremfya
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 207
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Sovaldi tablets
Coverage requires the following:
If cirrhosis is present: documentation of decompensated or compensated cirrhosis
AND one of the following:
1. Age 18 years or older
2. Diagnosis of chronic hepatitis C genotype 1, 2, 3, or 4
3. Trial of preferred medication: Epclusa or Zepatier
4. If treatment experienced, documentation of previous treatment experience for Hepatitis C
OR
1. Age 3 years or older
2. Diagnosis of chronic hepatitis C genotype 2 or 3
3. Using in combination with ribavirin
Drug will be reviewed on a case by case basis utilizing AASLD guidelines and FDA approved package labeling and trial and
failure of Epclusa or Zepatier
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 208
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Sovaldi oral pellets
Coverage requires the following:
If cirrhosis is present: documentation of decompensated or compensated cirrhosis
AND one of the following:
1. Age 18 years or older
2. Diagnosis of chronic hepatitis C genotype 1, 2, 3, or 4
3. Trial of preferred medication: Epclusa or Zepatier
4. If treatment experienced, documentation of previous treatment experience for Hepatitis C
OR
1. Age 3 years or older
2. Diagnosis of chronic hepatitis C genotype 2 or 3
3. Using in combination with ribavirin
Drug will be reviewed on a case by case basis utilizing AASLD guidelines and FDA approved package labeling and trial and
failure of Epclusa or Zepatier

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 209
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Spevigo
Coverage requires the following:
1. For the prevention of Generalized Pustular Psoriasis (GPP) as defined by the European Rare and Severe Psoriasis
Expert Network
2. Age ≥ 12 years old
3. Weight ≥ 40 kg
4. A GPPGA total score of 0 or 1
5. A history of at least 2 past moderate-to-severe GPP flares with new or worsening pustulation
6. Trial of at least one of the following systemic therapies for the prevention of GPP flares and continued to
experience GPP flares either during treatment, following dose reduction, or following/within one year of treatment
discontinuation, unless contraindicated or not tolerated: acitretin, methotrexate, cyclosporine, infliximab
7. Not to be used in combination with other biologics or targeted DMARDs
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Spritam
Coverage requires the following:
1. Treatment of seizure disorder/epilepsy
2. Member is unable to swallow tablets or capsules
3. Trial of 3 generic or preferred alternatives, one of which must be generic levetiracetam (Keppra) solution
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Sprycel
Coverage is provided for the treatment of the FDA approved indications
Staxyn
May be covered for the diagnosis of erectile dysfunction dependent on the plan’s benefit with quantity limit restrictions
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 210
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Stelara
Coverage requires the following:
1. Diagnosis of Psoriasis
2. Age > 6 years old
3. Trial and treatment failure of one topical steroid
OR
1. Diagnosis of Psoriatic Arthritis
2. Age > 6 years old
OR
1. Diagnosis of Crohn’s Disease
2. Age > 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
OR
1. Diagnosis of Ulcerative Colitis
2. Age > 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Stendra
May be covered for the diagnosis of erectile dysfunction dependent on the plan’s benefit with quantity limit restrictions
NC
NC
Stimufend
Coverage requires trial and failure or intolerance to Neulasta and Ziextenzo

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 211
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Stivarga
Coverage requires the following:
1. Diagnosis of metastatic or unresectable gastrointestinal stromal tumors and disease progression or intolerance to
treatment with imatinib and sunitinib
OR
2. Diagnosis of metastatic colorectal cancer (mCRC) and prior treatment with fluoropyrimidine-, oxaliplatin- and
irinotecan-based chemotherapy, an anti- VEGF therapy, and, if RAS wild type, an anti-EGFR therapy
OR
3. Treatment of hepatocellular cancer in patients who have previously been treated with sorafenib
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Strensiq
Coverage requires the following:
1. Diagnosis of perinatal/infantile and juvenile-onset hypophosphatasia.
2. < 18 years old at onset of symptoms
3. Diagnosis confirmed by one or two pathogenic variants in the ALPL gene +
4. Must have documentation of active disease manifestations such as: skeletal malformations/fractures, respiratory
difficulties, dental manifestations, kidney damage, or seizures
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 212
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Subsys
Coverage requires the following:
1. Medication is being used for the treatment of breakthrough cancer pain
2. Member is tolerant to high dose opioids
3. Currently receiving a long acting opioid
4. Treatment failure or intolerance to oral immediate release narcotics (examples include, but not limited to: morphine,
oxycodone, or hydrocodone containing products)
5. Treatment failure or intolerance to generic Actiq
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Sucraid
Coverage is provided for the treatment of congenital sucrase-isomaltase deficiency
sumatriptan
succinate/
naproxen sodium
(Treximet)
Coverage requires the following:
1. Treatment failure or intolerance to generic sumatriptan (Imitrex) and naproxen used in combination
2. Treatment failure or intolerance to a second generic triptan (Maxalt, Amerge, Zomig/ZMT)
OR
1. Age 12-17 years old
2. Treatment failure or intolerance to generic Maxalt (rizatriptan)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 213
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
sunitinib
(Sutent)
Coverage requires the following:
1. Treatment of advanced renal cell carcinoma (RCC)
OR
1. Treatment of gastrointestinal stromal tumor (GIST)
2. Disease progression or intolerance to imatinib (Gleevec)
OR
1. Treatment of progressive, well-differentiated pancreatic neuroendocrine tumors in patients with unresectable locally
advanced or metastatic disease
OR
1. Adjuvant treatment of adult patients at high risk of recurrent RCC following nephrectomy
Sunosi
Coverage requires the following:
1. Age > 18 years old
2. Diagnosis of excessive daytime sleepiness associated with narcolepsy or obstructive sleep apnea (OSA)
3. For a diagnosis of OSA: Nonpharmacologic treatment has been initiated (ex. CPAP)
4. Trial and treatment failure of modafinil or armodafinil
5. Trial and treatment failure of one generic or preferred treatment such as methylphenidate or dextroamphetamine
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 214
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Symdeko
Coverage requires the following:
1. Age > 6 years old
2. Diagnosis of cystic fibrosis (CF)
3. Presence of two copies of the F508del mutation OR at least one mutation in the CFTR gene that is responsive to
Symdeko as confirmed by genetic test
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Sympazan
Coverage requires the following:
1. Diagnosis of Lennox-Gastaut syndrome
2. Trial of generic clobazam tablets AND generic clobazam solution
OR
2. Documentation that the member is unable to swallow tablets/capsules/solution
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Synribo
Coverage requires the following:
Treatment of adult patients with chronic or accelerated phase chronic myeloid leukemia (CML) with resistance and/or
intolerance to two or more tyrosine kinase inhibitors
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 215
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tabrecta
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of metastatic non-small cell lung cancer (NSCLC)
3. Tumor has a mutation that leads to mesenchymal-epithelial transition (MET) exon 14 skipping
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
tadalafil
(Adcirca, Alyq)
Coverage requires the following:
1. Diagnosis of pulmonary arterial hypertension (WHO Group 1)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
tadalafil
(Cialis)
May be covered for the diagnosis of erectile dysfunction dependent on the plan’s benefit with quantity limit restrictions
NC
NC
Tadliq
Coverage requires the following:
1. Diagnosis of pulmonary arterial hypertension (WHO Group 1)
2. Member is unable to swallow tablets
3. Trial and failure, intolerance or contraindication to generic sildenafil suspension
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 216
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tafinlar
Coverage requires the following:
1. Diagnosis of melanoma
2. Presence of BRAF V600E or V600K mutation
3. Using as a single agent or in combination with Mekinist (trametinib)
OR
1. Diagnosis of metastatic non-small cell lung cancer or advanced or metastatic anaplastic thyroid cancer
2. Presence of BRAF V600 E mutation
3. Using in combination with Mekinist (trametinib)
OR
1. Age ≥ 1 year old
2. Diagnosis of unresectable or metastatic solid tumors who have progressed following prior treatment and have no
satisfactory alternative treatment options
3. Presence of with BRAF V600E mutation
4. Using in combination with Mekinist (trametinib)
OR
1. Age ≥ 1 year old
2. Diagnosis of low-grade glioma (LGG) with a BRAF V600E mutation requiring systemic therapy
3. Using in combination with Mekinist
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression or unacceptable toxicity

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 217
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tagrisso
Coverage requires the following:
1. Diagnosis of metastatic epidermal growth factor (EGFR) T790M mutation-positive non-small cell lung cancer
(NSCLC) as detected by an FDA-approved test
2. Progression on or after EGFR tyrosine kinase inhibitor (TKI) therapy
OR
1. Diagnosis of metastatic non-small cell lung cancer (NSCLC)
2. Presence of EGFR exon 19 deletions or exon 21 L858R mutation
OR
1. Adjuvant treatment of non-small cell lung cancer (NSCLC) after tumor resection
2. Presence of EGFR exon 19 deletion or exon 21 L858R mutation as detected by an FDA-approved test
OR
1. Diagnosis of locally advanced or metastatic non-small cell lung cancer (NSCLC)
2. Presence of EGFR exon 19 deletion or exon 21 L858R mutation as detected by an FDA-approved test
3. Using as first-line treatment in combination with pemetrexed and platinum-based chemotherapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 218
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Takhzyro
Coverage requires the following:
1. Diagnosis of hereditary angioedema (HAE)
2. Diagnosis confirmed by genetic testing or with the following laboratory findings:
i. C4 level below the limits of the laboratory’s normal reference range (normal range = 16-58 mg/dL)
ii. C1INH (antigenic or function) below the limits of the laboratory’s normal reference range (normal range ≥41%)
3. History of at least 2 HAE attacks per month OR a history of attacks that are considered severe with swelling of the
face, throat or gastrointestinal tract
4. Prescribed by an immunologist, allergist or hematologist
5. Not to be used in combination with other products indicated for HAE prophylaxis
Initial approval: 1 year
Renewal requires improvement in HAE demonstrated by a 50% reduction in the number of attacks OR the severity of HAE
attacks was reducted by 50% or more

