
October 2013
Patient Apps for
Improved Healthcare
From Novelty to Mainstream

Introduction
Apps have become ubiquitous in many aspects of our lives over the past ve years, fueled by the
widespread availability of tablet computers and smartphones. Tens of thousands of health, wellness,
and medical apps are now available for download to Apple or Android devices from online stores.
Harnessing the potential power of apps for healthcare has become a focal point of innovation,
in particular those apps which can be used by consumers or patients as part of their wellness,
prevention or treatment regimens.
While there is a great deal of interest in apps and enthusiasm for their use, they have yet to reach the
mainstream of healthcare provision, and indeed in many respects are still viewed as a novelty.
In this report, we share the results of a study we have undertaken to look more closely at the
consumer healthcare apps that are currently available, including an objective assessment of
their type, role, and functionality. We also look at the barriers to apps being more broadly and
systematically used by healthcare providers and patients or caregivers, and approaches that are
being taken to address these impediments.
The movement toward digital therapeutics is clear. Our intention is that this report provides some
objective and balanced perspective on how consumer apps can play a larger and more meaningful
role in the prevention and treatment of disease – resulting in improved health measures and
outcomes, and a more ecient healthcare system.
The study was undertaken independently by the IMS Institute for Healthcare Informatics as a public
service, without industry or government funding. The contribution of Carolyn Gauntlett to this report
is gratefully acknowledged.
Murray Aitken
Executive Director
IMS Institute for Healthcare Informatics
IMS Institute for Healthcare Informatics, 11 Waterview Boulevard, Parsippany, NJ 07054 USA
info@theimsinstitute.org www.theimsinstitute.org
Find out more
If you want to receive more reports
from the IMS Institute or be on our
mailing list please click here
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Find out more
Acknowledgements
The contributions to this report of Carolyn Gauntlett, John MacCarthy, Matthew Tindall,
Stephen Buck, Glenn Connery and many other colleagues at IMS Health are gratefully
acknowledged.
The authors would like to express sincere gratitude to people who have given their time
and expertise toward the development of this report. These individuals have participated
in interviews, roundtable discussions, chapter reviews and provided methodology
guidance.
Priyanka Agrawal, MD (University of California, San Francisco)
G. Caleb Alexander, MD, MS (Johns Hopkins Bloomberg School of Public Health)
Sameer Badlani, MD, FACP (University of Chicago Hospitals)
Jonathan Birnberg, MD (North Shore University Health System)
Philip Chan, PharmD (Pharmacist)
James Cunnar, MD (DuPage Family Medicine)
Michael Docktor, MD (Boston Children’s Hospital)
Israel Green-Hopkins, MD (Boston Children’s Hospital)
Alan Greene, MD, FAAP (Pediatrician)
James Homan, PharmD (St. Jude Children’s Research Hospital)
Cheng-Kai Kao, MD (University of Chicago)
Leslie Kernisan, MD, MPH (Geriatrician and caregiver educator)
Howard Landa, MD (Alameda Health System)
Elliot Levine, MD (Illinois Masonic Medical Center)
Creagh Milford, DO, MPH (Massachusetts General Physicians Organization)
Alisa Niksch, MD (Tufts University School of Medicine)
Kevin Patrick, MD, MS (University of California, San Diego)
Jordan Shlain, MD, FACP (HealthLoop Inc.)
Shannon Sims, MD, PhD (Rush University Medical Center)
Randall Staord, MD, PhD (Stanford University)
Lee Vermeulen, MS, RPh (University of Wisconsin Health)

Contents
EXECUTIVE SUMMARY
__________________________________________________
BACKGROUND
_________________________________________________________
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
_____________
ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
_______________________
CALL TO ACTION
_______________________________________________________
CONCLUSION
__________________________________________________________
METHODOLOGY
________________________________________________________
REFERENCES CITED
_____________________________________________________
ABOUT THE AUTHORS
___________________________________________________
ABOUT THE INSTITUTE
_________________________________________________
58
59
51
52
56
42
28
1
6
3
©2013 IMS Health Incorporated and its aliates. All reproduction rights, quotations, broadcasting, publications reserved. No part of this publication may be reproduced or
transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without express written
consent of IMS Health and the IMS Institute for Healthcare Informatics
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

1
Executive Summary
Little is currently understood about the diverse array of healthcare apps available to consumers,
their role in healthcare, the barriers to increasing their recommendation and support from
providers, and the requirements for mobile apps to move into the mainstream of healthcare.
This study includes the analysis of the 40,000+ healthcare apps available for download from the
U.S. Apple iTunes app store and an assessment of the potential value they provide throughout a
patient’s journey. This clearly demonstrates that to date most eorts in app development have
been in the overall wellness category, with diet and exercise apps accounting for the majority
available. Further an assessment of functionality of available apps nds that healthcare apps
available today have both limited and simple functionality - the majority do little more than
provide information.
There is a signicant skew in download volume for healthcare apps, with more than 50% of
available apps achieving fewer than 500 downloads. Conversely, 5 apps account for 15% of all
downloads in the healthcare category. The reason behind the limited downloads, and hurdles
to improved uptake, span all stakeholders. Patients currently face a dizzying array of healthcare
apps to choose from, with little guidance on quality or support from their doctors. Some eorts
are underway to help provide professional healthcare guidance in both the U.S. and the U.K.
but these are limited in scope and impact to date. Furthermore, apps developed to date do
not t well with the greatest areas of spend in healthcare – those patients facing multiple
chronic diseases and typically over the age of 65. These patients are likely to be among the top
healthcare spenders but smartphone penetration is lowest among this group, with only 18% of
the U.S. population using them, compared to 55% of those aged 45-54 years.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

2
EXECUTIVE SUMMARY
Physicians can see the potential benets of mobile healthcare apps but remain wary of formally
recommending apps to patients without evidence of their benet, clear professional guidelines regarding
their use in practice, and condence in the security of personal health information that may be generated
or transmitted by the app. Payers and employer wellness programs also want clear evidence of benet
before considering reimbursement or promoting the use of apps.
Over time, the app maturity model will see apps progress from being recommended on an ad hoc basis
by individual physicians, to systematic use in healthcare, and ultimately to an end goal of being a fully
integrated component of healthcare management. There are four key steps to move through on this
process: recognition by payers and providers of the role that apps can play in healthcare; security and
privacy guidelines and assurances being put in place between providers, patients and app developers;
systematic curation and evaluation of apps that can provide both physicians and patients with useful
summarized content about apps that can aid decision-making regarding their appropriate use; and
integration of apps with other aspects of patient care. Underpinning all of this will be the generation of
credible evidence of value derived from the use of apps that will demonstrate the nature and magnitude
of behavioral changes or improved health outcomes.
Meeting these preconditions will accelerate the movement of apps use from that of a novelty into the
mainstream of healthcare – and realizing their full potential in the years ahead.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

3
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
3
Background
Recent years have seen a gradual shift in the relative importance of dierent healthcare
stakeholders - between physician, payer and patient. Although the patient will never have the
tools to replace the roles of the physician and the payer, patients are encouraged to take a more
active interest in their overall wellbeing and understand the consequences of poor health in
later life. By having the patient aligned with the importance of wellness programs and sickness
prevention, health systems can hope to realize savings – especially from a lower burden of
multiple chronic conditions. As such, there are more frequent examples of healthcare payers
and/or governments pushing increasing responsibility for healthcare onto the patient, whether
that be by providing incentives to patients to stay healthy (eectively targeting preventive
measures) or for adhering to treatment regimes that are prescribed.
Figure 1: Evolution of Healthcare Stakeholders
In an attempt to rein in health care costs from chronic health conditions associated with
unhealthy behaviors, the Patient Protection and Aordable Care Act in the U.S. includes a
provision stating that beginning 2014 employers can use up to 30% of the total amount of an
employee’s health insurance premium to provide outcome based wellness incentives.
1
Bonuses
for health-related behavior in Europe are a key feature of private health insurance systems such
as in the U.K.
2
Recently in Dubai, local government ocials announced a 30-day challenge
(to coincide with Ramadan) in which it promised to pay participants a gram of gold for every
kilogram of weight lost.
3
Original Stakeholder: Physician
Previously Now Future
Key Stakeholder:
Payer now as important
as Physician
New Stakeholder:
Patient more involved in
healthcare decision making
and choices
In the past physicians were
key stakeholders acting as
gate keepers to healthcare
information and treatment
options
As the key budget holders,
payers have the most
inuence today over
healthcare treatments and
patterns and evaluation of
outcomes results
With the rise of the internet
and all its healthcare
information, patients are
better informed and enabled
to participate in the healthcare
decision making process
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
BACKGROUND
4
This push for the general population to have a higher awareness of - and be more involved in -
managing their health is occurring at the same time that technology is enabling the quick and
easy access of information. Websites such as WebMD, MDadvice, MedicineNet and NetDoctor all
oer patients medical advice and information for managing conditions. In 2013 the Pew Internet
and American Life Project released the latest Health Online survey which found that more than
half of all Americans have looked online for health information in the last year, and more than
one-third have used the internet to self-diagnose a condition.
4
The Global Observatory for eHealth (GOe) within the World Health Organization (WHO) denes
mobile health or mHealth as “medical and public health practice supported by mobile devices,
such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other
wireless devices”. mHealth involves the use of voice and short messaging service (SMS) as well
as more complex functionalities such as 3G systems, global positioning systems (GPS), and
Bluetooth technology.
5
The advent of smartphones has taken the potential for mHealth to a new level. The advanced
computing capability of smartphones that are typically optimized for internet usage means that
individuals can access information and advice from anywhere at any time. They also provide
functionality that is not available via a laptop such as the ability to capture information from sensors
on the move and the addition of GPS and camera functions. There are now estimated to be more
than 1 billion smartphones and tablets globally; some sources estimate that this will reach 2 billion
by 2014. In 2012 China overtook the U.S. to become the key smartphone market by volume, and
other key emerging economies are forecast to see strong growth rates for these devices too.
6
A mobile application (or mobile app) is a software application designed to run on smartphones,
tablet computers and other mobile devices. They are usually available through application
distribution platforms, which are typically operated by the owner of the mobile operating system,
such as the Apple App Store, Google Play (Android), Windows Phone Store, and BlackBerry App
World.
7
Across geographies the majority of smartphone users have more than 20 apps on their
device at present; in many cases this is closer to 30 apps.
8
Gaming apps and social media apps
such as Facebook remain the categories commanding most of users’ time.
9
Not all apps that have been developed in healthcare are widely available to consumers on their
mobile platform stores. Some of the most advanced medical apps are the 100 apps already
approved by the FDA and these are not necessarily designed to target general consumers.
Some apps have been designed for healthcare practitioners, others are for patients but require a
prescription, and others are intended for only a small subset of the population and hence are not
added to the general app stores.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
5
This report focuses only on the healthcare apps that are widely available to the general public
to aid in their everyday healthcare management in conjunction with their physician or other
healthcare professional. While apps are essentially without geographic boundaries, this report is
primarily focused on the use of apps in the context of the U.S. healthcare system. However, the
perspectives and considerations for more extensive use of apps are globally relevant.
BACKGROUND
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
6
Proling widely available
consumer healthcare apps
Development and use of healthcare related apps is growing rapidly but the current
level of functionality is limited and use is mostly for prevention and wellness
• Despite the large number of healthcare apps developed, the majority have only simple
functionality; however mobile apps can be used for remote monitoring providing potential for
extra data collection to aid healthcare management
• Almost 50% of healthcare apps available to consumers can be downloaded for free and are
produced by a variety of types of developer
• Apps are available across the full spectrum of the patient journey, although healthy living apps
dominate the space, whereas self-diagnosis, lling prescriptions and medication compliance
have the lowest numbers of apps developed to date
• Some apps cover the full patient journey and are therapy area specic or demographic specic
but there are still signicant areas of unmet need to be lled
With increasing interest in the use of mobile apps in healthcare, this study sought to undertake
the most comprehensive analysis of the 43,689 mobile healthcare apps available to the general
consumer through the English language U.S. iTunes store as of June 2013, assessing their
functionality, placement on the patient journey map and areas where unmet need still exists.
Every app categorised under “health and tness” or “medical” was reviewed. In seeking to focus
on apps that are purely related to patient health and treatment, examination of the content of
these apps led to the exclusion of 20,007 apps from further analysis since these were considered
not truly related to healthcare (e.g. salons, apps which use gimmicks with no real health benets)
(see Figure 2). Of the remaining 23,682 apps considered genuine healthcare apps, further content
analysis categorized 7,407 apps as healthcare professional (HCP) oriented, and the remaining
16,275 apps as consumer/patient oriented (see Figure 3). A full functionality analysis was
conducted on each of the apps targeting consumers/patients.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

