
Patient Safet
y
& Qualit
y
Patient Safet
y
& Qualit
y
yy
Improvement
Physician & Resident
Handbook
yy
Improvement
Physician & Resident
Handbook
Dr. Brian Murray
Chief Medical Officer, ECMCC
Associate Professor of Internal Medicine
State University of New York at Buffalo
Department of Medicine
E R I E C O U N T Y M E D I C A L C E N T E R C O R P O R A T I O N
Department
of
Medicine
898-3936
2017 – 2018 ed.
Table of Contents
I. Mission, Vision and Values
II. Helpful Tools
Hospital Schematic 4
Phone List 5-7
Policies, Medical Dental Staff Page, Consults 8
Interpreter Services 9
III. Health and Wellness
Duty Hour Rules 11
Fitness Center 12
Flu Shot
12
Flu Shot
12
Wellness Committee 12
Lounges and Call Rooms 13
IV. Quality & Patient Safety
1
8
2
5-27
2
4
Adult Medical Emergency
Antibiograms
Central Line Infection
CMS Core Measures
15-16
Constant Observation (formerly known as 1:1) 40
Consults and Studies 33
Critical Values Reporting – Lab and Radiology 32
Emergency Codes & Active Shooter Safety 19
Fall Reduction Program 46
Forensic Patients 45
Hand Washing & Infection Prevention 20-22
MRI Safety 34
Pain Management Guidelines 38-39
Present on Admission (POA) Conditions 30
Rapid Response Team 17
Restraints 41
Sepsis Bundle Orders
35
-
37
Sepsis Bundle Orders
35
37
Sharp Injury Prevention and Treatment 23
Telemetry Monitoring 31
Transfer of Internal Patients 42-44
Wound Prevention 28-29

Table of Contents (Con’t)
V. Documentation & Discharge Planning
Abbreviations 50
ALC S
61
ALC S
tatus
61
Autopsy Request 56
Case Management/Discharge Planning 62
Death Information Management 55
Discharge Summary & Documentation Reminders53-54
Documentation Improvement (CDI) Program 51-52
EMR Hotline 49
Home Care Services 63
Medication Reconciliation 58
Time Out and Consent 59
Verbal/Telephone Orders 60
VI. Professionalism
Behavioral Expectations &
Effective
Communication
64
67
Effective
Communication
64
-
67
VII. Ethics & Compliance
Compliance and Fraud 78
Family Healthcare Decisions Act 74-76
HepC Testing Requirements 73
HIPAA 71
HIV Testing Law 72
L f T
77
L
imitation
o
f T
reatment
77
Moral Objection 77
Occurrence Reporting (Quantros ©) 70
Risk Management 69
VIII. Programs & Regulations
DSRIP 80-81
I-Sto
p
Le
g
islation 83-84
pg
Patient Centered Medical Home (PCMH 82
I. Mission,
Vision Values
Vision
,
Values
What we strive for

Erie County Medical Center
Mission, Vision and Values
1

Erie County Medical Center
Mission, Vision and Values
2

II.
Helpful Tools
Helpful Tools
Schematic, Phone Lists, Intranet &
Interpreter Services
3
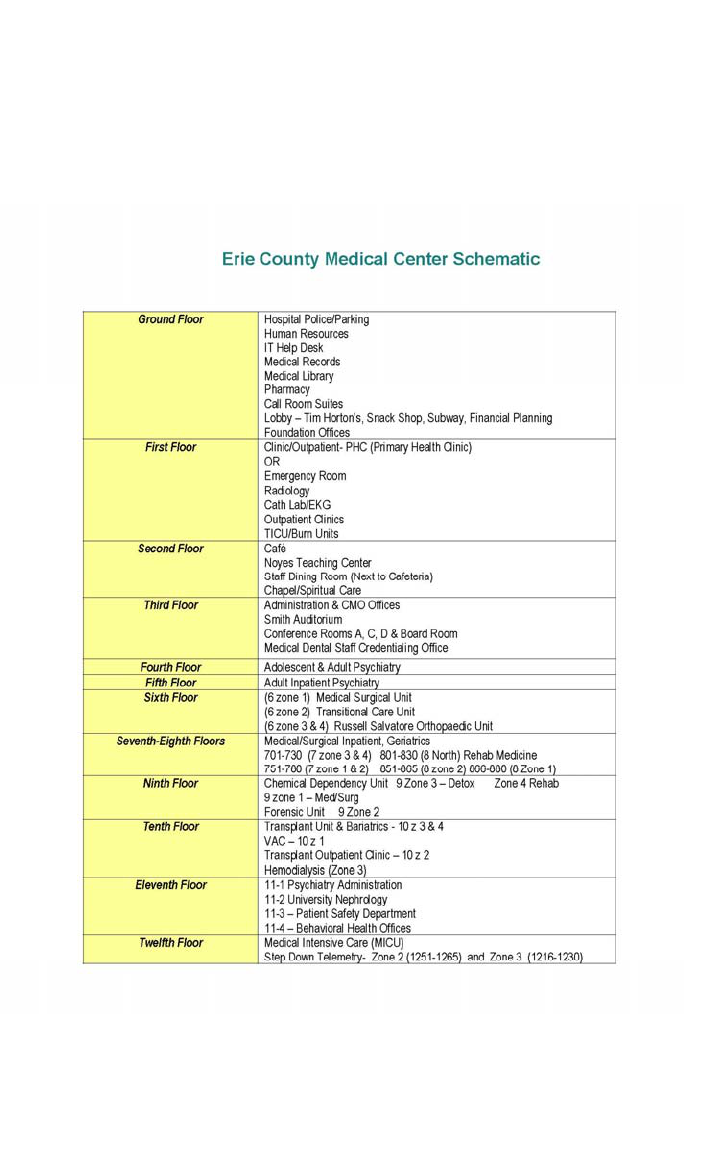
Erie County Medical
Center Schematic
4

AREA/Unit Manager PHONE FAX Manager
6 zone 1 - Lynne Golombek 3005 4863
6 North (Ortho) - Judy Haynes 3609 5397
7 Zone 2 - Renee Delmont (751-765) 4363 6284
7 Zone 3 - Patricia Kiblin
(
716-730
)
3605 5456 4376
Helpful Phone Numbers
()
7 zone 4 - (701-715) Jessica McGuigan 1945 5456 1971
8 Zone 1 - Jeremy Hepburn ( 866-880) 4831 3314
8 North - Jenna DeFilippo 3614 6144 4551
8 Zone 2 - Lisa Hauss 3606 4571
9th Floor - ACC Desk 3685
6 - Zone 2 - Santosha Gompah 5608 5455
9 - Zone 2 - (FORENSIC) - Nicole Cretacci 3621/4409 5455
9 - Zone 3 (Detox) - Shonda Cleckley 3687 5892
9 Z 4 (R h b) Sh d Cl kl
4206
5892
9
-
Z
one
4 (R
e
h
a
b)
-
Sh
on
d
a
Cl
ec
kl
ey
4206
5892
10 - Zone 1 (Inpatient Dialysis) Jamie Repec 4644
10 - Zone 2 (Transplant Center) Pam Riley 5001
10 zone 3 - Inpatient Transplant - Pam Riley
6220
10 Zone 4 - Inpatient T ransplant 6220
Transitional Care Unit (6 z 2) - Mary Molly Shea
3424 3084
Psychiatry Units
4 Zone 1 - Richard Waterstram 3592 4743
4 Zone 2 - Richard Waterstram 3592 4743
4 Zone 4 (Adol. Psych) - Laurie Carrol 5420 4657
CPEP - Donna Gatti 3465/3389 3566
5 zone 3 & 4 (Beh Health)- Denise Abbey 5059 4901
5 South (Beh Health) - Jillian Brown 5728 5817
12 Zone 2 (Rm 1251-65) Pam Riley 3667/4831 5062 4552
12 Zone 3 (Rm 1216-30) - Sonja Melvin 3672 5083 5730
MICU - Tim Kline 3673/3674 3666
Trauma/BURN - 1st Floor
Trauma ICU - Melinda Lawley 6171/3344 5267
Burn Unit - Audrey Hoerner 5231/5232 4378
Operating Room - Jim Turner 6211 6211
OR Reception Desk 4315
OR Staff Lounge 3553/3555
OR Recovery Room 4101/3348
OR Scheduling 4039
One Day Surgery 3654/4315
OR Main Desk 4315
Drs. Messages 4110
OR Preadm./T ests/Surg Holds 4110
EMERGENCY ROOM 5140/5660
Triage 3458/3161
Med/Surg POD 4166/4167
Trauma Corridor 3853
Off Hours/Holidays – Contact the Nursing Supervisor
for assistance at Pager – 642-9215
5

Department of Medicine PHONE
Chief Medicine Resident 4924 P: 642-1550
UB I ti t G i ti C lt S i
4845
S Gl NP
Helpful Phone Numbers
UB I
npa
ti
en
t G
er
i
a
t
r
i
c
C
onsu
lt S
erv
i
ce
4845
S
usan
Gl
ose,
NP
General Phone Numbers
Medical Director Office 3936 FAX
Admissions 3908/3153
AIS/SIU 3471
ARIS (Rehab) 4628
Adv erse Drug Reporting 4000
Autopsy 3520
Biochemistr
y
3532/3442
y
BioMed 3832
Blood Bank 4182/4177
Blood Gas 4184
Cardiology Consults
See intranet
Cath Lab 3386
Code Blue/C ode Stroke 4545
Cy tology 4123
Dietary 3559/3210
Dopplers
5238
Dopplers
5238
EC HO 3388
EEG 3371
EKG 3388
Apogee H ospitalists 6995
GI Office 3391
Family Health Center 4449
Help Desk (IT) 4477 x 5601 for EMR H otline
Hematology 4063
HIV Testing 4119
Immuno Serv ice 4119
Infection Control 3628
CALL SCHEDULES and CONSULT SERVICES
See Intranet Tab
CASE MANAGEMENT
See Phone List on Intranet (Medical Dental Staff Page)
See Phone List on Intranet (Medical Dental Staff Page)
6

Information (Patient) 8020
Internal Med C linic (Primary Health) 3334/3152
IV Team 4273
Library 3939
Laboratory Administration 3114
Hematology
3532
Helpful
Phone
Microbiolog
y
595
6
Parasitology 3535
Serology 4138
Virology 4211
Urinalysis 4056
Medical Dental Staff (Credentialing) 3130/5270
Medical Records 3190
Incomplete Records 5176
Old Medical Records 3917
Numbers
Morgue/H ospital 3520
Neurology C onsults 3638 On Call Page for Schedule
Neuropsy ch Ev als 5182
Nuclear Medicine 3383
Pastoral Care 3357/3356
Pathology 3117/3512
Patient Adv ocate 4155
P
e
r
so
nn
e
l H
ea
lth
3300
eso e ea
3300
Pharmacy 3925/3926
Stat Pharm Line 3286/3282
MetCare/Lobby 332-2866
Pulmonary C onsults 408-3075
Radiology 3446/3468
X-Ray Reports 3446/3468
CT 4040/3659
Ultrasound 3774/5294
ED X-Ray 3433/5905
MRI 5999 ext 1 Tech: 5577
Rapid Response T eam 8888
Rehabilitation 3235/3217
Physical Therapy 3904
PT Hydro 3902
Speech 3212
OT 3225
Renal Office 4803
Rit
3245
R
esp
i
ra
t
ory
3245
Security 3506/3505
Skilled Nursing - Terrace View 551-7100 551-7217
Social Work/DC Planning 3360
Tox icology 3821/3442
Vascular Lab 5238
7