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 219
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Taltz
Coverage requires the following:
1. Diagnosis of Psoriasis
2. Age ≥ 6 years old
3. Trial and treatment failure of one topical steroid
4. Trial and treatment failure of one of the following: Enbrel, Humira, Cimzia, Skyrizi, Stelara, or Tremfya
OR
1. Diagnosis of Psoriatic Arthritis
2. Age ≥ 18 years old
3. Trial and treatment failure of one of the following: Enbrel, Humira, Cimzia, Simponi, Stelara, Rinvoq, Skyrizi,
Tremfya, or Xeljanz/XR
OR
1. Diagnosis of active Non-Radiographic Axial Spondyloarthritis with objective signs of inflammation
2. Age ≥ 18 years old
3. Trial and treatment failure of Cimzia or Rinvoq
OR
1. Diagnosis of active Ankylosing Spondylitis
2. Age ≥ 18 years old
3. Trial and treatment failure of Enbrel, Humira, Cimzia, Simponi, Xeljanz/XR, or Rinvoq
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 220
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Talzenna
Coverage requires the following:
1. Diagnosis of HER2-negative locally advanced or metastatic breast cancer
2. Presence of deleterious BRCA mutation, as detected by an FDA approved test
OR
1. Diagnosis of metastatic castration-resistant prostate cancer (mCRPC)
2. Presence of homologous recombination repair (HRR) gene mutation
3. Using in combination with enzalutamide
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
tamoxifen
Coverage for $0 copayment will be provided when:
1. The member is a woman at least 35 years of age
2. The medication is being used for prevention of primary breast cancer in members classified as high risk
3. Does not have a history of breast cancer
4. Does not have a family or personal history of venous thromboembolic events (VTE)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 221
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tarpeyo
Coverage requires the following:
1. Intended to reduce the loss of kidney function for the diagnosis of primary immunoglobulin A nephropathy (IgAN) at
risk of disease progression
2. Age ≥ 18 years old
3. Trial and failure to maximally tolerated dose of angiotensin converting enzyme (ACE) inhibitor or angiotensin
receptor blocker (ARB) therapy unless contraindicated
4. Trial and failure, contraindication, or intolerance to generic methylprednisolone, prednisolone, or prednisone
Initial approval: 9 months
Tascenso ODT
Coverage requires the following:
1. Diagnosis of multiple sclerosis (MS)
2. Age ≥ 10 years old
3. Will not be used in combination with other disease-modifying treatments for multiple sclerosis
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 222
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
tasimelteon
(Hetlioz)
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of Non-24-hour sleep-wake disorder in patients who are totally blind and unable to perceive light
3. Trial and failure, contraindication, or intolerance to over-the-counter melatonin AND Rozerem (ramelteon)
OR
1. Age ≥ 16 years old
2. Diagnosis of nighttime sleep disturbances in Smith-Magenis Syndrome (SMS) confirmed by genetic testing
showing deletion of chromosome 17p11.2 OR mutation in the retinoic acid-induced 1 (RAI1) gene
3. Trial and failure, contraindication, or intolerance to over-the-counter melatonin AND acebutolol
4. For adults only- Trial and failure, contraindication, or intolerance to Rozerem (ramelteon)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Tavneos
Coverage requires the following:
1. Adjunctive treatment of severe active anti-neutrophil cytoplasmic autoantibody (ANCA)-associated vasculitis
(granulomatosis with polyangiitis [GPA] and microscopic polyangiitis [MPA]) in combination with standard therapy
including glucocorticoids
2. Age ≥ 18 years old
3. Must be initiated in combination with a standard therapy regimen that includes either cyclophosphamide plus
glucocorticoids or rituximab/rituximab biosimilar plus glucocorticoids
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 223
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tasigna
Coverage is provided for the treatment of the FDA approved indications
Tavalisse
Coverage requires the following:
Diagnosis of chronic immune thrombocytopenia (IT) and persistent thrombocytopenia (platelet count < 100,000mcl) for ≥ 3
months and all of the following:
1. Age ≥ 18 years old
2. Trial and treatment failure or not a candidate for treatment with corticosteroids, immunoglobulins or splenectomy
3. Current platelet count is < 20,000 mcl or < 30,000 mcl and symptoms of active bleeding
4. Trial of Promacta
Initial approval: 3 months
Renewal requires a stable platelet count of at least 50,000/mcL

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 224
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tazverik
Coverage requires the following:
1. Age ≥ 16 years old
2. Diagnosis of epithelioid sarcoma
3. Not eligible for complete resection
OR
1. Age > 18 years old
2. Diagnosis of relapsed or refractory follicular lymphoma with tumors that are positive for an EZH2 mutation as
detected by an FDA-approved test
3. Recieved at least 2 prior therapies
OR
1. Age > 18 years old
2. Diagnosis of relapsed or refactory folliclar lymphoma
3. No satisfactory alternative treatment options
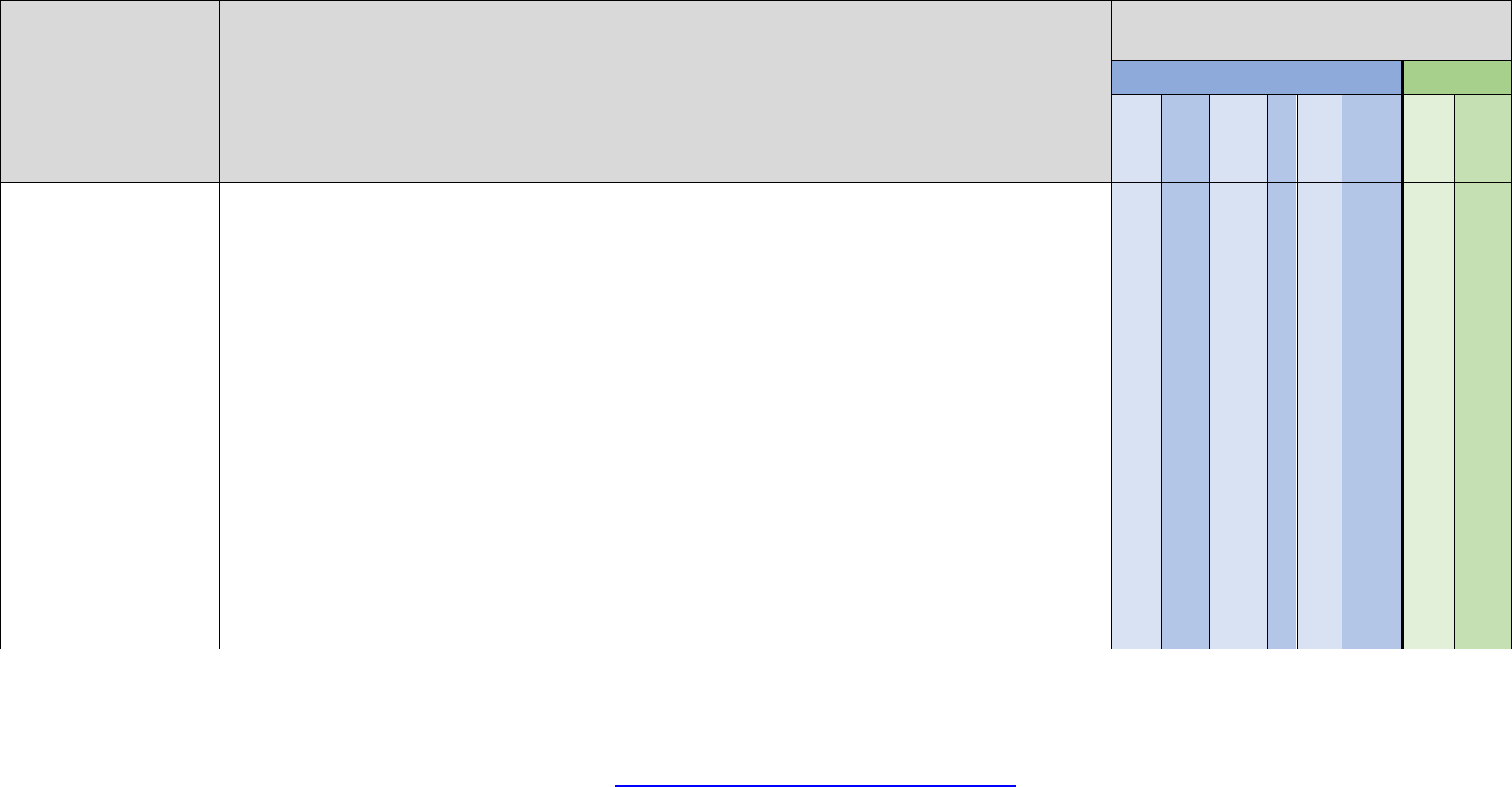
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 225
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tegsedi
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of peripheral nerve disease caused by hereditary transthyretin-mediated amyloidosis (hATTR) with aTTR
gene mutation
3. Signs and symptoms of ocular or cerebral area involvement (such as intraocular amyloidosis or
primary/leptomeningeal amyloidosis), if present, must not predominate over polyneuropathy symptomology
associated with hATTR
4. Documentation of clinical signs and symptoms of peripheral neuropathy (such as: tingling or increased pain in the
hands, feet and/or arms, loss of feeling in the hands and/or feet, numbness or tingling in the wrists, carpal tunnel
syndrome, loss of ability to sense temperature, difficulty with fine motor skills, weakness in the legs, difficulty
walking)AND/OR documentation of clinical signs and symptoms of autonomic neuropathy symptoms (such as:
orthostasis, abnormal sweating, dysautonomia [constipation and/or diarrhea, nausea, vomiting, anorexia, early
satiety])
5. Must have a baseline polyneuropathy disability (PND) score ≤ IIIb and/or baseline FAP Stage 1 or 2
6. Must not have New York Heart Association (NYHA) heart failure classification > 2
7. Must not have undergone a prior liver transplant
Tegsedi will not be approved for use in combination with other therapies approved for transthyretin-mediated amyloidosis
Initial approval: 1 year.
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 226
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tepmetko
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of metastatic non-small cell lung cancer (NSCLC)
3. Tumor has a mutation that leads to mesenchymal-epithelial transition (MET) exon 14 skipping
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
teriparatide (Forteo)
Coverage requires the following:
1. History of fragility fracture
2. Will not be used in combination with bisphosphonates, another anabolic bone-modifying agent or denosumab
OR
1. Diagnosis of osteoporosis
2. Treatment with a bisphosphonate has been ineffective after at least a 12-month treatment period based on
objective documentation (such as reduction in T score or fracture) UNLESS one of the following:
a. Treatment with bisphosphonates (both oral and intravenous) are not tolerated or contraindicated
b. History of fracture(s)
c. T-score less than -3.0
3. Will not be used in combination with bisphosphonates, another anabolic bone-modifying agent or denosumab
Initial approval: 2 years
Use of Forteo for more than 2 years should only be considered if high risk for fracture remains or has returned

