
January 2024
14-1
Antimicrobial Use and Resistance (AUR) Module
Contents
Antimicrobial Use and Resistance (AUR) Module ................................................................................. 1
Introduction .................................................................................................................................................. 1
1. Antimicrobial Use (AU) Option ................................................................................................................. 2
Introduction ......................................................................................................................................... 2
Requirements ....................................................................................................................................... 3
Data Analyses ....................................................................................................................................... 8
References .......................................................................................................................................... 17
Appendix A. Table of Instructions: Antimicrobial Use Option ........................................................... 18
Appendix B. List of Antimicrobials...................................................................................................... 20
Appendix C. Example Calculations of Antimicrobial Days .................................................................. 24
Appendix D: List of SAARs
a
................................................................................................................. 27
Appendix E: Antimicrobial Groupings for SAAR & Rate Table Calculations
a
...................................... 30
2. Antimicrobial Resistance (AR) Option ..................................................................................................... 37
Introduction ....................................................................................................................................... 37
Requirements ..................................................................................................................................... 38
Data Analyses ..................................................................................................................................... 47
References .......................................................................................................................................... 56
Appendix F. List of Eligible Organisms for the NHSN AR Option ........................................................ 57
Appendix G. Technical and Isolate Based Report Variables ............................................................... 65
Appendix H. Denominator Data Variables ......................................................................................... 70
Appendix I. NHSN AR Option Phenotype Definitions ......................................................................... 73
Appendix J. List of SRIRs and pSIRs .................................................................................................... 77
Introduction
This module contains two options: one focused on antimicrobial use and the second on antimicrobial
resistance. To participate in either option, facility personnel responsible for reporting antimicrobial use
(AU) or resistance (AR) data to the National Healthcare Safety Network (NHSN) must coordinate with
their pharmacy and/or laboratory information software providers to configure their system to generate
standard formatted file(s) to be imported into NHSN. The format provided for data submission follows
the Health Level 7 (HL7) Clinical Document Architecture (CDA)
standard.
7
Manual data entry is not
available for the AUR Module.
Purpose
The NHSN AUR Module provides a mechanism for facilities to report and to analyze antimicrobial use
and/or resistance data to inform benchmarking, reduce antimicrobial resistant infections through
antimicrobial stewardship, and interrupt transmission of resistant pathogens at individual facilities or
facility networks.
6

January 2024 Antimicrobial Use and Resistance Module
AUR
14-2
1. Antimicrobial Use (AU) Option
Introduction
Antimicrobial resistance rates continue to increase in hospitals across the United States.
1
One of the five
CDC core actions to combat the spread of antimicrobial resistance is improving the use of
antimicrobials.
2
Studies show that providing timely and reliable feedback of information to clinicians
regarding their prescribing practices, such as through antimicrobial usage reports, can improve
appropriateness of antimicrobial use.
3-5
Objectives: The primary objective of the Antimicrobial Use (AU) Option is to facilitate risk-adjusted inter-
and intra-facility antimicrobial use benchmarking. A secondary objective is to evaluate antimicrobial use
trends over time at the facility and national levels.
Methodology: The p
rimary antimicrobial use metric reported to the AU Option is antimicrobial days per
1,000 days present. An antimicrobial day (also known as day of therapy) is defined by any amount of a
specific antimicrobial agent administered in a calendar day to a particular patient as documented in the
electronic medication administration record (eMAR) and/or bar coding medication administration
(BCMA) system (refer to Numerator Data section starting on page 14-4 for more information); all
antimicrobial days for a specific agent administered across a population are summed in aggregate.
8-11
Days present are defined as the aggregate number of patients housed in a patient care location or
facility anytime throughout a day during a calendar month (refer to Denominator Data section starting
on page 14-6 for more information). For each facility, the numerator (antimicrobial days) is aggregated
by month for each patient care location and overall for inpatient areas facility-wide (specifically, facility-
wide inpatient or FacWideIN). Similarly, the denominator (days present) is calculated for the
corresponding patient care-location-month or facility-wide inpatient-month.
A
secondary antimicrobial use metric, antimicrobial days per 100 admissions, is reported to the AU
Option for facility-wide inpatient (FacWideIN) data. The numerator and denominators are further
defined below and must adhere to the data format specified by the HL7 CDA Implementation Guide
developed by the CDC and HL7.
7
Manual data entry is not available for the NHSN AU Option.
Settings: All inpatient facilities enrolled in NHSN and reporting to the Patient Safety Component can
participate in the AU Option. This includes facilities enrolled as general acute care hospitals, critical
access hospitals, children’s hospitals, long term acute care hospitals, pediatric long term acute care
hospitals, military and veterans’ hospitals, oncology hospitals, orthopedic hospitals, psychiatric
hospitals, rehabilitation hospitals, surgical hospitals, women’s hospitals, women’s and children’s
hospitals, government and non-government hospitals for public health emergencies. Facilities must have
the ability to collect the numerator and denominator data electronically and upload those data into
NHSN using the required CDA specifications. NHSN does not currently support the submission of data
into the AU Option from ambulatory surgery centers, long term care facilities (for example, skilled
nursing facilities, nursing homes) nor outpatient dialysis facilities.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-3
NHSN strongly encourages the submission of data from all NHSN-defined inpatient locations (including
procedural areas like operating rooms), facility-wide inpatient (FacWideIN), and select outpatient acute
care settings (specifically, outpatient emergency department [ED], pediatric ED, and 24-hour
observation area) from which the numerator and denominator data can be accurately electronically
captured. The AU Option does not accept data from other outpatient locations such as outpatient
clinics. The FacWideIN record should contain data from all inpatient locations and inpatient procedural
areas from which the numerator and denominator can be accurately electronically captured. A
comprehensive submission will enable a facility to optimize inter- and/or intra-facility comparisons
among specific wards, combined wards, and facility-wide data.
NHSN delineates a CDC-defined designation (CDC Location) for patient care areas/locations where
patients have similar disease conditions or are receiving care for similar medical or surgical specialties.
Each facility location is “mapped” to one CDC Location within the NHSN facility. The specific CDC
Location code is determined by the type of patients cared for in that area according to the NHSN
location mapping algorithm for acuity level and service type. The patient care areas include adult,
pediatric, and neonatal units as defined by NHSN Codes. See the NHSN Locations chapte
r for more
information regarding location mapping. Note: facilities should not map a whole separate set locations
for AUR reporting (for example, “1 North” and “1 North AUR”). Facilities are encouraged to report data
from all inpatient locations which means facilities may report AUR data for more locations than are used
for HAI reporting (for example, operating rooms, specialty ward locations like labor and delivery, etc.).
Please work with Infection Control/Infection Prevention to determine the correct location mapping for
your facility.
Requirements
Each month:
1. The facility must indicate the specific locations from which they plan to submit antimicrobial use
data in the Patient Safety Monthly Reporting Plan
.
a. When reporting AU Option data from inpatient and outpatient locations, list FacWideIN,
each individual inpatient location, and each individual outpatient location as separate
rows in the plan.
2. The CDA files submitted by the facility contain all data fields outlined in the Table of Instructions
(Appendix A
) for each location.
3. The facility uploads data via CDA files for all locations indicated in the Monthly Reporting Plan.
a. Submit one file for each individual patient care location as well as a separate file for
FacWideIN. As an example, a facility with three patient care locations will upload three
separate files for each individual location and one additional file for FacWideIN for a
total of four files per month.
NHSN recommends the facility uploads data into NHSN for a given calendar month by the end of the
subsequent calendar month.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-4
Numerator Data (Antimicrobial Days):
Antimicrobial Days (also known as Days of Therapy): Defined as the aggregate sum of days for which any
amount of a specific antimicrobial agent was administered to individual patients as documented in the
eMAR and/or BCMA.
8-11
Appendix B provides the full list of antimicrobial agents collected in the NHSN
AU Option. Aggregate antimicrobial days are reported monthly for inpatient locations, FacWideIN, and
three select outpatient acute care settings (specifically, outpatient ED, pediatric ED, and 24-hour
observation area) for select antimicrobial agents and stratified by route of administration (specifically,
intravenous, intramuscular, digestive, and respiratory).
Refer to Table 1 and Table 2
for the definitions of drug-specific antimicrobial days and stratification
based on route of administration. For example, when a health care professional administers a patient 1
gram Vancomycin intravenously twice daily for three days, three “Vancomycin Days (total)” and three
“Vancomycin Days (IV)” are counted when stratified by intravenous route of administration. Please note
antimicrobials that have an extended half-life, such as Dalbavancin, Oritavancin and Rezafungin, are only
counted as an antimicrobial day on the day of administration. Similarly, in the case of renal impairment,
antimicrobials such as Vancomycin are only counted as an antimicrobial day on the day of
administration.
Table 3 summarizes the data elements for numerator calculation. Appendix C provides
additional examples of antimicrobial day calculation.
A value (specifically, a number greater than or equal to “1”, “0”, or “NA”) must be reported for every
antimicrobial agent and route of administration listed in Appendix B
for every location record for each
month. Antimicrobial agents and routes of administration cannot be left blank. Facilities should report
“0” (zero) antimicrobial days when no aggregate use occurred during a given reporting period for a
specific antimicrobial agent/route (for example, Zanamivir via the respiratory route) and that
agent/route can be accurately captured in the eMAR or BCMA system.
Please note, facilities should report “NA” (Not Applicable) only when the administrations for an
agent/route cannot be electronically captured at that facility (specifically, data are not available for a
specific antimicrobial agent/route). Furthermore, facilities should consistently report “NA” across all
locations and FacWideIN. For example, if a facility was unable to electronically capture Amikacin
administered via the respiratory route (in the event of using the IV formulation for inhalation), the
facility would report “NA” for the respiratory route of Amikacin for all individual locations and
FacWideIN. Facilities should only use “NA” for non-formulary agents when those agents, if administered,
cannot be accurately electronically captured. If use of non-formulary agents can be accurately
electronically captured, no use of those agents in each location/month would be reported as “0” (zero).
The NHSN Team expects use of “NA” at a given facility to remain consistent across months (in other
words, we would expect facilities unable to electronically capture data for a given agent/route to
consistently report “NA”). Facilities should not switch back and forth between reporting a use value
greater than or equal to zero and “NA”.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-5
Table 1. Classification and Definition of Routes of Administration for Antimicrobial Days
Classification:
Route of Administration
a
Definition
b
Intravenous (IV)
An intravascular route that begins with a vein.
Intramuscular (IM)
A route that begins within a muscle.
Digestive Tract
A route that begins anywhere in the digestive tract extending from
the mouth through rectum.
c
Respiratory Tract
A route that begins within the respiratory tract, including the
oropharynx and nasopharynx.
a
Other routes of administration are excluded from the AU Option reporting (for example, antibiotic
locks, intraperitoneal, intrapleural, intraventricular, irrigation, topical) and should not be included in the
total antimicrobial days nor the sub-stratification of the routes of administration.
b
Definitions were drawn from SNOMED qualifier value hierarchy. Refer to the CDA Antimicrobial Use
(AU) Toolkit for specific codes corresponding to each route of administration.
c
For example, rectal administration of Vancomycin.
Table 2. Example Stratification of Antimicrobial Days by Route of Administration
Month/
Year-
Location
Antimicrobial
Agent
Drug-specific Antimicrobial Days
Total
a
IV
IM
Digestive
b
Respiratory
Month/
Year
Location
Tobramycin
Tobramycin
Days
(Total)
Tobramycin
Days
(IV)
Tobramycin
Days
(IM)
Tobramycin
Days
(Digestive)
Tobramycin
Days
(Respiratory)
01/2022
Med Ward
1 1 0 0 1
a
Drug-specific antimicrobial days (total) attributes one antimicrobial day for any route of administration.
For example, if Tobramycin was administered to a patient intravenously and via a respiratory route on
the same day, the antimicrobial days would be counted as “one Tobramycin Day (Total)” and the
stratification by route of administration would be “one Tobramycin Day (IV)” and “one Tobramycin Day
(Respiratory)”.
b
Tobramycin is used for an example of route stratification only and is not FDA approved for
administration via the digestive route.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-6
Table 3. Data Elements for Antimicrobial Days
Data Element
Details
Antimicrobial
Agents
Defined as select antimicrobial agents and stratified by route of administration
(specifically, intravenous, intramuscular, digestive, and respiratory). Refer to Appendix
B for a complete list of antimicrobials. The list of select antimicrobials will evolve with
time as new agents become commercially available and old agents are removed from
the market.
Topical antimicrobial agents are not included in the NHSN AU Option.
Data source
Antimicrobial days are derived from antimicrobial administration data documented in
the eMAR and/or BCMA only. Usage derived from other data sources (for example,
pharmacy orders, doses dispensed, doses billed) cannot be submitted.
Location
Antimicrobial days are aggregated for each inpatient location, facility-wide inpatient,
and three select outpatient acute-care settings (specifically, outpatient ED, pediatric
ED, and 24-hour observation area) per the
NHSN location definitions.
Time Unit
Antimicrobial days for a specific antimicrobial agent and stratification by route of
administration are aggregated monthly per location.
Denominator Data (Days Present and Admissions): The numerator will be analyzed against the
denominators of days present (all locations) and admissions (for facility-wide inpatient [FacWideIN]
only). The denominators are further defined below.
Days present: Days present are defined as the time period during which a given patient is at risk for
antimicrobial exposure in a given patient location. The definition of days present differs from the
definition of patient days used in other NHSN modules. Days present is further defined below in context
of calculation for patient care location-specific analyses and facility-wide inpatient analyses. Please note
that a separate calculation for days present is required for each patient care location compared to
facility-wide inpatient.
For patient care location-specific analyses, days present are calculated as the number of
patients who were present, regardless of patient status (for example, inpatient, observation),
for any portion of each day during a calendar month for a patient care location. The patients can
begin attributing to the days present count in an outpatient location such as an Emergency
Department as soon as triage is completed, regardless of when the patient is placed in a bed.
The aggregate measure is calculated by summing days present for that location and month. The
day of admission, discharge, and transfer to and from locations will be included in the days
present count. Below are examples that illustrate appropriate days present calculation:
• A patient admitted to the medical ward on Monday and discharged two days later on
Wednesday contributes three days present in the medical ward because the patient was
present in that specific location at some point during each of the three calendar days
(specifically, Monday, Tuesday, and Wednesday).
• On the day a patient is transferred from a medical critical care unit to a medical ward, the
patient contributes one day present in the medical critical care unit and one day present in

January 2024 Antimicrobial Use and Resistance Module
AUR
14-7
the medical ward because the patient was present in both locations at some point during
that calendar day. Similarly, a patient contributes days present to the operating room or ED
if data are submitted from these locations.
• One patient can only contribute one day present for a specific location per calendar day.
While a patient cannot contribute more than one day present to any one unique location on
the same day that patient can contribute a day present to two different locations on the
same day. For example, a patient transferred from the surgical ward to the operating room
and back to the surgical ward in a calendar day contributes one day present to the surgical
ward and one day present to the operating room.
For facility-wide inpatient (FacWideIN) analyses, days present are calculated as the number of
patients who were present in an inpatient location within the facility for any portion of each day
during a calendar month. The aggregate measure is calculated by summing up all the days
present for facility-wide inpatient for a given month. Thus, a sum of days present from location-
specific analyses would be higher than days present for the facility (FacWideIN) because
transfers between wards can account for multiple location “days present” for a given patient on
a single calendar day. Therefore, it is not permissible to sum the individual days present for
location-specific analyses to achieve the facility-wide inpatient (FacWideIN) days present count.
The calculation must be a separate summation for facility-wide inpatient analyses.
Please note that only inpatient locations in which both the antimicrobial days (numerator) and
the days present (denominator) can be accurately electronically captured should be included in
the FacWideIN counts. Additionally, outpatient locations (ED, pediatric ED, and 24-hr
observation) should not be included in FacWideIN counts.
Admissions: Admissions are defined as the aggregate number of patients admitted to an inpatient
location within the facility (facility-wide inpatient) starting on first day of each calendar month through
the last day of the calendar month. A patient is counted as an admission when they arrive in an NHSN
designated inpatient location regardless of patient status (for example, inpatient, observation). Further,
a patient admitted to an inpatient unit would be counted as an admission even if they were discharged
that same calendar day. If in the ADT system a patient appears to move from an inpatient to an
outpatient ED, pediatric ED or 24hr observation location then back to an inpatient location, it should be
counted as two separate admissions. In the AU Option, admissions are reported only for facility-wide
inpatient (FacWideIN). Please note, the definition of admissions used in the AUR Module is different
than the definition used in the NHSN MDRO/CDI Module.
January 2024 Antimicrobial Use and Resistance Module
AUR
14-8
Table 4. Location-specific and Facility-wide Inpatient Metrics
Patient Care Location-Specific Analyses
Rate of Antimicrobial Days per 1,000 Days Present
ℎ
ℎ
× 1000
Notes:
• One patient can contribute only one day present per calendar day for each specific location.
• Summed total may be higher when compared to facility-wide count (reflecting transfers
between locations).
Facility-wide Inpatient Analyses
Rate of Antimicrobial Days per 1,000 Days Present
ℎ
ℎ
× 1000
Notes:
• One patient can contribute only one day present per calendar day for a facility. Thus, one
denominator is obtained for all inpatient locations in an entire facility.
• The day present measure for facility-wide inpatient should be lower when compared to sum
total from location-specific comparison.
• Only include inpatient units where both the antimicrobial days (numerator) and the days
present (denominator) can be accurately electronically captured.
•
Exclude outpatient locations.
Rate of Antimicrobial Days per 100 Admissions
ℎ
ℎ
× 100
Notes:
• Only calculated for facility-wide inpatient for the AU Option.
• Only include inpatient units where both the antimicrobial days (numerator) and the days
present and admissions (denominators) can be accurately electronically captured.
• Exclude outpatient locations.
Data Analyses
All AU Option data reported to NHSN can be analyzed immediately after submission to NHSN. After
generating analysis datasets within NHSN, users can view reported data using various NHSN analysis
reports to visualize and analyze data in more detail. For example, descriptive analysis reports such as