7
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
7
Figure 2: App count methodology
Figure 3: Distribution of healthcare apps
43,689 “Healthcare and Fitness” or “Medical”
23,682 Apps genuine healthcare related
20,007 Mis-categorized or only
loosely healthcare related on App Store
• Fashion and beauty (e.g. salons)
• Apps intended for members of specic
clubs/universities
• Veterinary apps
• Apps which use gimmicks with no real health
benet (eg apps which make the user sound sick,
or demonstrate how the user would look if they
were obese)
• Apps related to health issues but which do not
focus on health (e.g. fertility)
• Product presentation apps for use by sales
reps/retailers
• Apps believed to have meaningless claims
e.g. “gives you a beautiful way to keep track of your
body's biorhythms”
Source: IMS Health analysis of widely available healthcare apps
16,275
Consumer
7407
HCP
Apple Store - Number of apps by customer
• IMS Analysis on all apps present in
App Store to June 2013 showed 23,682 apps
in the apple store related to healthcare
• More than 2/3 related to consumer
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
8
Assessment of app functionality
Although the number of healthcare apps is large and growing, there is signicant variation in
capabilities of the current apps, with most having only simple functionalities built into them.
An analysis of healthcare apps available to consumers through the iTunes app store resulted in
categorization of apps based on whether they could:
• Inform: Provide information in a variety of formats (text, photo, video)
• Instruct: Provide instructions to the user
• Record: Capture user entered data
• Display: Graphically display user entered data/output user entered data
• Guide: Provide guidance based on user entered information, and may further oer a
diagnosis, or recommend a consultation with a physician/a course of treatment
• Remind/Alert: Provide reminders to the user
• Communicate: Provide communication with HCP/patients and/or provide links
to social networks
It should be noted that there are mobile medical apps which are not available directly to the
public through the iTunes app store, including some of the mobile medical apps that have been
approved by the FDA, such as the BlueStar app from WellDoc which requires a prescription.
These apps do have signicant functionality components but as they are not available to the
general browsing public they are excluded from the functionality analysis below.
The most common capability of widely available consumer healthcare apps is the ability to
provide information - 10,840 consumer apps have this feature, or approximately 2/3 of all
consumer targeted apps. Fewer apps have other functionalities, for example, 5,823 can provide
instructions, 5,095 capture data entered by the user and 1,357 apps have a remind/alert function
built into them. About 10% of the consumer healthcare apps reviewed, 1,622 apps, have none
of these capabilities at all, and include apps such as those to help with relaxation and sleep,
and baby monitors. Although there is a subset of apps with impressive functionality (e.g.
electrocardiogram (ECG) readers, blood pressure monitors, blood glucose monitors) it is clear
that most of the healthcare apps available today are only simple in design and do little more than
provide information. This is echoed by an assessment of multi-functionality: although two-thirds
of healthcare apps can display information, only half of these can also provide instructions, and
only one-fth could track or capture user entered data (see Figure 4).
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
9
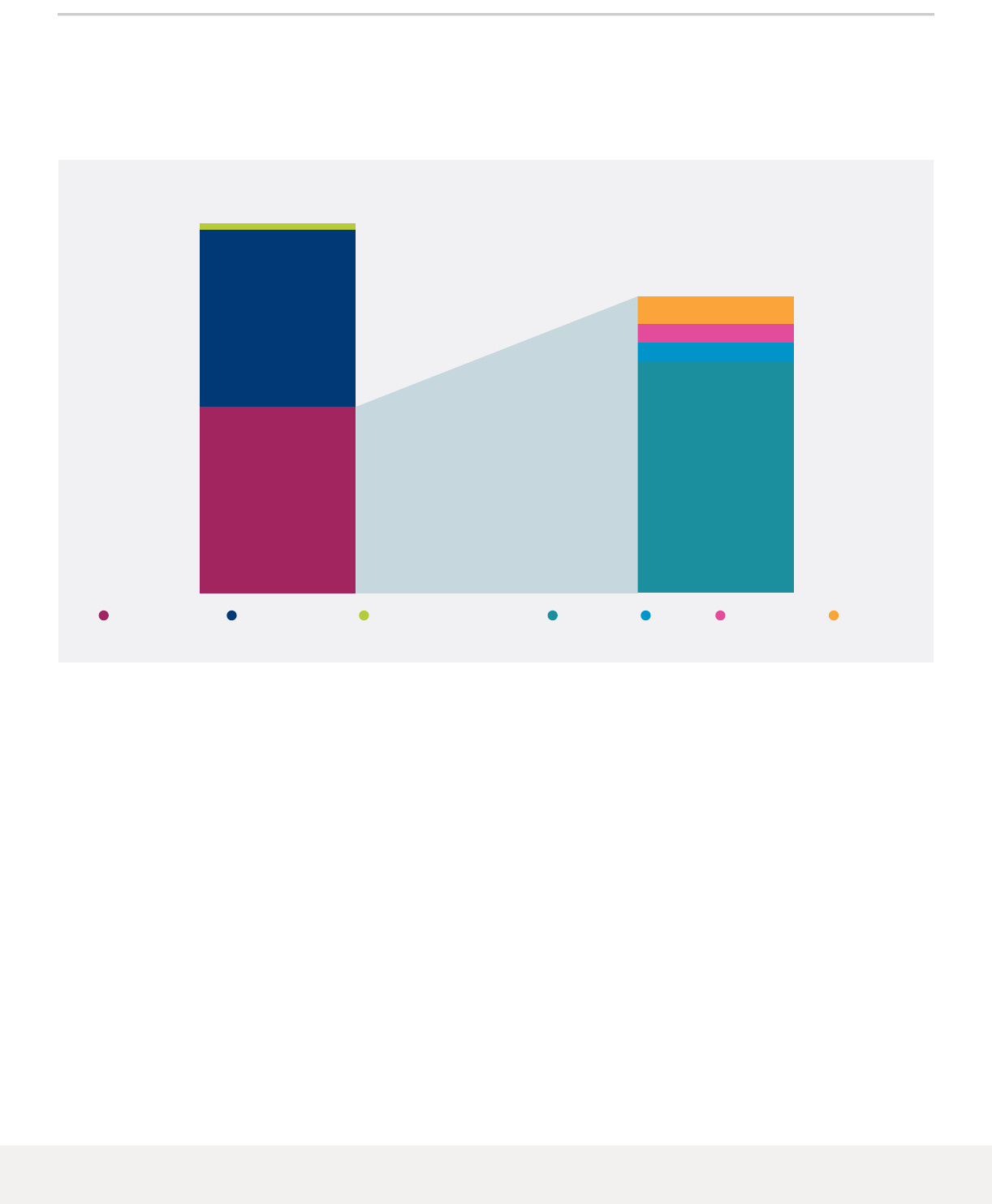
Figure 4: Assessment of consumer healthcare app functionality
Some mobile apps enable the remote monitoring of vitals that can be communicated back to the
healthcare practices. This oers the potential to enhance the value of provided care by taking
advantage of this patient reported data and embedding it into the clinical care plan:
if patients are regularly collecting health data they can, in consultation with their physician/nurse
practitioner, use that information to modify their behavior and better manage their condition.
As such, healthcare apps have the potential to bring eciencies into healthcare systems by
reducing the frequency and cost of direct interventions by healthcare professionals with patients.
Monitoring of vitals can be done remotely, and communication with healthcare professionals
– including pharmacists, physicians and nurse practitioners – can be done without the patient
having to physically meet with them.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Source: IMS Health analysis of widely available consumer targeted healthcare apps
Information Inform + Instruct
Information Inform + Record
Inform
10,000
5,000
0
10,000
5,000
0
Instruct
Record
Display
Guide
Remind/alert
Communicate
Number of apps Number of consumer apps
Individual Functionality Multi-Functionality
Less than ½ of apps
which provide
information also
provide instructions
Approx ⅕ apps which
provide information
also track/capture
user data
10,840
4,697
2,249
10,840
5,823
5,095
2,302
1,434
1,357
395
10,840
Patient uses app to
collect health data either
by choice or on physician
recommendation
Patient can transmit
data to physician or take
phone along to appt to
show physician
Patient and physician
together evaluate
the data
Necessary interventions
made: behavioral or
medication changes
Collect data Share data Evaluate data Intervene
10

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
10
Analysis of the widely available consumer healthcare apps on the iTunes app store shows that at
present there are 159 apps which link to sensors. However these are dominated by tness and
weight apps which monitor pulse rates when exercising and measure weight and body mass
index (BMI). Fewer than 50 of these 159 apps relate to actual condition management or provide
tools and calculators for users to measure their vitals. There is therefore considerable room for
growth in this sector.
IMS Health functionality scoring system
The IMS Health score for app functionality considers the results of 25 individual criteria assessed
during the app review process. These criteria include, but are not limited to, the type and
quantity of information provided by the app, how the app tracks or captures user data, the
communication processes utilized by the app, and the quantity of device capabilities included in
the app. In addition to looking at this result, weightings are applied specic to the category of the
app. For example, in a condition management app there will be a higher value placed on results
that focus on doctor communications than there would be for a reference app.
This scoring system was used for all consumer oriented healthcare apps with at least one
assessed level of functionality as dened in Figure 4, and conrmed that the majority of apps
have only simple functionality. This scoring system is based on our independent and objective
assessment of the app functionality and does not reect patient/user evaluation, physician
evaluation, or evidence that users benet from their use from an outcomes perspective.
The maximum score achievable is 100. As illustrated in Figure 5, the distribution of the 16,275
reviewed apps skews toward the low end of the 100 point scale, with more than 90% of the apps
receiving a score of 40 or less.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“I am really interested in feedback loops and how instant data can change behavior. I think apps
give an opportunity for patients to have instant access to themselves”
Jim Cunnar, MD – DuPage Family Medicine

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
11
Figure 5: IMS Health App functionality score distribution
In looking across all apps at their individual functionality score (each of which has a maximum
score of 100), the highest average scores accompanied the most prolic functionalities:
information and instructions (see Figure 6). Despite the thousands of apps with these
functionalities, few scored an excellent on this rating; instead average scores were only 40 out of
a possible 100. This reects the level of complexity of the app: the information score was assessed
based on whether the app provided text, photo and video formats, and how the level of detail
ranged from oering tips to detailed references. Therefore even though two-thirds of apps oer
some form of information, for the majority this is simple content in a simple format. There are,
however, signicant scoring dierences depending on the designed purpose of the app. Overall,
when considering all 16,000+ apps, reminder functions only achieved an average score of 5 out
of 100; however this varied dramatically. Those apps which are designed specically as reminders
to aid medication compliance and have a narrow purpose in this arena, saw scores reach as high
as 100 for this marker.
Functionality score
<50 6-10 16-20 26-30 46-50 56-60 61-65 65-70 71-75 76-80 86-90 91-9581-85 96-10011-15 21-25 31-35 36-40 31-45 51-55
3,000
2,500
1,500
0
2,000
1,000
500
Number of apps
Source: IMS Health analysis of widely available consumer targeted healthcare apps
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
12
Figure 6: IMS Health App scores by type of functionality
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Reminders Tracking/Guidance
InstructionsCommunications
Phone functionality Information
All Apps with functional information
40
35
30
25
2
15
10
5
0
Source: IMS Health analysis of widely available consumer targeted healthcare apps
One of the most advanced apps for condition management and remote monitoring,
approved by the FDA, is the WellDoc Diabetes Management software available through
the app store with partner AT&T. In the initial clinical trial of WellDoc (a 3 month non-
blinded randomized controlled trial of 30 T2D patients aged 18-70 years old) the
average decrease in A1c values for intervention patients was 2.03% compared to
0.68% (P<0.02, one-tailed) for control patients. Of the intervention patients 84% had
medications titrated or changed by their HCP compared to controls (23%, P = 0.002).
The WellDoc group also demonstrated improved self-care in diet, medication, and
exercise compared to that achieved by control patients receiving usual HCP care.
11
A key component
of the software is the Guided Compliance™ tool which directs patients to test their blood glucose
at optimal times to generate data for pattern analysis. The software also acts as a coaching tool
suggesting medication and lifestyle/self-management changes to patients (all suggested changes
are also communicated to the HCP). A follow-on trial consisted of a 12-month cluster-randomized
study with 163 participants. The trial demonstrated that the average decrease in A1c values for
intervention patients was 1.9% compared to 0.7% in the standard care control group (P<0.001). The
study therefore demonstrates that it is possible to improve treatment outcomes with mobile phone
and web portal communications when used by both patients and their HCPs.
12