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 227
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Testosterone,
topical
Androgel, generic
Androgel, Androderm.
generic Testim, generic
Vogelxo
Coverage requires the following:
1. Diagnosis of male hypogonadism
2. Two signs and symptoms specific to testosterone deficiency
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Testosterone,
topical
generic Axiron,
generic Fortesta
Testosterone 10mg (2%)
Testosterone 30mg
Testosterone 50mg (1%)
Coverage requires the following:
1. Diagnosis of male hypogonadism
2. Two signs and symptoms specific to testosterone deficiency
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
tetrabenazine
(Xenazine)
Coverage requires diagnosis of chorea associated with Huntington’s disease
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 228
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tezspire
Coverage requires the following:
1. Diagnosis of eosinophilic asthma
2. Age ≥ 12 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. Failure to maintain adequate control after at least a 3-month trial of daily oral corticosteroids or high dose inhaled
corticosteroids in combination with:
a. LABA (long acting inhaled β2 agonist)
OR
b. Leukotriene modifier
OR
c. LAMA (long acting muscarininc antagonist)
5. Cannot be used in combination with other biologic agents indicated for asthma
OR
1. Diagnosis of allergic asthma
2. Age ≥ 12 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. Failure to maintain adequate control after at least a 3-month trial of daily oral corticosteroids or high dose inhaled
corticosteroids in combination with:
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 229
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tezspire
(Continued)
OR
a. LABA (long acting inhaled β2 agonist)
OR
b. Leukotriene modifier
OR
c. LAMA (long acting muscarininc antagonist)
5. Cannot be used in combination with other biologic agents indicated for asthma
OR
1. Diagnosis of oral corticosteroid dependent asthma
2. Age ≥ 12 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. Failure to maintain adequate control after at least a 3-month trial of daily oral corticosteroids or high dose inhaled
corticosteroids in combination with:
a. LABA (long acting inhaled β2 agonist)
OR
b. Leukotriene modifier
OR
c. LAMA (long acting muscarininc antagonist)
5. Cannot be used in combination with other biologic agents indicated for asthma
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 230
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tezspire
(Continued)
OR
1. Diagnosis of severe asthma
2. Age ≥ 12 years old
3. Patient is currently receiving, and will continue to receive standard of care regimen
4. Failure to maintain adequate control after at least a 3-month trial of daily oral corticosteroids or high dose inhaled
corticosteroids in combination with:
a. LABA (long acting inhaled β2 agonist)
OR
b. Leukotriene modifier
OR
c. LAMA (long acting muscarininc antagonist)
5. Cannot be used in combination with other biologic agents indicated for asthma
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Tibsovo
Coverage requires the treatment of FDA approved indications
Teglutik
Coverage requires the following:
1. Diagnosis of Amyotrophic Lateral Sclerosis (ALS)
2. Trial of generic riluzole tablets
OR
2. Difficulty swallowing
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 231
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
tiopronin
(Thiola)
Coverage requires the following:
1. For the prevention of cystine stone formation in patients weighing ≥ 20 kilograms
2. Resistant to treatment with conservative measures of high fluid intake, sodium restriction, limited protein intake and
urine alkalization
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
tiopronin
(Thiola EC)
Coverage requires the following:
1. For the prevention of cystine stone formation in patients weighing ≥ 20 kilograms
2. Resistant to treatment with conservative measures of high fluid intake, sodium restriction, limited protein intake and
urine alkalization
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Tlando
Coverage requires the following:
1. Diagnosis of male hypogonadism
2. Two signs and symptoms specific to testosterone deficiency
3. Trial and failure, contraindication, or intolerance to one generic or preferred testosterone product (examples include
generic Androgel, Androderm, and generic Depo-Testosterone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 232
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tobi Podhaler
Coverage requires the following:
1. Member has cystic fibrosis and is infected with Pseudomonas aeruginosa
2. Trial and failure of generic Tobi (tobramycin) inhalation nebulization solution
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
tolvaptan
(Samsca)
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of clinically significant hyponatremia
3. Hyponatremia is defined as serum sodium <125 mEq/L or less marked hyponatremia that is symptomatic and has
resisted correction with fluid restriction
4. Therapy is initiated/re-initiated in a hospital
Approval: 60 days

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 233
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
topiramate ER
(Qudexy XR)
Coverage requires the following:
1. Treatment of seizure disorder/epilepsy
2. Treatment failure or intolerance to at least 3 generic alternatives, one of which must be generic topiramate
(Topamax)
OR
1. For preventative treatment of migraine headaches
2. Age ≥ 12 years old
3. Treatment failure or intolerance to 3 generic alternatives for the prevention of migraines, one of which must be
generic topiramate (Topamax)
OR
1. Diagnosis of Lennox-Gastaut Syndrome
2. Treatment failure or intolerance to at least 2 generic alternatives, one of which must be generic topiramate
(Topamax)
Initial approval: 1 year
Renewal requires that current criteria are met and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 234
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
topiramate extended
release
(Trokendi XR)
Coverage requires the following:
1. Treatment of seizure disorder/epilepsy
2. Treatment failure or intolerance to at least 3 generic alternatives, one of which must be generic topiramate
(Topamax)
OR
1. For preventative treatment of migraine headaches
2. Age ≥ 12 years old
3. Treatment failure or intolerance to 3 generic alternatives for the prevention of migraines, one of which must be
generic topiramate (Topamax)
OR
1. Diagnosis of Lennox-Gastaut Syndrome
2. Treatment failure or intolerance to at least 2 generic alternatives, one of which must be generic topiramate
(Topamax)
Initial approval: 1 year
Renewal requires that current criteria are met and that the medication is providing clinical benefit
NC
NC
Tracleer suspension
Coverage requires the following:
1. Diagnosis of pulmonary arterial hypertension (WHO Group 1)
2. Trial and treatment failure of sildenafil or tadalafil AND ambrisentan or bosentan

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 235
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tremfya
Coverage requires the following:
1. Diagnosis of Psoriasis
2. Age ≥ 18 years old
3. Trial and treatment failure of one topical steroid
OR
1. Diagnosis of Psoriatic Arthritis
2. Age ≥ 18 years old
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
trientine
hydrochloride
(Syprine)
Coverage requires the following:
1. Diagnosis of Wilson’s disease
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 236
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Trikafta
Coverage requires the following:
1. Diagnosis of cystic fibrosis
2. Age ≥ 2 years old
3. Presence of at least one copy of the F508del mutation OR at least one mutation in the cystic fibrosis
transmembrane conductance regulator (CFTR) gene that is responsive to Trikafta as confirmed by genetic test
4. Member is not using Trikafta in combination with an additional CFTR potentiator such as: Orkambi, Kalydeco, or
Symdeko
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Trintellix
Coverage requires trial and failure, contraindication, or intolerance to two antidepressant agents
Trulicity
Coverage requires the following:
1. For the treatment of Type 2 Diabetes or trial of one generic or preferred medication for the treatment of Type 2
Diabetes
2. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist-containing products
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 237
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Truqap
Coverage requires the following:
1. Diagnosis of hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative, locally
advanced or metastatic breast cancer
2. Age ≥ 18 years old
3. Presence of one or more PIK3CA/AKT1/PTEN-alterations as detected by an FDA-approved test
4. Progression on at least one endocrine-based regimen in the metastatic setting OR recurrence on or within 12
months of completing adjuvant therapy
5. Using in combination with fulvestrant
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 238
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tukysa
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of advanced unresectable or metastatic human epidermal growth factor receptor 2 (HER2)‐positive
breast cancer
3. Have received one or more prior anti‐HER2‐based regimens in the metastatic setting
4. Using in combination with trastuzumab and capecitabine
OR
1. Age ≥ 18 years old
2. Diagnosis of unresectable or metastatic RAS wild-type HER2-positive colorectal cancer
3. Previous treatment with fluoropyrimidine-, oxaliplatin-, and irinotecan-based chemotherapy
4. Using in combination with trastuzumab
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Turalio
Coverage requires the following:
1. Treatment of adult patients with symptomatic tenosynovial giant cell tumor (TGCT)
2. Condition is associated with severe morbidity or functional limitations
3. Will not be amenable to improvement with surgery.
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 239
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Tymlos
Coverage requires the following:
1. History of fragility fracture
2. Will not be used in combination with bisphosphonates, another anabolic bone-modifying agent or denosumab
OR
1. Diagnosis of osteoporosis
2. Treatment with a bisphosphonate has been ineffective after at least a 12-month treatment period based on
objective documentation (such as reduction in T score or fracture) UNLESS one of the following:
a. Treatment with bisphosphonates (both oral and intravenous) are not tolerated or contraindicated
b. History of fracture(s)
c. T-score less than -3.0
3. Will not be used in combination with bisphosphonates, another anabolic bone-modifying agent or denosumab
Tymlos will be approved for a maximum of 2 years
Tyvaso/Tyvaso DPI
Coverage requires the following:
1. Treatment of pulmonary arterial hypertension (WHO Group 1)
2. Trial and treatment failure of sildenafil or tadalafil AND ambrisentan or bosentan
OR
1. Treatment of pulmonary arterial hypertension associated with interstitial lung disease (PH-ILD; WHO Group 3)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 240
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ubrelvy
Coverage requires the following:
1. For acute treatment of migraine
2. Age ≥ 18 years old
3. Treatment failure or contraindication with 2 generic triptan medications
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Udenyca
Coverage requires trial and failure or intolerance to Neulasta and Ziextenzo
Uptravi
Coverage requires the following:
1. Diagnosis of pulmonary arterial hypertension (WHO Group 1)
2. Trial and treatment failure of sildenafil or tadalafil AND ambrisentan or bosentan
Valchlor
Coverage requires the following:
1. Diagnosis of Stage 1A or 1B mycosis fungoides type cutaneous T cell lymphoma
2. Trial and failure of two skin directed therapies (examples include phototherapy, total skin electron beam therapy,
topical retinoids, corticosteroids, carmustine)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 241
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Vanflyta
Coverage requires the following:
1. Age ≥ 18 years old
2. For the treatment of newly diagnosed acute myeloid leukemia (AML) that is FLT3 internal tandem duplication (ITD)-
positive as detected by an FDA-approved test
3. Using in combination with standard cytarabine and anthracycline induction and cytarabine consolidation
OR
3. Using as maintenance monotherapy following consolidation chemotherapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
vardenafil
(Levitra)
May be covered for the diagnosis of erectile dysfunction dependent on the plans benefit with quantity limit restrictions
NC
NC
varenicline
(Chantix)
Requires trial and failure of 2 preferred agents such as generic bupropion extended release (Zyban), nicotine patch,
nicotine gum, nicotine lozenge for $0 copayment