Policy and Procedures &
Medical Dental Staff Webpage
(when restored)
Please use the ECMC Intranet to find current
p
olicies
,
g
eneral
p
,g
info for all Medical Staff on the Med/Dent Staff page, call
schedules and contact information for Consults. The
ECMC intranet page is a primary source for communication for
many of our departments so please use this as a resource.
8

What if my patient doesn’t
speak/read English?
Professional Medical Interpreter Services are available at
no cost to the patient. DO NOT UTILIZE A FAMILY MEMBER
TO INTERPRET FOR YOU. It is essential to ensure proper
medical communication and to protect the patient’s
confidentiality.
Identify Patient
’
s Preferred Language
Identify Patient s Preferred Language
Language ID Card – Cards are available throughout the
hospital and has the phrase “Point to your language. An
interpreter will be called. The interpreter is provided at no
cost to you.” translated in 90 languages and grouped by
geographical regions of the world. A patient may be
given an ID card with preferred language written on it as
well. Stickers can be placed in the chart or on their ID
bracelet.
Interpreter Services
Phones are available throughout the hospital. They
are easy to use and can be accessed quickly through the
nursing staff.
Face-to-Face Services. Deaf Adult Services can be
accessed for sign language and the International Institute
f k l
C t t th ti t d t f
f
or
spo
k
en
l
anguage
–
C
on
t
ac
t th
e
pa
ti
en
t
a
d
voca
t
e
f
or
assistance – 642-7177.
Tips
Record the interpreter’s name and ID in the patient
chart.
Orient the interpreter and the patient
Speak directly with the patient in the first person
(Where is your pain?). Speak in short sentences
Check with the patient for understanding.
9

III.
Health & Wellness
Supporting your practice and your health
10

ACGME Post-Graduate Work
Hour Regulations
ii
- Some
i
mportant po
i
nt
s
All residents and faculty should familiarize themselves with the Work Hour
regulations.
These are some important points to remember.
Maximum duty hours per work week are a maximum of 80 hours
averaged over 4 weeks, inclusive of all in-house activities, clinic
assignments, and moonlighting activities.
Moonlighting – all moonlighting hours worked are included in the total
weekly work hours.
Residents must be scheduled for a minimum of 1 day in 7 free of
li i l k d i d d i h d 4 k A
c
li
n
i
ca
l
wor
k
an
d
requ
i
re
d
e
d
ucat
i
on
w
h
en
average
d
over
4
wee
k
s.
A
t
home call cannot be assigned on these free days.
Mandatory rest/time off between duty periods – all residents must
have 8 hours, should have 10 hours free between scheduled duty
periods. Intermediate level residents must have at least 14 hours free
of duty after 24 hours of in-house duty.
Maximum Duty Period Length – Different for each program year. See
information on the Medical Dental Staff Intranet Page or UB
W
ork Hour Rules policy.
Maximum On Call Frequency – Every third night averaged over 4
weeks; every third night if using surgical exemption.
Night Float Frequency – Residents must not be scheduled for more
than 6 consecutive nights of night float.
If you are required to log into the E-Value system, please ensure you
are logging accurately.
11

ECMC
Fitness Center
The Fitness Center is open 24/7 to Employees, Residents
and Physicians. You can obtain a consent to initiate your FREE access through
the Human Resources Offices located on the Ground Floor.
The Medical Dental Staff maintains a Provider Wellness Committee and is a
resource available for those who may require extra assistance. You may access
this resource via the Chief Medical Officer’s office.
Practitioner Wellness Committee
If you or a colleague are in need of help or support the ECMC Medical Dental
If you or a colleague are in need of help or support
,
the ECMC Medical Dental
Staff Practitioner Wellness Committee is here to assist you. They can provide
resources and/or intervene if a practitioner or resident is in need of further
assistance. Please don’t hesitate to reach out if you feel you need help or
support – we are here to ensure your success!
You may contact committee members via links on
Med/Dental Staff Intranet Page or email [email protected]
http://home.ecmc.local/depts/medicaldental/PractitionerHealth.htm
Flu Shot for you and your patients!
All NYS Hospital Health Workers are required to be vaccinated for flu annually
(or provide evidence of contraindication) or they must wear a face mask while in
the hospital. You may obtain your shot through the Teammate Health Office on
the Ground floor If you get your shot elsewhere please bring evidence and we
the Ground floor
.
If you get your shot elsewhere
,
please bring evidence and we
will give you a sticker for your badge. Please review your patient’s history and if
they have not acquired a flu shot or pneumonia vaccine should that be
warranted, encourage them to take advantage of the vaccine while they are here
either inpatient or in the clinic. Your encouragement goes a long way in
improving patient compliance!
12

For your comfort
and well being
and well being
Physician Lounges –
The medical dental staff and administration
provides a comfortable lounge located in the
rear of medical records on the ground floor.
Thi l i ll b f h
Thi
s
l
ounge
i
s
open
to
a
ll
mem
b
ers
o
f
t
h
e
medical-dental staff and residents. It is
available 24/7 for your use. Refreshments are
served M-F and coffee and tea is available
anytime. Please respect the space and leave it
in the condition you found it so all who need a
rest can enjoy it.
Sil Phii L
i l td
S
urg
i
ca
l Ph
ys
i
c
i
an
L
ounge
–
i
s
l
oca
t
e
d
across from the ORs. It is available for
attendings and extenders only. There is coffee,
newspaper and TV available for your comfort.
For your convenience, the computers in both
lounges are equipped with Dragon for
dictation.
Call Rooms –
Suite is available on the ground floor. Rooms
are assigned by the hospital police office and
are issued for 24 hours.
Some departments such as surgery and ED
h ithi th it
h
ave
rooms
w
ithi
n
or
near
th
e
un
it
–see
your
Chief Resident or Department Manager for
details.
13

IV.
Quality &
if
Pat
i
ent Sa
f
ety
Best Practices and
Guidelines
14

CMS Measures – Best Practices
CMS has identified the following practices as “best practices”. Hospitals are continuously
measured on how they adhere to these guidelines. If particular guidelines cannot be
followed, the reason must be clearly documented in the patient’s chart.
•
ED Throughput
-
ED Arrival to Departure Time & Decision to Admit to Depart Time
ED Throughput
ED Arrival to Departure Time & Decision to Admit to Depart Time
What you can do to meet the measure…Complete your admission orders promptly
and respond quickly to “ED Overcrowding” alerts by writing d/c orders early for
admitted patients.
• Immunization - Influenza Immunization (4Q & 1Q)
What you can do to meet the measure…Have a conversation with your patients on
the importance of flu vaccination – your encouragement helps compliance!
•
Venous
Thromboembolism
Venous
Thromboembolism
VTE Prophylaxis, ICU VTE Prophylaxis, VTE Discharge Instructions,
Potentially Preventable VTE
What you can do to meet the measure…Address and order VTE prophylaxis on
admission – if contraindicated, document in the record.
• Stroke
Thrombolytic for Ischemic Stroke
What you can do to meet the measure: ECMCC is a NYSDOH Designated Primary
Stroke Center We have attained Gold Plus Status in The American Heart and Stroke
Stroke Center
.
We have attained Gold Plus Status in The American Heart and Stroke
Association’s Get With the Guidelines 2016 Program.. When a stroke is suspected,
call a “Stroke Code” to assure guidelines for care are met.
• Complications following elective hip/knee surgeries
• Mortality Rates for AMI, HF, PN, COPD & Ischemic Stroke
What you can do to meet the measure: Utilize order sets for best practice
guidelines and protocols.
• Readmission Rates for HF,PN, COPD, Ischemic Stroke & the whole hospital
What you can do to meet the measure: Patient education is complete pertaining to
their diagnosis, medication and plan of care. Work closely with discharge planning
and social work to ensure a safe discharge for the patient.
Sometimes the recommended intervention may not be appropriate for a particular
ti t (i bl k i th ACEI i
hkli
ti t) I th t th
p
a
ti
en
t (i
.e.,
bl
oc
k
er
i
n
as
th
ma,
ACEI i
n
a
h
yper
k
a
l
em
i
c
p
a
ti
en
t)
.
I
n
th
a
t
case,
th
e
REASON WHY the intervention was not performed must be documented in the
medical record.
15

CMS Measures – Best Practices
Hospital Acquired Infections
To Prevent Catheter-Associated Urinary Tract Infections
(CAUTIs:)
(CAUTIs:)
Insert catheters only for appropriate indications
Leave catheters in place only as long as needed
Insert catheters using aseptic technique and sterile equipment (acute care setting)
Follow aseptic insertion, maintain a closed drainage system
To Prevent Central Line-Associated Bloodstream Infections
(CLABSIs)
Remove unnecessary central lines
Fa
cilitate proper insertion practices
Fa
cilitate proper insertion practices
Avoid femoral route for central venous cannulation (CVC)
Use maximal sterile barrier precautions (cap, mask, sterile gown and sterile gloves)
and a sterile full-body drape while inserting CVCs, peripherally inserted central
catheters, or guidewire exchange
Use appropriate agent for skin antisepsis
To Prevent Ventilator Associated Pneumonia (VAP)
Implement a continuous (24-hour) oral care protocol
El t th h d f b d (HOB) b t l t 30 d
El
eva
t
e
th
e
h
ea
d
o
f b
e
d (HOB) b
y
a
t l
eas
t 30 d
egree
s
Regular (at least once daily) eval of patient’s readiness to wean, including at least
daily sedation vacation
To Prevent Clostridium difficile Infections (CDI)
Contact Precautions for duration of treatment
Comply with CDC hand hygiene recommendations
To Prevent Surgical Site Infections (SSIs):
Before sur
g
er
y
gy
Administer antimicrobial prophylaxis in accordance with evidence-based standards
and guidelines
Avoid hair removal at the operative site unless it will interfere with the operation; do
not use razors
Use appropriate antiseptic agent and technique for skin preparation
During Surgery
Keep OR doors closed during surgery except as needed for passage of equipment,
personnel and the patient
personnel
,
and the patient
After Surgery
Maintain immediate postoperative normothermia
Protect primary closure incisions with sterile dressing
Discontinue antibiotics according to evidence-based standards and guidelines
16

Rapid Response
T
eam
(
RRT
)
()
At ECMC, the RAPID RESPONSE TEAM is
run by the HOSPITALIST (MED H – Apogee
Physicians) service. The resident teams
should respond to assist and provide any
needed su
pp
ort.
A
RR ma
y
be called b
y
a
pp
yy
nurse, provider or a family member who
notes a significant medical change in the
patient.
Do not dismiss the RRT until you are sure
the patient’s needs have been met. Do not
ait to start critical care ntil transfer into an
w
ait
to
start
critical
care
u
ntil
transfer
into
an
ICU – be sure care is administered
immediately and/or as ordered.
Be sure the patient’s condition and treatment
are documented properly in the medical
record. Be sure to time, date and sign your
record.
Be
sure
to
time,
date
and
sign
your
entry.
Please discuss the need to contact the
Health Care Agent regarding the change in
patient’s condition and discuss with the
Attending of Record.
The Rapid Response Team Record will be
completed by the Rapid Response Team and
is included in the medical record.
17

Adult Medical
Emergency
All Internal Medicine residents as assigned by your
department are to report to Adult Medical Emergency
(cardiac/pulmonary arrest) and offer help until the person
running the code dismisses them. The Internal Medicine
resident on call or the Chief Resident is in charge of the
code
code
.
Be sure all patient information is documented in the
medical record. If you are the team leader, you must
review the Adult Medical Emergency Sheet and sign,
date and time your documentation.
If the coded patient is from your team, ensure that the
patient’s family has been contacted and updated on
the patient’s condition and location if transferred to
an ICU.
Refer to the Internal Medicine Program Code Blue policy/
recommendations for further information.
Ensure that the patient’s Attending Physician is notified of
the arrest and its outcome.
Please note: It is the responsibility of the PHYSICIAN
(or Resident) to contact the family/health care agent.
18