13
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
13
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
Business models for apps
The healthcare apps that are available to consumers today are produced by a variety of developers,
from individuals with a novel idea to address unmet need, to large organizations with a commercial
strategy involving an app. As such there is a wide range of scale, investment, and return in the
current business models supporting consumer apps.
Examples of healthcare app developers:
Table 1: Developers of mobile healthcare apps
Developer Motivation Typical app functionality Example apps
Individual app
developers/
academic
research groups
• Initially start out with small
development to address unmet
need out of interest or with
ambitions to attract investment
Simple functionality designed for
specic need
• Living Proof: Breast Cancer
Survivor Stories
• Fat Burning Zone Calculator for
Fitness
Patient
organizations/
charities
• Creation of app products
which aid users in condition
management and provide
emotional support and other
patient success stories
Typically provide limited
functionality, oering
information, social media
connections and physician
recommendations
• Diabetes GPS
• Diabetes UK Tracker
• MyCancerManager
• PCR tracker
Corporate/
investment
backed app
developers
• Medium- to long-term nancial
returns as user base expands
and revenue model grows
May span the full range of
functionality:
• Display • Record
• Diagnose • Remind/Alert
• Communicate
• Calorie Counter by
MyFitnessPal
Pharmaceutical
manufacturers
• Increase awareness of
condition
• Increase adherence to
prescribed treatment
• Display health information
• Explain drug mode of action
and side eects
• Remind/alert
• Ab Educator
• Hoop4Diabetes
• MyBETapp
Large consumer/
retailing brands
• Link app to present oerings,
typically links to website
• Reach extended audience
• Display health information
• Record user entered data
• Provide reminders of service
renewal
• Weight Watchers Mobile
• Walgreens
• Watsons Asia
Health insurance
groups
• Inform members with general
healthcare advice/condition
management
• Enable HCP/facility search
• Display health plans
• Symptom checkers
• Physician locators
• Submit and monitor claims
• Medibank Australia symptom
checker
• Singhealth HealthBuddy
• BUPA Mobile
National health
systems
• Reach larger audience
to inuence healthcare
management
• Lessen burden on clinical
services
• Symptom checkers
• Physician locators
• Appointment reminders
• NHS Choices
• NHS Symptom Checker
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
14
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
With such a variety of backing to apps development, there is unquestionably a range of
nancial models, which in turn aects the pricing of the available apps. Of the 16,275 consumer
healthcare apps available in the Apple app store, 7,717 are free, 7,689 are priced in the range
$0.99 - $4.99, and 869 are more than $5 (of which 23 are more than $100). Despite initial
appearances, many of the 7,717 free apps oer paid content within the app. In many cases, the
free app is just a sample and the user needs to buy an upgrade or a subscription.
Investment funding can be signicant in the healthcare app space. In August 2013 it was
announced that Calorie Counter by MyFitnessPal, the most popular free calorie counter and
tness tracker on Google Play in the U.S. and the #2 on Apple App store in the U.S.
13
, with
both a website and mobile app covering 40 million users, had attracted $18 million of venture
capital nancing. The app, which has always been free to users, achieved protability through
successfully advertising tness and weight loss products and with the majority of revenues
coming from desktop use. Future growth in revenue through partnerships with hospitals or
health insurers is the aim and focus of the recent investment. Underpinning this investment by
venture capital rm Kleiner Perkins Caueld & Byers and Accel Partners is a belief that insurers will
pay for this app, or corporations will oer it as part of their employee health plans.
14
Apps placement on the patient journey
An entire continuum of healthcare needs can be addressed via apps, broadly in two main focus
areas for healthcare organizations across the patient journey:
• Changing consumer/patient behavior in areas that aect health, particularly exercise and diet
• Improving the implementation of prescribed treatment regimens
• Understanding physician instructions
• Ensuring polypharmacy is appropriately managed
• Medication compliance or adherence to physician instructions
A further detailed analysis of the consumer focused apps places them along a patient journey,
consisting of overall wellness, diagnosis, HCP visit, further information, prescription lling and
compliance. A total of 14,243 apps were placed on the patient journey, including those specic
to a particular demographic group or disease area, which can be distributed across the full
journey steps as displayed in Figure 7.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

15
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
15
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
Figure 7: Consumer healthcare app placement along patient journey
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
The Patient Journey
Therapy Area Specic: 1,980
Demographic Specic: 1,440
Prevention/Healthy Lifestyles
Healthy living, diet and exercise,
addiction quitting, stress, relaxation, and sleep
8,786
Self-diagnosis
Symptom checker and self diagnosis
304
Finding a HC profession or facility
Doctor reviews and referrals
Second opinions
931
Compliance
Persistence, Compliance
225
Filling prescription
Finding a pharmacy, availability,
price and insurance coverage
200
Diagnosis/ Education
Medical information, condition management
information, emotional support post-diagnosis
562
Number of apps
Source: IMS Health analysis of widely available consumer targeted healthcare apps

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
16
Table 2: App placement on the patient journey
Patient journey stage Description No. Functionality Example
Prevention/Healthy Living Focus on factors associated
with overall wellness:
• Healthy eating
• Weight management
• Fitness
• Tips for healthy living
• Smoking cessation
• Stress management
• Sleep
8,786
apps
• Display information
• Display pre-loaded
instructions for diet &
tness
• Record and display user
entered data
• Track weight
measurements over time
• CalorieCounter
• NikeTrainingClub
• OneSportsMan
• Weight and BMI diary
Symptomatic/
Self-diagnosis
• Reference for common
symptoms/conditions
• Diagnosis based on
data inputted/question
answered
• Communication with
medical professionals
304
apps
• Display reference
information
• Record users answers
and display appropriate
guidance
• Communication interface
between patient and
physician
• NHS Health and Symptom
Checker
• SingHealth Health Buddy
• Medibank Symptom
Checker
• Melanoma Visual Risk
Checker
• Am I depressed?
• HealthTap
Finding a Physician • Locate most appropriate
physician or healthcare
facility and nd contact
information
• Rate and review
physicians
• Appointment reminders
931
apps
• Display search results
• Display location information
(and connect to GPS)
• Connect to phone function
• Display reviews
• Remind appointments
• BetterDoctor
• US Hospitals Lite
• Patient fusion
• Doctor visit manager
Education post-diagnosis Provide health reference
material:
• Drugs/medication
information
• Emergency and rst aid
information
• Condition management
information
562
apps
• Display drug information
• Display condition
information
• Record user entered data
• Can connect to healthcare
professionals or
emergency services
• Drug Guide for Consumers
• Family Drug Guide
• Pill identier by drugs.com
• Health Handbook
• Emergency Info 4Family
• Medical Facts+
Filling prescription • Finding pharmacy
• Price scans for
medications/special oers
• Relling of prescriptions
• Drug interactions and
side eects
200
apps
• Display search results
• Display location information
(and connect to GPS)
• Connect to pharmacy
systems to register
prescriptions
• Oer discounts on
medications
• CVS Pharmacy
• Walgreens
• LowestMed Mobile
Compliance Assisting the patient to
act within the prescribed
interval and dose of a
dosing regimen:
• Pill reminders
• Medication trackers
• Alert support network if
dose not recorded
225
apps
• Provide reminders
• Display information
• Record user entered data
(e.g. register dose was
taken)
• Communicate with
support network
• Medicine Reminder HD -
with Local Notications
• MediSafe – virtual pillbox
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
17
The most dominant category on the journey is healthy living, while the least populated are self-
diagnosis, lling prescriptions, and compliance.
Healthy living: Earlier this decade Mokdad et al found that 40% of all premature deaths have to
do with health behaviors. Specically, the leading causes of death in the year 2000 were tobacco
(435,000 deaths; 18.1% of total U.S. deaths), poor diet and physical inactivity (400,000 deaths;
16.6%).
15
Since then employee wellness programs in the U.S. have claimed that 70% of all healthcare
costs are the direct result of behavior and have designed healthcare plans that reward healthy
behavior. For example at Safeway, employees are tested for tobacco usage, healthy weight, blood
pressure and cholesterol levels and receive discounts o a “base level” premium for each test they
pass.
16
As a result of encouraging healthy behaviors, the company saw its per capita healthcare costs
remain at while most American companies’ costs increased by 38% over the same period.
With almost 9,000 apps available to help the population lead healthy lives there is a real
opportunity to make an impact on overall health and wellbeing. By far the largest category
within this grouping of apps is diet and tness, with more than 5,400 of these apps solely
designed for the purpose of counting calories or tracking calorie consumption, providing tness
routines and monitoring weight or body mass index (BMI). It has already been demonstrated that
self-monitoring of physical activity and dietary intake are key components of behavioral weight
loss programs.
17
Thus the variety of apps in this space could act to provide signicant support
and guidance for individuals to achieve their health targets and lessen the burden of behavior on
overall healthcare costs.
Self-diagnosis: Although many apps provide symptom guidance and information, few propose an
actual diagnosis to the end user and it is essential that those which do are approached with caution
as not all are connected to a HCP. Recent research evaluated smartphone apps that claim to detect
cancer based on a picture of a mole.
18
Only one of the apps sent the picture of a suspected mole to a
dermatologist. It was correct 98% of the time. Three others may have serious medical repercussions
since they missed melanoma between 30% and 90% of the time, according to the report.
19
The FDA released its guidance document on mobile medical apps on September 25, 2013. One
of the areas that the FDA has been clear they intend to regulate is when mobile medical apps
transform a mobile platform into a regulated medical device. As stated in the FDA guidelines
“When the intended use of a mobile app is for the diagnosis of disease or other conditions… the
mobile app is a device”
20
This means that apps which clearly serve the purpose of providing a
diagnosis will be subject to FDA clearance as a medical device. This should lead to a higher
standard of diagnosis accuracy from the apps, and potentially increase the numbers of apps in
this category now that developers have clear guidelines to work within.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

18
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
18
Filling prescriptions: In the U.S., pharmacy apps provide weekly deals along with price
comparisons, allowing pharmacists to attract customers. These apps typically provide pricing
information for drugs sold at major retailers, and are intended to help both insured and uninsured
consumers nd the best deal on prescriptions by including pricing information for proprietary
brands and generic drugs across the most commonly prescribed medicines.
21
These apps have
the opportunity to be extended to the large audiences in emerging markets where smartphone
penetration is growing rapidly, and where out-of-pocket costs are such a high proportion of
healthcare expenditure and hence aordability is a key hurdle for access. As such there is likely to
be an increased number in this app category as target audience expansion occurs.
The U.S. market is also the most advanced market for chain pharmacy mobile apps. Walgreens has
developed an app which can be used to rell prescriptions and to remind patients when to take
their medications; they claim the most popular feature of the app is the “Rell by Scan function”,
allowing patients to scan the bar codes on their prescription vials to order rells. This accounts for
more than 40% of all online rells and generates more transactions than any other Walgreens app
feature.
22
Similarly an app from CVS Caremark also enables patients to manage their prescriptions,
with functionality that allows patients to ll prescriptions, access their prescription history, and
transfer prescriptions between dierent CVS/pharmacy locations.
23
The company claims the app
is used 1,000 times per day. If these apps can be linked to improved medication adherence and
customer loyalty, more extensive use of these sort of apps can be expected.
Medication compliance: This may be dened as “the extent to which a patient acts in
accordance with the prescribed interval and dose of a dosing regimen”.
24
To date there are no
public studies published in academic journals or whitepapers which demonstrate eective use
of apps for improved compliance. Indeed the only notable results have been released by app
developers themselves. For example MediSafe Project has released a statement claiming that its
mobile pillbox health app produced compliance rates of about 80% for patients taking type 2
diabetes medications, leading them to state that compliance was more than 26% higher for type
2 diabetic users when they used mobile technology. However, neither the compliance rates for
these individuals prior to using the app, nor the characteristics of this particular patient group,
are reported for comparison.
25
It remains to be seen whether randomized trials of mobile apps
for medication compliance can demonstrate a clinical benet resulting from the use of these
tools and hence show their value in the reduction of the multi-billion dollar non-adherence costs
to the healthcare system. Such a demonstration of evidence of value would likely drive a surge of
apps in this category.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
19
Apps specic to a demographic group or disease
Chronic diseases – such as heart disease, stroke, cancer, diabetes, and arthritis – are among the
most common, costly, and preventable of all health problems. Seven out of ten deaths among
Americans each year are from chronic diseases, with heart disease, cancer and stroke accounting
for more than 50% of all deaths.
26
About 1/4 of people with chronic conditions have one or more
daily activity limitations.
27
Arthritis is the most common cause of disability, with nearly 19 million
Americans reporting activity limitations.
28
In addition to suering early mortality, patients with chronic diseases also incur signicant avoidable
costs to the healthcare system through non-adherence to treatment. In a recent IMS Institute report
on avoidable healthcare costs in the U.S., it was demonstrated that six disease areas (congestive
heart failure, HIV, osteoporosis, hypertension, diabetes and hypercholesterolemia) accounted for
$105 billion in annual avoidable costs from non-adherence to medication treatment
29
(see Figure 8).
Figure 8: Non-adherence avoidable costs by disease, US$bn
Source: Avoidable Costs in U.S. Healthcare, IMS Institute for Healthcare Informatics, 2013
Avoidable costs by disease, US$Bn
Congestive
heart failure
HIV Osteoporosis Hypertension Diabetes Hypercholesterolemia
15.5
1.8
1.0
18.6
24.6
44.0
105.4
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
20
Of the 1,980 apps developed to date which relate to specic therapy areas, chronic conditions
dominate. However the areas of focus of these apps are highly concentrated and not related to
leading causes of mortality or non-adherence. The largest category of apps for specic therapy
areas is in mental health and behavioral disorders – with autism, anxiety, depression and
attention decit hyperactivity disorder (ADHD) making up 2/3 of apps available in that area
(see Figure 9). Mental health and behavioral disorder apps also command some of the highest
prices for apps. Of the 23 apps commanding prices in excess of $100, 16 of these are categorized
under mental health and behavioral disorders, with autism again ranking highest with 12 of the
16. These apps are predominantly communication solutions to aid with speech and provide
pre-recorded messages.
Figure 9: Breakdown of apps by therapy area
Eyes & Hearing
Mental Health &
behavioural disorders
Endocrine, nutritional
& metabolic diseases
Heart /
Circulatory System
Autism
Anxiety
Others
Cancer
Musculoskeletal system/
connective tissue
ADHD
Depression
Source: IMS Health analysis of widely available consumer targeted healthcare apps
1,980
558
537
171
37
58
96
196
77
115
139
270
284
558
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
21
For other chronic disease areas, diabetes apps (categorized within endocrinology) account for
230 apps to date; 139 apps relate to the heart/circulatory system (of which only 12 target stroke)
and there are only 77 apps for the other leading cause of death - cancer. Despite the fact that
arthritis is the most common cause of disability, only 11 apps target rheumatoid arthritis, and 5
apps target osteoarthritis. It would therefore appear that there is still unmet need in the therapy
area space for apps which provide better condition management for patients living with the
most disabling chronic diseases, such as cancer, stroke and arthritis. These apps could provide
information for optimal condition management, the ability to track patient health levels over
time (and record improvements in wellbeing or condition), and the ability to communicate with
caregivers or other patients for motivation and the sharing of best condition management – the
latter is likely to be particularly important in emotive diseases such as cancer. One of the challenges
will be how to motivate app developers to address these areas. Although a higher proportion of
condition management apps are paid for than, for example, diet apps, only a small number cost
more than a few dollars. As such, unless there can be paid content within the apps there is little
nancial incentive to address these key areas of unmet need and the duty is likely to fall back on
pharmaceutical companies or healthcare providers themselves to generate the content.
Of the 1,440 apps categorized as being intended for demographic-specic target groups, women
and children’s health dominate. Within women’s health almost 80% of the apps are pregnancy
oriented (see Figure 10).
Senior Health is at present a very small category, accounting for only 27 apps. The main target
audience within these apps however is not directly the patient, but the caregiver, with most
of these apps targeting the carer network, enabling family members and friends to plan and
coordinate their caring activities and tasks. The 65+ age category is at present the group with
the lowest penetration of smartphones according to the latest Pew Internet and American Life
Project report on smartphone ownership.
30
It is therefore reasonable that apps directly targeting
the patient within the senior health category would be lowest in number, and that instead the
apps are designed for the caregiver base which is typically made up of younger, smartphone
using family members. In future years as smartphone penetration in the 65+ category increases
there should be a concomitant increase in apps for this target audience.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
22
Figure 10: Consumer healthcare apps breakdown by demographic target groups
IMS Health ranking of top apps
Functionality scores were calculated for all apps which fall along the patient journey. However,
recognizing that the best apps have not only strong content, but are also user friendly and oer a
positive user experience, the functionality score was combined with a user score. The user score
considers the number of reviews that an app has received in addition to its star rating. As app use
increases, and new sources of evaluation become available, rating scores will inevitably evolve
beyond functionality and user scores. In particular, it will be essential to also include physician
evaluations and evidence of app ecacy in future scoring systems.
Combining the currently available functionality scores with the user scores provided an IMS
Health App Score which has been used to identify the top apps in each category. As such the IMS
Health top apps by classication on the patient journey are listed here. These apps have strong
functionality combined with ease of use.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Demographic Specic Women’s Health
OtherChildren’s Health FertilitySenior Health Pregnancy BreastfeedingWomen’s Health
1,440
689
27
562
49
45
68
724
724
Source: IMS Health analysis of widely available consumer targeted healthcare apps