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 242
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Varubi
Coverage is provided for the prevention of chemotherapy-induced nausea/vomiting (CINV) and after a trial of all of the
following:
1. Generic 5HT3 antagonist (ex. generic Zofran, generic Kytril)
2. Preferred NK1 antagonist (ex. Emend)
3. Glucocorticoid (dexamethasone)
Initial approval: 1 year
Renewal requires continuation of chemotherapy
Vecamyl
Coverage requires treatment failure with or intolerance to all of the following drug classes:
1. Diuretic
2. Beta-Blocker
3. Ace-inhibitor
4. Angiotensin II receptor blocker
5. Calcium channel blocker
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Venclexta
Coverage requires the treatment of FDA approved indications
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 243
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ventavis
Coverage requires the following:
1. Diagnosis of pulmonary arterial hypertension (WHO Group 1)
2. Trial and treatment failure of sildenafil or tadalafil AND ambrisentan or bosentan
Verkazia
Coverage requires the following:
1. Diagnosis of vernal keratoconjunctivitis
2. Age ≥ 4 years old
3. Trial and failure, or intolerance to a dual acting, topical antihistamine/mast-cell stabilizer such as epinastine,
ketotifen and olopatadine
4. Trial and failure or intolerance to ophthalmic corticosteroids such as dexamethasone eye drops, Generic FML
liquifilm, FML, FML forte, loteprednol and generic Pred Forte
5. Trial and failure or intolerance to generic Restasis
OR
1. Diagnosis of vernal keratoconjunctivitis with compromised corneal epithelium/ corneal ulcers
2. Age ≥ 4 years old
3. Trial and failure or intolerance to generic Restasis
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 244
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Veozah
Coverage requires the following:
1. Treatment of moderate-to-severe vasomotor symptoms due to menopause
2. Age ≥ 18 years old
3. Trial and failure, contraindication, or intolerance to one preferred or generic medication for the treatment of
vasomotor symptoms
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
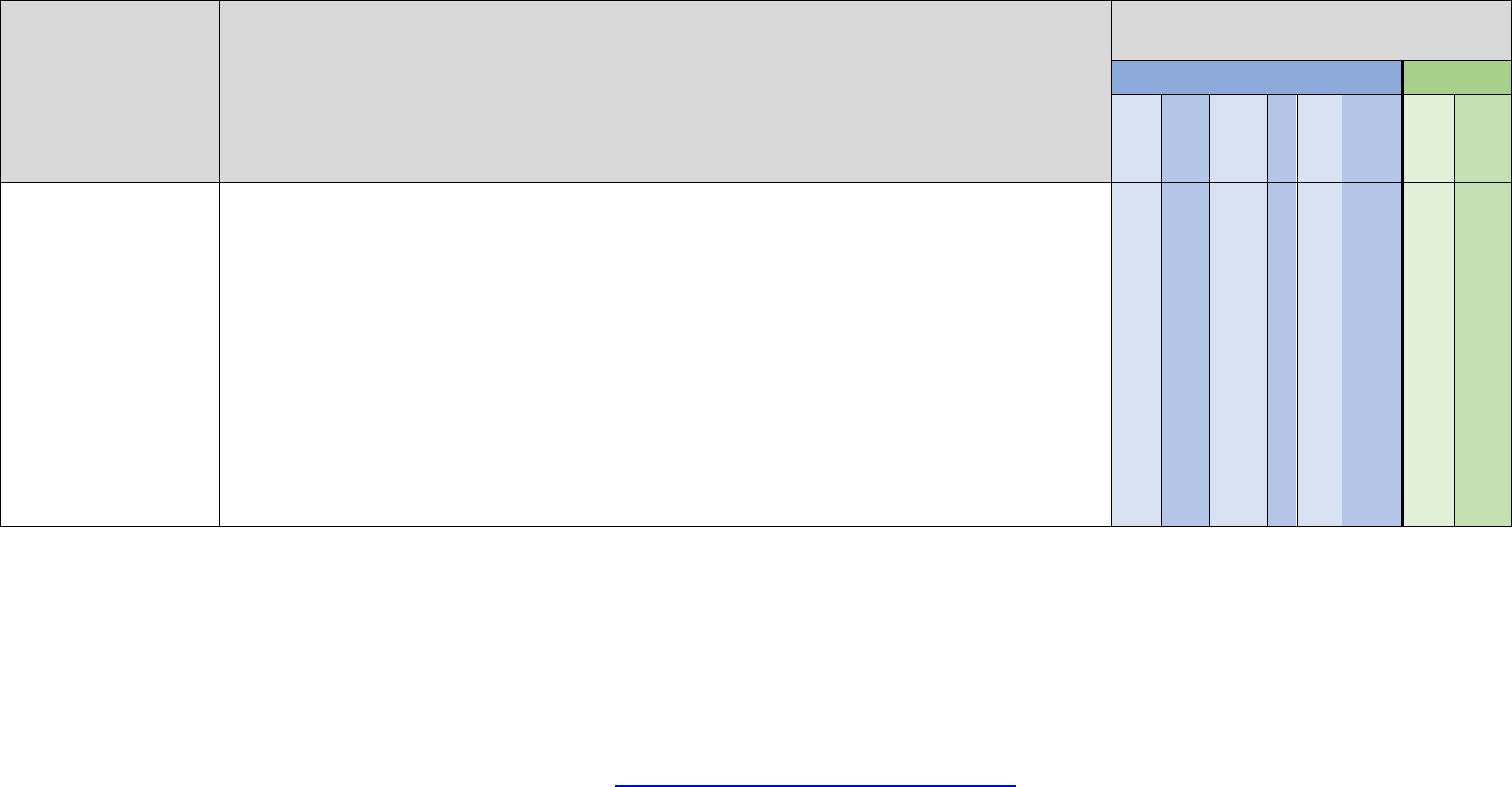
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 245
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Verquvo
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of chronic heart failure New York Heart Association (NYHA) Class II-IV
3. Left ventricular ejection fraction (LVEF) of less than 45%
4. History of ONE of the following:
i. Previous hospitalization for heart failure within prior 6 months OR
ii. Outpatient intravenous (IV) diuretic treatment for heart failure within prior 3 months
5. Taken in combination with at least TWO of the following unless contraindicated or not tolerated:
i. Metoprolol succinate, carvedilol, or bisoprolol
ii. An ACE-inhibitor (ACE, such as lisinopril), angiotensin receptor blocker (ARB, such as losartan), or
angiotensin receptor-neprilysin inhibitor (ARNI, such as sacubitril/valsartan)
iii. A sodium glucose cotransporter-2 (SGLT2) inhibitor approved for heart failure
iv. A mineralocorticoid receptor antagonist
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 246
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Verzenio
Coverage requires the following:
1. Diagnosis of HR-positive, HER-2 negative advanced or metastatic breast cancer and ONE of the following:
a. Using in combination with an aromatase inhibitor as initial therapy
OR
b. Using in combination with fulvestrant following endocrine therapy
OR
c. If metastatic, using as monotherapy following endocrine therapy AND prior chemotherapy
OR
1. Diagnosis of early HR-positive, HER-2 negative, node-positive breast cancer at high risk of recurrence
2. Using in combination with adjuvant endocrine therapy
Initial approval: 1 year
Continuation of coverage requires a lack of disease progression
Vesicare LS
Coverage requires the following:
1. Treatment of neurogenic detrusor overactivity (NDO)
2. Age ≥ 2 years old
3. Trial and failure of two anticholinergic drugs for the treatment of NDO
OR
3. Physician provides documentation that the member cannot swallow tablets/capsules and has tried and failed an
anticholinergic medication available as a solution
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 247
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Viberzi
Coverage requires the following:
1. Diagnosis of irritable bowel syndrome with diarrhea (IBS-D)
2. Trial and treatment failure, contraindication, or intolerance to a tricyclic antidepressant
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Victoza
Coverage requires the following:
1. For the treatment of Type 2 Diabetes or trial of one generic or preferred medication for the treatment of Type 2
Diabetes
2. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist-containing products
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
vigabatrin powder
(Sabril)
Coverage requires the following:
1. Diagnosis of infantile spasms
OR
1. Treatment of seizure disorder/epilepsy as adjunctive therapy
2. Trial and failure, contraindication, OR intolerance to three generic alternatives for the treatment of seizures
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 248
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
vigabatrin tablet
(Sabril)
Coverage requires the following:
1. Diagnosis of infantile spasms
OR
1. Treatment of seizure disorder/epilepsy as adjunctive therapy
2. Trial and treatment failure of three generic alternatives for seizure
3. Trial of Sabril powder
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Vijoice 50 mg, 125
mg tablet
Vijoice granules
Coverage requires the following:
1. Age ≥ 2 years old
2. Diagnosis of PIK3CA‐Related Overgrowth Spectrum (PROS) confirmed by detection of a PIK3CA mutation or
based on clinical features suspected of PROS
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Viokace
Coverage requires trial and treatment failure of Creon and Zenpep
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 249
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Vitrakvi
Coverage requires treatment of FDA approved indications
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Vivjoa
Coverage requires the following:
1. Diagnosis recurrent vulvovaginal candidiasis (RVVC) in females with history of RVVC who are not of reproductive
potential
2. Trial and failure, contraindication, or intolerance to generic oral fluconazole alone
Approval: 12 weeks
NC
NC
Vizimpro
Coverage requires the following:
Diagnosis of metastatic non-small cell lung cancer (NSCLC) with epidermal growth factor receptor (EGFR) exon 19 deletion
or exon 21 L858R substitution mutations as detected by an FDA-approved test
Vonjo
Coverage requires the following:
1. Diagnosis of intermediate or high-risk primary or secondary (post-polycythemia vera or post-essential
thrombocythemia) myelofibrosis with a platelet count < 50,000 mcl
2. Age ≥ 18 years old
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 250
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Voquezna
Coverage requires the following:
1. For the treatment of Helicobacter pylori (H. pylori) infection
2. Age ≥ 18 years old
3. Trial of a generic, guideline recommended, first-line regimen for H. pylori infection such as clarithromycin triple
therapy (proton pump inhibitor (PPI) + clarithromycin + amoxicillin or metronidazole) or bismuth quadruple therapy
(PPI + bismuth subcitrate or subsalicylate + tetracycline + metronidazole)
OR
1. For the treatment of erosive esophagitis (EE)
2. Age ≥ 18 years old
3. Trial and failure, contraindication, or intolerance to three of the following generic or over the counter (OTC) PPIs:
omeprazole (Prilosec), esomeprazole (Nexium), pantoprazole (Protonix), lansoprazole (Prevacid/Prevacid
Solutab), and rabeprazole (Aciphex)
Approval for H. pylori: 60 days
Approval for EE: 1 year
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 251
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Vosevi
Coverage requires the following:
1. Age 18 years or older
2. For patients with chronic hepatitis C genotype 1, 2, 3, 4, 5, or 6 infection that have failed treatment regimen
containing an NS5A (nonstructural protein 5A) inhibitor and have no liver damage or have liver damage and
showing no symptoms from the damage
3. For patients with chronic hepatitis C genotype 1a or 3 that have previously failed sofosbuvir containing regimen
without an NS5A inhibitor and have no liver damage or have liver damage and showing symptoms of the damage
4. Trial and failure to preferred medication: Epclusa or Zepatier
5. If treatment experienced, documentation of previous treatments for Hepatitis C
6. If cirrhosis is present: documentation of decompensated or compensated cirrhosis
Drug will be reviewed based on a case by case basis utilizing AASLD guidelines and FDA approved package labeling with
trial and failure of Epclusa or Zepatier
Vowst
Coverage requires the following:
1. To prevent the recurrence of Clostridioides difficile infection (CDI)
2. Age ≥ 18 years old
3. Had at least 1 recurrence after a primary episode of CDI AND completed one or more round(s) of standard-of-care
antibiotic therapy (ex: metronidazole, vancomycin, fidaxomicin)
OR
3. Two or more episodes of severe CDI resulting in hospitalization within the past year
4. Positive C. difficile stool test with toxin A/B results within the previous 30 days
5. Not to be used in combination with other products for prevention of CDI, such as Zinplava™ or Rebyota®
Approval: 60 days