Emergency Codes
(now in plain language)
ADULT MEDICAL EMERGENCY
ADULT MEDICAL EMERGENCY
FIRE – Fire Alarm Activation
BOMB THREAT
COMMAND CENTER ACTIVATION
Normal, Monitoring, Partial, Full
DANGEROUS PERSON
EVACUATION
HAZMAT INCIDENT
MASS CASUALTY INCIDENT
MISSING INFANT/CHILD/VISITOR
PATIENT ELOPEMENT
PEDIATRIC MEDICAL EMERGENCY
RAPID RESPONSE TEAM
SECURITY EVENT
STROKE TEAM
SUPPORT TEAM
UTILITY OUTAGE
WEATERH/NATURAL DISASTER WARNING
19

Handwashing &
Infection Prevention
Selling Soap
By STEPHEN J. DUBNER and STEVEN D. LEVITT
The Petri-Dish Screen Saver
In one Australian medical study, doctors self-
reported their hand-washing rate at 73
percent, whereas when these same doctors
were observed, their actual rate was a paltry 9
p
ercent.
Washing your hands every time you enter and exit
a patient room is the single, most effective way of
preventing hospital infections for you and your
preventing hospital infections for you and your
patients.
ISOLATION PRECAUTIONS!!!
Always comply with isolation precautions – use
full gown, gloves to ensure you and your patients
do not come in contact with unnecessary infection!
Be aware – be careful – EVERY TIME!
20

Your 5 moments for Hand
Hygiene
Hygiene
21

All surfaces in a patient
room are susceptible to
contamination!
The Inanimate Environment Can
The
Inanimate
Environment
Can
Facilitate Transmission
X represents VRE culture positive sites
~ Contaminated surfaces increase cross-transmission ~
Abstract: The Risk of Hand and Glove Contamination after Contact with a
Abstract:
The
Risk
of
Hand
and
Glove
Contamination
after
Contact
with
a
VRE (+) Patient Environment. Hayden M, ICAAC, 2001, Chicago, IL.
22

Sharp Injury
Prevention
Eliminate the use of unnecessary needles and sharps.
Properly dispose of sharps in appropriate puncture
it t ti
res
i
s
t
an
t
con
t
a
i
ners.
Maintain constant communication with those in the area
when sharps are used.
Use safety devices - alter user technique to promote
safety
If you are stuck by a contaminated needle
please
If you are stuck by a contaminated needle
,
please
report to Teammate Health Office on the ground floor
7:00 a.m. to 3:00 p.m. or the Emergency Room after
hours for appropriate treatment.
State law protects the rights of THE PATIENT. You may
not have legal rights to know the status of your patient so
the best
p
rotection is PREVENTION. Source
p
atients
pp
have a right to refuse an HIV test and “backdoor” tests (t-
cell counts, p24 antigen, etc) are a violation of the HIV
Confidentiality Law. Patients cannot be pressured to test
and it is never
appropriate for the exposed employee to
approach the source of their exposure about testing.
23

Central Line Infection
• Avoid femoral site when possible.
• Always use Central Line Checklist and Maximum
Barrier Kit which includes: chloraprep. Kits
available on ALL UNITS.
If you plan to send a central catheter
tip for culture…
• Don’t send a catheter tip for culture unless a
catheter-related infection is clinically
suspected; in most cases you should have sent
blood cultures already Culturing a tip is NOT
blood
cultures
already
.
Culturing
a
tip
is
NOT
standard procedure if you are just removing a line
because you are done with it.
• Disinfect the skin around the exit site before
removing the catheter. You can use an alcohol
wipe for this.
C t ff l th f th th t ( t l t
•
C
u
t
o
ff
a generous
l
eng
th
o
f
th
e ca
th
e
t
er
(
a
t
l
eas
t
5 cm) with sterile scissors and drop it into a sterile
specimen container.
24

What is an Antibiogram?
Antibiograms are collections of information obtained from culture and sensitivity tests performed
in the institution within a given time frame (annually at ECMC)
in the institution within a given time frame (annually at ECMC)
Provides the percentage of samples for a given organism which were sensitive to certain
antibiotics
Two files: one for Gram positive organisms and one for Gram negative organisms
What is the purpose of the antibiogram?
To guide empiric antibiotic therapies for suspected bacterial infections based on local
susceptibility data while awaiting culture and sensitivity results
P f i f i l id if f ibi i ibili d k
P
art
o
f i
n
f
ect
i
on
contro
l
measures
to
id
ent
if
y
patterns
o
f
ant
ibi
ot
i
c
suscept
ibili
ty
an
d
trac
k
changes in susceptibility over time. Data can be utilized to:
-improve overall appropriate antimicrobial use
-guide antibiotic Formulary changes or restrictions
How is an antibiogram used?
Numbers on tables represent the percentage of isolates susceptible to a given antibiotic
-
When two numbers are displayed the top number indicates the percent susceptible
When two numbers are displayed the top number indicates the percent susceptible
isolates from non-ICU areas, the lower shows percent susceptible from ICU samples
Numbers in parentheses next to the organism indicates the number of isolates tested
Larger numbers of isolates increases the predictive value for that bug – drug combination
•
What are some limitations of the antibiogram?
Susceptibility limited to specific institutions, not predictive of other hospitals or nursing facilities
Does not account for specific patient history or previous infections
D t id ifi h ki ti d
hdi
ti f ti i bi l
D
oes
no
t
cons
id
er
spec
ifi
c
p
h
armaco
ki
ne
ti
c
an
d
p
h
armaco
d
ynam
i
c proper
ti
es
o
f
an
ti
m
i
cro
bi
a
l
s
–
will the drug kill the bug where the bug lives
-Site of infection should still be considered as well as predicted drug concentrations
-Rapid resistance may be seen of specific pathogens to antibiotics
oi.e. Fluoroquinolones and MRSA
Miscellaneous information
Only initial isolates are included to prevent bias of data
Only initial isolates are included to prevent bias of data
Fewer than 30 isolates may skew data and create statistically insignificant results
Only clinically relevant “bug-drug” combinations are assessed
Patient specific characteristics always outweigh the use of the antibiogram
Antibiogram should be utilized to guide empiric therapy in conjunction with clinical judgment
Culture and sensitivity results should guide definitive therapy
Refer to Department of Pharmacy Therapeutic Pearls / Guidelines for additional information
-http://home.ecmc.edu/depts/pharmacy/Pearls.htm
25

Gram Positive
Antibiogram
26

Gram Negative
Antibiogram
27

28

At least once per week, need to examine wound, review nursing
documentation, indicate if you agree with staging and plan of wound care.
Document -
Treatment/interventions, Patient’s response,
Compliance, Noncompliant, Refusing interventions/treatment/care
29

The following conditions are deemed
‘
preventable
’
by Medicare. If your
Present on Admission (POA)
The
following
conditions
are
deemed
preventable
by
Medicare.
If
your
patient has any of these conditions on admission, it is important for the
PHYSICIAN to document these conditions on admission
. Failure to
document on admission may cause the condition to
be attributed to your care.
•
Catheter-associated UTI
Decubitus ulcers
Vltht
itdif ti
•
V
ascu
l
ar ca
th
e
t
er-assoc
i
a
t
e
d
i
n
f
ec
ti
on
• Mediastinitis after CABG
• Ventilator-associated pneumonia
•DKA
•PE
• Staph aureus septicemia
•Object left in during surgery
• Air embolism
Bl d i tibilit
•
Bl
oo
d
i
ncompa
tibilit
y
•
Latrogenic pneumothorax with venous catheterization
• Surgical site infection following certain orthopedic procedures (i.e.,
spine, neck, shoulder, elbow, hip, knee)
• Surgical site infection following bariatric surgery for obesity
•
Surgical s
ite infection following cardiac implantable electronic device
Documenting on the H & P is essential and must
be done by the physician, not by nursing in order to
be considered POA. Please be sure you are aware
of these conditions and look for them upon
examination and admission of the patient.
30
Falls and Trauma
Manifestation of Poor Glycemic Control
New ---

As telemetry tends to be over-utilized, we ask that you please evaluate patients who
are placed on telemetry on a daily basis and discontinue as soon as possible.
Excessive use of telemetry monitoring can lead to decompensation as it restricts
Telemetry Monitoring
patient’s mobility. As soon as your medical discretion allows, please discharge
patients from telemetry to avoid unwarranted monitoring. The need for continued
telemetry should be discussed with the attending on daily rounds.
It is NOT appropriate to discontinue telemetry monitoring for the purpose of taking a
patient off-unit for a test or study. When test or study is ordered, the following will
occur:
1. A Floor Nurse will accompany the patient if staffing allows.
2. If the Floor Nurse is unable to leave the unit, the charge nurse is to be
contacted by the nursing staff to see if other arrangements can be made. If
needed, the Charge Nurse will contact the nursing supervisor for further
assistance.
3. In extreme circumstance where no nursing staff is available or if patient
acuity warrants, the resident or extender may be required to accompany the
patient for the test or study. Before doing so, please confirm nursing
supervision has been contacted and is unable to provide support.
Guidelines for discontinuing telemetry in patients suspected of Myocardial
Infarction / ACS
All parameters must be met:
o With negative cardiac enzymes
o No furthe
r
chest pain
suggestive of cardiac ischemia
o Normal potassium level
o No hypotension or ventricular arrhythmias
o No EKG changes (2 EKGs unchanged)
31

Critical Values Reporting – LAB
Critical Values Reporting
o Requirement: All values defined as critical by the laboratory are
reported to a responsible licensed caregiver within time frames
established by the laboratory (defined in cooperation with nursing
and medical staff).
o
All critical lab values are reported to the physician
and
the nurse
o
All critical lab values are reported to the physician
and
the nurse
caring for the patient. You may receive an additional call from the
nursing staff to be sure you have received this urgent report.
o Critical Values Reporting –
Radiology/Imaging
o Radiology Critical Value Reporting-
A
ll critical radiologic values
are reported to the ATTENDING OF RECORD. A color code
system is used to alert the status of the finding:
o Red – patient is in imminent danger of death, significant
morbidity or serious adverse consequences unless
treatment is initiated immediately.
o Orange – requires prompt attention, although do not reflect
a potential immediate life
threatening condition
a potential immediate life
-
threatening condition
.
o Yellow – Significant abnormality that may threaten life – are
targeted at diseases that merit rapid detection and
evaluation.
o See policy: Radiology Critical Test/Critical Value
Communication Policy (RAD-109) - under the Radiology section
of the Policy and Procedures section of the intranet
of the Policy and Procedures section of the intranet
.
32

All consults and studies ordered must include the
clinical information and/or indication.
Consults and Studies
Request should also indicate whether you need a
consult only
or to consult and manage for a
condition (e.g., diabetes).
All elective consults should be
ordered or approved
All elective consults should be
ordered or approved
by an Attending Physician.
STAT consults – please provide an immediate
contact to the attending physician ordering (such as
Cell number) for the consulting service along with
the major concern/diagnosis for the consult.
All contact information for consult services are
located on the intranet under “Consults”.
33