23
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
Table 3: Top apps by classication on the patient journey
Patient Journey: Prevention/Healthy Lifestyles
App Name Developer Description
Calorie Counter
and Diet Tracker by
MyFitnessPal HD
MyFitnessPal.com Diet app featuring large calorie counting database and features such as
food tracking, exercise and weight goals and links to friends
Calorie Counter PRO by
MyNetDiary
MyNetDiary Inc. Diet app featuring large calorie counting database and features such as
food tracking, exercise and weight goals
Chest Trainer :
powered by
Fitness Buddy
Azumio Inc. Weight training and tness application which claims to mimic having a
personal trainer in the home, requires no equipment
Cycle Tracker Pro -
TrainingPeaks GPS
Peaksware, LLC Converts phone into a GPS-enabled cycling computer, with a wide
range of workouts, providing custom readouts and activity reports
Quit It 3.0 - stop
smoking
Tommy Kammerer A stop smoking motivational program, supporting and encouraging
smokers to quit smoking, helping ex-smokers to stay quit; keeps track of
the cigarettes not smoked and how much money saved as a result
Quit Smoking Now HD
- Hypnotherapy with
Max Kirsten
Max Kirsten A four week quit smoking program with personal hypnotherapy
sessions
Patient Journey: Finding a HCP or facility
Healow eClinicalWorks Lets patients communicate with their doctor’s oce and access up-to-
date health records, includes visit summaries and appointment reminders
Vitals – Your top 10
doctors!
Vitals Provides customized lists of the best local doctors, as rated by their
patients, allowing for searches by symptom, condition or medical
specialty
ZocDoc - Doctor
Appointments Online!
ZocDoc Tool to nd and book doctor’s appointments based on zip code
searches
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

24
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
24
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Patient Journey: Diagnosis/Education
App Name Developer Description
HealthTap - free doctor
answers to medical and
health questions
HealthTap Provides health answers and healthy tips on any symptom, condition,
medication, health concern, or even wellness topics from 47,000 U.S.
doctors; provides current and vetted health information
iTriage Healthagen LLC Provides clear, concise, and useful information covering thousands of
medical symptoms, diseases, conditions, procedures, medications and
drugs
WebMD for iPad WebMD Provides mobile-optimized health information and decision-support
tools including WebMD’s Symptom Checker, Drugs & Treatments, First
Aid Information and Local Health Listings
Patient Journey: Filling Prescription
GoodRx GoodRx GoodRx compares prices for prescription drugs and provides prices,
coupons and savings tips for more than 6,000 drugs at most pharmacies
in the U.S.
MyRell Rx Intelecare
Compliance
Solutions, Inc.
Order medications straight from the phone and get them delivered to
the door, as well as medication reminders and appointment reminders
Walgreens Walgreen Co. Rell by Scan function, Points for Rells, Pill Reminders, Transfer
Prescription feature, Rell Reminders, Health Reference encyclopedia
Patient Journey: Compliance
Dosecast Montuno Software,
LLC
Flexible medication reminder with customizable dose amounts and
instructions, a large drug database and the ability to support multiple
users
Pill Monitor Free –
Medication Reminders
and Logs
Maxwell Software Prescription reminder that alerts the user every time they need to take
a prescription. Allows user to enter all prescriptions, set up reminders,
and track when they have been taken
RxmindMe Prescription
/ Medicine Reminder
and Pill Tracker
RxmindMe, LLC Prescription reminder that alerts the user every time they need to take
a prescription. Allows user to enter all prescriptions, set up reminders,
and track when they have been taken
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
25
In addition to apps that relate to a specic step in the patient journey, apps with the highest
IMS Health App Scores in specic therapy areas are as follows.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Table 4: Top apps by therapy area
Therapy Area Specic : Diabetes
App Name Developer Description
Daily Carb -
Carbohydrate, Glucose,
Medication, Blood
Pressure and Exercise
Tracker
Maxwell Software Tracks daily nutrition intake of food, carbs, ber, fat, tracks quantity of
water intake, readings of glucose, HbA1c, blood pressure, heart rate,
weight, exercise, medications and insulin
Glucose Buddy -
Diabetes Logbook
Manager w/syncing,
Blood Pressure, Weight
Tracking
Azumio Inc. Designed as a data storage utility for people with diabetes. Users can
manually enter glucose numbers, carbohydrate consumption, insulin
dosages, and activities
GoMeals Sano-Aventis
U.S. LLC
Food, activity and glucose tracker designed to aid the user make healthy
lifestyle choices
Therapy Area Specic : Mental health & behavioral disorders
ADHD Angel Daniel Anderton Reminders to take medication, a process for sending reports ahead of
physician visits, ADHD information/reference, advice on the 8 main ADHD
'Tipping Points'
Live OCD Free Pocket Therapist,
LLC
Claims to reduce OCD symptoms by 34% in 8 weeks; includes video
tutorials as well as extensive user guide
T2 Mood Tracker The National
Center for
Telehealth and
Technology
Allows users to monitor their moods on six pre-loaded scales (anxiety,
stress, depression, brain injury, post-traumatic stress, general wellbeing).
Custom scales can also be built
Therapy Area Specic : Musculoskeletal system and connective tissue
Oce-Fit Medicus 42
GmbH
Provides exercises against work-related pains and stress
WebMD Pain Coach WebMD Oers a holistic approach to balancing lifestyle with chronic pain
conditions. In particular provides help for those suering from back
pain, neck pain, nerve pain, bromyalgia, migraine, osteoarthritis and
rheumatoid arthritis
Zimmer Arthritis 411 Zimmer, Inc Patient education resource for people who suer from osteoarthritis. Can
be used at home to learn more about arthritis pain and treatment options

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
26
Therapy Area Specic : Oncology
Dr K's Breast Checker Lingopal
Holdings Pty Ltd
Designed to help women keep track of change in breasts using
interactive tools, provides practical information and reminders
PCR Tracker Cheryl-Anne
Simoneau
Specically designed by CML patients for CML patients, allows user to
track and graph results from lab tests, treatment reminders, understand
treatment milestones, access educational tools and videos, reference to a
glossary of terms used
SkinKeeper The Health Safari
Pty Ltd
Enables user to monitor moles, capture important personal and family
skin cancer risk factors, and share this information with their doctor
Therapy Area Specic : Nervous system
Noteness (Multiple
Sclerosis)
Martin Hartl Is a multiple sclerosis diary app. Monitors injections and symptoms, and
provides reminders
Parkinson Diary Health Wave
Signals, LLC
App for patients and caregivers to record, report and review symptoms
easily. Features symptom logger, graphical representation of changing
symptoms, animation to visually see how symptoms have changed over
time
Young Epilepsy Young Epilepsy Designed for young people with epilepsy, and parents or carers of a child
with epilepsy. Contains an up-to-date information portal, video and diary
that helps track and manage seizures and symptoms
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

27
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
PROFILING WIDELY AVAILABLE CONSUMER HEALTHCARE APPS
27
Top-rated apps that are specic to women’s health or children’s health are as follows:
Table 5: Top apps by demographic
Demographic Specic : Women’s Health
App Name Developer Description
Ovulation Calendar
Ladytimer Free
Vipos.com Tracks and predicts menstrual cycle days, helping women to become
pregnant or avoid pregnancy
Period Diary (Period,
Fertile & Ovulation
Tracker)
nanobitsoftware.
com
Fully animated period and ovulation tracker. Monitor menstrual
symptoms, body weight, temperature, and add notes
Pregnancy Tracker from
WhatToExpect.com
Everyday Health, Inc. Guides women through pregnancy day-by-day. Based on entered
due date user receives personalized content, gets access to the latest
parenting news and health information, and can be connected to a
community of other expecting moms
Demographic Specic : Children’s Health
Baby Connect (Activity
Logger)
Seacloud Software Baby tracking application which provides graphical reports and
trending charts, weekly averages, medicine, vaccine and growth
tracking, timers, notications, reminder alarms
Baby Food Pee Poo
Free
Colorful Drop Combines baby logger/tracker, reminders (feeding, diaper change,
and sleep) with built-in alarm sound or human voice, as well a white
noise recorder/player
Total Baby ANDESigned Baby logging and tracking function which covers: Diapers, Nursing,
Pumping, Bottles, Solids, Sleeping, Bath, and Other (timing and
tracking), Diary, Milestones, Doctor Visits, Growth, Vaccines, and
Allergies (logging)
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
28
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Achieving greater uptake of healthcare apps
Patients, physicians and payers all face obstacles in accessing or supporting
the use of apps, providing barriers to their greater use and usefulness across
healthcare
• Despite the thousands of healthcare apps available, downloads are heavily skewed toward a
small number of apps
• Barriers to wider uptake and use of healthcare apps span all stakeholders
• Patients currently face a maze of healthcare apps with little guidance on quality although this is
starting to be addressed in the U.K. and U.S.
• The demographic skew of smartphone users makes it more dicult to reach those who are the
most expensive users of the healthcare system
• Physicians see six key hurdles to the widespread recommendation of apps to patients
• Payers expect to see evidence of improved outcomes and reduced hospitalizations before they
will reimburse mobile apps
Assessment of app functionality
Installs data from the Google Play (Android) app store shows the skew in download volumes for
healthcare apps. The majority of these healthcare apps receive very few downloads: more than
50% of the apps in this category receive less than 500 downloads, with only 2% receiving more
than 100,000 downloads. In fact, 5 apps account for 15% of an estimated 660 million downloads
in this category (see Figure 11).
31
It would therefore appear that despite the choice available the
market is already very concentrated and consumers are consistently choosing the same apps.
Since analysts’ estimates for downloads of apps in 2013 across all geographies and categories
range from 56 to 82 billion, this shows the current limitation of healthcare app use.
32

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
29
Figure 11: Android healthcare apps installs from the Google Play store
There are many reasons for both the skew and the limited number of downloads observed, and
they span all stakeholders. These barriers result in a current lack of incentive to recommend and
use mobile apps in healthcare and hence the full potential of apps is far from being reached:
• Patients have to navigate a maze of healthcare apps with little guidance, meaning those apps
with the most downloads are considered best and continue to receive the most downloads
– a self reinforcing cycle
• The demographic skew of smartphone users makes it harder for the most expensive healthcare
system users – the elderly suering multiple chronic conditions - to be targeted
• Prescribers are faced with the same widespread choice of apps as patients and with limited
information regarding app performance and benets may be wary to choose an app to
recommend to their patient
• Payers are unwilling to consider providing reimbursement for mobile apps without
evidence that they bring clinical or cost benet - and to date there are minimal studies
demonstrating ecacy
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
30%
501-10k
28%
51-500
29%
1-50
11%
10k-100k
85%
33,247 apps
15%
5 apps
2% >100k
100% = 33,252 apps 100% = est 660m downloads
Number of installs obtained
Google Play App Store: Health/Fitness and Medical Apps:
Share of installs volume
Source: IMS Health analysis of installs data
31