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 252
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Voxzogo
Coverage requires the following:
1. Diagnosis of achondroplasia
3. Presence of fibroblast growth factor receptor 3 (FGFR3) gene mutation confirming diagnosis
4. Open epiphyses
5. Recent growth velocity and height (growth velocity must be > 1.5 cm/year)
Initial approval: 1 year
Renewal requires the presence of open epiphyses, and an updated height and growth velocity to show that growth has
been maintained or increased from baseline
Voydeya
Coverage requires the following:
1. Age ≥ 18 years old
2. Using as add-on therapy to Ultomiris or Soliris for the treatment of extravascular hemolysis (EVH) with paroxysmal
nocturnal hemoglobinuria (PNH)
3. Must have clinically significant extravascular hemolysis (EVH) due to paroxysmal nocturnal hemoglobinuria (PNH)
with the following:
i. Hemoglobin (Hgb) ≤ 9.5 g/dL
ii. Absolute reticulocyte count ≥ 120 × 109/L
4. Must be used in combination with Soliris® or Ultomiris® only
5. Trial and failure, contraindication, or intolerance to Empaveli and Fabhalta
Initial approval: 1 year
Renewal requires that current criteria are met and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 253
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Vraylar
Coverage requires the following:
6. Trial and failure, contraindication, or intolerance to two preferred second generation antipsychotics (examples
include: aripiprazole, clozapine, risperidone, quetiapine, olanzapine, ziprasidone)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Vtama
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of plaque psoriasis
3. Trial and failure, contraindication, or intolerance to a generic medium or high potency topical corticosteroid
4. Trial and failure, contraindication, or intolerance to at least one of the following generic topical steroid-sparing
agents: calcipotriene, tazarotene, tacrolimus, or pimecrolimus
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
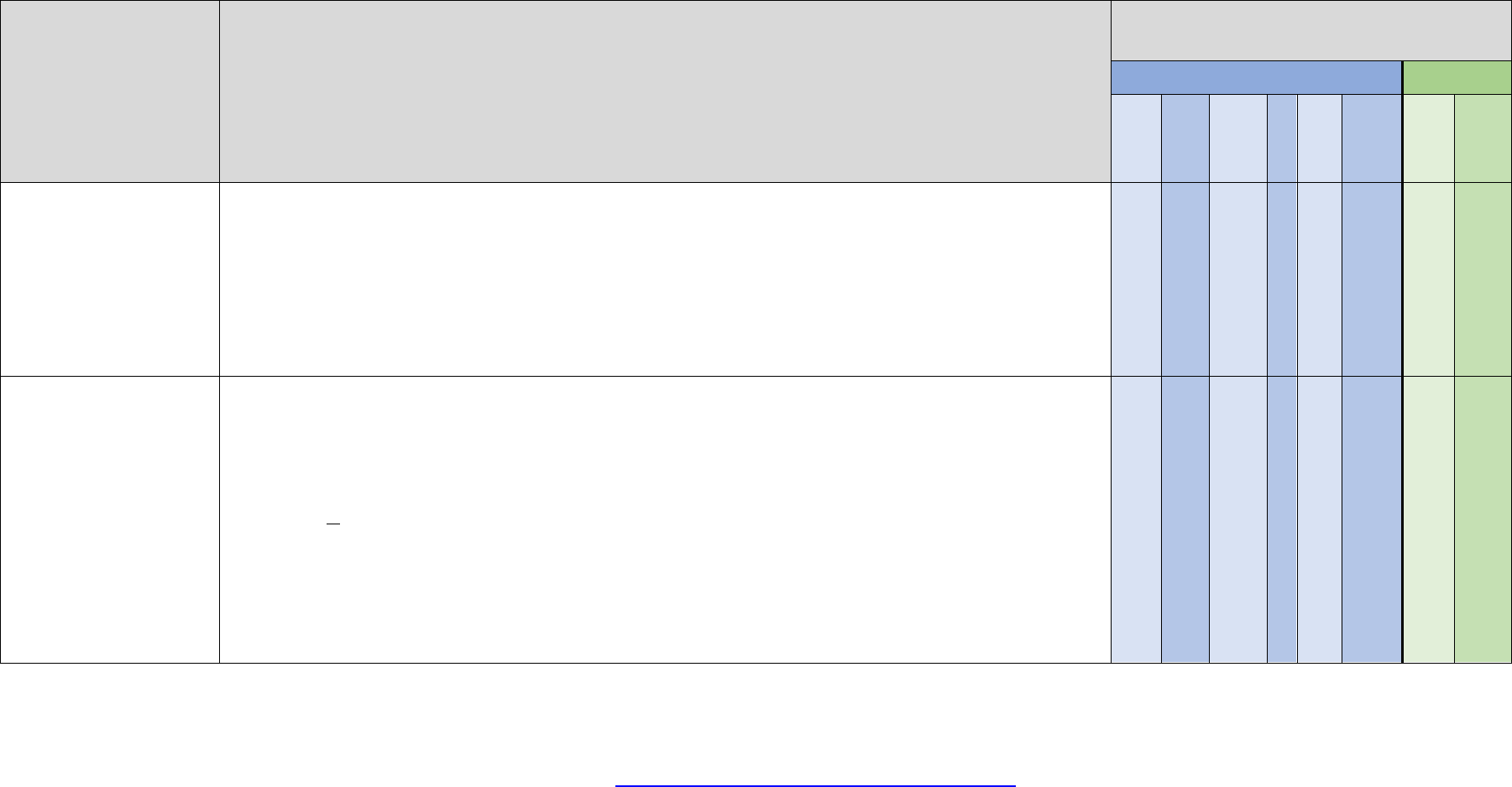
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 254
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Vyleesi
Coverage requires the following:
1. Premenopausal female ≥ 18 years old
2. Diagnosis of acquired, generalized hypoactive sexual desire disorder (HSDD) that has been ongoing for more than
6 months
3. Other causes (such as relationship difficulty, substance abuse, medication side effects) of HSDD must be ruled out
Initial approval: 60 days
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Vyndamax
Coverage requires the following:
1. Diagnosis of transthyretin-mediated amyloidosis with cardiomyopathy (ATTR-CM) confirmed by BOTH of the
following:
a. A negative monoclonal light chain screen ruling out amyloid light chain cardiomyopathy
b. Technetium-labeled bone scintigraphy
2. Age > 18 years old
3. Documentation of clinical signs and symptoms of ATTR-CM
Vyndamax will not be approved for use in combination with other therapies approved for transthyretin-mediated amyloidosis
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
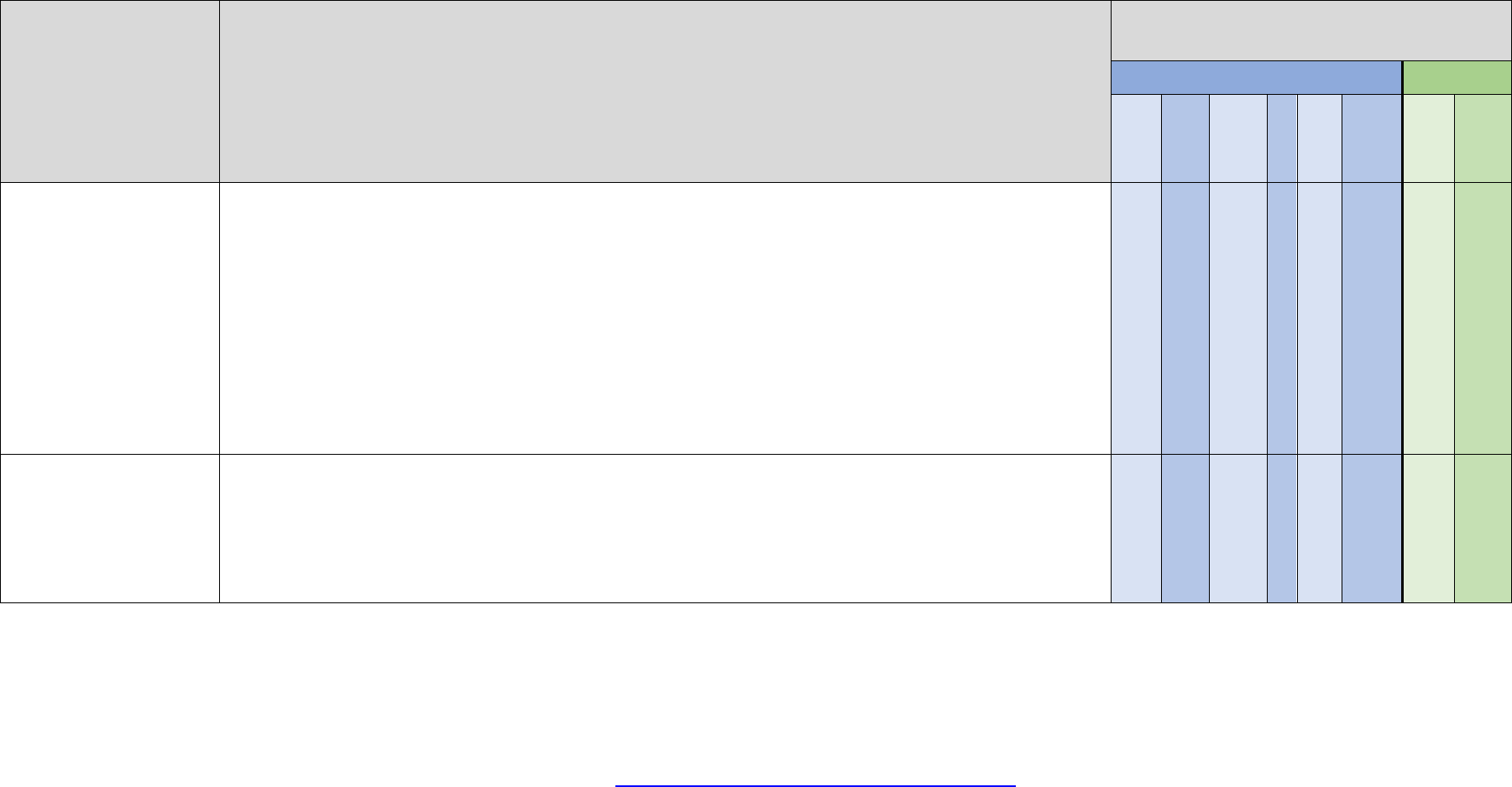
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 255
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Vyndaqel
Coverage requires the following:
1. Diagnosis of transthyretin-mediated amyloidosis with cardiomyopathy (ATTR-CM) confirmed by BOTH of the
following:
a. A negative monoclonal light chain screen ruling out amyloid light chain cardiomyopathy
b. Technetium-labeled bone scintigraphy
2. Age > 18 years old
3. Documentation of clinical signs and symptoms of ATTR-CM
Vyndaqel will not be approved for use in combination with other therapies approved for transthyretin-mediated amyloidosis
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Vyzulta
Coverage requires the following:
1. Diagnosis of elevated intraocular pressure
2. Trial of all preferred medications (generic Xalatan, generic Lumigan, generic Travatan Z)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 256
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Wainua
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of peripheral nerve disease caused by hereditary transthyretin amyloidosis (hATTR; formerly known as familial
amyloidosis polyneuropathy or FAP) with documented TTR mutation
i. Signs and symptoms of ocular or cerebral area involvement (such as in ocular amyloidosis or
primary/leptomeningeal amyloidosis), if present, must not predominate over polyneuropathy symptomology
associated with hATTR
3. Documentation of clinical signs and symptoms of peripheral neuropathy (such as: tingling or increased pain in the hands,
feet and/or arms, loss of feeling in the hands and/or feet, numbness or tingling in the wrists, carpal tunnel syndrome, loss
of ability to sense temperature, difficulty with fine motor skills, weakness in the legs, difficulty walking)
AND/OR
3. Documentation of clinical signs and symptoms of autonomic neuropathy symptoms (such as: orthostasis, abnormal
sweating, dysautonomia [constipation and/or diarrhea, nausea, vomiting, anorexia, early satiety])
4. Must have a baseline FAP or Coutinho Stage 1 or 2
5. No prior liver transplant
6. Must not have New York Heart Association (NYHA) heart failure classification > 2
Wainua will not be used in combination with other therapies approved for transthyretin-mediated amyloidosis
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 257
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Wakix
Coverage requires a diagnosis of narcolepsy AND:
1. Age ≥ 18 years old
2. Cataplexy
OR
2. Excessive daytime sleepiness
3. Trial and failure, contraindication, or intolerance to at least one generic or preferred treatment such as methylphenidate or
dextroamphetamine, AND modafinil or armodafinil, AND Sunosi
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 258
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Wegovy
Coverage criteria is determined by group benefit and requires one of the following:
1. Age ≥ 18 years old
2. BMI ≥ 30, or ≥ 27 with one weight related comorbid condition
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active participation for a
minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food diaries, exercise logs, program
receipts, app participation, etc.) if member does not have access to a covered BCBSM/BCN program
5. Not to be used in combination with other weight loss products
6. Cannot be used in combination with other glucagon-like peptide-1(GLP-1) agonist containing products
OR
1. 12 to 17 years of age
2. BMI ≥ 95th percentile, standardized for age and sex
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active participation for a
minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food diaries, exercise logs, program
receipts, app participation, etc.) if member does not have access to a covered BCBSM/BCN program
5. Not to be used in combination with other weight loss products
6. Cannot be used in combination with other glucagon-like peptide-1(GLP-1) agonist containing products
Initial approval: 6 months
For adults, continued coverage will be reviewed annually and may be provided if the member has maintained at least a 5% weight loss from
baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30 days) and BMI ≥ 18.5kg/m2 must be
submitted to the plan for review. Wegovy cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products
For pediatrics, continued coverage will be reviewed annually and may be provided if the member has maintained at least a 1% reduction in BMI
from baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30 days) and BMI-for-age percentile ≥
5th percentile must be submitted to the plan for review. Wegovy cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist
containing products
OR
1. Age ≥ 18 years old
2. Body mass index (BMI) ≥ 35 kg/m2
3. Documentation of current (within 30 days) baseline weight
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 259
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Wegovy
(continued)
4. Documentation of active participation for a minimum of 6 months in a lifestyle modification program and documentation of current active
participation in Teladoc Health Weight Management Program** must be submitted to the plan
5. Must be prescribed by a PCP or provider who has an established relationship with the member that the member has seen in-person
6. Not to be used in combination with other weight loss products
7. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products
8. Will not be covered for members with Type 2 Diabetes Mellitus
OR
1. 12 to 17 years of age
2. BMI ≥ 95th percentile, standardized for age and sex
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active participation for a
minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food diaries, exercise logs, program
receipts, app participation, etc.) if member does not have access to a covered BCBSM/BCN program
5. Not to be used in combination with other weight loss products
6. Cannot be used in combination with other glucagon-like peptide-1(GLP-1) agonist containing products
Initial approval: 6 months
Continued coverage for adults may be provided if the member has maintained at least a 5% weight loss from baseline AND
1. Documentation of active participation for a minimum of 6 months in a lifestyle modification program and documentation of current active
participation in Teladoc Health Weight Management Program** must be submitted to the plan AND
2. Must be prescribed by a PCP or provider, with an established relationship with the member, that the member has seen in-person AND
3. Current weight (within 30 days) must be submitted to the plan for review AND
4. Patient's BMI was ≥ 35 kg/m2 prior to starting treatment, current BMI ≥ 18.5kg/m2 AND
5. Patient must have a proportion of days covered ≥ 80% AND
6. Not to be used in combination with other weight loss products AND
7. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products AND
8. Will not be covered for members with Type 2 Diabetes Mellitus
(criteria continued next page)
NC
NC
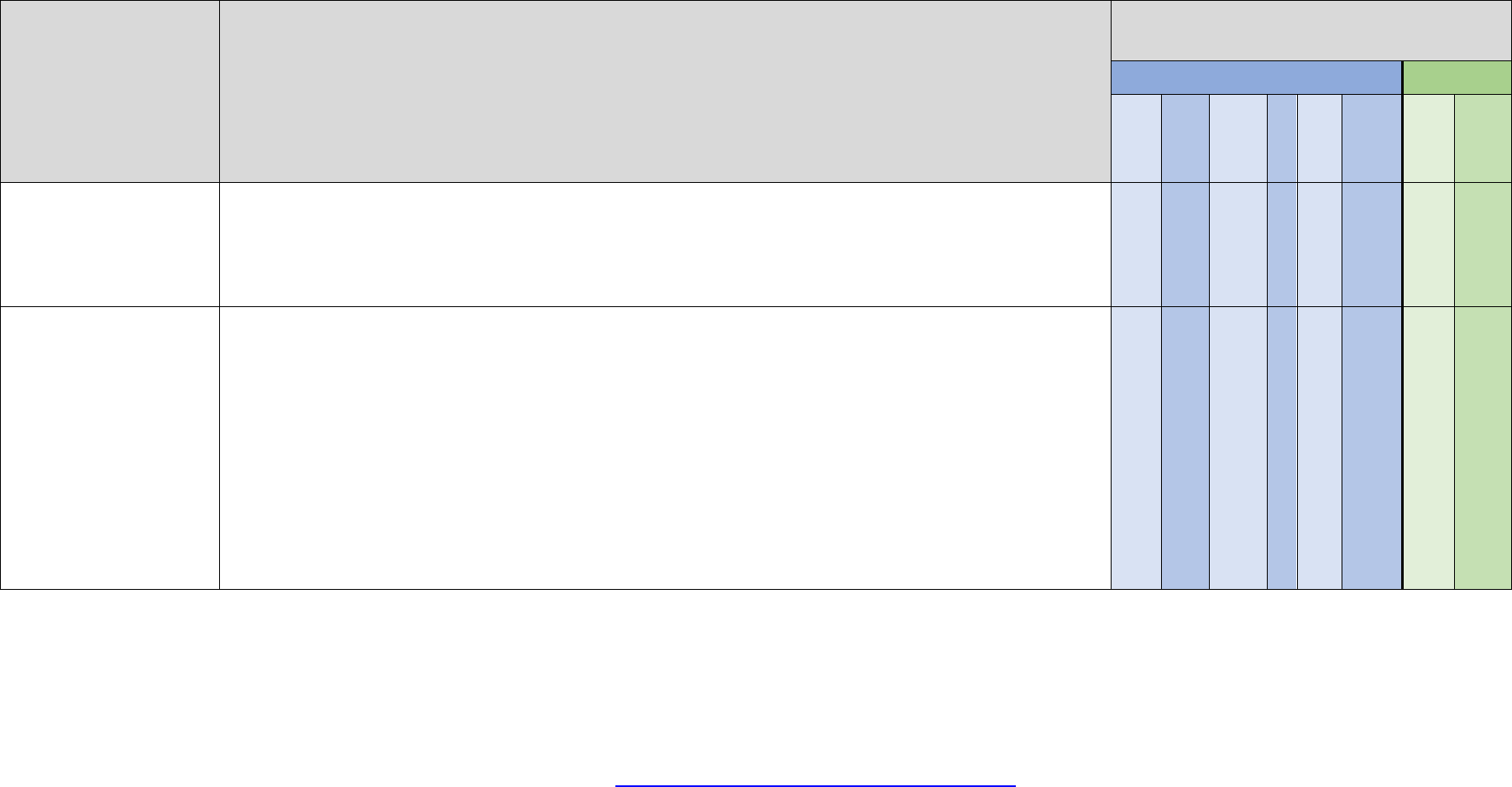
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 260
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Wegovy
(continued)
Continued coverage for pediatrics will be reviewed annually and may be provided if the member has maintained at least a 1% reduction in BMI
from baseline AND requires continued participation in a lifestyle modification program. Current weight (within 30 days) and BMI-for-age percentile ≥
5th percentile must be submitted to the plan for review. Wegovy cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist
containing products
**Proof of active engagement requires at a minimum: documentation that the member has met with a Teladoc weight management coach and the
member has a plan of action
NC
NC
Welireg
Coverage requires the following:
1. Age ≥ 18 years old
2. Treatment of von Hippel‐Lindau (VHL) disease requiring therapy for associated renal cell carcinoma (RCC), central
nervous system (CNS) hemangioblastomas, or pancreatic neuroendocrine tumors (pNET), not requiring immediate
surgery
OR
1. Diagnosis of advanced renal cell carcinoma (RCC)
2. Age ≥ 18 years old
3. Previously treated with a programmed death receptor-1 (PD-1) or programmed death-ligand 1 (PD-L1) inhibitor and a
vascular endothelial growth factor tyrosine kinase inhibitor (VEGF-TKI)
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 261
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Winlevi
Coverage requires the following:
1. Treatment of acne
2. Age ≥ 12 years old
3. Trial and failure contraindication, or intolerance to one oral agent (examples include: generic Monodox, generic
Vibramycin, generic Minocin, generic Bactrim, or generic Aldactone)
4. Trial and failure contraindication, or intolerance to three topical agents (examples include: generic Benzaclin,
generic Benzamycin, generic Retin-A, or generic Differin cream/gel)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Winrevair
Coverage requires the following:
1. For the treatment of pulmonary arterial hypertension (PAH, WHO Group 1) to increase exercise capacity, improve
WHO functional class (FC) and reduce the risk of clinical worsening events
2. Age ≥ 18 years old
3. Trial and failure, intolerance, or contraindication to ALL of the following:
a. Generic sildenafil or tadalafil
AND
b. A generic or preferred endothelin receptor antagonist (ERA)
4. The member will self-administer Winrevair unless clinically unable to do so
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 262
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xalkori
Coverage requires the following:
1. Diagnosis of metastatic non-small cell lung cancer (NSCLC) whose tumors are anaplastic lymphoma kinase (ALK)
or ROS1-positive as detected by an FDA-approved test
OR
1. Diagnosis of relapsed or refractory, systemic anaplastic large cell lymphoma (ALCL) that is ALK-positive in
pediatric patients 1 year of age and older and young adults
OR
1. Diagnosis of unresectable, recurrent, or refractory inflammatory myofibroblastic tumor (IMT) that is ALK-positive
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Xcopri
Coverage requires the following:
1. Treatment of seizures in patients with epilepsy
2. Treatment failure or intolerance to at least 3 generic alternatives for the treatment of seizures
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Xdemvy
Coverage requires the following:
1. Diagnosis of Demodex blepharitis confirmed via the presence of collarettes upon examination with a slit lamp
2. Age ≥ 18 years old
Approval: 60 days