MRI Safety
Wheeled IV pole with
infusion pumps flew into
the bore of this magnet. If
there had been a patient
there had been a patient
on the scanning table, the
patient could have been
severely injured.
Image used with permission of Moriel
Ness Aiver, PhD,
www.simplyphysics.com .
• MRI Ordering – Please make sure you
complete the MRI Safety Checklist
when ordering an MRI study to assure
patient safety in the magnet The
patient safety in the magnet
.
The
checklist prints automatically when the
test is entered into the Meditech
system. Use caution when entering
the MRI suite as the MAGNET IS
ALWAYS ON
ALWAYS ON
.
34

Sepsis bundle orders are available under ‘Sets’ in CPOE. The order set
includes general information regarding goals of therapy, laboratory and microbiology
orders, IV access orders, IV fluids, and antimicrobials by suspected source of
infection. As with all order sets, some suggested components are pre-checked,
d th bl t b i l d d/ dit d i dditi
Sepsis Bundle Orders
an
d
o
th
ers
are
a
bl
e
t
o
b
e
i
nc
l
u
d
e
d/
e
dit
e
d i
n
a
dditi
on.
All providers are encouraged to use the Sepsis order set to initiate
management of patients suspected to have sepsis/septic shock. Using the
sepsis bundle orders will help streamline the ordering process to ensure all
components of the sepsis bundles are met in a timely manner according to the
guideline. This includes obtaining appropriate diagnostic studies, administering
adequate IV fluids, and administering timely antibiotics after obtaining microbiologic
lt
cu
lt
ures.
Sepsis Bundles:
TO BE COMPLETED WITHIN 3 Hours:
• Lactate level
• Blood cultures prior to antibiotics
• Broad-spectrum antibiotics
• 30 mL/kg crystalloid for hypotension or lactate ≥ 4mmol/L
TO BE COMPLETED WITHIN 6 HOURS:
• Vasopressors (hypotension not responding to initial fluid resuscitation)
to maintain a MAP ≥65 mm Hg.
• Persistent arterial hypotension despite volume resuscitation (Septic Shock)
or initial lactate ≥ 4mmol/L:
-Measure CVP (Target ≥8 mm Hg)
-Measure Scvo2 (Target ≥70%)
Remeasure lactate if initial lactate was elevated(Target normalization)
The Sepsis Committee will continue their efforts to monitor treatment and
outcomes of septic patients, while improving compliance with requirements set forth
by CMS and New York State’s Sepsis Regulations.
A nursing order will also be generated to notify the RN that the sepsis orders
are being initiated. All first doses of antibiotics should be dispensed and
administered as STAT orders as indicated in the comments section of the
medication label
medication label
.
Sepsis bundles can be found under “STANDARD ORDER SETS”, “CRITICAL
CARE”, “MEDICINE” and “ED CPOE”. Please see next pages for a step-by-step
ordering process example.
35

Sepsis Order Sets
36

Sepsis Sample Order
37

Pain Management
Resources
Mandatory Prescriber Education
Pursuant to Public Health Law (PHL) 3309-a(3), prescribers licensed under Title
Eight of the Education Law in New York to treat humans and who have a DEA
registration number to prescribe controlled substances, as well as medical residents
who prescribe controlled substances under a facility DEA registration number, must
complete at least three (3) hours of course work or training in pain management,
palliative care and addiction The course work or training must be completed by
palliative care
,
and addiction
.
The course work or training must be completed by
July 1, 2017, and once every three years thereafter.
For additional detail, a listing of approved courses and the process to file an
attestation of course completion with the New York State Bureau of Narcotic
Enforcement, visit their website at:
http:/www.health.ny.gov/professionals/narcotic/docs/mandatory_education_guidance.pdf
-or-
wwwwww.hhealtealthh.nyny.gov/gov/pprrooffessiessiononal/al/nnararccoottiicc
General Principles of Pain Management
1. Speak to the patient about the presence of pain and the effect of the
prescribed medications.
2. Consider patient comfort and avoid IM administration of opioids when possible.
3. Treat persistent pain with scheduled medications. Controlled release oral
prepa
rations are typically dosed every 12 hours and therefore
can eliminate
the need for
administration during sleeping hours.
4. Utilize only immediate release medications for PRN rescue dosing. Dose PRN
medications to the
pain scale being utilized for the patient (i.e., Lortab
5/500
one
tablet q 4 hours as needed for pain 1-5, 2 tablets every 4 hours for pain 6-
10)
10)
5. Transdermal Fentanyl is often not recommended for the treatment of acute
pain due
to delayed onset of effect.
38

Pain Management
DOSING AND CONVERSION CHART FOR OPIOID ANALGESICS
D
RUG
E
QUIANALGESIC
O
RAL
D
OSE
E
QUIANALGESIC
P
ARENTERAL
D
OSE
S
TARTING
D
OSE
A
DULTS
≥ 50
KG
O
RAL
P
ARENTERAL
Morphine
1
30
MG Q
3-4
H
10
MG Q
3-4
H
15-30
MG
3-4
H
10
MG Q
3-4
H
C
ODEINE
2
130
MG Q
3-4
H
75
MG Q
3-4
H
60
MG Q
3-4
H
60
MG Q
2
H
IM
OR
SQ
F
ENTANYL
0.1
H
YDROMORPHONE
7.5
MG Q
3-4
H
1.5
MG Q
3-4
H
6
MG Q
3-4
H
1.5
MG Q
3-4
H
H
YDROCODONE
30
MG Q
3-4
H
N
OT AVAILABLE
10
MG Q
3-4
H
N
OT AVAILABLE
L
EVORPHANOL
4
MG Q
6-8
H
2
MG Q
6-8
H
4
MG Q
6-8
H
0.04
MG
/
KG Q
6-8
H
M
EPERIDINE
300
MG Q
2-3
H
75
MG Q
3
H
N
OT RECOMMENDED
100
MG Q
3
H
M
ETHADONE
20
MG Q
6-8
H
10
MG Q
6-8
H
20
MG Q
6-8
H
10
MG Q
6-8
H
O
XYCODONE
20
MG Q
3-4
H
N
OT AVAILABLE
10
MG Q
3-4
H
N
OT AVAILABLE
O
XYMORPHONE
N
OT AVAILABLE
1
MG Q
3-4
H
N
OT AVAILABLE
1
MG Q
3-4
H
CALCULATING THE RESCUE DOSE
Calculate 10% of the provided total daily opioid dose as an immediate-release formulation.
1
Morphine, Hydromorphone, And Oxymorphone, Rectal Administration is an alternate route for
patients unable to take oral medications, but equianalgesic doses may differ from oral
and parenteral doses because of pharmacokinetic differences
and parenteral doses because of pharmacokinetic differences
.
2
Caution: Codeine doses above 65 mg often are not appropriate, due to diminishing incremental
analgesia with increasing doses but continually increasing constipation and other side
effects.
(excerpt)
CDC Guideline for Prescribing Opioids for Chronic Pain – United States, 2016
Recommendations & Reports/March 18, 2016 (we recommend review of entire
document either on the CDC Website or on the Medical Dental Staff Intranet page)
Determining When to Initiate or Continue Opioids for Chronic Pain
1. Nonpharmacologic therapy and nonopioid pharmacologic therapy are
preferred for chronic pain. Clinicians should consider opioid therapy only expected
benefits for both pain and function are anticipated to outweigh risks to the patient. If
opioids are used they should be combined with nonpharmacologic therapy and
opioids are used
,
they should be combined with nonpharmacologic therapy and
nonopioid pharmacologic therapy, as appropriate.
39

Constant
Observation
Constant Observation is ordered for Medical Surgical patients
who may be a danger to self or others. Constant Observation
requires the patient to be in full visual contact by the assigned
caregiver. Constant Observation may be assigned as a 1:1 or 1:2
staff to patient ratio as ordered/determined by the psychiatrist.
The observer will document observations of the patient behavior
every 15 minutes on the Patient Observation form
every 15 minutes on the Patient Observation form
.
Constant Observation may be ordered initially by the Medical
Surgical Services. The service will place an order for a routine
psychiatric consult. The consult will be performed as soon as
possible, but within 24 hours of the consult being ordered. The
consultant psychiatrist will determine the need for ongoing
Constant Observation. If the physician deems a Stat consult is
needed, the physician must call CPEP and discuss the case with
the attending on duty The order for Constant Observation must
the attending on duty
.
The order for Constant Observation must
be reviewed every 24 hours. In an emergent situation, the RN
may initiate Constant Observation, pending the provider’s
assessment of the patient; if the provider is not readily available,
the RN will call a Rapid Response. The provider/rapid response
team will assess the need for the Constant Observation and write
the initial order if indicated. The RN will notify the supervisor on
call to inform them of the order for Constant Observation.
F ll i th li i l t b hi t i t th
F
o
ll
ow
i
n
g th
e
c
li
n
i
ca
l
assessmen
t by
a
ps
y
c
hi
a
t
r
i
s
t
,
th
e
psychiatrist will determine if the patient requires the ongoing need
for observation and the level of observation required: 1:1
observation or 1:2. When it is determined that the patient no
longer requires CO, the order will be discontinued.
Please see policy NUR-086 – “Constant Observation for
Medical Surgical Patients” for the full policy and procedure.
(
Located on the ECMC Intranet under “Policies”
)
.
()
40

USE OF
RESTRAINTS
RESTRAINTS
Physical restraints are extremely dangerous and should be
used only in exceptional circumstances
. They should not be
used as a substitute for evaluation and treatment of the
underlying cause of the patient’s condition and should be used
only after other less restrictive approaches have failed to
t l th ti t’ b h i diti
con
t
ro
l th
e
pa
ti
en
t’
s
b
e
h
av
i
or
or
con
diti
on.
Make a face-to-face assessment of the patient as to the cause
of their behavior /condition and document this either in the
space provided on the restraint order form (see attached)
which is preferred or in the progress notes with a note that is
dated and timed.
Notify the patient’s attending physician and document this
notification (also can be done on the restraint order form).
If restraints are applied by the nursing staff in an emergency
situation the treating physician must respond as soon as
possible to write the order and perform the assessment but no
later than 30 minutes.
For restraints applied for medical/surgical indications the order
is good for up to 24 hours provided the restraints are not
removed during that period. If there is a continued need for
restraints beyond 24 hours then a new order and assessment
i i d
i
s
requ
i
re
d
.
If restraints are discontinued and there is a need to reapply
restraints a new order and assessment is needed even if this
occurs within 24 hours of the previous order.
If the form of restraint is changed (e.g. 4-point to Canopy
Bed) then a new order and assessment is required.
PLEASE NOTE: Mitts ARE a form of restraint.
See Policy: RESTRAINTS
–
#CLIN-002.
41

Transfer of Internal Patients between
Clinical Services
(refers to policy #MS-001)
Patient Care Transfer Procedure
1. Physicians or teams desiring to transfer a patient to another service need to
first have that team accept the transfer. This is preferably done at an
Attending-to-Attending level but may be initiated by extenders or residents.
2. House staf
f
or extenders should have discussed the case with their
Attending before initiating a transfer. The receiving team should then
consult with their Attending. IN THE EVENT THAT THE TRANSFER IS
DENIED, THE REFUSAL TO ACCEPT IS TO BE MADE ATTENDING-TO-
ATTENDING ONLY. If the patient is accepted, that can be conveyed at an
extender/resident level. Transfers out of the medical or surgical ICUs
cannot be declined. In the event a service feels that the transfer from an
ICU is inappropriate, the Service Attending should contact the Chief
Medical Officer.
3. On acceptance, the referring service should dictate a discharge
summary/transfer note to summarize the patient’s course to that point
unless the patient has been in-house or on that service for <72 hours.
Transfer orders must be written and receiving team must be notified that the
patient has been transferred and is now their responsibility. In addition, all
transfers between different services will require a verbal provider to
provider handoff. When there is a delay between transfer of service and
p
h
y
sical transfer o
f
p
atien
t
from critical care to an in
p
atien
t
floor
,
the
py
p
p
,
transferring team must then call the receiving team to advise them the
patient is being moved to a new location.
4. Transfer orders must be completed electronically through CPOE (except
when and where this functionality is unavailable in which case they can be
written).. VERBAL/TELEPHONE ORDERS FOR TRANSFER ARE NOT
ACCEPTABLE. The receiving team should then see the patient, review the
transfer orders and make any changes they feel are indicated.
5. I
t
is the res
p
onsibilit
y
o
f
the referrin
g
service to communicate the transfer
py
g
plan to the family/significant other. When possible, it should be the
Attending of the referring service.
Transferring
Patient
42