January 2024 Antimicrobial Use and Resistance Module
AUR
14-9
line lists, bar charts and pie charts are available. In addition, measures of antimicrobial use are available
in rate tables and Standardized Antimicrobial Administration Ratios (SAAR) reports.
Types of AU Option Analysis Reports
Standardized Antimicrobial Administration Ratio (SAAR):
The Standardized Antimicrobial Administration Ratio (SAAR) is a metric developed by CDC to analyze and
report antimicrobial use data in summary form. The SAAR is calculated by dividing observed
antimicrobial use by predicted antimicrobial use.
=
The observed antimicrobial use is the number of days of therapy, or antimicrobial days, reported by a
facility for a specified category of antimicrobial agents in a specified group of patient care locations. The
predicted antimicrobial use is calculated using predictive models developed by CDC and applied to
nationally aggregated 2017 adult and pediatric or 2018 neonatal AU data reported to NHSN from the
same group of patient care location types. Separate predictive models are developed for each specific
antimicrobial agent category.
The SAAR can be generated for 22 antimicrobial agent categories (7 adult, 8 pediatric, and 7 neonatal)
and 17 specific NHSN location types (8 adult, 5 pediatric, and 4 neonatal), for a total of 47 possible
SAARs (see Appendix D
), each of which can serve as a high-value target or high-level indicator for
antimicrobial stewardship programs. The antimicrobial agent categories were determined by CDC with
input from external adult, pediatric, and neonatal infectious disease physicians and pharmacists. The
SAAR agent categories are listed below. The specific antimicrobial agents in each category can be found
in
Appendix E.
• Adult SAAR antimicrobial agent categories
o All antibacterial agents
o Broad spectrum antibacterial agents predominantly used for hospital-onset infections
o Broad spectrum antibacterial agents predominantly used for community-acquired
infections
o Antibacterial agents predominantly used for resistant Gram-positive infections (e.g.,
MRSA)
o Narrow spectrum beta-lactam agents
o Antibacterial agents posing the highest risk for CDI (not mutually exclusive, agents may
overlap with other categories)
o Antifungal agents predominantly used for invasive candidiasis
• Pediatric SAAR antimicrobial agent categories
o All antibacterial agents
o Broad spectrum antibacterial agents predominantly used for hospital-onset infections
o Broad spectrum antibacterial agents predominantly used for community-acquired
infections

January 2024 Antimicrobial Use and Resistance Module
AUR
14-10
o Antibacterial agents predominantly used for resistant Gram-positive infections (e.g.,
MRSA)
o Narrow spectrum beta-lactam agents
o Azithromycin
o Antibacterial agents posing the highest risk for CDI (not mutually exclusive, agents may
overlap with other categories)
o Antifungal agents predominantly used for invasive candidiasis
• Neonatal SAAR antimicrobial agent categories
o All neonatal antibacterial agents
o Vancomycin predominantly used for treatment of late-onset sepsis
o Broad spectrum antibacterial agents predominantly used for hospital-onset infections
o Third generation Cephalosporins
o Ampicillin predominantly used for treatment of early-onset sepsis
o Aminoglycosides predominantly used for treatment of early-onset and late-onset sepsis
o Fluconazole predominantly used for candidiasis
At present, SAARs are available to facilities that have submitted AU data from one of the 17 eligible
adult, pediatric, and neonatal SAAR location types included in Table 5
. As an important note, the SAARs
generated in NHSN only include the SAAR eligible location types listed in Table 5. None of the SAARs
contain AU data from all inpatient locations in a given facility. Therefore, none of the SAARs would be
considered a “facility-wide” SAAR. In the future, as more facilities submit AU data, the NHSN Team plans
to develop SAARs for additional location types.
Table 5. Location types able to generate SAARs
CDC Location Type
CDC Location Code
NSHN Healthcare
Service Location
(HL7) Code
Adult Locations
Medical Critical Care
IN:ACUTE:CC:M
1027-2
Surgical Critical Care
IN:ACUTE:CC:S
1030-6
Medical-Surgical Critical Care
IN:ACUTE:CC:MS
1029-8
Medical Ward
IN:ACUTE:WARD:M
1060-3
Surgical Ward
IN:ACUTE:WARD:S
1072-8
Medical-Surgical Ward
IN:ACUTE:WARD:MS
1061-1
ONC General Hematology-Oncology Ward
IN:ACUTE:WARD:ONC_HONC
1232-8
Adult Step Down Unit
IN:ACUTE:STEP
1099-1
Pediatric Locations
Pediatric Medical Critical Care
IN:ACUTE:CC:M:PED
1044-7
Pediatric Medical-Surgical Critical Care
IN:ACUTE:CC:MS_PED
1045-4
Pediatric Medical Ward
IN:ACUTE:WARD:M_PED
1076-9
Pediatric Surgical Ward
IN:ACUTE:WARD:S_PED
1086-8
Pediatric Medical-Surgical Ward
IN:ACUTE:WARD:MS_PED
1081-9

January 2024 Antimicrobial Use and Resistance Module
AUR
14-11
CDC Location Type CDC Location Code
NSHN Healthcare
Service Location
(HL7) Code
Neonatal Locations
Special Care Nursery (Level II)
IN:ACUTE:STEP:NURS
1041-3
Neonatal Critical Care (Level II/III)
IN:ACUTE:CC_STEP:NURS
1039-7
Neonatal Critical Care (Level III)
IN:ACUTE:CC:NURS
1040-5
Neonatal Critical Care (Level IV)
IN:ACUTE:CC:NURS_IV
1269-0
A high SAAR that achieves statistical significance (specifically, a SAAR value statistically significantly
larger than 1.0) may indicate antimicrobial overuse. A SAAR that is not statistically different from 1.0
indicates antimicrobial use is equivalent to the referent population’s antimicrobial use. A low SAAR that
achieves statistical significance may indicate antimicrobial underuse. Please note, a SAAR alone is not a
definitive measure of the appropriateness or judiciousness of antimicrobial use, and any SAAR may
warrant further investigation. For example, a SAAR above 1.0 that does not achieve statistical
significance may be associated with meaningful excess of antimicrobial use and further investigation
may be needed. Also, a SAAR that is statistically different from 1.0 does not mean that further
investigation will be productive. SAARs were created for hospital reporters to compare their use of
antimicrobials in each SAAR category against the national benchmark. The groupings of antimicrobials
for SAAR categories were based on expert opinions with a goal to optimize the usefulness for
antimicrobial stewardship. Since these conditions are often multifactorial and often lagged in time,
higher SAARs are not meant to indicate a definitive and immediate clinical consequence (for example,
CDI incidence or specific antimicrobial resistant infection).
SAARs can be produced by month, quarter, half-year, year, or cumulative time periods. The SAAR report
can be modified to show SAARs by a specific location or a subset of location types. However, keep in
mind that SAARs can only be generated and/or modified to show data for the 17 select location types
listed above in Table 5
.
Additional details and guidance for the SAARs are available in the resources listed below:
SAAR Guide: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/au-saar-guide-508.pdf
Keys to Success with the SAAR: https://www.cdc.gov/nhsn/ps-analysis-resources/keys-to-success-
saar.html
SAAR Table: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-SAARTables.pdf
SAAR Table – by Location: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-
SAARTables-Location.pdf
SAAR Plot: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-SAARDotPlot-508.pdf
SAAR Bar Chart in Excel: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/au-qrg-saar-
bartable-location-508.pdf

January 2024 Antimicrobial Use and Resistance Module
AUR
14-12
Targeted Assessment for Antimicrobial Stewardship (TAS):
The Targeted Assessment for Antimicrobial Stewardship (TAS) is a framework for quality improvement
developed by the CDC to use NHSN AU Option data for action to optimize AU at facilities. TAS is
available to hospitals participating in the NHSN AU Option. TAS can be used by antimicrobial stewards
and others focused on optimizing AU within groups, such as health departments and health systems, as
well as individual facilities.
The TAS Reports use a metric called the antimicrobial use cumulative attributable difference (AU-CAD).
The AU-CAD represents the difference between the observed days and a selected Standardized
Antimicrobial Administration Ratio (SAAR) target. The TAS Reports allow for ranking facilities within
groups, or location groups and locations within individual facilities, by the AU-CAD, to identify where
stewardship efforts may have the greatest impact. Since the SAAR is not a definitive measure of the
appropriateness or judiciousness of AU, CDC cannot define SAAR targets for facilities or groups. Facilities
and groups, however, can use their information on antibiotic use (for example, a medication use
evaluation to assess appropriate courses of therapy) to establish improvement goals that can then be
monitored with NHSN AU Option metrics (for example, the AU-CAD and SAAR).
The AU-CAD is the number of antimicrobial days needed to achieve a desired SAAR target. The higher
the AU-CAD value, the greater the number of antimicrobial days that need to be reduced to meet the
SAAR target. For example, if a facility has an AU-CAD of 75 when they run a TAS report with a SAAR
target of 0.95, the interpretation would be “The facility would have needed 75 fewer antimicrobial days
to reach their SAAR target of 0.95 during this time period.”
TAS Reports are located within the Analysis section of NHSN. You’ll notice the TAS Reports have their
own subfolder within the Antimicrobial Use and Resistance Module folder. The TAS reports are
separated by population (adult, pediatric, or neonatal) and by level of aggregation (group, facility,
location group, and location). TAS reports include only those location types that can generate SAARs; in
other words, the same locations in the SAAR reports will also be included in the TAS reports.
Table 6. Location types able to generate SAARs and included in TAS reports
Location Group
in TAS Reports
CDC Location Type CDC Location Code
NSHN
Healthcare
Service
Location (HL7)
Code
Adult
ICU
Medical Critical Care
IN:ACUTE:CC:M
1027-2
ICU
Surgical Critical Care
IN:ACUTE:CC:S
1030-6
ICU
Medical-Surgical Critical Care
IN:ACUTE:CC:MS
1029-8

January 2024 Antimicrobial Use and Resistance Module
AUR
14-13
Location Group
in TAS Reports
CDC Location Type
CDC Location Code
NSHN
Healthcare
Service
Location (HL7)
Code
Stepdown
Adult Step Down Unit
IN:ACUTE:STEP
1099-1
Ward
Medical Ward
IN:ACUTE:WARD:M
1060-3
Ward
Surgical Ward
IN:ACUTE:WARD:S
1072-8
Ward
Medical-Surgical Ward
IN:ACUTE:WARD:MS
1061-1
Oncology
ONC General Hematology-
Oncology Ward
IN:ACUTE:WARD:ONC_HONC
1232-8
Pediatric
ICU
Pediatric Medical Critical Care
IN:ACUTE:CC:M:PED
1044-7
ICU
Pediatric Medical-Surgical Critical
Care
IN:ACUTE:CC:MS_PED
1045-4
Ward
Pediatric Medical Ward
IN:ACUTE:WARD:M_PED
1076-9
Ward
Pediatric Surgical Ward
IN:ACUTE:WARD:S_PED
1086-8
Ward
Pediatric Medical-Surgical Ward
IN:ACUTE:WARD:MS_PED
1081-9
Neonatal
N/A
Step down Neonatal Nursery
IN:ACUTE:STEP:NURS
1041-3
N/A
Neonatal Critical Care (Level II/III)
IN:ACUTE:CC_STEP:NURS
1039-7
N/A
Neonatal Critical Care (Level III)
IN:ACUTE:CC:NURS
1040-5
N/A
Neonatal Critical Care (Level IV)
IN:ACUTE:CC:NURS_IV
1269-0
The TAS reports are available at different levels of aggregation:
• Group
o Available only when running the TAS reports within an NHSN Group.
o One table displays metrics pooled at the group level. All other tables in the Group
reports display metrics at the facility level for each member facility in the group by SAAR
type.
• Facility
o Available only when running the TAS reports within an individual facility.
o The reports display metrics pooled at the facility level for an individual facility.
• Location Group
o The reports display metrics for a group of patient care locations based on how the
locations are mapped in NHSN (see Table 6
).
Adult location groups: ICUs, Wards, Stepdown, Oncology
Pediatric location groups: ICUs, Wards
Location groups are not available for neonatal TAS reports.
o Two types of location group reports are available depending on your preferred sort:

January 2024 Antimicrobial Use and Resistance Module
AUR
14-14
Location groups (Separated): Rank is based on location group SAAR Type AU-
CAD values within the location group. In other words, the SAAR Types are
ranked based on location group AU-CAD value within that specific location
group.
Location groups (Combined): Rank is based on location group SAAR Type AU-
CAD values among all SAAR Types and location groups. In other words, SAAR
Types and location groups are ranked according to the AU-CAD value alone.
• Locations
o AU-CAD values are provided for each individual location able to generate SAARs (see
Table 6
).
Separately, the TAS Dashboard, found on the NHSN Patient Safety Component Home Page or in the
Dashboard section of the left-hand navigation menu, allows NHSN facilities to visualize locations with
the greatest need for antimicrobial stewardship. The TAS Dashboard displays AU-CADs over time, by
quarter, for the most recent complete four calendar quarters at the group, facility, and location level.
Unlike the TAS Reports, the time period and level of aggregation displayed by the TAS Dashboard cannot
be changed.
Additional detail and guidance for the TAS reports and dashboards are available in the resources listed
below:
TAS Guide: https://www.cdc.gov/nhsn/ps-analysis-resources/tas/tas-guide-508.pdf
TAS Report – Facility-level: https://www.cdc.gov/nhsn/ps-analysis-resources/tas/facility-level-508.pdf
TAS Report – Location group-level: https://www.cdc.gov/nhsn/ps-analysis-resources/tas/location-group-
level-508.pdf
TAS Report – Location-level: https://www.cdc.gov/nhsn/ps-analysis-resources/tas/location-level-508.pdf
TAS Report – Group-level: https://www.cdc.gov/nhsn/ps-analysis-resources/tas/group-level-508.pdf
TAS Dashboard – Facility: https://www.cdc.gov/nhsn/ps-analysis-resources/tas/facility-508.pdf
TAS Dashboard – Group: https://www.cdc.gov/nhsn/ps-analysis-resources/tas/group-508.pdf
Rates:
As a supplement to the SAARs, rate tables showing the pooled mean rates and percentile distributions
of specific antimicrobials for specific adult, pediatric and neonatal locations are available. Adult and
pediatric SAAR location types can generate rates for antimicrobials predominantly used for extensively
antimicrobial resistant bacteria. This rate table shows the antimicrobial days per 1,000 days present for
a grouping of five specific drugs (listed in Appendix E
) along with the pooled mean rate and percentile
distributions for the 25
th
, 50
th
, 75
th
, and 90
th
percentiles based on the 2017 baseline adult and pediatric
AU data. Rates can also be generated for well baby and special care (Level II) neonatal nurseries for
select antimicrobial groupings. These rate tables show the antimicrobial days per 1,000 days present for
specific antimicrobial groupings (listed in
Appendix E) along with the pooled mean rate and percentile
distributions for the 25
th
, 50
th
, 75
th
, and 90
th
percentiles based on the 2018 baseline neonatal AU data.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-15
SAAR Baseline Rate Tables: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/au-qrg-ratetable-
drugs-508.pdf
Additionally, users can generate basic rate tables as incidence density rates of antimicrobial days per
1,000 days present stratified by patient care location and facility-wide inpatient. A rate of antimicrobial
days per 100 admissions can also be generated for facility-wide inpatient only. Default rate tables can be
generated by antimicrobial category (specifically, antibacterial, antifungal, anti-influenza, antiviral) and
class (for example, aminoglycosides, carbapenems, cephalosporins) for the most recent month of data
submitted or all months of data submitted for FacWideIN or each individual location. Modifications can
be made to any rate table to show specific months or locations. Specific rate tables can also be modified
to produce a rate per individual antimicrobial, select antimicrobials within the same class, and select
antimicrobials within different classes.
Rate Table – by location:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-
RateTables-Location.pdf
Rate Table – FacWideIN: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-
RateTables-FACWIDEIN.pdf
Descriptive analysis:
Line Lists: Line lists are the most customizable AU Option analysis report. The default line lists show the
total antimicrobial days and the sub-stratification of routes of administration for each antimicrobial as
well as the days present and admissions for each month and location of data submitted. Default line lists
can be generated for the most recent month of data submitted or all months of data submitted, for
FacWideIN or each individual location. Users can modify any line list to show specific months, locations,
antimicrobials, and/or routes of administration. The line lists are the most helpful AU Option report
when validating the data.
Line List: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-LineList.pdf
Bar Charts & Pie Charts: Bar charts and pie charts provide visualizations of the antimicrobial use within a
facility. Default bar charts and pie charts can be generated for the most recent month of data submitted
or all months of data submitted for FacWideIN or each individual location. There is also a bar chart that
shows selected agent distribution by month.
Bar Chart: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-BarChart.pdf
Bar Chart – Selected drugs: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-
BarChart-drugs-508.pdf
Pie Chart: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AU-QRG-PieChart.pdf
All AU Option data analysis reports can be exported from NHSN in various formats including Excel, CSV,
SAS.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-16
NHSN Group Analysis:
NHSN Group users can visualize and analyze AU data shared with them by member facilities using NHSN
analysis reports. In addition to the Analysis Quick Reference Guides (QRGs) referenced in each section
above and available from in the Antimicrobial Use and Resistance Module Reports section of the
Analysis Quick Reference Guide page, Groups can find Group-specific resources on the
NHSN Group
Users page.
Additional Analysis Resources:
Users can find recorded training sessions and Quick Learn videos highlighting AU Option analysis reports
on the AUR Training
page.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-17
References
1. Weiner LM, Webb AK, Limbago B, et al. Antimicrobial-resistant pathogens associated with adult
healthcare-associated infections: summary of data reported to the National Healthcare Safety
Network at the Centers for Disease Control and Prevention, 2015-2017. Infect Control Hosp
Epidemiol 2020;41:1-18.
2. Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States,
2019. Available at:
https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-
report-508.pdf.
3. Davey P, Marwick CA, Scott CL, et al. Interventions to improve antibiotic prescribing practices for
hospital inpatients. Cochrane Database Syst Rev 2017:2;CD003543.
4. Ansari F, Gray K, Nathwani D, et al. Outcomes of an intervention to improve hospital antibiotic
prescribing; interrupted time series with segmented regression analysis. J Antimicrob
Chemother 2003;52:842-8.
5. Solomon DH, Van Houten L, Glynn RJ. Academic detailing to improve use of broad-spectrum
antibiotics at an academic medical center. Arch Inter Med 2001;161:1897-902.
6. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an Antibiotic Stewardship Program:
Guidelines by the Infectious Diseases Society of America and the Society for Healthcare
Epidemiology of America. Clin Infect Dis. 2016 May 15;62(10):e51-77. doi: 10.1093/cid/ciw118.
Epub 2016 Apr 13. PMID: 27080992; PMCID: PMC5006285.
7. National Healthcare Safety Network (NHSN) Patient Safety Component: Clinical Document
Architecture. http://www.cdc.gov/nhsn/cdaportal/index.html
8. Schwartz DN, Evans RS, Camins B, et al. Deriving measures of intensive care unit antimicrobial
use from computerized pharmacy data: methods, validation, and overcoming barriers. Infect
Control Hosp Epidemiol 2011;32:472-80.
9. Polk RE, Fox C, Mahoney A, Letcavage J, MacDougall C. Measurement of adult Antibacterial Drug
Use in 130 US Hospitals: Comparison of Defined Daily Dose and Days of Therapy. Clin Infect Dis
2007;44:664-70.
10. Kuster SP, Ledergerber B, Hintermann A, et al. Quantitative antibiotic use in hospitals:
comparison of measurements, literature review, and recommendations for standards of
reporting. Infection 2008; 6:549-59.
11. Berrington A. Antimicrobial prescribing in hospitals: be careful what you measure. J Antimicrob
Chemother 2010:65:163-168.
12. CLSI. 2020 Performance standards for antimicrobial susceptibility testing, 30
th
edition. CLSI
document M100-ED20. Wayne, PA: Clinical and Laboratory Standards Institute; 2020.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-18
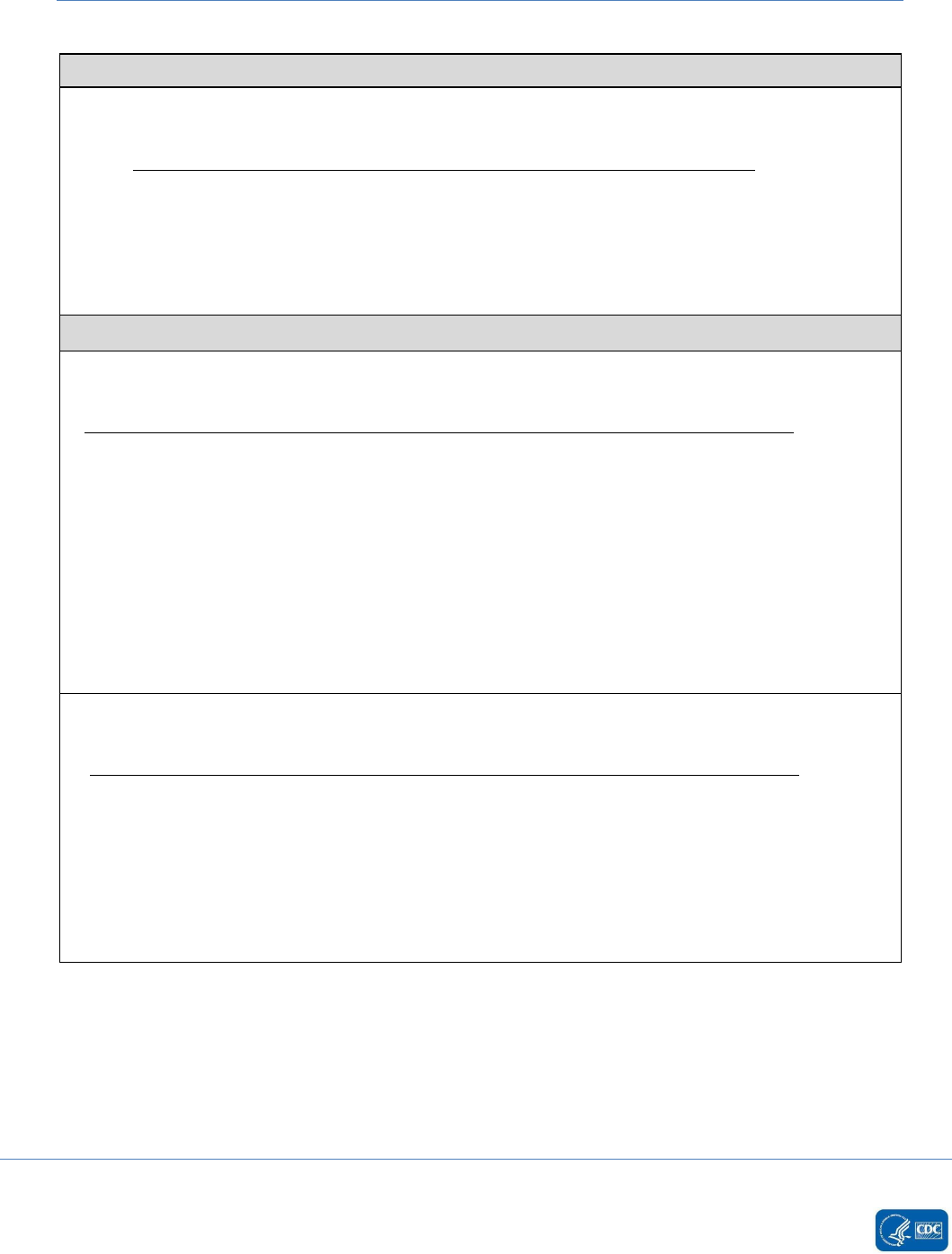
Appendix A. Table of Instructions: Antimicrobial Use Option
Data Field
Data Field Description
Facility OID
a
Required. Must be assigned to facility and included in the CDA data file prior to
submission to NHSN.
Vendor
(Application)
OID
b
Required. Must be assigned to a vendor’s software application and included in the
AU CDA data file prior to submission to NHSN. The Vendor (Application) OID should
be obtained by the software vendor and is distinct from the Facility OID.
SDS Validation ID
Required. The Synthetic Data Set (SDS) Validation ID will be provided to the AU CDA
vendor by the AUR Module Team upon confirmation that the AU Summary SDS
Excel file passed validation as part of the AU SDS initiative.
c
Vendor Software
Name
Optional. Vendor software name is the name of the software application that
generates the AU CDA file. NHSN collects this information to more effectively
troubleshoot CDA files when needed.
Software Version
Optional. Software version is the version of the software application that generates
the AU CDA file. NHSN collects this information to more effectively troubleshoot
CDA files when needed.
Vendor Name
Optional. Vendor name is the name of the vendor that owns the software
application that generates the AU CDA file. NHSN collects this information to more
effectively troubleshoot CDA files when needed.
Month
Required. Record the 2-digit month during which the data were collected for this
location.
Year
Required. Record the 4-digit year during which the data were collected for this
location.
Location
Required. The patient care location for which the data are being uploaded.
Numerator:
Antimicrobial
days per month
per location
Required. Antimicrobial days are defined as the aggregate sum of the days of
therapy for which a specific antimicrobial was administered. These are required to
be extracted from electronic medication administration record (eMAR) and/or bar
coding medication administration (BCMA) system. Antimicrobial days are collected
for select antimicrobial agents (refer to
Appendix B) and stratified by route of
administration.
Denominator(s):
Days present
Required.
Days present are defined as risk for antimicrobial exposure per each day of the
calendar month stratified by location. For patient care location-specific analyses,
days present is calculated as the number of patients who were present for any
portion of each day during a calendar month for a patient care location. The patient
can begin attributing to the days present count in an outpatient location such as an
Emergency Department as soon as triage is completed, regardless of when the
patient is placed in a bed. For facility-wide inpatient analyses, days present are
calculated as the number of patients who were present in an inpatient location
within the facility for any portion of each day during a calendar month.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-19
Data Field
Data Field Description
Admissions
Admissions are defined as the aggregate number of patients admitted to an
inpatient location within the facility (facility-wide inpatient) starting on first day of
each calendar month through the last day of the calendar month. A patient is
counted as an admission when they arrive in an NHSN designated inpatient location
regardless of patient status (for example, inpatient, observation). Further, a patient
admitted to an inpatient unit would be counted as an admission even if they were
discharged that same calendar day. A patient movement from an inpatient to an
outpatient ED, pediatric ED, or 24hr observation location then back to an inpatient
location is counted as two separate admissions. In the AU Option, admissions are
only reported for facility-wide inpatient. Please note, the admissions definition
used in the AUR Module is different than the definition used in the NHSN
MDRO/CDI Module.
a
Facilities interested in submitting data to NHSN via CDA must obtain a Facility OID (object identifier).
More information on how to obtain an OID for your facility can be found on the
CDA Submission Support
Portal.
b
AU CDA files are required to include a Vendor (Application) OID (object identifier) as part of the AU
Option Synthetic Data Set initiative. More information on how to obtain a Vendor (Application) OID can be
found on the Vendor (Application) Object Identifier
page.
c
More detailed information about the AU Synthetic Data Set validation process can be found on the AUR
Synthetic Data Set Validation page.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-20
Appendix B. List of Antimicrobials
Please note that mapping of standardized terminology (RXNORM) is provided in the Information Data
Model (IDM) found in the Antimicrobial Use Toolkit
. The list of NHSN drug codes as well as the drug values
used for the development of the CDA files can be found here: Eligible Antimicrobials.
Antimicrobial Agent
Antimicrobial
Category
Antimicrobial
Class
a
Antimicrobial
Subclass
a
AMANTADINE
Anti-influenza
M2 ion channel
inhibitors
AMIKACIN
Antibacterial
Aminoglycosides
AMIKACIN LIPOSOMAL
b
Antibacterial
Aminoglycosides
AMOXICILLIN
Antibacterial
Penicillins
Aminopenicillin
AMOXICILLIN/
CLAVULANATE
Antibacterial
β-lactam/β-lactamase
inhibitor combination
AMPHOTERICIN B
Antifungal
Polyenes
AMPHOTERICIN B LIPID
COMPLEX
Antifungal
Polyenes
AMPHOTERICIN B
LIPOSOMAL
Antifungal
Polyenes
AMPICILLIN
Antibacterial
Penicillins
Aminopenicillin
AMPICILLIN/
SULBACTAM
Antibacterial
β-lactam/β-lactamase
inhibitor combination
ANIDULAFUNGIN
Antifungal
Echinocandins
AZITHROMYCIN
Antibacterial
Macrolides
AZTREONAM
Antibacterial
Monobactams
BALOXAVIR MARBOXIL
Anti-influenza
Polymerase acidic
endonuclease
inhibitors
CASPOFUNGIN
Antifungal
Echinocandins
CEFACLOR
Antibacterial
Cephalosporins
Cephalosporin 2
nd
generation
CEFADROXIL
Antibacterial
Cephalosporins
Cephalosporin 1
st
generation
CEFAZOLIN
Antibacterial
Cephalosporins
Cephalosporin 1
st
generation
CEFDINIR
Antibacterial
Cephalosporins
Cephalosporin 3
rd
generation
CEFEPIME
Antibacterial
Cephalosporins
Cephalosporin 4
th
generation
CEFIDEROCOL
Antibacterial
Cephalosporins
Siderophore
CEFIXIME
Antibacterial
Cephalosporins
Cephalosporin 3
rd
generation
CEFOTAXIME
Antibacterial
Cephalosporins
Cephalosporin 3
rd
generation
CEFOTETAN
Antibacterial
Cephalosporins
Cephamycin
CEFOXITIN
Antibacterial
Cephalosporins
Cephamycin