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 263
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xeljanz tablet
Coverage requires the following:
1. Diagnosis of Rheumatoid Arthritis
2. Age > 18 years old
3. Trial and failure of one Disease-Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial (examples
include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Psoriatic Arthritis
2. Age > 18 years old
3. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Ulcerative Colitis
2. Age > 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Polyarticular Juvenile Idiopathic Arthritis (JIA)
2. Age ≥ 2 years old
3. Trial and treatment failure of one Disease-Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, leflunomide)
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 264
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xeljanz tablet
(continued)
OR
1. Diagnosis of ankylosing spondylitis
2. Age ≥ 18 years old
3. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Xeljanz solution
Coverage requires the following:
1. Diagnosis of Polyarticular Juvenile Idiopathic Arthritis (JIA)
2. Age ≥ 2 years old
3. Trial and treatment failure to one Disease-Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial
(examples include methotrexate, leflunomide)
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 265
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xeljanz
XR
Coverage requires the following:
1. Diagnosis of Rheumatoid Arthritis
2. Age > 18 years old
3. Trial and failure of one Disease-Modifying Anti-Rheumatic Drug (DMARD) after a minimum 3-month trial (examples
include methotrexate, hydroxychloroquine, leflunomide, sulfasalazine)
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Psoriatic Arthritis
2. Age > 18 years old
3. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of Ulcerative Colitis
2. Age > 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
4. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
OR
1. Diagnosis of ankylosing spondylitis
2. Age ≥ 18 years old
3. Trial and treatment failure of one or more tumor necrosis factor (TNF) inhibitor(s)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 266
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xelpros
Coverage requires the following:
1. Treatment of elevated intraocular pressure
2. Trial and treatment failure of two preferred medications such as generic Xalatan, Lumigan or Travatan Z
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Xelstrym
Coverage requires the following:
1. Diagnosis of Attention Deficit Hyperactivity Disorder
2. Age ≥ 6 years old
3. Treatment failure or intolerance to both a generic methylphenidate and a generic amphetamine product, one of
which must be a long-acting formulation
OR
3. Member cannot swallow tablets/capsules and has tried and failed one of the agents that can be opened and
sprinkled on applesauce (methylphenidate ER, Adderall XR)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Xembify
Requires appropriate diagnosis for coverage, subcutaneous administration and other criteria may apply depending on
diagnosis. Dosing must be based on ideal body weight (IBW) unless the patient's BMI is greater than 30. If the patient’s BMI
is greater than 30 or if actual body weight is 20-30% greater than IBW, adjusted body weight must be used.
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 267
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xepi
Coverage requires the following:
1. Diagnosis of impetigo
2. Trial of generic Bactroban
Approval: 60 days
NC
NC
Xermelo
Coverage requires the following:
1. Diagnosis of carcinoid syndrome diarrhea
2. Age ≥ 18 years’ old
3. Trial and treatment failure of somatostatin analog (SSA) (octreotide, lanreotide)
4. Using in combination with SSA
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 268
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xifaxan 550mg
Coverage requires the following:
1. Diagnosis of irritable bowel syndrome with diarrhea (IBS-D)
2. Trial and treatment failure, contraindication, or intolerance to a tricyclic antidepressant
OR
1. Diagnosis of small intestinal bacterial overgrowth (SIBO) as detected by an appropriate breath test
2. Trial and failure of TWO generic antibiotics
OR
1. Diagnosis of intestinal methanogen overgrowth (IMO) as detected by an appropriate breath test
2. Using in combination with neomycin unless contraindicated
Initial approval for IBS-D and SIBO: 60 days
IBS-D and SIBO/IMO renewal: requires the presence of recurrent symptoms after the completion of the prior course of
treatment (maximum of 2 renewals will be provided in accordance with FDA label for IBS-D)
OR
1. Diagnosis of hepatic encephalopathy (HE)
2. Trial and failure of lactulose
Initial approval for HE: 1 year
HE renewal: requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 269
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xolair
Coverage requires the following:
1. Diagnosis of uncontrolled moderate to severe allergic asthma
2. Age ≥ 6 years old
3. Positive skin test or in-vitro reactivity to a perennial aeroallergen
4. Failure to maintain adequate control after at least a 3 month trial of daily oral corticosteroids or high dose inhaled
corticosteroids in combination with:
a. LABA (long acting inhaled β2 agonist)
OR
b. Leukotriene modifier
OR
c. LAMA (long acting muscarininc antagonist) in adults and children ≥ 12 years old
5. IgE level > 30 but < 700 IU/ml for patients 12 years of age and older
OR
5. IgE level > 30 but < 1300 IU/ml for patients between the ages of 6 to < 12 years old
6. Cannot be used in combination with other biologic agents indicated for asthma
7. For self-administration of Xolair prefilled syringe: the patient has received the first 3 doses under the guidance of a
health care provider
OR
1. Diagnosis of chronic idiopathic urticaria
2. Documentation of diagnosis per the American Academy of Allergy Asthma and Immunology (AAAI) guidelines:
a. Must have occurrence of almost daily hives and itching for at least 6 weeks
3. Age ≥ 12 years old
(criteria continued next page)