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
30
Challenges for patients using healthcare apps
With more than 16,000 healthcare apps in the Apple app store alone to choose from, the choice
for consumers is confusing. Healthcare app developers include pharma companies, retailers,
national health systems, insurance companies, as well as small businesses and individuals. There
is a recognizable split between those apps which are developed as part of a commercial strategy,
and those which are developed simply to try and cover an area of unmet need. For a consumer
approaching an app store, at rst glance it would appear that healthcare apps are in a state of
chaos with little structure or order to help the patient determine the optimal app out of the
thousands available for their particular needs.
In March 2013 the National Health Service (NHS) Commissioning Board in the U.K. unveiled a
library of NHS-reviewed health apps intended to help people manage their health. The apps are
produced by a variety of developers and then reviewed by the NHS to ensure they are clinically
safe. At present the library is a working project with more apps being added over time. Apps in
the library to date include those which provide advice on specic medical conditions (such as
mental health or diabetes), allow users to book repeat prescriptions, access test results, and nd
the most appropriate NHS service. The library has been designed by the NHS to put patients
in control, in the hope that giving patients easy access to information will encourage them to
participate in their care. This initiative by the NHS is also in response to the large number of apps
available that are of varying levels of quality with respect to the medical advice provided. It is
intended to provide an NHS stamp of approval so users know the apps are safe.
33
Progress is also being made in the U.S. HealthTap has developed a product called AppRx, which
enables its 40,000 physician users to evaluate health and medical apps. Doctors in the network
review the apps on a high level, based on three questions.
34
• Is the app medically sound?
• Is the app useful?
• Is the app easy to use and understand?
Doctors have the option to write a review to explain their choice, and their reviews do not enter
the system until at least 30 reviews have been made and the HealthTap medical review board has
approved them. These reviews are then available to all of HealthTap’s non-doctor customers –
patients will be able to see the reviews and see how many/which doctors recommended the app.
Separately, patients will also be able to recommend the app with the “applaud an app” function.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
31
More recently in the U.S. the “Go You Cigna Marketplace” was launched providing a landing site
for members that features certied health and wellness apps. As development continues the aim
is to certify additional health improvement apps that receive positive customer feedback.
35
These rst steps towards healthcare app-verication are essential for consumers to have trust in
the app they are using. Without such measures consumers are reliant on numbers of downloads
and individual reviews as a guide to usage by the wider public, and hence become involved in a
self-reinforcing cycle of most downloads continuing to inspire further downloads.
Smartphone penetration vs healthcare expenditure
The 2012 Pew Internet and American Life Project report on cell phone activities showed that 31%
of cell phone owners in the U.S. use their phone to look for health/medical related information.
36
With the increasing number of healthcare apps and their uptake by the general population,
technology is providing the opportunity for individuals to be at the heart of their own healthcare.
In moving to a situation where patients/consumers have increasing personal responsibility for
their own health, there is the potential to move towards a society focused on overall wellness and
preventive measures rather than reactive measures.
However, it is important to recognize that apps are not a panacea and optimal deployment does
not mean for every individual, in every situation.
Although for many people apps in healthcare have progressed from being a novelty to a
mainstream tool the fundamental question remains: can healthcare apps really improve
healthcare eciency and lessen healthcare costs? In the U.S. it is estimated that 5% of the
population account for 50% of all healthcare expenditure; 20% of the population account for 80%
healthcare expenditure
37
(see Figure 12). The pertinent issue then is whether apps can really turn
the dial for the 20% of the population who are the nation’s top users of healthcare services.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“There is a tendency among certain populations to over analyze… there is always a limitation when
you’re designing an app of how much raw data you want the consumer to know versus having
a built-in back end where there is somebody with a medical background, some kind of structure
or framework, where the data that’s being collected can be interpreted and analyzed for the
consumer.”
Alisa Niksch, MD – Tufts University School of Medicine

Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
32
Figure 12: Percent of total healthcare expenditures for percentiles of the U.S. population
37
The elderly (age 65+) are much more likely to be among the top healthcare spending percentiles. A
principal reason for this is that a much higher proportion of the elderly than the nonelderly have
expensive chronic conditions. However, those over the age of 65 are least likely to own a smartphone or
to have downloaded an app, according to recent surveys (see Figure 13).
Figure 13: Smartphone penetration and app download by age group
30,36
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Source: IMS Lifelink Health Plan Claims Database, Dec 2010
Distribution of spending in the privately insured
Percent of health plan members, ranked by healthcare spending ($)
25.6% 50.6% 65.2% 74.3% 80.7% 85.4% 96.9% 3.1%
Top 1%
> $44,957
Top 5%
> $14,947
Top 10%
> $8,528
Top 15%
> $5,773
Top 20%
> $4,169
Top 25%
> $3,130
Top 50%
> $874
Bottom 50%
< $874
Sources: Pew Internet and American Life Project: Smart phone ownership June 2013, Cell phone activities Nov 2012
79
81
69
55
39
18
18-24
25-34
35-44
45-54
55-64
18-29
Age group
Age group
34-49
50-64
65+
65+
65
25
8
53
Smartphone Penetration by age group (%), USA % US phone owners who have downloaded an app

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
33
Methods for increasing smartphone penetration and app downloads amongst the elderly are
essential to unlock the full potential of mobile apps in healthcare eciency improvements. An
alternative approach is to consider family and caregivers of the elderly and the role they can play,
supported by specic apps. For example, the hundreds of apps developed to help patients nd an
appropriate medical professional/facility can also be used by family; obtaining a prescription rell
simply by scanning the current product barcode can be done by friends and family members who
can ensure from a single visit to the patient that their medications remain well stocked. When it
comes to medication adherence, several apps serve not only as pill reminders, but allow the patient
to nominate a “support network” who will also receive notications if a medication dose has been
missed or not entered into the system. In this way the carer network is using healthcare apps to
become or remain involved with healthcare management plans for elderly patients.
In the case of older patients with multiple medical problems, it would not necessarily be benecial
to use apps that are narrowly focused on one disease area, and instead it would be optimal for these
patients to be supported in taking their multiple medications that their physician has prescribed,
and to be supported in remembering the combination of diet tips suggested as a reasonable t
for their preferences and combination of medical conditions. The burden on the patient if every
specialist seen decided to recommend or prescribe their own preferred app for adherence would
quickly lead to app overload, similar to that experienced by patients receiving uncoordinated
guideline-recommended care for multiple co-existing chronic conditions.
38,39
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“There’s a group [of patients] who each have several medical problems and often they have several
specialists, all making recommendations. It’s often overwhelming for the patient and for the
caregiver. They get overwhelmed by the number of pills and the number of recommendations that
they have been given, so I feel that if everybody starts prescribing apps it could quickly lead to app
overload”
Leslie Kernisan – Geriatrician and caregiver educator
“The challenge we face as practicing physicians is that we have an aging population who can be
very savvy with a smart phone and tablets but may not view these technologies as an essential part
of their life. And then you have the millennials who were born after the internet was created, and
that is the life they know, the connected life. So, from an enterprise standpoint, we have to gure
out a way to engage both these patient groups”
Sameer Badlani, MD – CMIO, University of Chicago Medicine

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
34
It is feasible that with increasing smartphone penetration amongst the elderly – the 18% of
Americans age 65+ who now own a smartphone compares to only 13% in 2012
30
, and high
smartphone penetration amongst the younger generations who are likely to make up the
caregiver base, mobile healthcare apps can begin to make an impact on healthcare eciency in
the highest healthcare-spending group.
Finding appropriate medical attention promptly, enabling caregivers and family members to
access further detailed information on the condition, order prescription rells and receive their
own notications if the patient has not taken their medication, enables a more solid support
network than might otherwise be envisioned and can lead to avoidance of costly complications
arising from delayed access to healthcare or non-adherence to treatment. However it is important
to note that most patients and families have only limited time available for daily healthcare
management tasks and while apps can help people to manage a medical plan, not all patients
or carers will be willing to try, or will respond, to mobile apps. Technology is an enabler, but the
challenge remains in changing a patient’s behavior.
In fact it is changing a patient’s behavior that may well hold the key to healthcare savings in the
future. Younger people are prolic users of apps on smartphones and apps related to diet/tness/
weight management account for half of all apps on the healthcare app store and are the top
ranking apps within the category. Over time, the positive inuence these apps have in changing
behavior and attitudes toward wellness, exercise, diet and health could potentially have a very
signicant impact on future levels of chronic disease and the associated healthcare burden.
Six key hurdles for widespread physician app recommendation
At present, physicians do not recommend apps as standard practice, though they show strong
interest and the current level of activity looks set to change in the near future as the infrastructure
and evidence for use becomes more widespread. The pioneer in this space is Dr. Erik Topol MD,
a practicing cardiologist with Scripps Clinic, who has said in interviews that he prescribes
more apps than pills.
40
A near-term opportunity exists for other physicians globally to become
condent in going beyond an ad hoc assessment of the ratings of individual apps and actually
recommend or even prescribe to their patients the use of such a tool to monitor behavioral
patterns, to access information and to monitor their treatment remotely or provide extra data to
the healthcare professional.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
35
In-person discussions with leading physicians and opinion-leaders in the U.S. suggest a diverse
set of hurdles for widespread app-prescribing currently exist (see Figure 14):
• Choice of apps and evidence behind them
• Infrastructure for app prescribing
• Regulations
• Data privacy and security
• Reimbursement
• Liability
Figure 14: Hurdles to widespread physician recommendation of apps
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“I conceptually love the idea of apps in engaging our patients. As a physician, if I could get this
fantastically digestible data that allows me to better care for them, that’s the Holy Grail. But I think
we’re, as we all know, a long way from there”
Michael Docktor, MD – Boston Children’s Hospital
How can a physician
be condent in
prescribing an app
to a patient?
Choice/
Ratings
Data privacy/
Security
Legal
Reimbursement
Regulations
Infrastructure
to prescribe
Which apps are the most relevant
for my patients and can I trust
they are good?
How do I go about
recommending /prescribing
an app to my patient?
What are the regulations for mobile
apps: am I safe to recommend an
app without FDA clearance?
Are these apps endorsed by my
institution with legal agreement?
If there are any repercussions
from app use am I liable?
How will my patient pay for
the app I recommend unless
it is free? Will they have to pay
themselves or will insurance
reimburse the cost?
If I am prescribing an app to my
patient can I be condent that all of
their health data is secure and stored
in a HIPAA compliant manner?

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
36
Choice of apps/lack of evidence: In the same manner that the sheer volume of available apps
can be confusing to patients, physicians face the same challenge. When a patient is seeking a
recommendation, the physician has limited resources to help guide their choice and may fall back
on personal preference or peer recommendation rather than the specic needs of the individual
patient. Physicians more than patients are likely to look for evidence that apps work and can
demonstrate improved outcomes, hence apps which have evidence to demonstrate their ecacy
are more likely to stand out and be recommended.
Some physicians also expressed a downside potential in that apps may create “data overload” that
leaves a physician awash in data but nothing fundamentally useful to make important decisions.
If apps start overwhelming physicians with data to interpret, there will be a need for “data triage”
to separate the important signals from the noise of information overload. There is a risk in the
short term that recommending a patient use an app could lead to longer, not necessarily shorter
and more meaningful patient encounters.
Infrastructure to recommend: At present, the infrastructure necessary for physicians to formally
recommend apps to patients is limited and many instead resort to writing down an app name
and giving it to the patient during their consultation. To address this challenge for physicians,
in 2012 testing of an app formulary was undertaken by Happtique, but to date there has been
no public release of results from that test.
41
App formularies could be a signicant asset to
physicians if they contain simple functionality such as grouping apps by type, rating their
functionality and ease of use as well as their medical content, and displaying the frequency of
recommendation so that physicians can see which apps are recommended the most by others in
their profession. Formularies will need to be designed such that physicians can directly send the
app recommendation securely to the patient’s phone for them to download and be able to follow
up as to whether the app was in fact downloaded.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“It goes without saying that 40,000 apps within any store is the denition of poor design, because
you know that 90% of them are terrible designs and I would say that’s the number one cause of lack
of adoption”
Israel Green-Hopkins, MD – Boston Children’s Hospital