January 2024 Antimicrobial Use and Resistance Module
AUR
14-21
Antimicrobial Agent
Antimicrobial
Category
Antimicrobial
Class
a
Antimicrobial
Subclass
a
CEFPODOXIME
Antibacterial
Cephalosporins
Cephalosporin 3
rd
generation
CEFPROZIL
Antibacterial
Cephalosporins
Cephalosporin 2
nd
generation
CEFTAROLINE
Antibacterial
Cephalosporins
Cephalosporins with anti-
MRSA activity
CEFTAZIDIME
Antibacterial
Cephalosporins
Cephalosporin 3
rd
generation
CEFTAZIDIME/AVIBACTAM
Antibacterial
β-lactam/β-lactamase
inhibitor combination
CEFTOLOZANE/
TAZOBACTAM
Antibacterial
β-lactam/β-lactamase
inhibitor combination
CEFTRIAXONE
Antibacterial
Cephalosporins
Cephalosporin 3
rd
generation
CEFUROXIME
Antibacterial
Cephalosporins
Cephalosporin 2
nd
generation
CEPHALEXIN
Antibacterial
Cephalosporins
Cephalosporin 1
st
generation
CHLORAMPHENICOL
Antibacterial
Phenicols
CIPROFLOXACIN
Antibacterial
Fluoroquinolones
CLARITHROMYCIN
Antibacterial
Macrolides
CLINDAMYCIN
Antibacterial
Lincosamides
COLISTIMETHATE
Antibacterial
Polymyxins
COLISTIN
c
Antibacterial
Polymyxins
DALBAVANCIN
Antibacterial
Glycopeptides
Lipoglycopeptides
DAPTOMYCIN
Antibacterial
Lipopeptides
DELAFLOXACIN
Antibacterial
Fluoroquinolones
DICLOXACILLIN
Antibacterial
Penicillins
Penicillinase-stable
penicillins
DOXYCYCLINE
Antibacterial
Tetracyclines
ERAVACYCLINE
Antibacterial
Tetracyclines
Fluorocycline
ERTAPENEM
Antibacterial
Carbapenems
ERYTHROMYCIN
Antibacterial
Macrolides
FIDAXOMICIN
Antibacterial
Macrocyclic
FLUCONAZOLE
Antifungal
Azoles
FOSFOMYCIN
Antibacterial
Fosfomycins
GENTAMICIN
Antibacterial
Aminoglycosides
IMIPENEM/
CILASTATIN
Antibacterial
Carbapenems
IMIPENEM/CILASTATIN/
RELEBACTAM
Antibacterial
β-lactam/β-lactamase
inhibitor combination
ISAVUCONAZONIUM
Antifungal
Azoles

January 2024 Antimicrobial Use and Resistance Module
AUR
14-22
Antimicrobial Agent
Antimicrobial
Category
Antimicrobial
Class
a
Antimicrobial
Subclass
a
ITRACONAZOLE
Antifungal
Azoles
LEFAMULIN
Antibacterial
Pleuromutilins
LEVOFLOXACIN
Antibacterial
Fluoroquinolones
LINEZOLID
Antibacterial
Oxazolidinones
MEROPENEM
Antibacterial
Carbapenems
MEROPENEM/
VABORBACTAM
Antibacterial
β-lactam/β-lactamase
inhibitor combination
METRONIDAZOLE
Antibacterial
Nitroimidazoles
MICAFUNGIN
Antifungal
Echinocandins
MINOCYCLINE
Antibacterial
Tetracyclines
MOLNUPIRAVIR
Antiviral
Nucleoside Analog
MOXIFLOXACIN
Antibacterial
Fluoroquinolones
NAFCILLIN
Antibacterial
Penicillins
Penicillinase-stable
penicillins
NIRMATRELVIR
d
Antiviral
Protease Inhibitor
NIRSEVIMAB
e
Monoclonal
Antibody
Fusion inhibitor
NITROFURANTOIN
Antibacterial
Nitrofurans
OMADACYCLINE
Antibacterial
Tetracyclines
Aminomethylcycline
ORITAVANCIN
Antibacterial
Glycopeptides
Lipoglycopeptides
OSELTAMIVIR
Anti-influenza
Neuraminidase
inhibitors
OXACILLIN
Antibacterial
Penicillins
Penicillinase-stable
penicillins
PENICILLIN G
Antibacterial
Penicillins
Penicillin
PENICILLIN V
Antibacterial
Penicillins
Penicillin
PERAMIVIR
Anti-influenza
Neuraminidase
inhibitors
PIPERACILLIN/
TAZOBACTAM
Antibacterial
β-lactam/β-lactamase
inhibitor combination
PLAZOMICIN
Antibacterial
Aminoglycosides
POLYMYXIN B
Antibacterial
Polymyxins
POSACONAZOLE
Antifungal
Azoles
REMDESIVIR
Antiviral
Nucleotide Analog
REZAFUNGIN
Antifungal
Echinocandins
RIFAMPIN
Antibacterial
Rifampin

January 2024 Antimicrobial Use and Resistance Module
AUR
14-23
Antimicrobial Agent
Antimicrobial
Category
Antimicrobial
Class
a
Antimicrobial
Subclass
a
RIMANTADINE
Anti-influenza
M2 ion channel
inhibitors
SULBACTAM/
DURLOBACTAM
Antibacterial
β-lactam/β-lactamase
inhibitor combination
SULFAMETHOXAZOLE/
TRIMETHOPRIM
Antibacterial
Folate pathway
inhibitors
TEDIZOLID
Antibacterial
Oxazolidinones
TELAVANCIN
Antibacterial
Glycopeptides
Lipoglycopeptides
TETRACYCLINE
Antibacterial
Tetracyclines
TIGECYCLINE
Antibacterial
Glycylcyclines
TINIDAZOLE
Antibacterial
Nitroimidazoles
TOBRAMYCIN
Antibacterial
Aminoglycosides
VANCOMYCIN
Antibacterial
Glycopeptides
Glycopeptide
VORICONAZOLE
Antifungal
Azoles
ZANAMIVIR
Anti-influenza
Neuraminidase
inhibitors
a
Adapted from CLSI M100
12
b
While reported separately in the CDA file, Amikacin Liposomal will be rolled up and reported in the NHSN
AU Option analysis reports with Amikacin.
c
While reported separately in the CDA file, Colistin will be rolled up and reported in the NHSN AU Option
analysis reports with Colistimethate.
d
Per Paxlovid prescribing information, Nirmatrelvir must be co-administered with Ritonavir. However, for
public health surveillance, NHSN AU Option will be capturing only administered Nirmatrelvir.
e
Nirsevimab is a long-acting monoclonal antibody for the prevention of respiratory syncytial virus–
associated lower respiratory tract infection among infants and children aged <24 months.
(reference: Jones JM, Fleming-Dutra KE, Prill MM, et al. Use of Nirsevimab for the Prevention of
Respiratory Syncytial Virus Disease Among Infants and Young Children: Recommendations of the Advisory
Committee on Immunization Practices — United States, 2023. MMWR Morb Mortal Wkly Rep
2023;72:920–925. DOI: http://dx.doi.org/10.15585/mmwr.mm7234a4
.)

January 2024 Antimicrobial Use and Resistance Module
AUR
14-24
Appendix C. Example Calculations of Antimicrobial Days
Example 1. Example eMAR and Calculation of Antimicrobial Days
This example illustrates the antimicrobial days calculation for a patient receiving 1 gram Meropenem
intravenously every 8 hours and 1000mg Amikacin intravenously every 24 hours in the medical ward.
Table 1 provides an example of administered doses for this patient documented in eMAR. Table 2
illustrates the calculation of Meropenem and Amikacin days by antimicrobial (total) and stratified by route
of administration based on the administered doses of Meropenem and Amikacin documented in eMAR.
Table 3 illustrates the contribution of this patient’s antimicrobial days to the aggregate monthly report per
patient care location.
Table 1. Example eMAR for patient housed in Medical Ward
Medical Ward
Monday
December 28
Tuesday
December 29
Wednesday
December 30
Meropenem 1g
intravenously every 8 hours
Given: 2300
Given: 0700
Given: 1500
Given: 2300
Given: 0700
Amikacin 1000mg
intravenously every 24 hours
Given: 2300
Given: 2300
Table 2. Example of calculation of antimicrobial days
Calculation
Monday
December 28
Tuesday
December 29
Wednesday
December 30
Drug-specific Antimicrobial
Days (total)
Meropenem Days = 1
Amikacin Days = 1
Meropenem Days = 1
Amikacin Days = 1
Meropenem Days = 1
Amikacin Days = 0
Drug-specific Antimicrobial
Days Stratified by Route of
Administration
Meropenem Days (IV)
= 1
Amikacin Days
(IV) = 1
Meropenem Days
a
(IV) = 1
Amikacin Days
(IV) = 1
Meropenem Days
(IV) = 1
Amikacin Days
(IV) = 0
a
Please note, despite receiving three administrations of Meropenem on December 29, the patient only
contributed one total Meropenem antimicrobial day per calendar day.
Table 3. Example of antimicrobial days per month per patient care location
Month/
Year-Location
Antimicrobial
Agent
Drug-specific Antimicrobial Days
Total
IV
IM
Digestive
Respiratory
December
Medical Ward
Meropenem
3
3
0
0
0
December
Medical Ward
Amikacin
2
2
0
0
0

January 2024 Antimicrobial Use and Resistance Module
AUR
14-25
Example 2. Differences in Calculations for Patient Care Location and Facility-Wide Inpatient for a Patient
Transferred Between Patient Care Locations
This example illustrates the antimicrobial days calculation for a patient receiving 1 gram Vancomycin every
8 hours that was transferred from the MICU to a medical ward on December 1. Table 1 provides an
example of doses documented in eMAR administered to this patient in the MICU and Medical Ward. Table
2 illustrates the calculation of Vancomycin days by antimicrobial (total) and stratified by route of
administration based on the administered doses of Vancomycin documented in eMAR. One Vancomycin
day is attributed to both the MICU and Medical Ward locations since administrations took place in both
units during the calendar day. Further, despite receiving two administrations of Vancomycin in the
Medical Ward, the patient only attributes one total Vancomycin antimicrobial day for the Medical Ward
per calendar day. Table 3 shows the contribution of this patient’s Vancomycin days to the aggregate
monthly report per location and facility-wide inpatient. Note that while the patient attributes one total
Vancomycin day for both the MICU and the Medical Ward on December 1, only one total Vancomycin day
can be attributed to the FacWideIN count that calendar day.
Table 1. Example eMAR for patient transferred from MICU to Medical Ward on December 1
eMAR
Tuesday
December 1
Location: MICU
Tuesday
December 1
Location: Medical Ward
Vancomycin 1g intravenously every 8
hours
Given: 0700
Given: 1500
Given: 2300
Table 2. Example of calculation of antimicrobial days for December 1
Calculation
Tuesday
December 1
Location: MICU
Tuesday
December 1
Location: Medical Ward
Drug-specific Antimicrobial Days
(total)
Vancomycin Days = 1
Vancomycin Days = 1
Drug-specific Antimicrobial Days
Stratified by Route of Administration
Vancomycin Days (IV) = 1
Vancomycin Days (IV) = 1
Table 3. Example of antimicrobial days per month per patient care location and facility-wide inpatient
contributed from December 1
Month/
Year-Location
Antimicrobial
Agent
Drug-specific Antimicrobial Days
Total
IV
IM
Digestive
Respiratory
December
MICU
Vancomycin
1
1
0
0
0
December
Medical Ward
Vancomycin
1
1
0
0
0
December
Facility-wide inpatient
Vancomycin
1
1
0
0
0

January 2024 Antimicrobial Use and Resistance Module
AUR
14-26
Example 3. Calculation of Antimicrobial Days for a Patient Care Location when a Patient Admission
extends over Two Different Months
This example illustrates the antimicrobial days calculation for a patient receiving 1 gram Ceftriaxone
intravenously every 24 hours for two days in the Surgical Ward (but spanning different months). Table 1
provides an example of administered doses for this patient documented in eMAR. Table 2 illustrates the
calculation of Ceftriaxone days by antimicrobial (total) and stratification of route of administration
based upon the administered doses of Ceftriaxone documented in eMAR. Table 3 illustrates the
contribution of this patient’s Ceftriaxone days to the aggregate monthly report per patient care location.
Note: The patient’s FacWideIN admission (denominator) would be attributed to the month the patient
was first physically located in an inpatient location within the facility. In the scenario highlighted here,
the patient would attribute 1 admission to December and no admission to January (specifically, the
patient would not be counted in the total January admissions count). The patient would continue to
contribute one day present for each day the patient was in the location/facility.
Table 1. Example eMAR for patient housed in Surgical Ward
eMAR
Thursday
December 31
Location: Surgical Ward
Friday
January 1
Location: Surgical Ward
Ceftriaxone 1g intravenously
every 24 hours
Given: 0800
Given: 0800
Table 2. Example of calculation of antimicrobial days
Calculation
Thursday
December 31
Location: Surgical Ward
Friday
January 1
Location: Surgical Ward
Drug-specific Antimicrobial
Days (total)
Ceftriaxone Day = 1
Ceftriaxone Day = 1
Drug-specific Antimicrobial
Days Stratified by Route of
Administration
Ceftriaxone Day (IV) = 1
Ceftriaxone Day (IV) = 1
Table 3. Example of antimicrobial days per month per patient care location
Month/
Year-Location
Antimicrobial
Agent
Drug-specific Antimicrobial Days
Total
IV
IM
Digestive
Respiratory
December/
Surgical Ward
Ceftriaxone
1
1
0
0
0
January/
Surgical Ward
Ceftriaxone
1
1
0
0
0

January 2024 Antimicrobial Use and Resistance Module
AUR
14-27
Appendix D: List of SAARs
a
Table 1. Adult SAARs
SAAR Antimicrobial Agent
Category
Locations
SAAR Type in NHSN
All antibacterial agents
All Adult SAAR Locations
Adult_All-Antibacterial_2017
Broad spectrum
antibacterial agents
predominantly used for
hospital-onset infections
Adult Medical, Medical-Surgical,
Surgical ICUs
Adult_BSHO_ICU_2017
Adult Medical, Medical-Surgical,
Surgical Wards
Adult_BSHO_Ward_2017
Adult Step Down Units
Adult_BSHO_Step_2017
Adult General Hematology-Oncology
Wards
Adult_BSHO_ONC_2017
Broad spectrum
antibacterial agents
predominantly used for
community-acquired
infections
Adult Medical, Medical-Surgical,
Surgical ICUs
Adult_BSCA_ICU_2017
Adult Medical, Medical-Surgical,
Surgical Wards
Adult_BSCA_Ward_2017
Adult Step Down Units
Adult_BSCA_Step_2017
Adult General Hematology-Oncology
Wards
Adult_BSCA_ONC_2017
Antibacterial agents
predominantly used for
resistant Gram-positive
infections (e.g., MRSA)
Adult Medical, Medical-Surgical,
Surgical ICUs
Adult_GramPos_ICU_2017
Adult Medical, Medical-Surgical,
Surgical Wards
Adult_GramPos_Ward_2017
Adult Step Down Units
Adult_GramPos_Step_2017
Adult General Hematology-Oncology
Wards
Adult_GramPos_ONC_2017
Narrow spectrum beta-
lactam agents
Adult Medical, Medical-Surgical,
Surgical ICUs
Adult_NSBL_ICU_2017
Adult Medical, Medical-Surgical,
Surgical Wards
Adult_NSBL_Ward_2017
Adult Step Down Units
Adult_NSBL_Step_2017
Adult General Hematology-Oncology
Wards
Adult_NSBL_ONC_2017
Antibacterial agents
posing the highest risk for
CDI
Adult Medical, Medical-Surgical,
Surgical ICUs
Adult_CDI_ICU_2017
Adult Medical, Medical-Surgical,
Surgical Wards
Adult_CDI_Ward_2017
Adult Step Down Units
Adult_CDI_Step_2017
Adult General Hematology-Oncology
Wards
Adult_CDI_ONC_2017

January 2024 Antimicrobial Use and Resistance Module
AUR
14-28
SAAR Antimicrobial Agent
Category
Locations
SAAR Type in NHSN
Antifungal agents
predominantly used for
invasive candidiasis
Adult Medical, Medical-Surgical,
Surgical ICUs
Adult_Antifungal_ICU_2017
Adult Medical, Medical-Surgical,
Surgical Wards
Adult_Antifungal_Ward_2017
Adult Step Down Units
Adult_Antifungal_Step_2017
Adult General Hematology-Oncology
Wards
Adult_Antifungal_ONC_2017
Table 2: Pediatric SAARs
SAAR Antimicrobial Agent
Category
Locations
SAAR Type in NHSN
All antibacterial agents
All Pediatric locations
Ped_All-Antibacterial_2017
Broad spectrum
antibacterial agents
predominantly used for
hospital-onset infections
Pediatric Medical and Medical-Surgical
ICUs
Ped_BSHO_ICU_2017
Pediatric Medical, Medical-Surgical,
Surgical Wards
Ped_BSHO_Ward_2017
Broad spectrum
antibacterial agents
predominantly used for
community-acquired
infections
Pediatric Medical and Medical-Surgical
ICUs
Ped_BSCA_ICU_2017
Pediatric Medical, Medical-Surgical,
Surgical Wards
Ped_BSCA_Ward_2017
Antibacterial agents
predominantly used for
resistant Gram-positive
infections (e.g., MRSA)
Pediatric Medical and Medical-Surgical
ICUs
Ped_GramPos_ICU_2017
Pediatric Medical, Medical-Surgical,
Surgical Wards
Ped_GramPos_Ward_2017
Narrow spectrum beta-
lactam agents
Pediatric Medical and Medical-Surgical
ICUs
Ped_NSBL_ICU_2017
Pediatric Medical, Medical-Surgical,
Surgical Wards
Ped_NSBL_Ward_2017
Azithromycin
Pediatric Medical and Medical-Surgical
ICUs
Ped_Azith_ICU_2017
Pediatric Medical, Medical-Surgical,
Surgical Wards
Ped_Azith_Ward_2017
Antibacterial agents posing
the highest risk for CDI
Pediatric Medical and Medical-Surgical
ICUs
Ped_CDI_ICU_2017
Pediatric Medical, Medical-Surgical,
Surgical Wards
Ped_CDI_Ward_2017