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 270
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Xolair
(continued)
4. Past trial and failure all of the following for at least 2 months:
a. Trial and failure of a second-generation antihistamine at the maximal tolerated dose for at least 2 months
b. Trial and failure one of the following at maximal dosing:
i. Another second-generation antihistamine
ii. H2 antagonist
iii. Leukotriene receptor antagonist
iv. First generation antihistamine given at bedtime
v. Hydroxyzine
vi. Doxepin
5. Other diagnoses have been ruled out
6. Cannot be used in combination with other biologic agents indicated for chronic idiopathic urticaria
7. For self-administration of Xolair prefilled syringe: the patient has received the first 3 doses under the guidance of a health
care provider
OR
1. Diagnosis of nasal polyps
2. Age ≥ 18 years old
3. Patient is currently receiving and will continue to receive standard of care regimen
4. Inadequate response to treatment with intranasal corticosteroids
5. Baseline serum total IgE level of 30 IU/mL to 1,500 IU/mL prior to initiating treatment with Xolair
6. Cannot be used in combination with other biologic agents indicated for nasal polyps
7. For self-administration of Xolair prefilled syringe: the patient has received the first 3 doses under the guidance of a health
care provider
OR
1. Diagnosis of IgE-mediated food allergy
2. Age ≥ 1 year old
3. Clinical history of allergic reaction following consumption of at least one of the following: peanuts, milk, eggs, wheat,
cashews, hazelnuts, and walnuts
4. Confirmed diagnosis of an allergy to either peanuts, milk, eggs, wheat, cashews, hazelnuts, or walnuts confirmed by one
of the following:
a. IgE specific antibodies greater than or equal to 6 kUA/L
b. Food-specific skin prick test (SPT)
5. Provider attestation that the member will be on an allergen avoidant diet while on Xolair therapy
6. Must have a current prescription for epinephrine and access to an epinephrine autoinjector while using Xolair
7. Serum total IgE level greater than 30 but less than or equal to 1850 IU/mL
8. Must not be used in combination with any other food allergy desensitization therapy
9. Cannot be used in combination with other biologic agents indicated for any of the conditions listed in the policy and other
targeted DMARDs
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 271
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xolremdi
Coverage requires the following:
1. Age ≥ 12 years old
2. Diagnosis of WHIM (warts, hypogammaglobulinemia, infections, and myelokathexis) syndrome
3. Clinical diagnosis of WHIM syndrome with confirmed CXCR4 mutation
4. ANC < 400 cells/μL or total WBC count ≤400 cells/μL if ANC below lower limit of detection
Initial approval: 1 year
Renewal requires that current criteria are met and that the medication is providing clinical benefit
Xospata
Coverage requires the following:
Treatment of relapsed or refractory acute myeloid leukemia (AML) in adult patients with an FMS-like tyrosine kinase 3
(FLT3) mutation as detected by an approved test
Xphozah
Coverage requires the following:
1. Age ≥ 18 years old
2. For the reduction of serum phosphorus for the diagnosis of chronic kidney disease (CKD) on dialysis
3. Using as add on therapy for those with inadequate response to phosphate binders or intolerance of any dose of
phosphate binder therapy
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
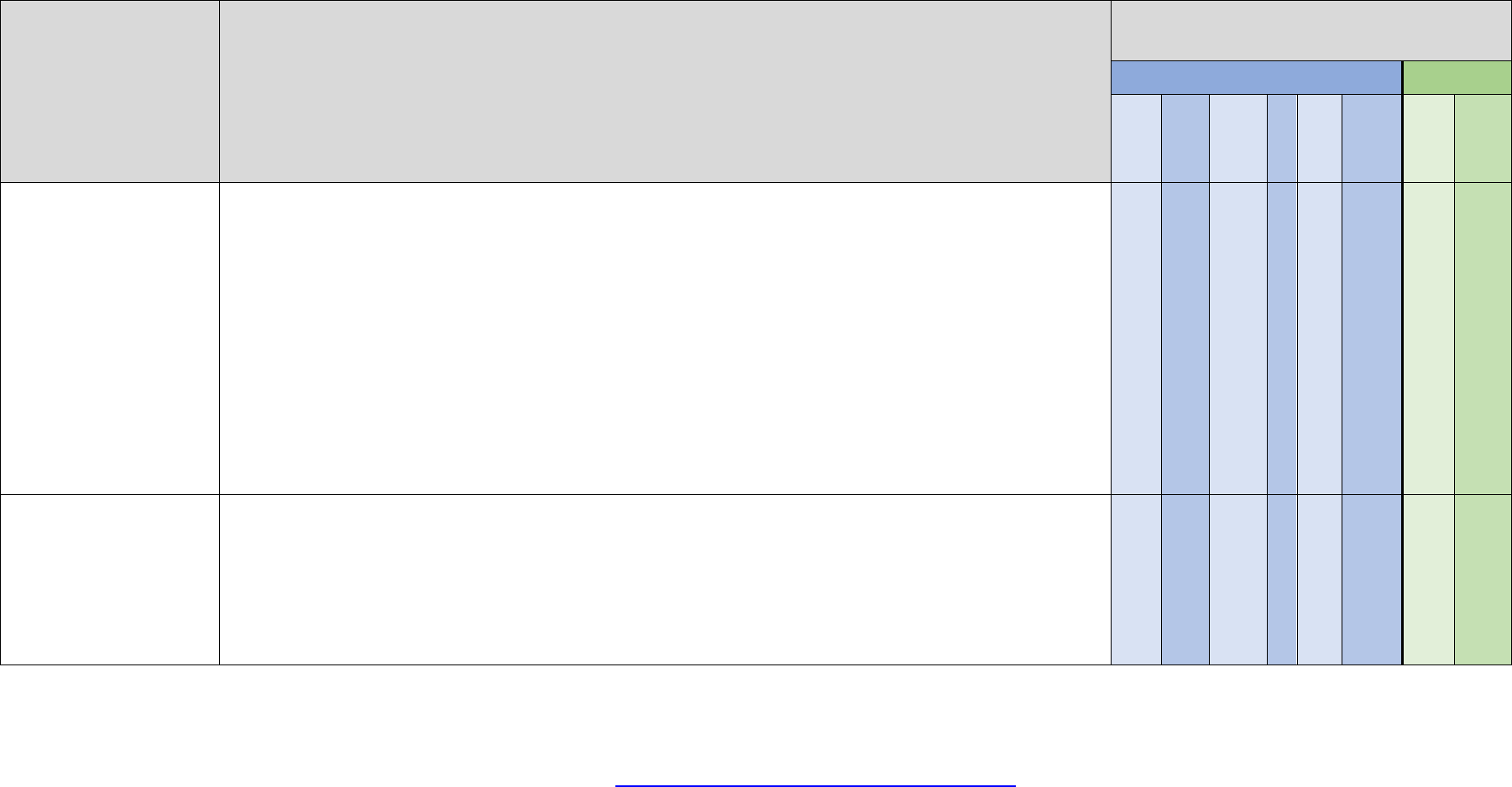
Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 272
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xpovio
Coverage requires the following
1. Treatment of relapsed or refractory multiple myeloma
2. Used in combination with dexamethasone
3. Received ≥4 prior therapies and whose disease is refractory to ≥2 proteasome inhibitors, ≥2 immunomodulatory
agents, and an anti-CD38 monoclonal antibody;
OR
1. Treatment of relapsed or refactory diffuse large B-cell lymphoma
2. Recieved at least 2 prior systemic therapies
OR
1. Treatment of multiple myeloma
2. Used in combination with Velcade (bortezomib) and dexamethasone
3. Received at least one prior therapy
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Xtampza ER
Coverage requires the following:
1. Diagnosis of moderate to severe chronic pain requiring around the clock opioid analgesia for an extended period of
time
Initial appoval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Note: Coverage will not be provided if the patient is on more than one long acting opioid concurrently