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
37
Seamless integration with other health information technology systems including electronic
health records (EHR) will be a necessity for any system designed to provide a means for
physicians to recommend apps to their patients, as they – or the chief information ocer of
their provider organization - will likely resist a stand-alone IT system at a time when so much
eort and attention is being placed on implementing or upgrading EHR systems. Large
provider networks or integrated delivery systems are also likely to require apps to contribute to
patient engagement, consistent with the Meaningful Use requirements under the 2009 Health
Information Technology for Economic and Clinical Health (HiTech) Act. The overall goal of the
Meaningful Use program is to promote the widespread adoption of EHR systems, ultimately
creating an infrastructure that improves the quality, safety and eciency of patient care.
To qualify for Meaningful Use incentive payments, eligible providers must not only adopt an EHR,
but also show that they are “meaningfully using” their EHR by meeting a number of objectives
designed by the Centers for Medicare & Medicaid Services (CMS) to have a positive impact on
patient care.
Regulations: The FDA recently released its guidelines for mobile medical apps stating clearly that
the two groups of apps it will regulate are those which are intended to be used as an accessory
to a regulated medical device and those which transform a mobile platform into a regulated
medical device. To date, the FDA has approved about 100 mobile medical apps - including
40 in the last year - most of which are focused on chronic condition management including
diabetes, asthma, and blood pressure management.
42
However the FDA has also made clear
that it intends to exercise discretion in regulating apps that provide patients with simple tools
to organize and track their health information, such as apps that enable patients with specic
conditions or chronic diseases to log, track, or trend their events or measurements and share this
information with their HCP as part of a disease-management plan, and also apps that provide
or facilitate supplemental clinical care, by coaching or prompting, to help patients manage their
health in their daily environment. With the issuance of this guidance, physicians can be condent
going forward that the apps they are likely to be recommending to their patients are receiving
appropriate levels of regulatory scrutiny.
Data privacy and security: It is essential that there is both transparency and awareness of how
data entered into the app is used and that patient consent is obtained for use of that data.
If a healthcare app collects, stores, and/or transmits information that constitutes Protected Health
Information (PHI) it is essential that it does so in full compliance with the Healthcare Information
Portability and Accountability Act (HIPAA), and any other applicable laws or regulations of
the country concerned. Any app that is intended to connect to an Electronic Health Record or
Personal Health Record (PHR), enabling users to send and retrieve patient information between
a mobile device and the EHR/PHR, must do so in a secure manner and all stakeholders involved
must accept their stewardship role for protecting the data contained within.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
38
Reimbursement: How the patient will pay for the app is a concern for many physicians.
Although almost half of healthcare apps available to consumers can be downloaded for free, the
other half range in price from $0.99 to more than $100. In particular, therapy area specic apps
are more likely to only be available with a patient charge. At present patients need to cover the
cost of the app directly although as evidence emerges for ecacy there is likely to be a push for
reimbursement. WellDoc’s BlueStar diabetes management system is now available to employees
at a number of Fortune 500 companies who have decided to oer it as a reimbursed program
for their employees and their dependents with diabetes.
43
The product is on prescription benet
plans, requiring a healthcare professional to prescribe BlueStar to one of these employees before
they can use it. WellDoc is pursuing a new path to condition management with its reimbursed
mobile software and it is likely that this will be mirrored by other developers in the future.
Reimbursement for physicians to review remotely generated patient data via apps is also seen as
a consideration prior to recommending such an app, particularly for physicians operating on a fee
for service basis.
Legal: Discussions with leading physicians make clear that taking the leap from recommending
an app to a patient to ocially prescribing an app would add a whole new dimension to
the process. Chief medical information ocers (CMIO) would recommend the prescription
of a subset of apps by that institution’s physicians to their patients only after receiving the
endorsement of their organization’s legal team. Liability from any medical repercussions as a
result of app use is also a concern for physicians.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“Doctors have to be able to trust the app and the data that it’s collecting and distributing”
Creagh Milford, DO, MPH – Massachusetts General Physicians Organization
“When an individual physician says ‘I like this app, you should use it’, it is very dierent from the
CMIO or the Associate CMIO saying ‘These are the endorsed apps from the organization, we have
evaluated the app and physicians are welcome to use them’. Now you are putting an institutional
stamp on an app and you have to have supporting evidence for use, liability, and technical support
amongst many aspects.”
Sameer Badlani , MD – CMIO, University of Chicago Medicine

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
39
Payer requirements for app reimbursement
Before payers will be willing to reimburse mobile apps, encouraging uptake by both patients
and physicians, there will be a need for evidence which shows the benets of using apps as part
of standard healthcare management. The evidence requirements will vary depending on the
intended utility of the app (see Figure 15).
Figure 15: The app evidence divide
Self-diagnosis apps: These apps are likely to require the highest level of evidence and the
results from evaluating several apps intended to diagnose melanoma suggest this is an urgent
and critical need.
18
Diagnosis apps may be less likely to be reimbursed by payers in mature
markets where there is an expectation that a HCP will be undertaking the diagnosis, but the FDA
will be regulating such apps as medical devices and hence will be expecting to see evidence of
their utility before approval. There is a strong likelihood of self-diagnosis apps becoming widely
used in emerging markets where access to physicians can be severely limited in remote locations,
and yet where smartphone penetration is continually increasing. As such patients should be
reassured of the accuracy of such applications through thorough testing and regulation by the
FDA or other agencies.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Critical need for evidence
Clinical trials to demonstrate ecacy Regulation to verify safety of diagnosis
Need for evidence to demonstrate benets to all stakeholders
Observational studies to demonstrate ecacy Need for regulation when apps link to device or sensor
Need for evidence for reimbursement
Observational studies necessary to improve uptake No foreseen need for regulation
Download popularity/3rd party ratings suce
Ranking by professionals likely to aid
consumer condence
Download volume likely to be inuencing
factor for choice
Self-Diagnosis
Apps
Condition
Management
Remote
Monitoring
Prevention/
Healthy Lifestyle
Compliance
Rx lling
Finding HCP
Education
post-diagnosis

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
40
Condition management/remote monitoring apps: The largest trial carried out to date in the
condition management/remote monitoring area is the WellDoc diabetes management software
trial.
11,12
As well as demonstrating improved A1c levels in patients, feedback from physicians was
also very encouraging. The product is now reimbursed by several large corporations’ healthcare
plans. However reimbursement for other medical apps, including others approved by the FDA,
has not been secured and many questions remain for reimbursement. For condition management
medical apps, payers are likely to expect to see evidence of a dened improvement in specic
outcomes measures, whether this be therapy area specic measures such as A1c levels or blood
pressure levels or an overall dened improvement in adherence to prescribed treatment as a
result of remote monitoring, medication reminders and healthcare task management.
Wellness apps: A recent RAND report estimated that approximately 50% of employers with
more than 50 employees oer wellness programs. Although only about half of all employers
oer wellness programs, more than 75% of employees working for companies with more than
50 employees have access to a wellness program, because large employers, who account for a
greater share of the workforce, are more likely to have such programs.
44
With many corporations
in the U.S. and Europe enrolling employees in wellness programs, and with measures such as
those in the Aordable Care Act encouraging employers to set aside premiums for wellness
based incentives, there is growing interest in how apps may support patients in this manner.
It is likely that to fully realize this potential, payers of wellness programs will want to see
meaningful evidence of the ecacy of relevant apps. Evidence for apps in a wellness setting is
much more likely to come from real world use than an randomized clinical trial, and to date few
studies have analyzed this. A pilot study by Carter et al followed 128 overweight volunteers over
a time period of 6 months, comparing the outcomes of a group of patients randomized to self-
monitor weight management via a mobile app against patients using either a website or a paper
diary.
45
The pilot trial was not statistically powered to detect change in anthropometric measures;
however trial retention was 40/43 (93%) in the smartphone group, 19/42 (55%) in the website
group, and 20/43 (53%) in the diary group at 6 months. Adherence was statistically signicantly
higher in the mobile app group with a mean of 92 days (SD 67) of dietary recording compared
with 35 days (SD 44) in the website group and 29 days (SD 39) in the diary group (P<.001).
Larger scale real-world trials such as this are likely to be conducted in the future to satisfy the
requirements of payers in a wellness setting. However it remains to be seen if there will be a
“class eect” and whether one large trial with a specic calorie counting app or a tness app will
be seen as sucient to cover all calorie counting and tness apps, or whether ease of use and
individual functionalities of the app will lead to a more individual evidence scenario. If that is
to be the case then there will inevitably be a fall out from the smaller app developers who are
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

ACHIEVING GREATER UPTAKE OF HEALTHCARE APPS
41
unable to aord such an extensive analysis of their user base. Evidence that is collected by the
use of apps in such Wellness programs could also be used by physicians and payers looking for
outcomes evidence before widely adopting such technology.
Finding a HCP/healthcare information apps: These apps serve to provide the consumer
with information on relevant healthcare services and their condition management/medication
regimen “on the go”, providing a convenience factor, and do not sit on a part of the patient
journey that is ever likely to see reimbursement or recommendation. As such apps are
downloaded on the basis of consumer interest, and download popularity or reviews from other
users are likely to suce, formal evidence of utility is unlikely to be required in the future.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

CALL TO ACTION
42
Call to action
For mobile apps in healthcare to move along the maturity curve and become
a fully integrated component of healthcare delivery, all stakeholders must be
engaged and evidence developed
• The app maturity process will be driven by four key elements which involve all stakeholders
- Payer and provider recognition of the potential role of apps in healthcare management
- Creation of a standard benchmark for security/privacy guidelines that protects PHI globally
- Curation and evaluation of healthcare apps
- Integration of apps with other health IT systems
• Systematic development of credible evidence of the value derived from using healthcare apps
will also be necessary
For app use in healthcare to evolve across the maturity spectrum from present day novelty factor
and ad hoc use, to become a fully integrated component of healthcare delivery with widespread
recommendation by healthcare professionals and reimbursement from payers, there are four key
issues to address on the model to app maturity (see Figure 16). There are a range of stakeholders
which form the “app ecosystem” and each of the four steps requires collaboration between these
stakeholders: the app developer, the regulator, the provider, the patient and the payer (see Figure 17).
Additionally underpinning the entire maturity model will be increasing evidence of app eectiveness.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

CALL TO ACTION
43
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Promoting Adoption
Process is underscored by increasing evidence of healthcare benets
Implementation
Recognition of apps
Security/Privacy guidelines
Curation and evaluation of apps
Integration with health IT systems
Level of maturity of app prescribing
Time
Fully integrated delivery of healthcare
Apps have a fully integrated role in the
delivery of healthcare
Systematic use of mobile apps in healthcare
Systems and policies in place to enable
widespread use of apps in healthcare
Individual physician recommendation
A small number of progressive physicians
are recommending apps to their patients
Stakeholder dened
unmet need
Stakeholder
Collaboration
App
developer
Regulator
Provider
Patient
Payer
Figure 16: The app maturity model
Figure 17: Stakeholders in the app maturity model

CALL TO ACTION
44
Recognition of the potential role for apps: Apps should not be used as a replacement for
human care, rather they should provide a strengthening of the care provided. Across the patient
journey mobile apps have the potential to empower patients to live a healthier lifestyle, and to
ensure adherence to prescribed treatment.
In the U.S. the Patient Protection and Aordable Care Act is driving dramatic changes in
healthcare. Improving the quality of care and treatment outcomes is one of the priorities of
healthcare reform. Delivery of care changes center on the patient and creating connections
between all settings of care; an additional component of healthcare delivery reform is
preventative healthcare. Payers and providers should recognize the potential of mobile apps in
this setting. A key benet to the physician in charge of the patient’s healthcare management
is the remote monitoring of vitals which can be communicated back to the healthcare practice.
Alongside patient logging of healthcare activities this can help to improve continuity of care
in cases where there is a transition of care management after hospital discharge, avoiding
the penalties that will be introduced for hospital readmissions. Public health literacy can be
improved through use of informational apps and patient awareness of preventative healthcare
services can also be targeted.
A further aim of the healthcare reform is to encourage the meaningful use of EHRs in order to
enable information-sharing between healthcare stakeholders and across settings of care. Apps
also have a potential role here with providers oering apps from which patients can directly
access their EHR, and with the potential for patient-reported healthcare measures being
transferred from the app to the EHR.
For providers and payers to recognize the potential value of apps to healthcare eciencies they
will also be looking for evidence that the patient is actively engaging with the technology (see
Figure 18).
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“There is a big desert that you enter once you leave the hospital or the doctor’s oce. So that is
where I really see a lot of opportunity and personal excitement around using an app as a tool to
help ll that space”
Jonathan Birnberg, MD – North Shore University Health System
CALL TO ACTION
45
Figure 18: Evolution of evidence of app implementation
Security/Privacy: The main risks posed to data protection by apps at present stem from the
consumer’s lack of awareness or understanding of the types of data collected and a failure to
obtain the consumer’s consent for the processing, storing or accessing of any personal data on their
smartphones. As such, a typical privacy policy for mobile applications (not specic to healthcare)
would contain as a minimum four published elements:
46
• The categories of personally identiable information (PII) collected and the types of third
parties with whom the information is shared
• A description of the process for users to review and request changes to their PII that has
been collected
• The process by which material changes to the privacy policy will be communicated
• The eective date of the policy
With healthcare apps it is essential that any information that constitutes PHI is treated in full
compliance with HIPAA, and any other applicable laws or regulations of the country concerned.
The challenge for app developers today is there is no published standard which shows that an app
is in fact HIPAA compliant and dierent regions globally are at dierent stages of mobile app privacy
guideline design.
In a time of rapidly evolving technology, industry self-regulation is the most eective way to
maintain the balance between consumer condence in privacy and continued innovation. As such
the mobile healthcare apps industry should itself dene a standard which ensures that all healthcare
apps adhere to the highest privacy standards. This standard should include, but not be limited to,
the following points:
47
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Today: Adhoc patient use
Short to Medium Term:
Systematic patient use
Medium to Long Term:
Integrated healthcare component
• Patients are downloading apps
• Patients are using apps
• Patients are using apps eectively
• Patients are receiving clinical benet
• Patient Reported Outcomes