January 2024 Antimicrobial Use and Resistance Module
AUR
14-29
SAAR Antimicrobial Agent
Category Locations SAAR Type in NHSN
Antifungal agents
predominantly used for
invasive candidiasis
Pediatric Medical and Medical-Surgical
ICUs
Ped_Antifungal_ICU_2017
Pediatric Medical, Medical-Surgical,
Surgical Wards
Ped_Antifungal_Ward_2017
Table 3: Neonatal SAARs
SAAR Antimicrobial Agent
Category
Locations
SAAR Type in NHSN
All antibacterial agents
Special Care Nursery (Level II),
Neonatal Critical Care (Level II/III),
Neonatal Critical Care (Level III),
Neonatal Critical Care (Level IV)
Neo_All-antibacterial_2018
Vancomycin predominantly
used for treatment of late-
onset sepsis
Special Care Nursery (Level II),
Neonatal Critical Care (Level II/III),
Neonatal Critical Care (Level III),
Neonatal Critical Care (Level IV)
Neo_Vancomycin_2018
Broad spectrum
antibacterial agents
predominantly used for
hospital-onset infections
Special Care Nursery (Level II),
Neonatal Critical Care (Level II/III),
Neonatal Critical Care (Level III),
Neonatal Critical Care (Level IV)
Neo_BSHO_2018
Third generation
Cephalosporins
Special Care Nursery (Level II),
Neonatal Critical Care (Level II/III),
Neonatal Critical Care (Level III),
Neonatal Critical Care (Level IV)
Neo_3G-
Cephalosporins_2018
Ampicillin predominantly
used for treatment of
early-onset sepsis
Special Care Nursery (Level II),
Neonatal Critical Care (Level II/III),
Neonatal Critical Care (Level III),
Neonatal Critical Care (Level IV)
Neo_Ampicillin_2018
Aminoglycosides
predominantly used for
treatment of early-onset
and late-onset sepsis
Special Care Nursery (Level II),
Neonatal Critical Care (Level II/III),
Neonatal Critical Care (Level III),
Neonatal Critical Care (Level IV)
Neo_Aminoglycosides_2018
Fluconazole predominantly
used for candidiasis
Neonatal Critical Care (Level II/III),
Neonatal Critical Care (Level III),
Neonatal Critical Care (Level IV)
Neo_Fluconazole_2018
a
Users can find 2014 baseline SAAR details here: https://www.cdc.gov/nhsn/pdfs/ps-analysis-
resources/aur/saar-2014-508.pdf

January 2024 Antimicrobial Use and Resistance Module
AUR
14-30
Appendix E: Antimicrobial Groupings for SAAR & Rate Table
Calculations
a
Adult SAAR Antimicrobial Agent Categories
Adult All antibacterial agents
All antibacterial agents in the AUR protocol except:
• AMIKACIN LIPOSOME
• CEFIDEROCOL
• COLISTIN
• DELAFLOXACIN
• ERAVACYCLINE
• IMIPENEM/CILATATIN/RELEBACTAM
• LEFAMULIN
• MEROPENEM/VABORBACTAM
• OMADACYCLINE
• PIPERACILLIN
• PLAZOMICIN
• SULBACTAM/DURLOBACTAM
• TICARCILLIN/CLAVULANATE
Adult Broad spectrum antibacterial agents predominantly used for hospital-onset infections
• AMIKACIN (IV only)
• AZTREONAM (IV only)
• CEFEPIME
• CEFTAZIDIME
• DORIPENEM
• GENTAMICIN (IV only)
• IMIPENEM/CILASTATIN
• MEROPENEM
• PIPERACILLIN/TAZOBACTAM
• TOBRAMYCIN (IV only)
Adult Broad spectrum antibacterial agents predominantly used for community-acquired infections
• CEFACLOR
• CEFDINIR
• CEFIXIME
• CEFOTAXIME
• CEFPODOXIME
• CEFPROZIL
• CEFTRIAXONE

January 2024 Antimicrobial Use and Resistance Module
AUR
14-31
• CEFUROXIME
• CIPROFLOXACIN
• ERTAPENEM
• GEMIFLOXACIN
• LEVOFLOXACIN
• MOXIFLOXACIN
Adult Antibacterial agents predominantly used for resistant Gram-positive infections (e.g., MRSA)
• CEFTAROLINE
• DALBAVANCIN
• DAPTOMYCIN
• LINEZOLID
• ORITAVANCIN
• QUINUPRISTIN/DALFOPRISTIN
• TEDIZOLID
• TELAVANCIN
• VANCOMYCIN (IV only)
Adult Narrow spectrum beta-lactam agents
• AMOXICILLIN
• AMOXICILLIN/CLAVULANATE
• AMPICILLIN
• AMPICILLIN/SULBACTAM
• CEFADROXIL
• CEFAZOLIN
• CEFOTETAN
• CEFOXITIN
• CEPHALEXIN
• DICLOXACILLIN
• NAFCILLIN
• OXACILLIN
• PENICILLIN G
• PENICILLIN V
Adult Antibacterial agents posing the highest risk for CDI
This category contains antimicrobials that are part of other SAAR categories.
• CEFDINIR
• CEFEPIME
• CEFIXIME
• CEFOTAXIME
• CEFPODOXIME
• CEFTAZIDIME

January 2024 Antimicrobial Use and Resistance Module
AUR
14-32
• CEFTRIAXONE
• CIPROFLOXACIN
• CLINDAMYCIN
• GEMIFLOXACIN
• LEVOFLOXACIN
• MOXIFLOXACIN
Adult Antifungal agents predominantly used for invasive candidiasis
• ANIDULAFUNGIN
• CASPOFUNGIN
• FLUCONAZOLE
• MICAFUNGIN
Adult Rate Table
Adult Antibacterial agents predominantly used for extensively antibiotic resistant bacteria
• CEFTAZIDIME/AVIBACTAM
• CEFTOLOZANE/TAZOBACTAM
• COLISTIMETHATE (IV only)
• POLYMYXIN B (IV only)
• TIGECYCLINE
Pediatric SAAR Antimicrobial Agent Categories
Pediatric All antibacterial agents
All antibacterial agents in the AUR protocol except:
• AMIKACIN LIPOSOME
• CEFIDEROCOL
• COLISTIN
• DELAFLOXACIN
• ERAVACYCLINE
• IMIPENEM/CILATATIN/RELEBACTAM
• LEFAMULIN
• MEROPENEM/VABORBACTAM
• OMADACYCLINE
• PIPERACILLIN
• PLAZOMICIN
• SULBACTAM/DURLOBACTAM
• TICARCILLIN/CLAVULANATE
Pediatric Broad spectrum antibacterial agents predominantly used for hospital-onset infections
• AMIKACIN (IV only)

January 2024 Antimicrobial Use and Resistance Module
AUR
14-33
• AZTREONAM (IV only)
• CEFEPIME
• CEFTAZIDIME
• CIPROFLOXACIN
• DORIPENEM
• ERTAPENEM
• GEMIFLOXACIN
• IMIPENEM/CILASTATIN
• LEVOFLOXACIN
• MEROPENEM
• MOXIFLOXACIN
• PIPERACILLIN/TAZOBACTAM
• TOBRAMYCIN (IV only)
Pediatric Broad spectrum antibacterial agents predominantly used for community-acquired infections
• AMOXICILLIN/CLAVULANATE
• AMPICILLIN/SULBACTAM
• CEFACLOR
• CEFDINIR
• CEFIXIME
• CEFOTAXIME
• CEFPODOXIME
• CEFPROZIL
• CEFTRIAXONE
• CEFUROXIME
Pediatric Antibacterial agents predominantly used for resistant Gram-positive infections (e.g., MRSA)
• CEFTAROLINE
• CLINDAMYCIN
• DALBAVANCIN
• DAPTOMYCIN
• LINEZOLID
• ORITAVANCIN
• QUINUPRISTIN/DALFOPRISTIN
• TEDIZOLID
• TELAVANCIN
• VANCOMYCIN (IV only)
Pediatric Narrow spectrum beta-lactam agents
• AMOXICILLIN
• AMPICILLIN
• CEFADROXIL
• CEFAZOLIN
• CEFOTETAN

January 2024 Antimicrobial Use and Resistance Module
AUR
14-34
• CEFOXITIN
• CEPHALEXIN
• DICLOXACILLIN
• NAFCILLIN
• OXACILLIN
• PENICILLIN G
• PENICILLIN V
Pediatric Azithromycin
• AZITHROMYCIN
Pediatric Antibacterial agents posing the highest risk for CDI
This category contains antimicrobials that are part of other SAAR categories.
• CEFDINIR
• CEFEPIME
• CEFIXIME
• CEFOTAXIME
• CEFPODOXIME
• CEFTAZIDIME
• CEFTRIAXONE
• CIPROFLOXACIN
• CLINDAMYCIN
• GEMIFLOXACIN
• LEVOFLOXACIN
• MOXIFLOXACIN
Pediatric Antifungal agents predominantly used for invasive candidiasis
• ANIDULAFUNGIN
• CASPOFUNGIN
• FLUCONAZOLE
• MICAFUNGIN
Pediatric Rate Table
Pediatric Antibacterial agents predominantly used for extensively antibiotic resistant bacteria
• CEFTAZIDIME/AVIBACTAM
• CEFTOLOZANE/TAZOBACTAM
• COLISTIMETHATE (IV only)
• POLYMYXIN B (IV only)
• TIGECYCLINE
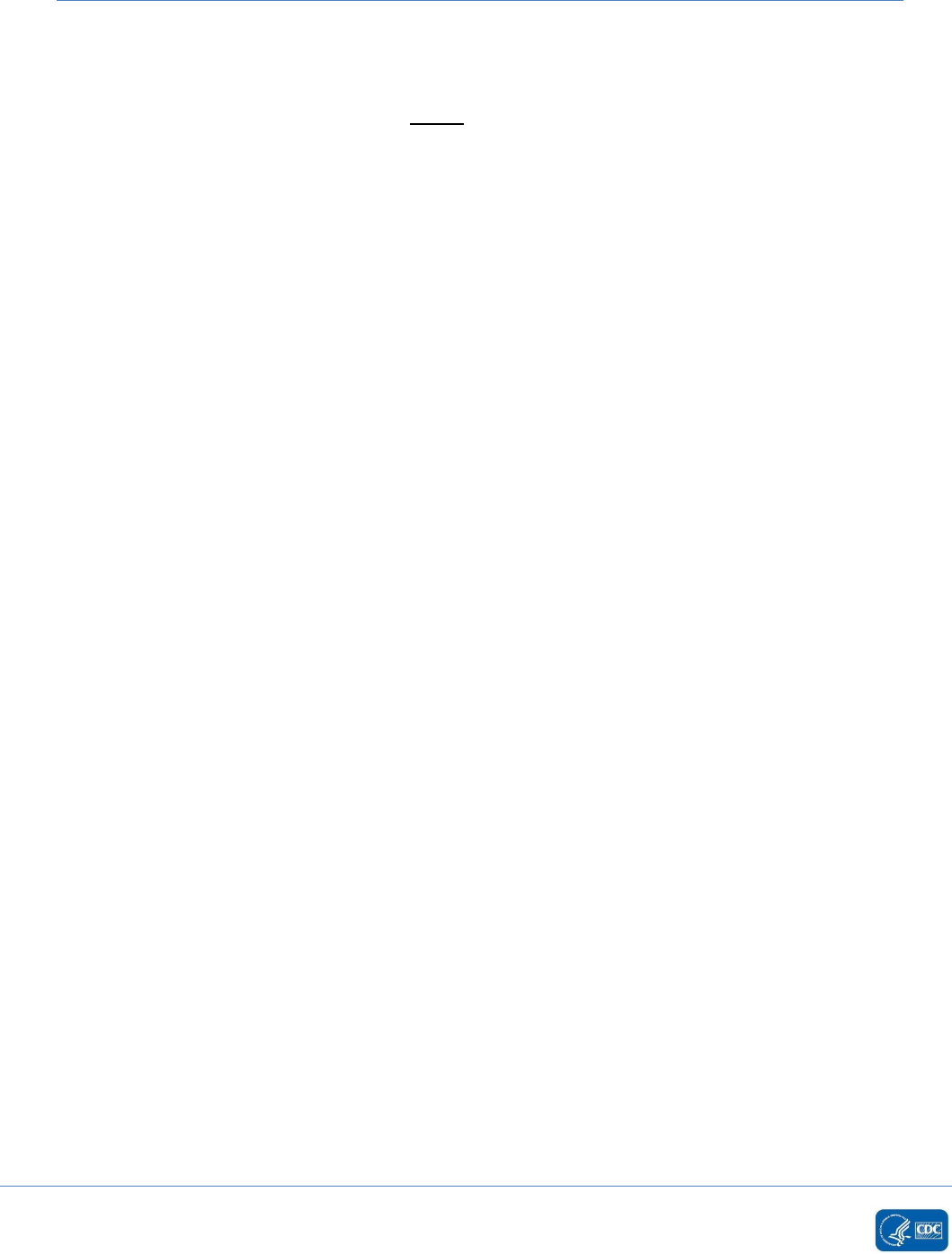
January 2024 Antimicrobial Use and Resistance Module
AUR
14-35
Neonatal SAAR Antimicrobial Agent Categories
Neonatal All antibacterial agents
All antibacterial agents in the AUR protocol except:
• AMIKACIN LIPOSOME
• CEFIDEROCOL
• CHLORAMPHENICOL
• COLISTIN
• DALBAVACIN
• DELAFLOXICIN
• DORIPENEM
• DOXYCYCLINE
• ERAVACYCLINE
• ERYTHROMYCIN/SULFISOXAZOLE
• GEMIFLOXACIN
• IMIPENEM/CILASTATIN/RELEBACTAM
• MEROPENEM/VABORBACTAM
• MINOCYCLINE
• OMADACYCLINE
• ORITIVANCIN
• PIPERACILLIN
• PLAZOMICIN
• SULBACTAM/DURLOBACTAM
• TETRACYCLINE
• TIGECYCLINE
Neonatal Vancomycin predominantly used for treatment of late-onset sepsis
• VANCOMYCIN (IV only)
Neonatal Broad spectrum antibacterial agents predominantly used for hospital-onset infections
• CEFEPIME (IV only)
• ERTAPENEM (IV only)
• IMIPENEM/CILASTATIN (IV only)
• MEROPENEM (IV only)
• PIPERACILLIN/TAZOBACTAM (IV only)
Neonatal Third generation Cephalosporins
• CEFOTAXIME (IV only)
• CEFTAZIDIME (IV only)
• CEFTRIAXONE (IV only)
Neonatal Ampicillin predominantly used for treatment of early-onset sepsis
• AMPICILLIN (IV only)