Transfers from Floor to
Medical Intensive Care Unit
1. Such transfers will be initiated by requesting an ICU consult for possible
transfer to the MICU service. MICU consults should be requested by paging
the Hospitalist Provider on-call 642-8779, discussin
g
thecaseandthespecific
reason for the consult. Please note, unless the patient is in extremis, house
staff or extenders should discuss the patient with their Attending before
requesting an ICU consult.
2. MICU service will see and assess the patient. If accepted, transferring service
will be responsible for dictating a transfer summary, summarizing patient care
to that point (unless patient has been in-house for <72 hours).
3. Responsibility for caring for the patient will remain with the referring service
until actual transfer to the MICU bed and in mos
t
cases will require continued
presence of a team member with the patient until they are transferred
physically to the MICU bed when a direct face-to-face handoff can occur to the
MICU service.
4. MICU service will then write the MICU admission orders.
5. If MICU service feels transfer to MICU is not indicated, THIS SHOULD BE
CONVEYED BY THE MICU ATTENDING TO THE RELEVANT SERVICE
ATTENDING. The exception to this is when the attempt to transfer occurs
durin
g
the 11:00 pm
–
7:00 am shift in which case the reason for den
y
in
g
transfer should be conveyed the following morning.
6. Transfers post codes: In general, medical patients who code on the floor will be
admitted to the MICU. The physician who runs the code should stay with the
patient until they are physically transferred to an ICU bed and then hand off
face-to-face with the MICU physician/extender. MICU service will be
responsible for such patients even if the only available bed is in a non-medical
ICU UNIT e.g. Trauma, Burn or CTU.
7. In the case o
f
patients on sur
g
ical services who code, the
y
should be admitted
to the Surgical ICU. If the Surgical ICU Attending feels that the patient would
be more suited to be treated on the MICU service, his/her team should contact
the MICU service and request a transfer as outlined above. Surgical ICU
service will remain responsible for the patient until such time as patient is
accepted by MICU service.
8. It is the responsibility of the referring service to communicate the change
in the patient’s clinical status and the transfer to the family/significant
Transfer of Internal Patients between Clinical Services
(refers to policy #MS-001)
othe
r
. When possible, it should be the
A
ttendin
g
o
f
the referrin
g
service.
43

Transfers from Floor to
Trauma (Surgical) Intensive Care Unit
1. In general, patients admitted to the Surgical Intensive Care Unit will come
throu
g
htheEmer
g
enc
y
Departmen
t
or be transferred from the Sur
g
ical Floor
services. Transfers from other services will generally only occur after the
patient is first seen in consultation by a surgical service or after a patient has
required an operative procedure. In either case the surgical service caring for
the patient will arrange for appropriate ICU admission.
2. Transfers to the Surgical Intensive Care Unit are generally arranged by
contacting the ICU resident /extender. (2nd Year for Burn, 3
rd
year for trauma,).
3. Since these patients are either already on a surgical service or have been seen
in consultation b
y
such a service no transfer summar
y
is
g
enerall
y
needed.
4. Responsibility for caring for the patient will remain with the referring service
until actual transfer to the Surgical Intensive Care bed and in most cases will
require continued presence of a team member with the patient until they are
transferred physically to the ICU bed.
5. The ICU resident/ will then write the ICU Admission Orders.
6. It is the responsibility of the referring service to communicate the change in the
patient’s clinical status and the transfer to the family/significant other. When
possible, it should be the
A
ttendin
g
o
f
the referrin
g
service.
7. Inpatients initially admitted to a Medical Service who require surgery will return
to the service of origin post-operatively except if they are admitted to TICU or
accepted in transfer by the surgical service. Once they no longer require TICU
care, transfer back to the service of origin will occur as in Section III.
Transfer of Internal Patients between Clinical Services
(refers to policy #MS-001)
44

New York State Forensic
Patients
-
Reminders
Patients
-
Reminders
Wende Correctional Facility security coverage can be contacted in
the 9
th
floor lockup at ext. 3863 or 937-4000, ext. 5200 off hours.
Dept of Corrections security officers must be able to maintain
visual contact with their inmate patients at all times. They are
bound by confidentiality rules.
Do not advise an inmate patient of the date of a scheduled
procedure; follow up visit, admission or discharge.
Do not leave any medical tools or equipment within reach of an
inmate patient. Be aware of what you have in your lab coat/shirt
pockets. Inmate patients may use these items to cause injury to
you or others. Pagers, cell phones, syringes, scissors, percussion
hammers and other sharp objects are coveted items. Please check
for your belongings after examining an inmate patient and
immediately report any suspected loss to security personnel.
Do not share any personal information with an inmate patient.
No items are to be given to or received from an inmate unless
approved by the security staff.
Do not make personal phone calls or send emails on the behalf of
an inmate.
Medical staff may share medical information with the inmate
patient’s family utilizing the same privacy regulations employed
when communicating with the families of non-prisoner patients.
Inmates who are admitted to ECMC may have visitors and must be
approved by the DOC security staff
approved by the DOC security staff
.
45

“Catch a Falling Star”
Patient Falls & Fall
Reduction Program
“Catch
a
Falling
Star”
Patients are assessed every shift using the
Hendrich II Assessment Tool
Risk Assessment in the EMR under Care Trends
(Safety Panel) – Score of 5+
Patient assessed as a 5+ risk will be issued a red
itb d
tlttfffikOttit
t
wr
i
s
tb
an
d
t
o a
l
er
t
s
t
a
ff
o
f
r
i
s
k
.
O
u
t
pa
ti
en
t
s
–
s
t
ar
affixed to front of chart
Please be careful with diuretics and medications
that cause sedation. Assess patients for fall risk
accordingly.
Make sure any outside rails are up after
examining patients and bed is in low position
examining
patients
and
bed
is
in
low
position
.
Restraints are not to be ordered to prevent falls.
For patients in acute substance withdrawal, there is
an order set available that is evidence-based and
recommended to treat the patient’s symptoms and
reduce falls.
“
Constant Observation
”
must
be authorized by the
Constant
Observation
must
be
authorized
by
the
administrator or administrator on call. Orders
written for these type observations without
authorization will not be accepted.
Patient’s provider will be notified of every fall.
In the event of a fall, the physician is to notify
p
atient famil
y
(
if
p
atient is co
g
nitivel
y
im
p
aired
)
p
y( p g y p )
promptly of condition of patient and if any injury was
sustained.
Patient fall, assessment and condition as well as
family notification must be accurately documented
in the progress note by the provider.
46

47

V.
Documentation &
Di h g Pl i g
Di
sc
h
ar
g
e
Pl
ann
i
n
g
Ensuring the safety of our patients with
quality documentation and discharge
48

EMR – Training is required on both
Meditech and AllScripts
–
please ensure
EMR Training
Meditech and AllScripts
please ensure
you have attended training prior to your
rotations.
49

Dangerous AbbreviationsDangerous Abbreviations
Abbreviations located on the ECMCC
Intranet under the Abbreviations tab,
Never Use MUST WRITE
QD
Dil
left side. http://home.ecmc.edu/abbrev.htm
QD
D
a
il
y
QOD Every Other Day
UUnits
IU
International Units
IU
International Units
µg
Micrograms
AU Both Ears
AS
Left Ear
AS
Left Ear
AD Right Ear
TIW Three times a week
MS/MSO
MgSO
Write out drug name
MS/MSO
4/
MgSO
4
Write out drug name
DO NOT MAKE UP YOUR OWN ABBREVIATIONS or
use Texting abbreviations. Only hospital approved
abbreviations are permitted.
50

The purpose of the Clinical Documentation Improvement program is to
create a clear picture of the patient’s hospital stay to anyone who picks
up the chart, to accurately code the chart, and to capture CCs and
MCCs that are a
pp
ro
p
riate for
y
our
p
atient while the
y
are in the
Clinical Documentation Improvement
pp p y p y
hospital.
CC – co-morbidity/complication. Impact reimbursement on a
chart, justify length of stay, impact mortality rates and
increase case mix index.
MCC – major co-morbidity. Significantly impact
reimbursement and length of stay.
Clinical Documentation Specialists (CDS) do a concurrent chart review
on ever
y
in
p
atient in order to clarif
y
documentation for coders. A coder
yp y
has guidelines they must follow, and cannot code a diagnosis based on
what’s written in the chart, it must be documented as a diagnosis. For
example, if the physician writes “transfuse 2 units of PRBC for low
hemoglobin,” for a patient with a GI bleed, a coder can only code
ANEMIA but if physician lists for “Acute blood loss anemia” that code
carries a higher complexity and leads to more appropriate levels of
reimbursement for the hospital. This is an opportunity for a CDS to
q
uer
y
.
qy
Specialists will send an electronic query via Cortext (texting app):
Respond to the query in the Medical Record (Progress Note,
Discharge Summary). Do not answer on Cortext
as this is not part of
the permanent medical record. If you disagree with the query, please
let the CDS know via Cortext. They may place a query in the paper
chart like the below sample.
51

Use these terms when documenting
conditions listed
Documentation Tips
Specificity
Document the reason for admission; if it’s a symptom, document probable/possible cause in differential
Document every condition impacting patient’s stay, including chronic conditions
Medications and treatments should be linked to a diagnosis
Acute vs. chronic
Etiology of condition
Proper staging of chronic conditions (CKD)
Benign vs. malignant when neoplasm involved
Congestive heart failure – specify if it is acute/chronic, systolic/diastolic
Diabetes – Always specify it simply as CONTROLLED or UNCONTROLLED. Avoid qualifying terms such as
“poorly controlled” as CMS considers this controlled, NOT uncontrolled. Specify Type I or Type II.
Specify severity and type of malnutrition
Clinically significant diagnoses from diagnostic reports should be documented in the progress notes
Arrow, plus signs, and many abbreviations are not sufficient documentation, must use a diagnosis
For Anemia, always document the cause (i.e., due to blood loss, iron deficiency, etc.)
Common MCCs
Acute diastolic heart failure
Acute pulmonary edema
Acute respiratory failure
Acute renal failure due to acute tubular necrosis
Grand mal seizure
Hypovolemic shock
Pneumonia
Quadriplegia
Acute renal failure due to acute tubular necrosis
w/documented cause
Acute systolic heart failure
AIDS
Anoxic brain damage
Aspiration pneumonia
Decubitus ulcer stage 3 & 4 present on admit
Encephalopathy
Quadriplegia
Sepsis
Septic Shock
Septicemia
Severe malnutrition
Severe protein calorie malnutrition
SIRS
Common CCs
Acidosis
Acute coronary syndrome (unstable angina)
Acute Renal Failure
Drug dependence, continuous
Drug withdrawal
Hemiplegia
Acute Renal Failure
Acute blood loss anemia
Alcohol withdrawal
Alkalosis
Chronic diastolic heart failure
Chronic kidney disease – Stage IV or V
Chronic respiratory failure
Chronic schizophrenia
Chronic systolic heart failure
COPD, acute exacerbation
Hemiplegia
Hyperkalemia
Hypernatremia
Hyponatremia
Morbid obesity, BMI >40
Paraplegia
UTI
52