CALL TO ACTION
46
• App developers should request consent before the app starts to collect data from the device or
place data on the device: this consent should be informed and specic
• Apps should only collect data that is strictly necessary for the app to perform the desired
functionality
• Developers should dene a reasonable period of time for data retention. Dormant apps should
be treated as expired and the data should be deleted
• HIPAA standards should be translated into a global benchmark which forms the basis for
privacy and security of all PHI data transmission, encrypting data and making eorts to de-
identify user data before sharing it with another party
Once mobile healthcare app developers have designed their global privacy standard, providers
and patients can be reassured of the benets of apps in healthcare rather than detracted by their
concerns over protection of personal information.
Curation and evaluation: Systematic curation and evaluation of apps that can provide both
physicians and patients with summarized content to aid decision-making regarding the appropriate
app choice will be an essential step towards promoting the widespread adoption of healthcare
apps. There are initial steps being taken in the U.S. and the U.K. but new services with widespread
medical endorsement that ensure this information is made available in the proper format and
context to support patient care will be required in future.
Evaluation services must group apps by functionality, and contain user evaluations, physician
evaluations and evidence to support the use of the app in the context for which is was designed.
Professional healthcare societies, such as the American Medical Association or other similar
organizations, should be involved in the process endorsing the apps with the highest evaluation
rating for use by their members since credibility and trust are a strong factor in who curates.
Integration of apps: The integration of mobile apps with other aspects of patient care including
use of electronic health records and patient portals requires the least collaboration between
stakeholders but will be one of the pivotal steps on the app maturity journey to facilitate the
widespread prescription of mobile healthcare apps. This requires consideration by provider
organizations, EHR software vendors, and the support of the Oce of the National Coordinator for
Health Information Technology (ONC) and CMS regarding meaningful use.
Stakeholder collaboration: Across these four steps dierent stakeholders have dierent roles to
play. In addition to the main stakeholders there are professional service enablers who also need to
contribute to the process.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

CALL TO ACTION
47
Table 6: Stakeholder call to action
Recognition Security/Privacy Curation/
evaluation
Integration
App Developer
✔ ✔ ✔ ✔
Regulator (Approver)
✔
Provider
✔ ✔ ✔ ✔
Patient
✔ ✔
Payer
✔
The call to action is therefore clear: app developers and healthcare providers need to be the main
drivers of progress for app maturity. As the key starting point in the process, app developers have
the power to drive recognition through the design of apps which a) satisfy key areas of unmet need
(such as condition management in leading chronic diseases or disabling conditions), b) clearly
address elements of healthcare reform, c) have a clear value proposition backed up by evidence
of eectiveness which can be used in the evaluation of the app and d) which respect the data
protection rights of the user and ensure all sensitive information is handled appropriately. App
developers must also be willing to work with other developers of healthcare IT system infrastructure
to ensure that there can be a seamless integration of systems.
A fundamental challenge here is the range of app developers. App developers range from National
Health Systems and large retailing brands with sucient resources to tackle all of the above calls
to action, to individual app creators with no nancial backing and no resources available to collect
outcomes evidence. A consortium of app developers needs to be formed which represents equally
the interests of all app developers, and which lays out a clear plan to overcome the hurdles on the
app maturity curve. Providers also need to work together to share best-practice on app policies and
to design national guidelines for the systematic use of mobile apps in health delivery.
App developers and providers must then work together to ensure maximum benet and cost
eciencies for the healthcare system.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

CALL TO ACTION
48
Evidence
There is a pressing need for credible evidence of value derived from the use of healthcare apps
that will meet the needs of physicians and payers. This evidence will inevitably evolve and become
more sophisticated over time. Although at present observational studies are accepted as the best
available, it will be essential that over time randomized trials are conducted with the long-term goal
being outcomes based evidence.
There are at present opposing sides of the debate as to the necessity of conducting randomized
clinical trials (RCT)with mobile apps but these arguments tend to be based more on logistics than
evidence requirements. Those against performing randomized trials typically argue that the cost
would prevent small app developers from conducting them, and that the time taken to generate
results is too slow considering the pace at which technology evolves. It is also argued that since
multiple medical devices marketed with FDA approval do not have randomized trials to back them
up simply because they are unlikely to cause harm, there is no reason for apps to be treated any
dierently, especially now that the FDA has stated it is likely to exercise discretion for the majority of
mobile apps.
48
However, these arguments are looking at the process of the randomized clinical trial purely from a
development and approval perspective. The call to action for evidence generation from randomized
trials and outcomes based results is based on the belief that without this evidence there will not be
widespread uptake by providers and payers, making apps a fundamental component of healthcare
delivery and instead skepticism will remain amongst these key stakeholders. Since at present there
is almost no scientic evidence published in peer-reviewed journals regarding dened benets of
mobile app use, it is necessary to approach the evidence evolution in stages.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“Patient reported outcomes, or whatever term you want to use - those will be the future that we, as
providers and health systems, will be measured on”
Creagh Milford, DO, MPH – Massachusetts General Physicians Organization
“I am not aware of any scientic literature that proves the benet [of mobile apps]. While there are
a lot of industry sponsored white papers we really need to see randomized control studies - which
is the gold standard for calling an intervention evidence based. Even a prospective case control or
cohort studies would be a good start.”
Sameer Badlani, MD - CMIO – University of Chicago Medicine
CALL TO ACTION
49
Observational studies are appropriate for comparing the eectiveness of apps within a given
classication (e.g. diet and tness, compliance) and for encouraging uptake, whereas RCTs should
be used to demonstrate improved healthcare outcomes from an mHealth strategy (hence not app
specic). In the future since providers will be measured on patient reported outcomes, it will be
essential to have data providing evidence conducive to outcomes based results (See Figure 19).
Figure 19: Evolution of evidence development for ecacy
Observational studies: Although observational studies may not be the gold standard when it
comes to making statements of fact about safety, ecacy, or eectiveness, they provide valuable
data on “real world” use and practice, and help formulate hypotheses to be tested in subsequent
studies. In the current situation where there is a complete absence of evidence, beginning with
observational studies which are feasible and aordable to push on what is known in the world of
mobile health apps is a strong start, and these observational studies will be a useful way to generate
empirical evidence for testing in RCT.
Randomized Controlled Trials: In the short to medium term, work needs to commence on the
design and recruitment for an RCT to demonstrate the overall health outcomes associated with
using mobile apps. To design such a trial there needs to be a consensus on the criteria for evaluation
of apps, with researchers, clinicians, and entrepreneurs freely sharing and debating their work.
A 3-4 year RCT as seen in the development of drugs is wholly unnecessary for mobile apps, but
evidence of behavior change or change in dened health measures in an appropriate time scale are
essential to ensure the eectiveness of the mHealth approach. The trial must be designed with the
appropriate power to isolate the impact of the app from other variables such as the quality of the
patient-physician interaction.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Today: Observational Studies
Short to Medium Term:
Randomized Trials
Medium to Long Term:
Outcomes based results
• Observational studies demonstrate
improved adherence to weight loss plans,
increased adherence to treatment (through
timely Rx lls and medication trackers)
• Several academic papers question ecacy
of apps
• Prospective case control studies of use of
apps at large medical groups
• Multiple randomized control trials which
have sucient power to isolate the impact
of the app from other variables such as
patient-physician interaction
• Widespread demonstration of dened
patient outcomes in a real world setting
• Professional societies base guidelines for
app recommendation on clinical
outcomes data
• Steady stream of peer reviewed mhealth
app publications and clinical trial results

CALL TO ACTION
50
Further it must be recognized that a patient may be using their own online tools regardless of
physician recommendation and hence if one arm is the “app intervention” arm and the other a
“current care” control arm, the control arm must acknowledge that people are likely to passively
use open websites and mobile tools themselves. The key is to know how information, support, and
communication impacts on the patient’s wellbeing and, as such, these longer term RCTs should be
formulated in terms not of a specic app but in terms of a functional assessment of what is needed,
for example, dierent ways of providing information, support and communication.
48
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
“Right now there is scant scientic evidence that apps work. The main, respectable journals have
not published any ‘interesting ‘ peer-reviewed and reproducible results. When they do, you will
have the attention of the medical community. We are taught to trust our journals. Sadly, medical
research has not embraced the technologies that are out there and continue to focus on basic
research and meta-analysis studies - which they should. Doctors are not techno-phobic, they’re
just afraid of new applications without a demonstrable ROI on time and outcomes.”
Jordan Shlain, MD, FACP – HealthLoop Inc.

51
Conclusion
As evidenced by the most detailed analysis of widely available consumer healthcare apps
to date, there has been a tremendous development of mobile apps to assist consumers
and patients in every step of their healthcare management - from preventive measures that
encompass overall wellness, through to adhering to a prescribed treatment regime.
The apps developed to date are supported by a wide range of backers and have very
dierent business models and propositions. They also vary widely in their functional
capabilities.
One of the main challenges stemming from the wide variety of mobile healthcare apps
available is the confusion amongst consumers regarding the most appropriate app to
meet their needs, resulting in a signicant download skew whereby the most downloaded
apps continue to receive the most installs as a result of high review numbers and ratings.
Physicians face the same challenge when they try and recommend an app to a patient.
For healthcare apps to move through a maturity cycle from being an ad hoc
recommendation to a systematic, integrated component of healthcare delivery, all
stakeholders will need to work together. Healthcare payers and providers will increasingly
recognize the potential benet apps can bring, app developers will ensure privacy and
security of patient data, and a concerted eort will be made to evaluate healthcare apps
and to integrate them with other health IT oerings. Moreover, signicant investment
will be made in evidence generation to demonstrate that mobile apps can lead to dened
improvements in health outcomes. Many of these steps will require considerable upfront
investment – meaning there must be an incentive to move apps towards maturity.
One such incentive in developed markets is the ongoing shift to patient centered care
models. Stakeholders need to see patients as responsible and capable partners in
healthcare management - and patient engagement through mobile apps is an exemplary
rst step in this process. Some of the areas where substantial gains can be made in the
healthcare system involve exciting an interest in healthy lifestyles through diet and tness
apps, combined with the potential for remote monitoring and patient collected data being
used to develop the healthcare management program. This could lead to fewer people
contracting chronic conditions and actively adhering to treatment recommendations -
improving patient outcomes at lower overall cost.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

52
Methodology
Count of widely available consumer healthcare apps
All 43,689 apps available for download from the Apple iTunes App store as of June 2013
were scraped from the store and analyzed. A thorough examination of the content of
these apps led to the exclusion of 20,007 apps from further analysis since these were
considered not truly related to healthcare (e.g. salons, apps with gimmicks). Of the
remaining 23,682 apps considered genuine healthcare apps, further content analysis
categorized 16,275 apps as consumer/patient oriented and 7,407 apps as HCP oriented.
A full analysis was only conducted on those apps targeting consumers/patients.
The intention of this analysis was to categorize apps along the full patient journey,
as opposed to other reports which simply grouped apps based on target audience
(women’s health, tness etc). As such a further detailed analysis of the 16,275 consumer
focused apps sought to place them along a patient journey consisting of overall wellness,
diagnosis, HCP visit, further information, prescription lling and compliance; recognizing
also that some apps cover the full patient journey and are intended for specic groups of
patients (demographic specic or therapy area specic).
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
43,689 “Healthcare and Fitness” or “Medical”
23,682 Apps genuine healthcare related
20,007 Mis-categorized or only
loosely healthcare related on App Store
16,275 Consumer/Patient Oriented
7,407
HCP oriented
• Fashion and beauty (e.g. salons)
• Apps intended for members of specic
clubs/universities
• Veterinary apps
• Apps which use gimmicks with no real health
benet (eg apps which make the user sound sick,
or demonstrate how the user would look if they
were obese)
• Apps related to health issues but which do not
focus on health (e.g. fertility)
• Product presentation apps for use by sales
reps/retailers
• Apps believed to have meaningless claims
e.g. “gives you a beautiful way to keep track of your
body's biorhythms”

METHODOLOGY
53
A further 2,032 apps were therefore excluded at this point, although they relate to healthcare
they would not sit on a patient journey (e.g. nding an optician or dentist, specic tness centers
class timetables, cosmetic surgery). This left 14,243 general consumer healthcare apps which
belong on a typical patient journey.
Quality control was built into the mobile app review process. After each app was reviewed,
it underwent a second round of examination by a separate group of reviewers, verifying the
results of the rst review, even if the app was rejected initially. A smaller random set of apps
were selected for a weekly or monthly review. Since each app’s reviewer and date of review was
recorded, any misclassication trends uncovered during the reviews were linked to a specic
individual or time frame and these aected apps were sent for reclassication in their entirety.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
16,275 Consumer/patient targeted genuine healthcare related apps
14,243 Apps can be placed on patient journey
2,032
not
patient health
specic*
Overall Wellness
• Diet and Nutrition
• Fitness and Exercise
• Weight/BMI tracking
• Stress, relaxation and sleep
• Cognition IQ and memory
• Addiction quitting
Diagnosis
• App has built in
functionality to provide
diagnosis based on user
inputted information/
answers
Finding HCP
• Directs user to nearest
HCP/medical facility
• Review and create
ratings for HCPs
• Appointment
reminders
Is it intended for a specic group of
consumers / patients or their caregivers?
• Women’s Health
• Children’s Health
• Senior Health
• Therapy Area Specic
Finding Information
• Healthcare education
and information
• Drug information
• Medical information
• Emergency care
Finding Information
• Healthcare education
and information
• Drug information
• Medical information
• Emergency care
Prescription lling
• Finding a pharmacy
• Prescription rells
• Price checkers
• Polypharmacy
management
Compliance
• Medication reminders
• Medication trackers
• General patient
calculators
* cosmetic surgery, alternative care, opticians,
dentists and specic tness centers

METHODOLOGY
54
Functionality assessment score for consumer healthcare apps
The IMS app functionality score is calculated for the 6 key areas of information, instruction,
tracking and guidance, reminder, communication and use of phone functionality. Each app
undergoes a rigorous assessment for each function. Apps are assessed within use case.
The following criteria are considered:
Information
• Level of detail of information
• Provides information as text
• Provides information as picture
• Provides information as video
• Provides audio information
Instruction
• Provides instructions to the user
Tracking and guidance
• Ability to track and capture user entered data
• Graphically displays user entered data
• Outputs user data
• Can link to sensor
• Provides guidance based on entry
Reminder
• Built in reminder function
Communication
• Uses email
• Uses SMS
• Provides secure communication
• Provides link to social networks
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