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 273
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xtandi
Coverage requires the following:
1. Treatment of castration-resistant prostate cancer
OR
1. Treatment of metastatic castration-sensitive prostate cancer
OR
1. Treatment of non-metastatic castration-sensitive prostate cancer with biochemical recurrence at high risk for
metastasis
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Xuriden
Coverage requires the following:
1. Diagnosis of Hereditary Orotic Aciduria
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Xyosted
Coverage requires the following:
1. Diagnosis of male hypogonadism
2. Two signs and symptoms specific to testosterone deficiency
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 274
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Xywav
Coverage requires the following:
1. Age ≥ 7 years old
2. Diagnosis of narcolepsy and cataplexy
3. For adults only - Trial and failure, contraindication, or intolerance to Wakix
OR
1. Diagnosis of narcolepsy and excessive daytime sleepiness
2. Trial and failure, contraindication, or intolerance to at least one generic or preferred treatment such as
methylphenidate or dextroamphetamine
3. For adults only - Trial and failure, contraindication, or intolerance to modafinil or armodafinil, AND Sunosi, AND
Wakix
OR
1. Age ≥ 18 years old
2. Diagnosis of idiopathic hypersomnia
3. Trial and failure, contraindication, or intolerance to at least one generic or preferred treatment such as
methylphenidate or dextroamphetamine
4. For adults only - Trial and failure, contraindication, or intolerance to modafinil or armodafinil
Xywav will not be approved if patient is being treated with sedative hypnotic agents, other central nervous system (CNS)
depressants or using alcohol
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 275
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zavzpret
Coverage requires the following:
1. For acute treatment of migraine
2. Age ≥ 18 years old
3. Trial and treatment failure, contraindication, or intolerance to 2 generic triptan medications, one of which must be a
generic intranasal triptan
4. Trial and treatment failure, contraindication, or intolerance to to Ubrelvy and Nurtec ODT
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Zejula
Coverage requires the treatment of FDA approved indications
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression
Zelboraf
Coverage requires the following:
1. Diagnosis of unresectable or metastatic melanoma with BRAF V600E mutation
OR
2. Diagnosis of Erdheim-Chester Disease with BRAF V600 mutation
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 276
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zembrace
SymTouch
Coverage requires the following:
Trial and failure of generic Imitrex (sumatriptan) injection and one other generic triptan (examples include: generic Maxalt
(rizatriptan), generic Amerge (naratriptan), generic Zomig/ZMT(zolmitriptan))
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Zepatier
Coverage requires the following:
1. Age ≥ 12 years old or weight ≥ 30 kilograms
2. Diagnosis of Chronic Hepatitis C genotype 1 or 4
3. For genotype 1a patients, test results for NS5a resistance-associated polymorphisms
4. If treatment experienced, documentation of previous treatment experience for Hepatitis C
5. If cirrhosis is present: documentation of decompensated or compensated cirrhosis
Drug will be reviewed based on a case by case basis utilizing AASLD guidelines and FDA approved package labeling

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 277
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zepbound
Coverage criteria is determined by group benefit and requires one of the following:
1. Age ≥ 18 years old
2. BMI ≥ 30, or ≥ 27 with one weight related comorbid condition
3. Current weight (within 30 days) must be submitted to the plan for review
4. Active participation for a minimum of 6 months in a covered BCBSM/BCN lifestyle modification program OR active participation for a
minimum of 6 months in an alternative concurrent lifestyle modification program (e.g. recent food diaries, exercise logs, program
receipts, app participation, etc.) if member does not have access to a covered BCBSM/BCN program
5. Not to be used in combination with other weight loss products
6. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products
Initial approval: 6 months
Continued coverage will be reviewed annually and may be provided if the member has maintained at least a 5% weight loss from baseline AND
requires continued participation in a lifestyle modification program. Current weight (within 30 days) and BMI ≥ 18.5kg/m2 must be submitted to the
plan for review. Zepbound cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products
OR
1. Age ≥ 18 years old
2. Body mass index (BMI) ≥ 35 kg/m2
3. Documentation of current (within 30 days) baseline weight
4. Documentation of active participation for a minimum of 6 months in a lifestyle modification program and documentation of current active
participation in Teladoc Health Weight Management Program** must be submitted to the plan
5. Must be prescribed by a PCP or provider who has an established relationship with the member that the member has seen in-person
6. Not to be used in combination with other weight loss products
7. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products
8. Will not be covered for members with Type 2 Diabetes Mellitus
(criteria continued next page)
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 278
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zepbound
(continued)
Initial approval: 6 months
Continued coverage may be provided if the member has maintained at least a 5% weight loss from baseline AND
1. Documentation of active participation for a minimum of 6 months in a lifestyle modification program and documentation of current active
participation in Teladoc Health Weight Management Program** must be submitted to the plan AND
2. Must be prescribed by a PCP or provider, with an established relationship with the member, that the member has seen in-person AND
3. Current weight (within 30 days) must be submitted to the plan for review AND
4. Patient's BMI was ≥ 35 kg/m2 prior to starting treatment, current BMI ≥ 18.5kg/m2 AND
5. Patient must have a proportion of days covered ≥ 80% AND
6. Not to be used in combination with other weight loss products AND
7. Cannot be used in combination with other glucagon-like peptide-1 (GLP-1) agonist containing products AND
8. Will not be covered for members with Type 2 Diabetes Mellitus
**Proof of active engagement requires at a minimum: documentation that the member has met with a Teladoc weight management coach and the
member has a plan of action
NC
NC
Zeposia
Coverage requires the following:
1. Diagnosis of ulcerative colitis
2. Age ≥ 18 years old
3. Treatment with an adequate course of conventional therapy (such as steroids for 7 days, immunomodulators such
as azathioprine for at least 2 months) has been ineffective or is contraindicated or not tolerated
4. Trial and treatment failure of two of the following: Humira, Simponi, Stelara, Xeljanz/XR, or Rinvoq
OR
1. Diagnosis of multiple sclerosis
2. Age ≥ 18 years old
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 279
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zetonna
Coverage requires trial and failure or intolerance of 2 of the following intranasal steroids:
1. Generic fluticasone (Flonase)
2. Generic flunisolide (Nasalide)
3. Nasacort (over-the-counter)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
NC

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 280
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zilbrysq
Coverage requires the following:
1. Diagnosis of generalized myasthenia gravis (gMG)
2. Age ≥ 18 years old
3. Documented anti-acetylcholine receptor (AChR) antibody positive myasthenia gravis (MG) identified by:
a. Lab record or chart notes identifying the patient is positive for anti-AChR antibodies
AND
b. One of the following confirmatory tests:
i. Positive edrophonium test
ii. History of clinical response to oral cholinesterase inhibitors (for example: pyridostigmine)
iii. Electrophysiological evidence of abnormal neuromuscular transmission by repetitive nerve
stimulation (RNS) or single-fiber electromyography (SFEMG)
4. Patients must NOT have a history of:
a. Thymectomy within 12 months
b. Current thymoma
c. Other neoplasms of the thymus
5. Previous treatment courses of at least 12 weeks with one of the following standards of care have been ineffective:
methotrexate, azathioprine, cyclophosphamide, cyclosporine, mycophenolate mofetil, or tacrolimus unless all are
contraindicated or not tolerated
6. Patient is currently receiving, and will continue to receive, a stable standard of care regimen
7. Must not be used with other biologic therapies for myasthenia gravis or immunoglobulin therapy
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 281
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zokinvy
Coverage requires the following:
1. Age ≥ 1 year old
2. Body surface area (BSA) ≥ 0.39 m
2
3. The requested dose is appropriate for the patient’s current body surface area (BSA)
4. Diagnosis of Hutchinson-Gilford Progeria Syndrome (HGPS) confirmed by a mutation in the LMNA gene
OR
4. Diagnosis of processing-deficient Progeroid Laminopathies with one of the following:
i. Heterozygous LMNA gene mutation with progerin-like protein accumulation
OR
1. Homozygous or compound heterozygous ZMPSTE24 gene mutations
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Zolinza
Coverage is provided for the treatment of the FDA approved indications
zolmitriptan nasal
spray
(Zomig)
Coverage requires the following:
1. Trial and treatment failure or intolerance to two generic triptans (generic Imitrex, generic Maxalt, generic Amerge or
generic Zomig/ZMT tablets)
OR
1. Age 12-17 years old
2. Trial and treatment failure or intolerance to generic Maxalt (rizatriptan)
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 282
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
zolpidem tartrate
sublingual
(Intermezzo)
Coverage requires treatment failure of 3 of the following: immediate-release zolpidem (Ambien), eszopiclone (Lunesta),
zaleplon (Sonata), trazodone (Desyrel), or doxepin (Silenor)
Coverage will not be approved for combination therapy with other sedative hypnotics
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
NC
NC
Zonisade
Coverage requires the following:
1. Treatment of seizure disorder/epilepsy
2. Age ≥ 16 years old
3. Trial of 3 generic alternatives, one of which must be generic Zonegran (zonisamide) capsules
OR
3. Member is unable to swallow tablets or capsules
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 283
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zoryve cream
Coverage requires the following:
1. Diagnosis of plaque psoriasis
2. Age ≥ 6 years old
3. Trial and failure, contraindication, or intolerance to a generic medium or high potency topical corticosteroid
4. Trial and failure, contraindication, or intolerance to at least one of the following generic topical steroid-sparing
agents: calcipotriene, tazarotene, tacrolimus, or pimecrolimus
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Zoryve foam
Coverage requires the following:
1. Diagnosis of seborrheic dermatitis
2. Age ≥ 9 years old
3. Trial and failure, contraindication, or intolerance to at least two of the following generic or preferred agents: topical
antifungal, topical corticosteroids, or topical calcineurin inhibitors
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 284
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Ztalmy
Coverage requires the following:
1. Diagnosis of seizures associated with cyclin‐dependent kinase‐like 5 (CDKL5) deficiency disorder
2. CDKL5 deficiency disorder confirmed by genetic testing showing mutations on the CDKL5 gene
3. Age ≥ 2 years old
Initial approval: 1 year
Renewal requires that current criteria are met, and that the medication is providing clinical benefit
Zurzuvae
Coverage requires the following:
1. Age ≥ 18 years old
2. Diagnosis of postpartum depression (PPD) with an onset of depressive symptoms in the third trimester or
within 4 weeks postpartum
3. Patient is currently ≤ 12 months postpartum
4. Will be used in combination with or a recommendation will be given for psychotherapy
Approval: 60 days
Zydelig
Coverage requires the following:
1. Relapsed chronic lymphocytic leukemia (CLL), in combination with rituximab
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 285
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
Drug
name
Current Blue Cross and BCN
coverage criteria
Prior Authorization and Step Therapy
programs
Blue Cross
BCN
Custom
Drug List
Clinical
Drug List
Custom
Select
Drug List
Lite PA
Preferred
Therapy
Off-Label/
High-Cost
Specialty
Custom
Drug List
Custom
Select
Drug List
Zykadia
Coverage requires the following:
Diagnosis of anaplastic lymphoma kinase (ALK) positive, metastatic non-small cell lung cancer as detected by an FDA-
approved test
Initial approval: 1 year
Continuation of treatment requires a lack of disease progression

Blue Cross Blue Shield of Michigan
Blue Care Network
Prior Authorization and Step Therapy Coverage Criteria
March 2019
= Prior Approval/Step Therapy may apply Page 286
NC = Not Covered. You may be responsible for the full cost of the medication. Revised: 8-1-2024
* For drugs covered under the commercial Blue Cross or BCN medical benefit, please see the Blue Cross and BCN Utilization Management Medical Drug List.
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association.