Discharge Summary
Use the Documentation Template that starts
with your services name
(EX: BH – DC SUMMARY) :
•All discharge documentation is done within
M dit h D t ti (PDOC)
M
e
dit
ec
h D
ocumen
t
a
ti
on
(PDOC)
•Discharge Procedure must be completed and
finalized before starting DC Summary. (This
includes: Medication Reconciliation and
Discharge Instructions
•In DC Summary, click on MEDS tab and
update scripts. This will pull the information
f Dih Itti
f
rom
your
Di
sc
h
arge
I
ns
t
ruc
ti
ons
53

Documentation
Reminders
Please be very careful when using the “Cut and Paste” tool
within a progress note. As a general rule, every note must be
unique and contain appropriate and pertinent information
reflecting the care the patient received that day. Inappropriate
use of the cut and paste will can lead to fraudulent documentation
use of the cut and paste will can lead to fraudulent documentation
and cloning of the note and are strictly forbidden. It is important
to keep in mind that the daily progress notes must reflect a
timeline of the care the patient received further necessitating the
requirement that daily pertinent information is included and that
cutting and pasting should be avoided.
Patient record entries should be documented at the time the
treatment you describe is rendered
treatment you describe is rendered
.
If you are called to see a patient for a change in condition after
you have compiled your daily progress note, always input an
additional note.
Abbreviations and symbols in the patient record are permitted
only when approved according to hospital and medical staff
bylaws, rules and regulations. Avoid using any “texting”
abbreviations
abbreviations
.
All entries in the patient record are permanent.
All originals must stay with the chart.
Patient identifiers must be on all forms.
If a patient leaves AMA, the patient will still require discharge
instructions and scripts. The patient needs to sign an AMA form
and the MD needs to have a discussion with the
p
atient of the
p
risks of leavin
g
AMA and document this discussion in the medical
record. Please see the Elopement policy for further direction.
54

Death Information
Management
Management
When a patient dies, nursing staff is to notify the Nurse Manager
or Nursing Care Coordinator on duty. If the Attending Physician is
not present, he/she is to be notified by a physician in attendance
or his/her designee
or his/her designee
.
Next of Kin Notification: If the family is not present, the
attending physician or his/her designee will notify them by
telephone immediately. If contact is not made within a
reasonable period of time, the Social Work or Discharge
Planning staff or the Nursing Care Coordinator can assist in
Planning staff or the Nursing Care Coordinator can assist in
contacting the appropriate law enforcement agency to
establish contact. If next of kin is not known, immediate
referral is to be made to the Clinical Patient Care
Liaison(898-5769) during business hours and the Nursing
Care Coordinator after business hours for due diligence
efforts to find a next of kin.
Medical Examiner’s Referral: The physician who
pronounces the patient determines whether the death meets
the criteria for a medical examiner’s referral by completing
the “Record of Death” form (found on e-forms). If it does,
immediately contact the Medical Examiner’s Office (961-
7591).
55

Autopsy Request
Autopsy Request: If the case is not accepted as an
ME case, the physician should ask the family if they
would like an autopsy performed which is at no cost to
would
like
an
autopsy
performed
which
is
at
no
cost
to
the family. The physician or his/her designee must
obtain written consent from the deceased patient’s
family to perform an autopsy (ADM.LGL.003), in
accordance with all applicable state and local laws. If
they inquire, family members should be told that they
will incur no additional cost for the autopsy. Bodies
f i i ddtddtid
o
f
persons carry
i
ng a s
i
gne
d
,
d
a
t
e
d
an
d
no
t
ar
i
ze
d
card indicating opposition to dissection or autopsy
cannot be subject to autopsy or dissection, except as
required by law.
The legal right to grant autopsies in NYS is vested in the
following order:
Surviving Spouse
ALL hild f
ALL
c
hild
ren o
f
age
Father and Mother. Both parents, if living and of sound
mind, must sign for an unmarried child. If child is
unmarried and neither parent is living, all brothers and
sisters of age must sign the consent.
All brothers and sisters of age
All grandchildren of age
It is the sole responsibility of the attending
It
is
the
sole
responsibility
of
the
attending
physician to ensure that the consent form is
correctly completed and attached to the Record of
Death form (ADM.LGL.018)
Death Certificates – Death certificates must be
c
ompleted by an attending physician within 48 hours of death. These are
electronically completed through the NYS Health Commerce System.
Please see policy “Death Information Management:
Autopsy Procedures, Death Paperwork, and
Release of Human Remains” #ADM-017, for full
policy and procedure.
56

Death/Autopsy
Algorithm
61
57

Medication
Reconciliation
is completed by creating the most complete and accurate list
possible of all home medications for each patient and then
comparing that list against the physician’s admission,
transfer, and discharge orders
is intended to bring discrepancies to the attention of the
p
h
y
sician so that chan
g
es ma
y
be made to the orders when
py g y
appropriate
Medication Reconciliation is a National Patient Safety Goal
This system leads toward future community efforts to
improve home medication list management electronically.
Medication errors are one of the leading causes of injury
to hospital patients, and chart reviews reveal that over half
of all hospital medication errors occur at the interfaces of
care.
Poor communication of medical information at transition
points is responsible for as many as 50% of all medication
errors in the hospital and up to 20% of adverse drug events.
Medication Reconciliation should be completed by the
admitting physician/resident. Home medications are
admitting
physician/resident.
Home
medications
are
documented medication reconciliation and must be updated
at the time of admission and discharge. It must be viewed
as an integral part of the H & P and discharge summary.
It is unacceptable especially upon discharge, to simply say
“continue on home meds” as part of your instruction. It is
essential that you reconcile all medications the patient is to
take when dischar
g
ed includin
g
continuation of medications
gg
they were on prior to admission. This will clarify for the
patient exactly what they are to take once they are
discharged.
58

Addressograph/patient label
PROCEDURAL PROGRESS NOTE
& INFORMED CONSENT FORM
PATIENT SAFETY –
The Universal Time Out
UNIVERSAL TIME OUTS are a critical contribution to patient safety and must be performed and
documented on the Procedural Progress Note EVERY TIME
. The purpose is to ensure that the
correct procedure is being done on the correct patient on the correct side. All those involved in the
procedure should participate.
59

Telephone/ Verbal Orders
- Read back required
Requirement: For verbal or telephone orders or for telephonic
reporting of critical test results, verify the complete order or test
result by having the person receiving the order or test result
result by having the person receiving the order or test result
"read-back" the complete order or test result.
If you are within the building and able to input your order into
the patient record, please do so rather than providing a
telephone order to the nurse. You may also utilize Affiliate (off
site EMR access) to input your order(s) into the patient record
rather than
g
ive a tele
p
hone order. Please ensure when usin
g
gp g
Affiliate you are on duty and not violating duty hour rules.
You must e-SIGN, DATE, TIME
your phone/verbal orders
within 48 hours.
60

ALC (Alternative
Level of Care) Status
Please note that ALC status is a billing designation
only and does not change the care a patient receives.
All patients on ALC status must be seen at least daily
and a daily note consistent with their condition
must be documented in the medical record.
IMPORTANT FOR RESIDENT AND ATTENDING: Should
a patient suffer an adverse outcome and there was
evidence that the patient had not been seen daily, the New
York State De
p
artment of Health confirmed the
y
would
py
consider this grounds for referral to the OPMC (Office of
Professional Medical Conduct).
61

Case Management/Discharge
Planning and Social Work
Assistance
RN Case Manager/ RN Assistant Case Manager are
geographically based on every zone. They lead the care
coordination efforts and assist the multidisciplinary team with
the throughput of the patient. They also serve as a resource
id f th id t d tt di hi h t ib t t
g
u
id
e
f
or
th
e
res
id
en
t
s
an
d
a
tt
en
di
n
g
w
hi
c
h
con
t
r
ib
u
t
es
t
o
strengthened physician-interdisciplinary
communication. This team member also completes the
utilization reviews of all patients on their zone.
Discharge Planners are geographically based on every
zone. They facilitate patients who are being discharge home
to the community
They arrange any necessary services
to the community
.
They arrange any necessary services
required after discharge including but not limited to home
care services, durable medical equipment, prescription
assistance and follow-up appointments discharge.
Social Worker – Hospital social workers are responsible for
the more complex cases within the hospital. They cover two
zones. Social workers assess the
p
s
y
chosocial functionin
g
,
py g
environmental and support needs of patients and families
and provide support as needed. Different interventions may
include connecting patients and families to necessary
resources and supports in the community; providing
psychotherapy, supportive counseling, or grief counseling; or
helping a patient to expand and strengthen their network of
social supports
social supports
.
62

Ordering Home Care
Services
Wound Care Orders must be written to include site, cleansing of
wound, treatment, and frequency. Also prescriptions for supplies must
be written. Any BID patients that that will not be discharged by 3:00
p.m. must have their treatment done prior to leaving and will start in
the morning to ensure staff safety.
Foley Care – there must be a specific order for changing and/or
irrigation including size of catheter and balloon, and frequency of foley
change.
Q12H Injectable Meds including Lovenox – order for BID if possible.
Diets must be specific – simply stating “renal, diabetic, and cardiac”
does not meet homecare regulations. Specify amount of calories,
protein, sodium and whether low fat.
Diabetics – order frequency of FSBS with glucometer and high and low
parameters for when MD should be called. Scripts for glucometer,
strips, lancets, and alcohol wipes need to be written. If 4:00 p.m. FS is
needed, if patient is not discharged by 3:00 p.m., the 4:00 p.m. BS must
be done prior to discharge and the agency will see the patient in the
morning.
Insulin – please issue scripts for insulin and insulin syringes.
Lantus Insulin – as per the manufacturers package insert, “Lantus may
be administered at anytime during the day. It exhibits a relatively
constant glucose-lowering profile over 24 hours that permits once daily
dosing.” Therefore, orders for Lantus insulin should be written for daily
rather than qhs to ensure staff safety.
IVAB/HAL – please be sure patient has PICC line or a Grosberg
catheter (preferred for patients with advanced CKD) in place as
peripheral IV’s are acceptable only in rare instances. Orders for drug
must be written early AM so arrangements for nurse and supplies can be
made. IV cases will not be accepted for start of care the same day as
discharge if orders are not received by 2:00 p.m. Also please note that
community pharmacies will not dispense IV meds if patient does not
community pharmacies will not dispense IV meds if patient does not
have insurance. If patient has Medicare only, patient is responsible for
the drug which must be paid for upfront.
SN, Behavior SN, PT, OT, HHA, MSW, and Dietician services are
available.
Discharge Planning can assist finding services in all counties.
63