January 2024 Antimicrobial Use and Resistance Module
AUR
14-36
Neonatal Aminoglycosides predominantly used for treatment of early-onset and late-onset sepsis
• AMIKACIN (IV only)
• GENTAMICIN (IV only)
• TOBRAMYCIN (IV only)
Neonatal Fluconazole predominantly used for candidiasis
• FLUCONAZOLE (IV and oral only)
Neonatal Rate Tables
Fluconazole predominantly used for candidiasis used in Level II special care neonatal nurseries
• FLUCONAZOLE
Ampicillin predominantly used for treatment of early-onset sepsis used in well baby nurseries
• AMPICILLIN (IV only)
Aminoglycosides predominantly used for treatment of early-onset and late-onset sepsis used in well
baby nurseries
• AMIKACIN (IV Only)
• GENTAMICIN (IV Only)
• TOBRAMYCIN (IV Only)
a
Users can find 2014 baseline SAAR details here: https://www.cdc.gov/nhsn/pdfs/ps-analysis-
resources/aur/saar-2014-508.pdf

January 2024 Antimicrobial Use and Resistance Module
AUR
14-37
2. Antimicrobial Resistance (AR) Option
Introduction
The proportion of isolates resistant to specific antimicrobial agents is a common measure of
antimicrobial resistance. Proportion susceptible (%S) can aid in clinical decision making (hospital
antibiograms) and assessing the impact of transmission prevention and antimicrobial stewardship
success, although the measure may not be very sensitive to measuring success of short-term efforts.
Proportion susceptible also facilitates local or regional assessment of progression or improvement of a
particular resistance problem to guide local or regional transmission prevention efforts. Validity of local
and regional assessments of the magnitude of a particular resistance phenotype can be improved by
using standardized methodology for aggregating proportion resistant.
Objectives:
1. Facilitate antimicrobial resistance data evaluation using a standardized approach to:
a. Provide local practitioners with an improved awareness of a variety of antimicrobial
resistance problems to aid in clinical decision making and prioritize transmission
prevention efforts.
b. Provide facility-specific measures in context of a regional and national perspective
(specifically, benchmarking) that can inform decisions to accelerate transmission
prevention efforts and reverse propagation of emerging or established resistant
pathogens.
2. Allow regional and national assessment of antimicrobial resistant organisms of public health
importance, including ecologic and infection burden assessment.
Methodology:
The AR Option reports antimicrobial resistance data as a proportion.
1
The proportion susceptible is
defined as the number of susceptible isolates divided by the number of isolates tested for the specific
antimicrobial agent being evaluated. For each facility, the numerator (specifically, number of susceptible
isolates) is derived from isolate-level reports submitted. The ultimate source of the isolate data included
in these reports is the laboratory information system (LIS). Laboratory results data from the electronic
health record system (EHRs) can be used to populate the AR Option numerator records submitted to
NHSN in healthcare settings where the LIS is directly connected to the EHRs. The AR Option obtains
denominators of patient days and admissions from the ADT system (or similar system that allows for
electronic access of required data elements). Facilities must not employ manual means of data
collection to report AR Option data to NHSN. Facilities that do not have access to discrete data elements
needed for AR Option reporting are not eligible to participate in the AR Option. For example, facilities
receiving results via PDF or fax will not be able to participate in the AR Option as those data are not
saved as discrete fields. The sections below further define the numerator and denominator, which must
adhere to the data format specified by the Health Level 7 (HL7) CDA Implementation Guide
developed
by the CDC and HL7.
2
Manual data entry is not available for the AR Option.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-38
Settings:
All inpatient facilities enrolled in NHSN and using the Patient Safety Component can participate in the AR
Option. This includes facilities enrolled as general acute care hospitals, critical access hospitals,
children’s hospitals, long term acute care hospitals, pediatric long term acute care hospitals, military and
veterans’ hospitals, oncology hospitals, orthopedic hospitals, psychiatric hospitals, rehabilitation
hospitals, surgical hospitals, women’s hospitals, women’s and children’s hospitals, government and non-
government hospitals for public health emergencies. Participating facilities must be able to collect the
numerator and denominator data electronically and upload those data into NHSN using the required
CDA specifications. NHSN does not currently support AR Option data submission from long term care
facilities (for example, skilled nursing facilities and nursing homes) nor outpatient dialysis facilities.
NHSN strongly encourages reporting specimens at each facility from all NHSN defined inpatient locations
(including inpatient procedural areas like operating rooms) and three select outpatient locations:
Emergency Department (ED), Pediatric ED, and 24-hour Observation Area from which the numerator
data can be accurately electronically captured. The AR Option does not accept specimens collected in
other outpatient location types, such as outpatient clinics. The denominators of patient days and
admissions are only reported at the facility-wide inpatient level (FacWideIN). The denominator of
outpatient encounters is reported separately from the three select outpatient location types: ED,
Pediatric ED, and 24-hour Observation Area. Previous experience with AUR Module implementation
suggests that reporting from all NHSN patient care locations is easier than reporting from selected
locations.
Requirements
Each month:
1. The facility must indicate they plan to submit AR Option data on the
Patient Safety Monthly
Reporting Plan.
a. The facility must add FacWideIN to the plan to report AR Option data from inpatient
locations. Individual inpatient locations should not be listed in the AR Option plan.
b. The facility must add each outpatient location separately to report AR Option data from the
three select outpatient location types.
2. The facility must report two record types for each month of surveillance.
a. One event file for each isolate-based report.
i. Isolate is defined as a population of a single organism observed in a culture obtained
from a patient specimen.
ii. Each AR Option event file contains the specific location of specimen collection.
iii. Note: If the facility has no AR Events to report (specifically, there were no isolates that
met the AR Option inclusion criteria), the facility can select the box on the NHSN Alert
screen to report “No AR Events”. More information can be found here:
Report No AR
Events Guide.
b. One summary file for the FacWideIN denominator data report and one summary file for
each outpatient location listed in the reporting plan.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-39
NHSN recommends AR Option data be submitted to NHSN for a given calendar month by the end of the
subsequent calendar month. However, facilities should wait at least seven calendar days following the
end of the month before submitting data to ensure the lab completed all susceptibility testing and
reported results back to the EHRs.
Isolate-based report
The facility must report all required data each month for each eligible isolate-based report (See
Appendix F
). The facility should only consider specimens collected in an inpatient or select outpatient
location (ED, pediatric ED, and 24-hour observation) for eligibility. Additionally, the facility should only
report specimens to the AR Option with susceptibility testing. For example, if a facility isolates Candida
albicans from a urine specimen but does not perform susceptibility testing on that isolate, the isolate is
not eligible for reporting to the AR Option.
The facility should report all eligible isolates that meet the reporting guidelines outlined in this protocol
to NHSN regardless of the antimicrobial resistance of the isolated organism. This means that even
isolates that are susceptible to all required antimicrobials are eligible to be reported to the AR Option.
Additionally, isolates in which all the NHSN required antimicrobials were not tested, but at least one
non-required drug was tested, are eligible to be reported into NHSN. For example, if a facility tested a
Staphylococcus aureus isolate for the non-required drug Telithromycin and none of the other 27 NHSN
required antimicrobials were tested, that isolate would still be considered eligible for reporting to the
AR Option. This is consistent with CLSI M39 Guidance on reporting cumulative susceptibility test results.
3
Non-culture based organism identification results (for example, T2 Magnetic Resonance [T2MR] or
Karius Test) should not be submitted.
Report two distinct events based on specimens obtained in inpatient and select outpatient locations
with susceptibility testing performed:
1. Each eligible organism isolated from an invasive source (blood or cerebrospinal fluid [CSF]) per
patient, per 14 day period even across calendar months:
a. There should be 14 days with no positive culture result from the laboratory for the
patient and specific organism before the facility enters another invasive source AR Event
into NHSN for the patient and specific organism. NOTE: The date of specimen collection
is considered Day 1.
b. After >14 days have passed with no positive culture results for that specific organism,
the facility can report another positive culture from an invasive source with that specific
organism as an AR Event. For example, if a facility obtained a positive blood culture from
a patient on January 1, the earliest another invasive specimen could be reported to
NHSN for that same patient and organism would be January 15 (assuming there were no
positive blood or CSF cultures in the interim).
2. The first eligible organism isolated from any eligible non-invasive culture source (lower
respiratory or urine), per patient, per month.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-40
a. Only one AR event is allowed per calendar month for the same patient/organism for
lower respiratory or urine specimens.
Note: The AR Option 14 day rule starts with the day of specimen collection and applies only to those
specimens collected in an inpatient location or select outpatient location (ED, pediatric ED, or 24-hour
observation area) in the reporting facility. Outpatient locations other than the ED, pediatric ED, and 24-
hour observation area (for example, wound clinic or outpatient laboratory) should not be included in the
14 day rule. Further, cultures obtained while the patient was at another healthcare facility should not be
included in the 14 day calculations.
A. Eligible organisms
Facilities and vendors should refer to the AR Option Pathogen Roll-up Workbook found in the
Antimicrobial Resistance Toolkit
for eligible organisms for AR Option reporting and the complete list
of their associated SNOMED codes. All organisms in the Workbook are eligible for reporting.
Facilities and vendors should first rollup the eligible organisms using the Pathogen Roll-up Workbook
before applying the isolate selection rules and rules for the removal of same day duplicates. Refer to
the AR Option Pathogen Roll-up Reference Guide, also found in the AR Toolkit, for guidance using
the workbook and determining which SNOMED codes are accepted into NHSN.
Eligible organisms include:
• All Acinetobacter species
• Candida albicans
• Candida auris
• Candida glabrata
• Candida parapsilosis
• Candida tropicalis
• Citrobacter amalonaticus
• Citrobacter braakii
• Citrobacter freundii
• Citrobacter freundii complex
• Citrobacter koseri
• Citrobacter youngae
• All Enterobacter species
• All Enterococcus species
• Escherichia coli
• Klebsiella aerogenes
• Klebsiella oxytoca
• Klebsiella pneumoniae
• Morganella morganii
• Proteus mirabilis
• Proteus penneri
• Proteus vulgaris
• Pseudomonas aeruginosa

January 2024 Antimicrobial Use and Resistance Module
AUR
14-41
• Serratia marcescens
• Staphylococcus aureus
• Stenotrophomonas maltophilia
• Streptococcus agalactiae
• Streptococcus pneumoniae
B. Specimen Sources
Eligible specimen source groups include blood, CSF, urine, and lower respiratory. Facilities and vendors
should refer to the Specimen Source tab of Information Data Model (IDM) found in the
Antimicrobial
Resistance Toolkit for the complete list of eligible specimen sources and their associated SNOMED
codes. Facilities should only report those SNOMED codes listed in the AR Specimen Source value set on
the Specimen Source tab in the IDM. Do not include SNOMED children specimen types unless specifically
listed. Wound specimens are not eligible for reporting into the AR Option.
1. Eligible invasive specimen sources include cerebrospinal fluid (CSF) and blood specimens. (
Table
1)
Note: Report blood or CSF cultures growing the same eligible specific organism (genus and
species or genus only if the species has not been identified) only if the patient had no positive
blood or CSF culture result with that specific organism (genus and species or genus only if the
species has not been identified) within the last 14 days, even across calendar months.
2. Eligible non-invasive specimen sources include lower respiratory (for example, sputum,
endotracheal, bronchoalveolar lavage) and urine specimens.
Table 1: Example of 14 day rule for a specific organism from a single patient in an inpatient
location
Date Lab Result
Reported to
NHSN? Justification
January 1
Staphylococcus aureus
isolated from blood
culture
Yes
Patient’s first blood culture of inpatient
admission; Staphylococcus aureus is
isolated; facility reports AR Event into
NHSN.
January 4
Staphylococcus aureus
isolated from blood
culture
No
It has been less than 14 days since the
last positive culture (January 1) from the
patient isolating Staphylococcus aureus.
January 16
Staphylococcus aureus
isolated from CSF
culture
No
It has been less than 14 days since the
last positive culture (January 4) from the
patient isolating Staphylococcus aureus.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-42
Date
Lab Result
Reported to
NHSN?
Justification
January 31
Staphylococcus aureus
isolated from blood
culture
Yes
It has more than 14 days since the last
positive culture (January 16) from the
patient isolating Staphylococcus aureus;
facility reports AR Event into NHSN.
The facility should evaluate all isolate test results using either the algorithm in Figure 1
(Invasive
specimens) or Figure 2 (Non-invasive specimens) to determine reportable AR events for each calendar
month.
• For eligible invasive specimens, there should be 14 days with no positive culture result from the
laboratory for the patient and specific organism before the facility enters another invasive source
AR Event into NHSN for the patient and specific organism (Figure 1
). Based on the 14 day rule, at
a maximum, a patient would have no more than three invasive isolates per specific organism
reported per month.
• For eligible non-invasive specimens, the facility should report all first non-invasive isolates
(chronologically) per patient, per month, per organism as an AR Event (Figure 2
).
C. Required Data
Required data include data available from the LIS, EHRs, and administrative data systems. The set of
variables for each isolate consists of a variable to identify the NHSN facility, specimen-/patient-related
data, and antimicrobial susceptibility data as outlined below.
For additional information on each variable please see Appendix G
.
• Facility identifier
o Unique NHSN Facility ID (Object Identifier [OID] is used in the CDA)
• Specimen-/Patient-related data
o Patient identifier
o Date of birth
o Gender
o Race (optional variable)
o Ethnicity (optional variable)
o Whether the patient was admitted to the facility during the encounter (True/False)
o Date admitted to facility (see details in Appendix G
)
o Specimen collection date
o Specimen source
o Location code (mapped to CDC location codes)
o Isolate identifier (unique isolate ID in the electronic laboratory report based upon the
isolate being reported with its own AST results)
o Organism (Appendix F
)

January 2024 Antimicrobial Use and Resistance Module
AUR
14-43
• Antimicrobial susceptibility data
o Antimicrobial (Appendix F
)
o Penicillin-binding protein 2a-agglutination (PBP2a) (required only if Staphylococcus
aureus)
o Polymerase chain reaction (PCR) mec-gene (required only if Staphylococcus aureus)
o E-test sign
o E-test value & unit of measure
o Interpretation of E-test
o Minimum Inhibitory Concentration (MIC) sign
o MIC value & unit of measure
o Interpretation of MIC test
o Disk diffusion (Kirby-Bauer or KB) test sign
o Disk diffusion (KB) test value & unit of measure
o Interpretation of disk diffusion (KB) test
o Final interpretation result
Notes:
• While many of these fields are required in the CDA report, facilities unable to electronically
obtain the results of the individual laboratory tests (specifically, E-test, MIC, Disk diffusion [KB])
may still report AR Option data by using “NA” to indicate “Not Tested” for these specific tests as
long as the final interpretation result can be provided for each antimicrobial tested.
• Only the lab tests listed above can be included in the CDA report. However, if your lab uses
additional tests like the cefoxitin screen or inducible clindamycin test and uses the results of the
additional test to change/amend the final interpretation for a given drug included in our panel,
we’d like you to report the same result you sent to the clinician to NHSN. For example, if the lab
updated the result for erythromycin based on the result of the inducible clindamycin test, you
should report the changed erythromycin result (same result reported to clinician) to NHSN.
• Facilities unable to electronically obtain the results of the PBP2a-agglutination and/or PCR mec-
gene tests for Staphylococcus aureus may report “Unknown” for these specific tests.
• Facilities should not employ manual means of data collection to report AR Option data to NHSN.
D. Reporting Guidelines
• Interpretation of test results (E-test, MIC test, Disk diffusion [KB] test) includes the following
results:
o S = Susceptible
o S-DD = Susceptible-Dose Dependent
o I = Intermediate
o R = Resistant
o NS = Non-Susceptible
o NA = Not Tested
Note: After upload into NHSN, Not Tested values appear as “N”.
o Specific to Gentamicin and Streptomycin results for Enterococcus testing high-level
resistance:

January 2024 Antimicrobial Use and Resistance Module
AUR
14-44
S = Susceptible/Synergistic
R = Resistant/Not Synergistic
• Facilities should only report final or corrected susceptibility testing to NHSN. Do not report
preliminary laboratory results for NHSN AR Option reporting.
• In circumstances where different breakpoints are required, rely on the specimen source to
determine which susceptibility results to report.
o If the specimen source is CSF, report the meningitis breakpoint susceptibility.
o If the specimen source is blood, urine, or lower respiratory, report the non-meningitis
breakpoint susceptibility.
• Facilities should report results based on clinical, not epidemiological, breakpoints.
• All organisms listed in the AR Option Pathogen Roll-up Workbook found in the
Antimicrobial
Resistance Toolkit are eligible for submission. Facilities/vendors should first perform the roll-up
of organisms before applying subsequent reporting rules.
E. Removal of Same Day Duplicates
Multiple isolates of the same organism from the same specimen may produce conflicting results.
Facilities should only report one isolate to NHSN, retaining the unique nature of the test results.
Facilities must follow the rules listed below to ensure removal of duplicate isolate reports.
Duplicates are defined as same species or genus, when identification to species level is not provided,
isolated from the same source type (specifically, invasive or non-invasive) from the same patient on
the same day. For example, if a patient has a blood specimen and urine specimen collected on the
same day and E.coli is isolated from both, because the specimens are from two different source
types (invasive vs non-invasive), they are not considered duplicates.
Select the isolate to report to NHSN based on these rules (see Figure 3
):
• For invasive source isolate selection, select CSF isolates over blood isolates.
• For non-invasive source isolate selection, select lower respiratory isolates over urine
isolates.
• Eliminate isolates on same day without susceptibility test results. Only report isolates with
complete/final laboratory testing to NHSN.
• Do not merge test results across multiple isolates (specifically, don’t summarize results
across different isolates tested on same day).
• If two isolates from the same day have conflicting susceptibilities to the panel of
antimicrobials tested, report the isolate with the most resistant final interpretation (NS > R >
I > S-DD > S > NA).
o If the lab validated susceptibility results of both isolates but did not provide a final
interpretation, report the isolate with the higher amount of drug resistance based
on the number of antimicrobials testing first “NS”, if equal amount of “NS” then
move to the amount of “R”, then “I”, then “S-DD” then “S”.
For example, a facility isolated Candida albicans from two blood specimens
collected from the same patient on the same calendar day and the lab
validated susceptibility results from both isolates. The first isolate tested “R”
to three of the eight antimicrobials and the second isolate tested “R” to four
of the eight antimicrobials. The facility should report the second isolate to
NHSN because it showed the higher amount of resistance.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-45
o If two or more isolates have the same number of antimicrobials testing “NS”, “R”,
“I”, “S-DD” and “S” and it cannot be determined which is most resistant, then report
the isolate that was the first entered into the LIS.
o Do not consider results from drugs that are outside of the NHSN-specified drug
panels when determining which isolate to report.
• If the lab performs the same test on the same isolate but the two tests produce conflicting
results, report the final interpretation provided by the lab.
o If the lab did not provide a final interpretation, then report the most resistant
interpretation (NS > R > I > S-DD > S > NA) for that specific antimicrobial.
For example, if a facility performs two E-tests for the same drug on the
same isolate and one produces “Intermediate” while the other produces
“Susceptible”, report “Intermediate” as the final interpretation for that
specific drug susceptibility.
• If the lab performs specific antimicrobial tests on the same isolate that produce conflicting
susceptibility interpretations, and the laboratory did not provide a final summary
interpretation, report the most resistant specific test interpretation as the final
interpretation (NS > R > I > S-DD > S > NA) for that specific antimicrobial.
o For example, if drug susceptibility results produced MIC = Resistant and E-Test =
Intermediate but the lab did not provide a final interpretation, report “Resistant” as
the final interpretation for that specific antimicrobial susceptibility.
Denominator Data
For each month, report combined denominator data for all inpatient locations within the facility (facility-
wide inpatient [FacWideIN]): (See Appendix H
f
or details)
1. Patient Days: Number of patients present in the facility at the same time on each day of the
month, summed across all days in the month.
2. Admissions: Number of patients admitted to an inpatient location in the facility each month.
a. A patient is counted as an admission when they arrive in an NHSN designated inpatient
location regardless of patient status (for example, inpatient, observation).
b. A patient admitted to an inpatient unit would be counted as an admission even if they
were discharged that same calendar day.
c. A patient transfer from an inpatient to an outpatient ED, pediatric ED, or 24hr
observation location then back to an inpatient location is counted as two separate
admissions.
d. Please note, the admissions definition used in the AUR Module is different than the
definition used in the NHSN MDRO/CDI Module.
Note: Neither the patient days nor admissions denominators should include the counts from
outpatient locations (ED, pediatric ED, and 24-hour observation area).
Report outpatient encounters for the three select outpatient locations: ED, Pediatric ED, and 24-hour
Observation Area:
1. Encounters: A visit to an eligible outpatient location counts as a single encounter. The patient
can begin attributing to the encounters count in an outpatient location such as an Emergency
Department as soon as triage is completed, regardless of when the patient is placed in a bed.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-46
a. If the patient’s stay in any eligible outpatient location continues into subsequent
calendar days, that patient should still be counted as 1 encounter. For example:
i. If the patient arrives in the ED on Monday and remains in the ED until
Wednesday, that patient should be counted as 1 encounter within the ED.
b. If the patient transfers from one outpatient location to another within the same facility,
that patient should be counted as 1 encounter for the first outpatient location and
should not be counted as an encounter for the receiving location (specifically, a patient
should not contribute two encounters when transferring between outpatient locations
in the same facility). For example:
i. If the patient arrives in the ED on Monday then is transferred to the 24hr
Observation Area on Tuesday, the patient should be counted only as 1
encounter within the ED and zero encounters within the 24hr Observation Area.
c. If the patient is discharged, or leaves, then returns to that outpatient unit during the
same calendar day, that patient should be counted as 2 encounters. For example:
i. If the patient arrives in the ED at 07:00 on Monday, is discharged at 11:00 on
Monday then returns to the ED at 18:00 on Monday, that patient counts as two
separate encounters for the ED.
d. If the patient transfers from outpatient to inpatient, then to outpatient, the second
outpatient stay (assuming it’s in an eligible location) would be considered a new
encounter because there was time spent in an inpatient location. For example:
i. If the patient arrives in the ED on Monday, is admitted or transferred to the
medical ICU on Monday then is transferred to the 24hr Observation Unit on
Tuesday and admitted or transferred back to the medical ward on Tuesday, the
patient contributes 1 encounter to the ED location and 1 encounter to the 24hr
Observation Unit since there was time spent in an inpatient location (medical
ward) in between the outpatient stays.
e. If the patient’s stay in the facility crosses calendar months, the patient will contribute an
encounter to the first month the patient was in an outpatient location. For example:
i. If patient is in outpatient location on January 31 and February 1 then count as 1
encounter to January and zero to February.
f. Please note, the encounters count will not be a direct match to the AU Option days
present count for these location types.
Minimizing Bias & Bypassing Suppression
The hospital LIS is the ultimate source of antimicrobial susceptibility test results, but in some healthcare
facilities not all susceptibility results are readily available in the LIS for reporting to NHSN. Concerted
efforts are needed to obtain antimicrobial susceptibility data for the purposes of reporting to NHSN. Due
to a practice referred to as selective reporting or cascade reporting, some antimicrobial susceptibility
results might be withheld from clinical end users. This practice can serve to control costs or to prevent
overuse of some antimicrobial agents, but it also can exert an adverse impact on the completeness of
antimicrobial susceptibility results reporting to public health surveillance systems and infection control
programs.
4
This can lead to significant biases in the calculation of cumulative antibiograms available for
surveillance or infection control. Facilities should make every effort to submit all antimicrobial

January 2024 Antimicrobial Use and Resistance Module
AUR
14-47
susceptibility data that meet the NHSN protocol requirements, regardless of whether those data are
suppressed from clinical end users.
Data Analyses
Facilities and groups can analyze all AR Option data reported to NHSN immediately after data upload.
After generating analysis datasets within NHSN, users can view all reported data in the NHSN analysis
reports. The data in NHSN can be visualized and analyzed in many ways. For example, descriptive
analysis reports such as line lists and bar charts are available. In addition, measures of antimicrobial
resistance are available in rate tables, antibiogram, Standardized Resistant Infection Ratio (SRIR) and
Pathogen-specific Standardized Infection Ratio (pSIR) reports.
Types of AR Option Analysis Reports
Standardized Resistant Infection Ratio (SRIR):
The Standardized Resistant Infection Ratio (SRIR) is a metric developed by CDC to enable facilities to
compare their rates of hospital-onset (HO) drug-resistant infection events to a national benchmark. The
SRIR adjusts for various facility level factors that contribute to AR risk within each facility. It compares
the actual number of resistant infections to the number predicted, given the standard population
(specifically, the 2019 NHSN baseline), adjusting for several risk factors that have been found to be
statistically significantly associated with rates of resistant infections. The SRIR is calculated by dividing
the number of observed resistant infections by the number of predicted resistant infections.
SRIR =
# Observed Resistant Infections
# Predicted Resistant Infections
The observed resistant infections are the number of HO AR Events that meet NHSN-specific resistance
definitions (for example, CRE, MRSA, multi-drug resistant Pseudomonas aeruginosa). The predicted
resistant infections are calculated using predictive models developed by CDC and applied to nationally
aggregated 2019 AR data reported to NHSN. Separate predictive models are developed for each specific
resistant organism definition and specimen source (blood, urine, and lower respiratory).
The SRIR can be generated for 7 drug-resistant phenotypes from 3 specimen sources (blood, urine, and
lower respiratory), for a total of 21 possible SRIRs (see Appendix J
). The resistant organisms eligible for
SRIR calculation were determined by CDC with input from external experts, including adult, pediatric,
and neonatal infectious disease physicians and pharmacists. The drug-resistant phenotypes are listed
below (see
Appendix I for definitions).
• Carbapenem-resistant Enterobacterales
• Extended-spectrum cephalosporin-resistant Enterobacterales
• Fluoroquinolone-resistant Enterobacterales
• Vancomycin-resistant Enterococcus
• Fluoroquinolone-resistant Pseudomonas aeruginosa
• Multi-drug-resistant Pseudomonas aeruginosa
January 2024 Antimicrobial Use and Resistance Module
AUR
14-48
• Methicillin-resistant Staphylococcus aureus
At present, SRIRs are available to facilities that have submitted at least one hospital-onset isolate of the
specific organism in the given specimen source during the time period of interest. For example, a
Vancomycin-resistant Enterococcus blood SRIR can be generated for the facilities that submitted at least
one HO Enterococcus blood event in the given time period.
A SRIR greater than 1.0 indicates that more resistant infections were observed than predicted. A SRIR
less than 1.0 indicates that fewer resistant infections were observed than predicted. An SRIR of 0
indicates a facility reported the organism of interest from the specimen source of interest during the
correct time period, but the organism was not resistant to the drug(s) specified. For example, using the
example of HO VRE in urine, if a hospital reports 10 hospital-onset Enterococcus isolates from urine
during the time of interest, and all 10 are reported to be susceptible to vancomycin, the HO VRE SRIR
would be 0 because there were 0 observed resistant infection events.
A SRIR value may be missing when
no HO isolates of the organism of interest were reported from the given
specimen source during the time period, or an HO organism of interest was reported for the specimen source
but <0.3 events were predicted (minimum precision criterion was not met)
. Using the example of HO VRE in
urine, a facility would receive a missing value for a SRIR if:
1) No HO Enterococcus was reported in a urine specimen or,
2) HO Enterococcus was reported from urine during the correct time period but there were
<0.3 HO VRE events predicted for the time period of interest.
SRIRs can be produced by quarter, half-year, year, or cumulative time periods.
SRIR Report:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-Option-SRIR-
Report_QRG_FINAL.pdf
Pathogen-specific Standardized Infection Ratio (pSIR):
The Pathogen-Specific Standardized Infection Ratio (pSIR) is a metric developed by CDC to enable
facilities to compare their rates of HO culture-positive infections of specific pathogen to a national
benchmark. It compares the actual number of events (pathogens isolated) to the number predicted,
given the standard population (specifically, the 2019 NHSN baseline), adjusting for several risk factors
that have been found to be statistically significantly associated with differences in infection incidence.
The pSIR is calculated by dividing observed infections of specific pathogens by predicted infections.
pSIR =
# Observed Infections of Specific Pathogens
# Predicted Infections of Specific Pathogens
The observed infections are the number of HO events reported to NHSN. The predicted infections are
calculated using predictive models developed by CDC and applied to nationally aggregated 2019 AR data
reported to NHSN. Separate predictive models are developed for each pathogen and specimen source
(blood, urine, and lower respiratory).

January 2024 Antimicrobial Use and Resistance Module
AUR
14-49
The pSIR can be generated for 4 pathogens/pathogen groups from 3 specimen sources (blood, urine,
and lower respiratory), for a total of 12 possible pSIRs (see Appendix J
).
• Enterobacterales: includes Escherichia coli, Klebsiella aerogenes, Klebsiella oxytoca, Klebsiella
pneumoniae, or Enterobacter spp.
• Enterococcus: includes all Enterococcus spp.
• Staphylococcus aureus
• Pseudomonas aeruginosa
At present, pSIRs are available to facilities that have submitted at least one HO pathogen in the correct
specimen source during the specified time period of interest.
A pSIR greater than 1.0 indicates that more infections were observed than predicted. A pSIR less than
1.0 indicates that fewer infections were observed than predicted. A pSIR value of 0 indicates a facility
reported at least one HO isolate from the specimen source of interest during the correct time period,
but the pathogen of interest was not isolated. For example, for hospital-onset Enterococcus in urine, if a
facility reported one or more HO isolates (any organism) from urine during the time period of interest,
but no HO Enterococcus was isolated, the facility would receive a pSIR of 0.
A pSIR value may be missing when no positive culture grew reportable AR organisms from the given
specimen source during the time period, or an HO organism of interest was reported for the specimen
source but <0.3 events were predicted (minimum precision criterion was not met). Using the example of
HO Enterococcus in urine, a facility would receive a missing value for a pSIR if:
1) No HO positive culture from a urine specimen grew Enterobacterales, Enterococcus,
Staphylococcus aureus, or Pseudomonas aeruginosa
2) At least one HO pathogen of interest was isolated from urine during the correct time period
but there were <0.3 HO Enterococcus events predicted for that time period
pSIRs can be produced by quarter, half-year, year, or cumulative time periods.
pSIR Report:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-Option-pSIR-
Report_QRG_FINAL.pdf
Facility-wide Antibiogram:
The facility-wide antibiogram table displays the calculated percent susceptible (see Table 2
) for each
organism-antimicrobial combination. Users can stratify the antibiogram table by specimen source, time
period, and/or by specific antimicrobial or organism. By default, the facility-wide antibiogram will
include isolates collected in eligible outpatient locations (ED, pediatric ED and 24hr observation area) if
the facility reports those to NHSN. Note: A facility must have tested and reported the antimicrobial
susceptibility results for at least 30 isolates for a specific organism/antimicrobial combination in the
given time period for results to appear in the Percent Susceptible table of NHSN antibiogram report.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-50
In addition to the facility-wide antibiogram, within the same report, NHSN creates a table displaying the
calculated percent tested (see Appendix F
) for each organism-antimicrobial combination reported from
all locations (inpatient and outpatient) to the AR Option.
Antibiogram and Percent Tested:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/ar-qrg-
antibiogram-508.pdf
Table 2. Facility-wide Antibiogram
Facility-wide: standard report for facility and group user
% susceptible is calculated for each organism-antimicrobial pairing:
%S =
Total # of isolates S
Total # of isolates tested
Antimicrobial Resistance Option (AR) Events
Five reports list all events reported into the NHSN AR Option regardless of susceptibility results.
Line List: Users can generate a line list to show all AR Events reported into NHSN for a given time
period. The line list is the most customizable type of AR Option analysis report. The line list is
also the most helpful AR Option report for data validation.
Line List: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-QRG-LineList.pdf
Bar Chart: Users can generate a bar chart to show all AR Events reported into NHSN for a given
time period. By default, the bar chart will show the number of AR Events by organism over the
most recent 12-month time period. Users can modify the bar chart to show the number of
Antimicrobial Resistant Organisms based on the AR Option phenotype definitions (Appendix I
).
Bar Chart: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/ar-qrg-barchart-508.pdf
Incidence Rate Table: Users can generate an incidence rate table that includes hospital-onset
(HO) events by individual specimen type and a combined all specimen type rate for select
pathogen groups.
HO incidence:
# HO AR Events
# patient days
× 10,000
Incidence Rate Table:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-Incidence-
by-Pathogen.pdf
Prevalence Rate Table: Users can generate two prevalence rate tables that include community-
onset (CO) events by individual specimen type and a combined all specimen type rate for select
pathogen groups.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-51
CO prevalence:
# CO AR Events from inpt and outpt locations
# admissions
× 10,000
O
utpatient CO prevalence:
# CO AR Events from outpt locations
# encounters
× 10,000
Prevalence Rate Tables:
Inpatient and outpatient:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-CO-
Prevalence-by-Pathogen.pdf
Outpatient only: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-Outpatient-
Prevalence-by-Pathogen.pdf
Antimicrobial Resistant Option (AR) Drug-resistant Organisms (AR Organisms)
Six reports use the AR Option phenotype definitions (Appendix I
) to determine Antimicrobial Resistant
Organisms. Specifically, only events with susceptibility results meeting the phenotype definitions will be
included in these reports.
Line List: Users can generate a line list to show all AR Organisms that meet the AR Option
phenotype definitions for a given time period. The default line list shows each AR Organism
reported to NHSN, patient information, specimen collection date, and the location where the
specimen was collected.
AR Organisms Line List:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/ar-qrg-
organisms-linelist-508.pdf
Frequency Table: Users can generate a frequency table to show the number of AR Events
meeting the AR Option phenotype definitions in a given time period. While the table default is
to display events by month, modifications can be made to display the data by quarter, half-year,
year, or cumulative time periods.
AR Organisms Frequency Table:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/ar-
qrg-freq-508.pdf
Rate Table: Users can generate a rate table to display the percent of resistant isolates by AR
Option phenotype. The percent resistant is calculated by dividing the number of resistant
isolates over the number of isolates tested multiplied by 100.
#
#
× 100
AR Organisms Rate Table:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/ar-qrg-
ratetable-508.pdf