METHODOLOGY
55
Phone functions
• Use of phone’s GPS
• Use of phone’s camera
• Use of phone’s scanner
• Use of phone’s voice recorder
The user rating score considers both the number of reviews the app has received on the iTunes
app store and the Google Play store, and the star rating assigned to the app.
Android data download analysis
Data for downloads of Android apps was purchased from AppMonsta in July 2013. This data
provided information including AppID, App name, Category, App URL, Description, Publisher,
Release Date and Downloads, where downloads were quoted in the following ranges: 10 million
to 50 million; 5 million to 10 million; 1 million to 5 million; 500,000 to 1 million; 100,000 to
500,000; 50,000 to 100, 000; 10,000 to 50,000; 5,000 to 10,000; 1,000 to 5,000; 500 to 1,000; 100 to
500; 10 to 50; 5 to 10; 1 to 5.
The median number of downloads was therefore taken for each range from which a total number
of downloads was estimated.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

56
1 Volpp, KG et al. Redesigning employee health incentives –
lessons from behavioural economics. N Eng J Med, 2011; 365 (5).
2 PruHealth UK Vitality Program. Accessed Sept 2013 at
http://pruhealth.pruhealth.co.uk/individuals/live ‐well/about-
pruhealth-vitality
3 Subramanian, C. The Ultimate Weight-Loss Incentive: Dubai
Will Pay Dieters in Gold. Time Newsfeed, July 2013. Accessed at:
http://newsfeed.time.com/2013/07/18/the-ultimate-weight-
loss-incentive-dubai-will-pay-dieters-in-gold/#ixzz2bwy4AdHJ
4 Fox, S and Duggan, M. Health Online 2013. Pew Internet and
American Life Project, 2013
5 mHealth: New horizons for health through mobile
technologies. Global Observatory for eHealth series, 2011.
Volume 3.
6 Gordon, ME. India, China, and the Map to Two Billion
Connected Devices. Flurry Blog. June 2013. Accessed at http://
blog.urry.com/bid/97962/India-China-and-the-Map-to-Two-
Billion-Connected-Devices
7 Wikipedia contributors. “Mobile app.” Wikipedia, The Free
Encyclopedia, 25 Sep. 2013. Accessed Oct 2013 at http://
en.wikipedia.org/wiki/Mobile_app.
8 Our mobile planet: Presented by google. Accessed August
2013 at http://www.thinkwithgoogle.com/mobileplanet/en/
graph/?wave=2013&age=all&gender=all&active=country
9 Khalaf, S. It’s an App World. The Web Just Lives in It. Flurry
ve year report. Apr, 2013. Accessed at http://blog.urry.com/
bid/95723/Flurry-Five-Year-Report-It-s-an-App-World-The-Just-
Web-Lives-in-It
10 Adapted from Center for Technology and Aging, Technologies
for Remote Patient Monitoring for Older Adults, April 2010
11 Quinn et al. WellDoc Mobile Diabetes Management
Randomised Controlled Trial: Change in clinical and
behavioural outcomes and patient and physician satisfaction.
Diabetes Technology and Therapeutics, 2008; 10 (3), 160-168
12 Quinn et al. Cluster-Randomised Trial of a Mobile Phone
Personalised Behavioural Intervention for Blood Glucose
Control. Diabetes Care, 2011; 34, 1934-1942
13 App Annie app store stats. Retrieved Sept 2013 at http://
www.appannie.com/top/iphone/united-states/health-and-
tness/
14 Dembosky, A. Venture capitalists weigh in on MyFitnessPal.
Financial Times. August 2013
15 Mokdad et al. Actual Causes of Death in the United States,
2000. JAMA, 2004; 291(10):1238-1245
16 How Safeway is cutting healthcare costs. Wall Street Journal.
2009. Accessed august 2013 at http://online.wsj.com/article/
SB124476804026308603.html
17 Burke LE et al. Self-monitoring dietary intake: current and
future practices. J Ren Nutr, 2005; 15, 281–90
18 Ferris et al. Diagnostic Inaccuracy of Smartphone
Applications for Melanoma Detection. JAMA Dermatology,
2013; 16, 1- 4
19 http://www.kaiserhealthnews.org/stories/2013/june/18/
doctors-patients-smartphone-apps.aspx
20 Mobile Medical Applications: Guidance for Industry and
Food and Drug Administration Sta. FDA document, Sept 25th
2013
21 http://www.eweek.com/c/a/Health-Care-IT/New-
Mobile-App-Allows-Consumers-to-Compare-Drug-Prices-at-
Pharmacies-132014/#sthash.1KkNf2sD.dpuf
22 http://drugtopics.modernmedicine.com/drug-topics/
news/drug-topics/chains-business/mobile-apps-managing-
health?page=0,0) http://mobihealthnews.com/22686/
walgreens-nds-mobile-customers-to-be-better-customers/
23 http://drugtopics.modernmedicine.com/drug-topics/
news/drug-topics/chains-business/mobile-apps-managing-
health?page=0,0) http://blog.arizonacollege.edu/2013/06/
pharmacy-apps/
24 Cramer et al. Medication compliance and persistence:
terminology and denitions. Value Health, 2008;11(1):44-7
25 Eweek and drug store news http://www.eweek.com/
mobile/mobile-pillbox-app-promotes-diabetes-medication-
adherence-Report/ http://drugstorenews.com/article/
medisafe-project-app-boosts-adherence-rates
26 Kung HC, Hoyert DL, Xu JQ, Murphy SL. Deaths: Final data
for 2005 National Vital Statistics Reports 2008; 56(10). Available
from: http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.
pdf
27 Anderson G. Chronic conditions: making the case for
ongoing care. Baltimore, MD: John Hopkins University; 2004.
References Cited
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

57
REFERENCES CITED
28 Centers for Disease Control and Prevention. Prevalence of
doctor-diagnosed arthritis and arthritis-attributable activity
limitation—United States, 2003–2005. MMWR 2006;55:1089–
1092
29 Aitken, M.; Valkova, S. Avoidable Costs in U.S. Healthcare:
The 200 Billion Opportunity from Using Medicines More
Responsibly. IMS Institute for Healthcare Informatics, June
2013
30 Pew Internet and American Life Project: Smart phone
ownership, June 2013
31 AppMonsta, data purchased June 2013. See methodology
section for analysis description
32 Mobithinking: Global mobile statistics 2013 Section E:
Mobile apps, app stores, pricing and failure rates
33 NHS Commissioning Board launches library of NHS-
reviewed phone apps to help keep people healthy. Accessed
at http://www.england.nhs.uk/2013/03/12/nhs-apps/
34 HealthTap takes on app curation, prescribing,
Mobihealthnews, May 2013. Accessed at http://
mobihealthnews.com/22707/healthtap-takes-on-app-
curation-prescribing/
35 Wicklund, E. Cigna’s new marketplace helps members pick
the right health and wellness apps. mHealthNews, Oct 2013
36 Pew Internet and American Life Project: Cell Phone
Activities Nov 2012
37 Aitken, M et al. Healthcare Spending Among Privately
Insured Individuals Under Age 65. IMS Institute for Healthcare
Informatics, Feb 2012
38 Kernishan, L. How should apps be prescribed? Accessed at
http://thehealthcareblog.com/blog/2013/03/13/how-should-
apps-be-prescribed/.
39 Boyd et al JAMA. 2005;294(6):716-724
40 NBC News Rock Center, Jan 2013: The key to better
health care may already be in your pocket... and it’s not
your wallet. Accessed at http://rockcenter.nbcnews.com/_
news/2013/01/24/16677207-the-key-to-better-health-care-
may-already-be-in-your-pocket-and- its-not-your-wallet?lite
41 Happtique to test its health app prescription
platform, Mobihealthnews, May 2012. Accessed at http://
mobihealthnews.com/17300/happtique-to-test-its-health-
app-prescription-platform/
42 Examples of MMAs the FDA has cleared or approved.
Accessed Sept 2013 at http://www.fda.gov/MedicalDevices/
ProductsandMedicalProcedures/ConnectedHealth/
MobileMedicalApplications/ucm3 68784.htm
43 Moukheiber, Z. Trailblazer WellDoc To Sell First Mobile
Prescription Therapy. Forbes. June 2013. Accessed Sept 2013
at http://www.forbes.com/sites/zinamoukheiber/2013/06/14/
trailblazer-welldoc-to-sell-rst-mobile-prescription-therapy/
44 Mattke et al. Workplace wellness programs study. RAND
Health sponsored by the US Dept of Labor, 2013
45 Carter et al. Adherence to a Smartphone Application for
Weight Loss Compared to Website and Paper Diary: Pilot
Randomized Controlled Trial. J Med Internet Res 2013;15(4):e32
46 California Online Privacy Protection Act
47 Adapted from EU Article 29 Working Party Opinion on Apps
on Smart Devices and its Implications
48 Payne, P. Do mHealth apps require randomized controlled
trials– panel discusses at mHealth Summit. iMedicalApps, Dec
2012
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

58
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
Authors
Murray Aitken
Executive Director, IMS Institute for Healthcare Informatics
Murray Aitken is executive director, IMS Institute for Healthcare Informatics, which provides
policy setters and decision makers in the global health sector with objective insights into
healthcare dynamics. He assumed this role in January 2011. Murray previously was senior vice
president, Healthcare Insight, leading IMS Health’s thought leadership initiatives worldwide.
Before that, he served as senior vice president, Corporate Strategy, from 2004 to 2007. Murray
joined IMS Health in 2001 with responsibility for developing the company’s consulting and
services businesses. Prior to IMS Health, Murray had a 14-year career with McKinsey & Company,
where he was a leader in the Pharmaceutical and Medical Products practice from 1997 to 2001.
Murray writes and speaks regularly on the challenges facing the healthcare industry. He is editor
of HealthIQ, a publication focused on the value of information in advancing evidence-based
healthcare, and also serves on the editorial advisory board of Pharmaceutical Executive. Murray
holds a Master of Commerce degree from the University of Auckland in New Zealand, and
received an M.B.A. degree with distinction from Harvard University.
Carolyn Gauntlett
Senior Consultant, European Thought Leadership
Carolyn is a researcher and project manager in the IMS Health European Thought Leadership
Team, leading the development of reports and analyses focused on biopharmaceuticals and
healthcare in Europe and globally. Carolyn’s primary and secondary market research experience
spans therapy areas including diabetes and oncology, emerging markets, and the yearly
pharmaceutical strategic management review. Carolyn joined the Thought Leadership team
at IMS Health in 2011 and has supported both the North Europe and Central Europe business
units. Prior to IMS Health, Carolyn was a research chemist working both in academia and biotech.
Carolyn began her consulting career at OC&C Strategy Consultants in London, working across
a range of consumer, retail and media projects. Carolyn holds a MA and PhD in Chemistry from
Cambridge University and was a postdoctoral Fulbright Scholar at Stanford University.

59
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.
About the Institute
The IMS Institute for Healthcare Informatics leverages collaborative relationships
in the public and private sectors to strengthen the vital role of information in
advancing healthcare globally. Its mission is to provide key policy setters and
decision makers in the global health sector with unique and transformational
insights into healthcare dynamics derived from granular analysis of information.
Fullling an essential need within healthcare, the Institute delivers objective,
relevant insights and research that accelerate understanding and innovation
critical to sound decision making and improved patient care. With access to
IMS Health’s extensive global data assets and analytics, the Institute works in
tandem with a broad set of healthcare stakeholders, including government
agencies, academic institutions, the life sciences industry and payers, to drive a
research agenda dedicated to addressing today’s healthcare challenges.
By collaborating on research of common interest, it builds on a long-standing
and extensive tradition of using IMS Health information and expertise to
support the advancement of evidence-based healthcare around the world.

60
ABOUT THE INSTITUTE
Research Agenda
The research agenda for the Institute
centers on ve areas considered vital to the
advancement of healthcare globally:
The eective use of information by healthcare
stakeholders globally to improve health outcomes,
reduce costs and increase access to available
treatments.
Optimizing the performance of medical care
through better understanding of disease causes,
treatment consequences and measures to
improve quality and cost of healthcare delivered
to patients.
Understanding the future global role for
biopharmaceuticals, the dynamics that shape
the market and implications for manufacturers,
public and private payers, providers, patients,
pharmacists and distributors.
Researching the role of innovation in health
system products, processes and delivery systems,
and the business and policy systems that drive
innovation.
Informing and advancing the healthcare agendas
in developing nations through information and
analysis.
Guiding Principles
The Institute operates from a set of
Guiding Principles:
The advancement of healthcare globally is a vital,
continuous process.
Timely, high-quality and relevant information is
critical to sound healthcare decision making.
Insights gained from information and analysis
should be made widely available to healthcare
stakeholders.
Eective use of information is often complex,
requiring unique knowledge and expertise.
The ongoing innovation and reform in all aspects
of healthcare require a dynamic approach to
understanding the entire healthcare system.
Personal health information is condential and
patient privacy must be protected.
The private sector has a valuable role to play in
collaborating with the public sector related to the
use of healthcare data.
Patient Apps for Improved Healthcare: From Novelty to Mainstream. Report by the IMS Institute for Healthcare Informatics.

IMS Institute for Healthcare Informatics, 11 Waterview Boulevard, Parsippany, NJ 07054 USA
info@theimsinstitute.org www.theimsinstitute.org