VI.
Professionalism
Professionalism
Improving the Patient and
Provider Ex
p
erience
p
64

Erie County Medical Center
Behavioral Expectations
Because we are dedicated to being the medical center of choice
through excellence in patient care and customer service it is our responsibility
Courtesy & Respect
Knock and ask permission before entering a patient’s room. Greet the
p
atient b
y
their surname but also ask the
p
atient how the
y
would like to
through excellence in patient care and customer service
,
it is our responsibility
to treat all our customers, including patients, families, physicians, co-workers
and all outside contacts with courtesy, dignity, respect and professionalism.
py
py
be addressed. Some prefer if you call them by their first name or first
and last rather than Mr. or Mrs.
If it is necessary to interrupt the patient’s sleep, visit with family or
another staff member, apologize for the interruption. Warn them before
you turn on lights.
Make eye contact; introduce yourself and tell them your role in their
care. If possible, sit
while speaking with patients and families.
Explain the presence of the "whole team" when enterin
g
the patient's
g
room on rounds. Make sure the patient and family know the name of
the “Doctor in Charge” of their care.
Politely ask visitors to step in the corridor. After they have stepped out,
ask the patient if he wants anyone in the room while you discuss the
care.
Close the door or pull the curtain prior to discussions or exams. Explain
what you are doing and keep patient properly draped.
If possible, position yourself at eye level. If not, stand at the side
rather than the foot of the bed.
Listen carefully; do not interrupt; give the patient your full attention.
Always include the patient in any teaching or conversation at the
bedside.
Respect cultural differences.
Demonstrate a professional attitude toward co-workers and customers;
use a respectful tone of voice.
Discuss confidential or sensitive information about patients employees
Discuss confidential or sensitive information about patients
,
employees
,
or hospital business only with those having a valid need to know, and
do so privately, never in public places.
65

Definitions of Inappropriate Conduct
• Belittling or berating statements;
• Name calling;
• Use of
p
rofanit
y
or disres
p
ectful lan
g
ua
g
e
;
py p gg;
• Inappropriate comments written in the medical record;
• Blatant failure to respond to patient care needs or staff
requests;
• Personal sarcasm or cynicism;
• Deliberate lack of cooperation without good cause;
• Deliberate refusal to return phone calls, pages, or other
messages concerning patient care or safety;
• Intentionall
y
condescendin
g
lan
g
ua
g
e
;
and
Communicate with Your
Attending, Nursing Teams and
Care Mana
g
ement Staff
yggg;
• Intentionally degrading or demeaning comments
For patients admitted between midnight and 6:00 a.m., notify
attending physician if patient is critical or unstable.
Any change in patient condition or patient deterioration should
be discussed with your attending physician 24/7.
When a patient requires to be placed in restraints communicate
g
When a patient requires to be placed in restraints
,
communicate
with nursing staff!
Whenever possible, check daily with patient’s nurse concerning
patient’s condition.
Discuss test results, changes in condition, plan of care with nursing
staff – they need to know what’s going on with their patient!
ECMC is trying to cohort (grouping patient’s of similar status/team
assignment together
)
y
our patients to one or two zones/units to
facilitate multi-disciplinary care planning.
66

Responsiveness,
Communication and Teamwork
Tell patients when you expect to visit them and when you are
available to speak to their family.
If you are unable to visit them as planned, send someone in your
place when possible or call the unit.
When your unavailability is planned, tell the patient who will be
covering you and for how long
covering you and for how long
.
If you order X-Rays or procedures, explain them to the patient.
Provide test results as soon as available. Explain any delays.
If delay is expected, let them know that.
Inform family of change in condition, transfer to ICU, time of
surgery, untoward events, expected discharge date.
Invite questions and comments from patients and their families.
Ensure the patient understands their care prior to leaving the
room
room
.
Communicate with clarity and professionalism both orally and in
writing.
Keep patients informed while resolving issues or getting answers
to questions.
Participate openly, honestly share opinions; take responsibility
for improving processes and systems.
Maintain positive working relationships with co-workers and
customers; perform duties in a way that makes it easier for
customers; perform duties in a way that makes it easier for
others to perform theirs.
NEVER disagree with other care providers in front of the patient
or family.
Wear your name badge so that name is clearly visible at all
times.
Limit eating and drinking to designated areas.
Do not make inappropriate or negative comments about patients
or co-workers in the
p
resence or within the hearin
g
of an
y
pgy
customer.
67

VII.
Ethics, Risk Management,
Com
p
liance
,
and
p,
Transitions of Care
Healthcare decision-making,
Reporting of Incidents
68

Risk Risk
ManagementManagement
ManagementManagement
Unsure about patient’s capacity, ability to
give consent, end of life issues, etc?
If in doubt, please ASK FOR HELP. We are
h
e
r
e
to
suppo
r
t
you
.
Your contact at ECMCC
Amy Flaherty, Esq.
e e to suppo t you
Vice-President of Patient Advocacy
X5769, x3162 or x5305
Ethics Consults
(any issues with advance directives or
limitation of treatment
See Family
limitation of treatment
–
See Family
Health Care Decision Act section for
more information on the New York State
law.)
Clinical Nurse Liaison
Pager - 642-7177
69

Report All Incidents!
If something ad erse occ rs
e ant to kno abo t it
If something ad
v
erse occ
u
rs
,
w
e
w
ant to kno
w
abo
u
t it
.
Improvement begins with you – report all occurrences through
the Quantros System (electronic reporting system) – Icon located
on all desktops in the hospital.
When reporting, please see Quantros Direct Reporting tips
hi h b f d th ECMC i t t hi h id
w
hi
c
h
can
b
e
f
oun
d
on
th
e
ECMC i
n
t
rane
t
w
hi
c
h
can
gu
id
e
you based on the occurrence. Please include :
patient name
medical record number
date/time of event
unit/area it occurred
Details of event
If you are comfortable, include your name and contact
information so we can get back to you.
Examples of Reportable Occurrences:
Missed orders
Disruptive behavior
Falls
All patient safety events (something that did or could injure
your patient)
Any process improvement opportunities
Adverse drug reactions
Delays in patient care
All medical errors
All medical errors
Lost Airway
70

HIPAAHIPAA
Confidentiality is
essential.
No cameras or cell phones may be used to photograph patients,
procedures or any diagnostic images
without consent
procedures or any diagnostic images
without consent
.
Only secure texting applications (Imprivata ®, Corext) may be used to
transmit PHI and photographs for diagnostic and care process ONLY.
If you will be utilizing patient information or images for educational
purposes, consent MUST be obtained. If it is for research purposes, it
must be a UB IRB/ECMC approved research project.
Accessing medical records is for care purposes only. Access of
medical records of a friend, your own or a patient who is not under
your care may be considered a HIPAA violation. If a patient or HCP
asks you to review their record, you must (a) have privileges at the
institution; (b) have written consent; and (c) have acknowledgement
from the doctor in charge of the patient’s care that you will be
reviewing the record. All your EMR views are tracked and can be
searched by our Privacy Officer.
Never discuss patients or case details in common areas such as
elevators, cafeteria, lobby, etc. to avoid an unnecessary and
unprofessional breach.
71

HIV Testing LawHIV Testing Law
As of September 1, 2010, New York State requires
that an HIV test be offered to every individual
between the ages of 13 and 64 at least once.
Offer should be made by providers offering primary
care services. Primary care services are defined as:
Family Medicine
General Pediatrics
Primary Care
Internal Medicine
Primary Care Obstetrics/Gynecology
Additional offers should be made for persons whose
risk behaviors indicate need for more frequent
testing
testing
.
Required Offer - Exceptions
When the individual is being treated for a life threatening
emergency
Individual has previously been offered test or actually
tested for HIV
(
unless otherwise indicated due to risk
(
factor)
Individual lacks capacity to consent and there is no other
person available to provide consent.
72

The requirement for the offering Hepatitis C testing applies to:
•
Persons receiving inpatient services at hospitals;
Hep C Testing Requirements
Policy # IC-062
Persons receiving inpatient services at hospitals;
• Persons receiving primary care services through hospital outpatient
clinics and diagnostic and treatment centers; and
• Persons receiving primary care services from physicians, physician
assistants, and nurse practitioners regardless of setting
The law does not
require an offer of testing to be made:
• When the individual is being treated for a life-threatening emergency.
• When the individual has previously been offered or has been the subject
of a hepatitis C related test (unless otherwise indicated due to on-going
risk factors).
• When the individual lacks the capacity to consent* (though in these
cases, the offer may also be made to an appropriate person who is
available to provide consent on behalf of the patient)
*The exception as stated in the law refers to the individual lacking the
it t t th ff (Th f t " it t t" d
capac
it
y
t
o
accep
t th
e
o
ff
er.
(Th
e
re
f
erence
t
o
"
capac
it
y
t
o
consen
t" d
oes
not imply written, informed consent for the hepatitis C test, but rather
capacity to understand the test offer)
• Emergency Departments are not required by the law to offer hepatitis C
screening testing, but are encouraged to do so.
A Hepatitis C screening test will be offered to every individual born
between 1945 and 1965
(Although the new law requires testing only for
between 1945 and 1965
(Although the new law requires testing only for
those born between 1945 and 1965, CDC recommends hepatitis C testing
be offered to all persons at risk for hepatitis C.)
• Patients will be asked directly in writing or orally if they would like a
hepatitis C test.
• A Physicians/Providers order to perform the test itself must then be
obtained
• The Nurse will document on the EMR that the
p
atient was offered this
p
testing and if the patient refused.
• There is no separate (special) consent required for hepatitis C testing.
• The general medical consent for medical services, this would cover HCV
testing. (please see policy for “Reactive Test Result” guidance.)
73

Family Healthcare
Decisions Act
On June 1, 2010 New York’s Family Health Care Decisions Act
(FHCDA) went into effect. This new law establishes the authority of
a patient’s family member or close friend to make health care
decisions for the patients in cases where the patient lacks decisional
capacity and did not leave prior instructors OR appoint a health care
agent. Prior to this New York had been one of the few states that
prohibited family members from making health care decisions for
incapacitated loved ones unless
the patient had signed a health care
proxy or left “clear and convincing evidence” of his or her treatment
wishes.
The FHCDA does NOT
apply to decisions for incapable patients
who:
‐ have completed a Health Care Proxy form
‐ have a court appointed Legal Guardian under SCPA
1750-b, for whom decisions
about life
‐
sustaining
treatment may be made
‐ whom treatment decisions may be made pursuant to
OMH or OMRDD surrogate decision-making
regulations
The statute sets forth
IN ORDER OF PRIORITY
the persons who
The statute sets forth
,
IN ORDER OF PRIORITY
,
the persons who
may act as a surrogate decision maker for the incapable patient:
1. MHL Article 81 court-appointed legal guardian.
2. Spouse / Domestic partner
3. Adult Children
4. Parent(s)
5. Siblings
6. Close friend or other
The surrogate has the authority to make all health care decisions for
the patient that the adult patient could make for himself or herself,
subject to certain
standards and limitations
This
“
surrogate
”
subject to certain
standards and limitations
.
This surrogate
decision maker is also empowered to direct withdrawal or
withholding of life-sustaining treatment when standards set forth in
the statute are satisfied. The FHCDA requires the surrogate to base
his or her decisions on the patient’s wishes, including the patient’s
religious or moral beliefs. If the patient’s wishes are not reasonably
know and cannot with reasonable diligence be ascertained, the
surrogate must base decisions on the patient’s best
interests.
One of the most significant features of the FHCDA is that it
establishes a procedure to secure a decision to provide needed
treatment for incapable patients who have NO family members or
treatment for incapable patients who have NO family members or
close friends that could act as the surrogate. With respect to
ROUTINE medical treatment, the statute simply authorizes the
attending physician to decide about such treatment for patients
without surrogates. For decisions about MAJOR medical treatment,
the attending physician must consult with other health care
professionals directly involved with the patient’s care, and a second
physician must concur in the decision.
74

Family Healthcare
Decisions Act,
continued from previous page
In contrast, decisions to withdraw
or withhold life-sustaining
treatment from isolated incapable patients is limited. Such decisions
can be made only (1) by a court, in accordance with the FHCDA
surrogate decision making standards; OR (2) if the attending
physician and a second physician determines that the treatment
offers the patient no medical benefit because the patient will die
imminently even if the treatment is provided and the provision of
imminently
,
even if the treatment is provided
,
and the provision of
treatment would violate accepted medical standards.
It is important to note that the FHCDA does not eliminate the need
for open and honest
conversations with loved ones about wishes
and desires for medical care. And it does not eliminate the need for
individuals to have advanced directives on file with doctors,
attorne
y
s and famil
y
member
yy
MOLST
MOLST is generally for patients with serious health conditions.
Consider the MOLST form for those who want to avoid or receive any or all
life-sustaining treatment, those who reside in a long-term care facility or who
require long-term care services. It is also appropriate for those patients
whose health status indicates that they may die within a year. The MOLST
form is signed by a
New York State licensed physician
and is unique in that
form is signed by a
New York State licensed physician
and is unique in that
it follows the patient as they are transferred through various facilities or
levels of care. It is bright pink so it is easy to spot in a patient’s medical
file. As a reminder, we ask you to think “MOLST MONDAY” and check
these orders at a minimum of each Monday.
For more information:
S
id t
S
ource:
www.compass
i
onan
d
suppor
t
.or
g
Patricia Bomba, MD, FACP, Chair, MOLST Statewide Implementation Team
75

Capacity/Consent
Decision-Making Flow Chart
76

Ethical Issues –
Limitation of Treatment
Ethics Committee Activation or Ethical Concerns
If you need assistance with end of life care or decision-making
issues, please do not navigate this alone. ECMCC provides
Ethics Consults 24/7 – you may activate by using the On-Call
schedule through the operator or on the intranet.
If you are not sure about completing a MOLST form with a patient
d/ f il t t th
li i l Li i
d h
an
d/
or
f
am
ily
,
y
ou
ma
y
con
t
ac
t th
e
c
li
n
i
ca
l
nurse
Li
a
i
son
an
d
s
h
e
will assist you at x5769 – Pager: 642-7177 or Risk Mana
g
ement.
The MOLST form must be signed by a New York State Licensed
Physician. And remember, be sure THE ATTENDING
PHYSICIAN is aware of all decisions made regarding the patient
at all times.
Limitation of Treatment
If
y
ou have concerns or questions about the limitation of treatment
for a patient, first discuss with the ATTENDING PHYSICIAN and if
additional review is needed, you may contact the Risk
Management department if there are legal and/or ethical
concerns.
Moral Objection
ECMCC has an approved Moral Objection Policy (ADM-044)
which can be located on the ECMCC intranet under Policies and
Procedures. Please review the process if you are in a situation
that conflicts strongly with your personal beliefs to ensure that
patient care will not be delayed or adversely affected in anyway.
77

Your Contact for Corporate Compliance Issues
Nadine Mund
Director of Corporate Compliance
898-4595
ECMCC Corporate Compliance Program
Located on ECMCC Intranet
http://home.ecmc.edu/depts/corpcom/docum
ents/CorporateComplianceProgram.pdf
Compliance Hotline
898-5555
Avoid Conflict of Interest Issues
-
Meals or other types of food directly provided or
funded by Industry are prohibited at all ECMCC
sponsored educational activities regardless of
whether such event is held onsite or offsite Support
whether such event is held onsite or offsite
.
Support
is permitted but must be achieved by financial
donations to an ECMCC component (ECMCC
Med/Dent Staff Office).
- Grants or gifts to fund meals may be received by
ECMCC components but not by individual
departments or divisions. Funds will be pooled to
ensure that an
y
g
rant or
g
ifts will be disassociated
yg g
from the receiving center and can avoid conflict of
interest or the perception thereof.
- Any other gifts offered by pharmaceutical reps or
other vendors is strongly discouraged.
- Please be sure to review the University at Buffalo
Conflict of Interest policy as well. The ECMCC policy
entitled Exchan
g
es between ECMCC and Industr
y
can
gy
be found on the ECMCC intranet policy page.
- When in doubt, feel free to contact Nadine Mund,
Corporate Compliance Officer at 898-4595 for input.
Corporate Compliance
78

VIII.
Programs and
Regulations
DSRIP, Patient-Centered
Medical Home
,
I-Sto
p
,
p
79

What is DSRIP?
How will it effect how I care for my patients?
Deliver
y
S
y
stem Reform Incentive Pa
y
ment
yy y
(DSRIP) Program
DSRIP is an agreement (1115 waiver) dating back to April 2014
between the Center for Medicare & Medicaid (MA) Services (CMS) permitting New
York State to reinvest $6.42B from previous federal savings generated by Medicaid
Redesign Team (MRT) reforms. The overall intent of the 5 year DSRIP effort is to
achieve the triple aim – better healthcare for individuals, better health for populations
and the lowest possible cost. Specificall
y
, DSRIP’s
g
oals are to:
•Reduce avoidable hospital admissions and emergency department use by 25 % over
5 years
•Preserve and transform NYS’ fragile healthcare safety net system
•Improve public health measures consistent with NYS’ prevention agenda
•Initially pay for reporting and process, ultimately pay for performance
•Ensure reforms continue beyond 5 year waiver period by leveraging managed care
pa
y
ment reform into value-based contractin
g
•DSRIP themes will not be unique to MA, and will become a way of life for future
doctors for all patients:
•Putting ‘system’ back into healthcare system through collaboration, collaboration,
collaboration
•Integrate medical care, behavioral health, substance abuse and other care (e.g.,
dental)
•Leveraging electronic health information
•Mana
g
in
g
populations and not
j
ust individual patients
•Inclusion of the social determinants of health
•Pay for outcomes (value-based), not fee for service – quality over quantity
(Cont’d, next pg)
DSRIP – Delivery System Reform Incentive Program
80

What is DSRIP?
Continued….
NYS designated 25 performing provider systems (PPS)
statewide. PPS are ACO-like DSRIP basic building block partnerships including
safety net (and even non-safety net) hospitals, primary care (including clinics &
federally qualified health centers or FQHCs), specialty care, post-acute care, long
term care, home care, hospice, palliative care, health homes, social service agencies,
etc. All NYS MA patients are assigned to a PPS. Each PPS selected 7 to 11
projects from a long menu. Total dollars each PPS can earn depend on a complex
formula including the impact of the projects selected, the number of MA patients
assigned and performance on the projects.
There are 2 PPS in the 8 counties of WNY. Millennium Collaborative Care (MCC) is
ECMC’s PPS in partnership with Kaleida Health, other hospitals, UB and many other
providers. MCC was awarded up to $243M to plan, administrate and pay for
programs, incentive partners and reimburse partners for loss of revenue. Based upon
a community needs assessment, MCC selected 11 projects to serve 273,000 MA
patients. They include:
• Integrating the delivery system (PCMH level 3, MU 2)
• ED Triage
• Inpatient Transfer Avoidance Program (INTERACT) for SNF
• Hospital-Home Care Collaboration
• Integration of Primary Care and Behavioral Health/Substance Abuse
• Behavioral Health Community Crisis Stabilization Services
• Cardiovascular Health
• Promote Mental, Emotional and Behavioral (MEB) Well-Being in Communities
• Increase Support Programs for Maternal & Child Health
• Reduce Premature Births
• Patient Activation Measures (PAM) – the 11
th
project including all uninsured
81

What is Patient Centered
Medical Home?
How will it effect how I care for my patients?
Defining the PCMH
Defining the PCMH
“Patient-centered medical homes (PCMH) are transforming primary
care practices into what patients want: a focus on patients themselves
and their health care needs. Medical homes are the foundation for a
health care system that gives more value by achieving the “Triple Aim”
of better quality, experience and cost. This is the overview to our vision
for achieving that goal; it chronicles the PCMH evolution to date, the
h ll th t li h d d t ti l l ti t th h ll
c
h
a
ll
en
g
es
th
a
t li
e
a
h
ea
d
an
d
po
t
en
ti
a
l
so
l
u
ti
ons
t
o
th
ose
c
h
a
ll
en
g
es—
some already underway, some yet to be developed.”
“Everyone in the practice—from clinicians to front desk staff—works as
a team to coordinate care from other providers and community
resources. This maximizes efficiency by ensuring that highly trained
clinicians are not
p
erformin
g
tasks that can be accom
p
lished b
y
other
pg py
staff, and helps avoid costly and preventable complications and
emergencies through a focus on prevention and managing chronic
conditions.”
The Standards are:
•
Patient Access
•
Patient Access
• Team Based Care
• Population Health Management
• Care Management and Support
• Care Coordination and Care Transitions
• Performance Measurement and Quality Improvement
St ff d R id t ill b i i dditi l t i i i h f th
St
a
ff
an
d R
es
id
en
t
s
w
ill b
e
rece
i
v
i
n
g
a
dditi
ona
l t
ra
i
n
i
n
g i
n
eac
h
o
f th
e
elements. All ECMC primary health programs are enrolled in the
PCMH program in an effort to improve primary care and access for
patients.
Patient Centered Medical Home (PCMH)
82

NEW YORK STATE I-STOP
LEGISLATION
Effective August 27, 2013: Prescription Monitoring Program Registry (PMP)
•All practitioners who prescribe a Schedule II, III or IV controlled substance are required to
view
their
patient
’
s
controlled
substance
history
contained
in
the
Department
of
Health
’
s
view
their
patient s
controlled
substance
history
contained
in
the
Department
of
Health s
Prescription Monitoring Program Registry (PMP). The data contained within the registry is
received from more than 6,000 separate reporting dispensers, including registered pharmacies
throughout New York State.
•The legislation requires prescribers to check the PMP before prescribing a controlled
substance. This can be prior to, but not more than 24 hours of a scheduled office visit. With
increased use of the real-time PMP, prescribers can identify addiction-related behavior,
including doctor-shopping. It will also allow prescribers to spot a potentially dangerous drug
interaction. The law allows for certain exceptions. (APPENDIX A - below)
1
*
*
2
*The PMP does not need to be accessed for drugs ordered
for administration on site at ECMC or at the Terrace View
Nursing
Home
It
MUST
be
checked
when
writing
Nursing
Home
.
It
MUST
be
checked
when
writing
prescriptions upon discharge from either facility.
Outside of the Emergency Department setting, limiting the
quantity to a five day supply (3) does NOT exempt a
prescriber from consulting the registry UNLESS criteria
(1)
and
(2) of that section are also met.
( - more, next pg.)
83

NEW YORK STATE I-STOP
LEGISLATION, continued
• Currently, any New York State licensed prescriber who holds a
valid DEA registration may access the PMP registry.
• Each LICENSED prescriber MUST have an individual Health
Commerce System Account (HCS) to gain access to the
PMP.
• IF YOU DO NOT HAVE AN HCS ACCOUNT - Instructions on how
to establish an account are available at the following website:
https://hcsteamwork1.health.state.ny.us/pub/top.html
1-866-811-7957
Access to the PMP Registry for
UNLICENSED PROFESSIONALS
• Licensed prescribers may give a licensed professional or an
unlicensed professional permission to access the PMP Application
on their behalf. The desi
g
nee
,
if unlicensed
,
will need to work
g, ,
with the HCS coordinator from their facility or medical practice to
establish their own HCS account.
• The ECMC HCS Coordinator is the Chief Safety Officer,
Charlene Ludlow 898-3435
• It is strongly encouraged that UB residents be granted
PMP designee access through their residency program.
Questions? Call 1
-
866
-
529
-
1890
Questions? Call 1
866
529
1890
Bureau of Narcotic Enforcement
Riverview Center
150 Broadway
Albany, NY
Phone: 866-811-7957
www.health.ny.gov/professionals/narcotic
E-mail: [email protected]
84