January 2024 Antimicrobial Use and Resistance Module
AUR
14-52
Incidence Rate Table: Users can generate an incidence rate table that includes hospital-onset
(HO) events that meet AR Option phenotype definitions by individual specimen type and a
combined all specimen type rate.
HO incidence:
#
#
× 10,000
Incidence Rate Table:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-Incidence-
by-Phenotype.pdf
Prevalence Rate Table: Users can generate two prevalence rate tables that include community-
onset (CO) events that meet AR Option phenotype definitions by individual specimen type and a
combined all specimen type rate.
CO prevalence:
#
#
× 10,000
Outpatient CO prevalence:
#
#
× 10,000
Prevalence Rate Tables:
Inpatient and outpatient:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-CO-
Prevalence-by-Phenotype.pdf
Outpatient only: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/AR-Outpatient-
Prevalence-by-Phenotype.pdf
Users can also export AR Option data from NHSN in various formats including Excel, CSV, and SAS.
Additional analysis reports will be available in future releases. Requests for additional reports can be
sent to: NHS[email protected]
.
NHSN Group Analysis:
NHSN Group users can visualize and analyze AR data shared with them by member facilities using NHSN
analysis reports. In addition to the Analysis Quick Reference Guides (QRGs) available in the Antimicrobial
Use and Resistance Module Reports section of the Patient Safety Analysis Quick Reference Guide
page.
Groups can find Group-specific resources on the NHSN Group Users page.
Additional Analysis Resources:
Users can also find recorded training sessions and Quick Learn videos highlighting AR Option analysis
reports on the AUR Training
page.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-53
Figure 1. Test Result Algorithm for Invasive Specimen Reporting
Figure 2. Test Result Algorithm for Non-Invasive Specimen Reporting

January 2024 Antimicrobial Use and Resistance Module
AUR
14-54
Figure 3. Reporting Algorithm for Same Day Duplicates

January 2024 Antimicrobial Use and Resistance Module
AUR
14-55

January 2024 Antimicrobial Use and Resistance Module
AUR
14-56
References
1. Schwaber MJ, De-Medina T, and Carmeli Y. Epidemiological interpretation on antibiotic
resistance studies – what are we missing? Nat Rev Microbiol 2004;2:979-83.
2. National Healthcare Safety Network (NHSN) Patient Safety Component: Clinical Document
Architecture. http://www.cdc.gov/nhsn/cdaportal/index.html
3. CLSI. Analysis and Presentation of Cumulative Antimicrobial Susceptibility Test Data; Approved
Guideline – Third Edition. CLSI document M39-A3. Wayne, PA: Clinical and Laboratory
Standards; 2009.
4. Council of State and Territorial Epidemiologists (CSTE). Recommendations for strengthening
public health surveillance of antimicrobial resistance in the United States.
https://cdn.ymaws.com/www.cste.org/resource/resmgr/PS/13-SI-01.pdf
. Accessed October 1,
2015.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-57
Appendix F. List of Eligible Organisms for the NHSN AR Option
Please note that standardized terminology (SNOMED) mappings are provided in the Antimicrobial
Resistance Toolkit. Facilities and vendors should refer to the AR Option Pathogen Roll-up Workbook
found in the Antimicrobial Resistance Toolkit for the eligible organisms for AR Option reporting and the
complete list of their associated SNOMED codes. Testing methods should follow most recent CLSI
guidance as appropriate.
Organism
Specimen Type
Antimicrobial Agents
Acinetobacter
(All Acinetobacter species
noted in the AR Option
Pathogen Roll-up
Workbook)
Blood, Urine, Lower
Respiratory, CSF
Amikacin
Ampicillin-sulbactam
Cefepime
Cefiderocol
Cefotaxime
Ceftazidime
Ceftriaxone
Ciprofloxacin
Colistin
Doripenem
Doxycycline
Gentamicin
Imipenem
Levofloxacin
Meropenem
Minocycline
Piperacillin-tazobactam
Polymyxin B
Tobramycin
Trimethoprim-sulfamethoxazole
Additional Agents for Urine
Tetracycline
Candida albicans
Candida auris
Candida glabrata
Candida parapsilosis
Candida tropicalis
Blood, Urine, CSF
Note: Lower respiratory will
not be collected for Candida
spp.
Anidulafungin
Caspofungin
Fluconazole
Micafungin
Posaconazole
Voriconazole
Additional Agents for Urine
None
Continued on the next page

January 2024 Antimicrobial Use and Resistance Module
AUR
14-58
Organism
Specimen Type
Antimicrobial Agents
Citrobacter amalonaticus
Citrobacter braakii
Citrobacter freundii
Citrobacter freundii complex
Citrobacter koseri
Citrobacter youngae
Enterobacter
(All Enterobacter species
noted in the AR Option
Pathogen Roll-up
Workbook)
Escherichia coli
Klebsiella aerogenes
Klebsiella oxytoca
Klebsiella pneumoniae
Morganella morganii
Proteus mirabilis
Proteus penneri
Proteus vulgaris
Serratia marcescens
Blood, Urine, Lower
Respiratory, CSF
Amikacin
Amoxicillin-clavulanic acid
Ampicillin
Ampicillin-sulbactam
Aztreonam
Cefazolin (urine or non-urine
breakpoints)
a
Cefepime
Cefiderocol
Cefotaxime
Cefotetan
Cefoxitin
Ceftaroline
Ceftazidime
Ceftazidime-avibactam
Ceftolozane-tazobactam
Ceftriaxone
Cefuroxime
Chloramphenicol
Ciprofloxacin
Colistin
Doripenem
Doxycycline
Ertapenem
Gentamicin
Imipenem
Imipenem-relebactam with Cilastatin
Levofloxacin
Meropenem
Meropenem-vaborbactam
Minocycline
Piperacillin-tazobactam
Polymyxin B
Tetracycline
Trimethoprim-sulfamethoxazole
Tobramycin
Additional Agents for Urine
Fosfomycin
Nitrofurantoin
Sulfisoxazole
Trimethoprim
Continued on the next page

January 2024 Antimicrobial Use and Resistance Module
AUR
14-59
Organism
Specimen Type
Antimicrobial Agents
Enterococcus
(All Enterococcus species
noted in the AR Option
Pathogen Roll-up
Workbook)
Enterococcus faecalis
Enterococcus faecium
Blood, Urine, Lower
Respiratory, CSF
Ampicillin
Dalbavancin
Daptomycin
Gentamicin
Gentamicin high potency
Linezolid
Oritavancin
Penicillin
b
Quinupristin-dalfopristin
Streptomycin
Streptomycin high potency
Tedizolid
Telavancin
Vancomycin
Note: For Gentamicin and Streptomycin
only:
Synergistic = Susceptible
Non-synergistic = Resistant
Additional Agents for Urine
Note: Exclude Gentamicin and
Streptomycin
Ciprofloxacin
Fosfomycin
Levofloxacin
Nitrofurantoin
Tetracycline

January 2024 Antimicrobial Use and Resistance Module
AUR
14-60
Organism
Specimen Type
Antimicrobial Agents
Pseudomonas aeruginosa
Blood, Urine, Lower
Respiratory, CSF
Amikacin
Aztreonam
Cefepime
Cefiderocol
Ceftazidime
Ceftazidime-avibactam
Ceftolozane-tazobactam
Ciprofloxacin
Colistin
Doripenem
Gentamicin
Imipenem
Imipenem-relebactam with Cilastatin
Levofloxacin
Meropenem
Piperacillin-tazobactam
Polymyxin B
Tobramycin
Additional Agents for Urine
None
Continued on the next page

January 2024 Antimicrobial Use and Resistance Module
AUR
14-61
Organism
Specimen Type
Antimicrobial Agents
Staphylococcus aureus
Blood, Urine, Lower
Respiratory, CSF
Azithromycin
Cefoxitin
Ceftaroline
Chloramphenicol
Ciprofloxacin
Clarithromycin
Clindamycin
Dalbavancin
Daptomycin
Doxycycline
Erythromycin
Gentamicin
Lefamulin
Levofloxacin
Linezolid
Minocycline
Moxifloxacin
Oritavancin
Oxacillin or Nafcillin
c
Penicillin
b
Rifampin
Tedizolid
Telavancin
Tetracycline
Trimethoprim-sulfamethoxazole
Vancomycin
Additional Agents for Urine
Nitrofurantoin
Sulfisoxazole
Trimethoprim
Stenotrophomonas
maltophilia
Blood, Urine, Lower
Respiratory, CSF
Cefiderocol
Ceftazidime
Chloramphenicol
Levofloxacin
Minocycline
Trimethoprim-sulfamethoxazole
Additional Agents for Urine
None
Continued on the next page

January 2024 Antimicrobial Use and Resistance Module
AUR
14-62
Organism
Specimen Type
Antimicrobial Agents
Streptococcus agalactiae
Blood, Urine, Lower
Respiratory, CSF
Ampicillin
Azithromycin
Cefepime
Cefotaxime
Ceftaroline
Ceftriaxone
Chloramphenicol
Clarithromycin
Clindamycin
Dalbavancin
Daptomycin
Erythromycin
Levofloxacin
Linezolid
Oritavancin
Penicillin
b
Tedizolid
Telavancin
Vancomycin
Additional Agents for Urine
None
Continued on the next page

January 2024 Antimicrobial Use and Resistance Module
AUR
14-63
Organism
Specimen Type
Antimicrobial Agents
Streptococcus pneumoniae
Blood, Urine, Lower
Respiratory, CSF
Amoxicillin
Amoxicillin-clavulanic acid
Azithromycin
Cefepime (meningitis or non-meningitis
breakpoints)
d
Cefotaxime (meningitis or non-
meningitis breakpoint)
d
Ceftaroline
Ceftriaxone (meningitis or non-
meningitis breakpoint)
d
Cefuroxime (parenteral breakpoint)
Chloramphenicol
Clarithromycin
Clindamycin
Doxycycline
Ertapenem
Erythromycin
Gemifloxacin
Imipenem
Lefamulin
Levofloxacin
Linezolid
Meropenem
Moxifloxacin
Penicillin
b
(meningitis or non-meningitis
breakpoint)
d
Penicillin V
b
(oral breakpoint)
Rifampin
Tetracycline
Trimethoprim-sulfamethoxazole
Vancomycin
Additional Agents for Urine
None
a
If the LIS produces urine and non-urine breakpoint results, rely on the specimen source to determine
which susceptibility results to report. If the specimen source is urine, report the urine breakpoint
susceptibility. If the specimen source is blood, CSF, or lower respiratory, report the non-urine breakpoint
susceptibility.
b
If the LIS does not differentiate between Penicillin G and Penicillin V, list susceptibility results under
Penicillin G and indicate that Penicillin V was not tested (NA).
c
For Staphylococcus aureus susceptibility testing, if the LIS tests Nafcillin instead of Oxacillin, report
Nafcillin susceptibility results as Oxacillin.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-64
d
If the LIS produces meningitis and non-meningitis breakpoint results, rely on the specimen source to
determine which susceptibility results to report. If the specimen source is CSF, report the meningitis
breakpoint susceptibility. If the specimen source is blood, urine, or lower respiratory, report the non-
meningitis breakpoint susceptibility.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-65
Appendix G. Technical and Isolate Based Report Variables
Facility, Patient, and Specimen sections
Name Description of Field
Code Value
List
Level of
Requirement
in CDA file
Facility OID
a
Must be assigned to facility and included in the
importation file prior to submission to NHSN
Required
Vendor
(Application)
OID
b
Must be assigned to a vendor’s software application
and included in the AR CDA data file prior to
submission to NHSN. The Vendor (Application) OID
should be obtained by the software vendor and is
distinct from the Facility OID.
Required
SDS Validation
ID
b
The Synthetic Data Set (SDS) Validation ID will be
provided to the AR CDA vendor by the AUR Module
Team upon confirmation that the AR SDS Excel files
pass validation as part of the AR SDS initiative.
c
Required
Vendor
Software Name
Vendor software name is the name of the software
application that generates the AR CDA file. NHSN
collects this information to more effectively
troubleshoot CDA files when needed.
Optional
Software
Version
Software version is the version of the software
application that generates the AR CDA file. NHSN
collects this information to more effectively
troubleshoot CDA files when needed.
Optional
Vendor Name
Vendor name is the name of the vendor that owns
the software application that generates the AR CDA
file. NHSN collects this information to more
effectively troubleshoot CDA files when needed.
Optional
Patient ID
Alphanumeric patient ID assigned by the hospital and
may consist of any combination of numbers and/or
letters. This ID remains the same for the patient
across all visits and admissions for all NHSN
reporting.
Required
Date of Birth
The date of the patient’s birth including month, day,
and year.
Required
Gender
The gender of the patient.
M (Male),
F (Female),
O (Other)
Required
Race
The patient’s race
American
Indian/
Optional

January 2024 Antimicrobial Use and Resistance Module
AUR
14-66
Name Description of Field
Code Value
List
Level of
Requirement
in CDA file
Alaska
Native,
Asian,
Black or
African
American,
Native
Hawaiian/
Other
Pacific
Islander,
White
Ethnicity
The patient’s ethnicity.
Hispanic or
Latino, or
Not
Hispanic or
Not Latino.
Optional
Admission
status
Whether the patient was admitted to the facility
during the encounter.
Notes:
• Report True (Yes) if the specimen was
collected in an inpatient location.
• Report True (Yes) if the specimen was
collected in an outpatient location (for
example, ED) and the patient was transferred
to an inpatient location.
• Report True (Yes) if the specimen was
collected in an outpatient location and the
facility discharges from the ED or 24hr
observation area, then admits to inpatient
(instead of transferring), when less than 24
hours between ED or 24hr observation area
discharge and inpatient admit (at the same
hospital).
• Report False (No) if the specimen was
collected in an outpatient location and the
patient was discharged and did not return
within 24 hours.
True/False
Required

January 2024 Antimicrobial Use and Resistance Module
AUR
14-67
Name Description of Field
Code Value
List
Level of
Requirement
in CDA file
Date admitted
to facility
The date admitted to the facility is the calendar date
that the patient physically locates to an inpatient
location.
Notes:
• If the specimen was collected in an inpatient
location, use the date of admission for this
field
• If the specimen was collected in an
outpatient location, use the admission status
variable as a guide:
o If the admission status variable is True
(Yes), then use the date the patient was
admitted to the inpatient location for this
field
o If the admission status variable is False
(No), then use the encounter date (the
date the patient arrived in the first
outpatient location) for this field
If the specimen was collected on day
2 in an outpatient location, report
the date of the first day in the
outpatient location
If patient is transferred to a
subsequent outpatient location and
specimen is collected in the second
outpatient location, report the date
the patient entered the first
outpatient location
Required
Specimen
collection date
Date the specimen was collected including month,
day, and year.
Required
Specimen
source
Specimen source from which the isolate was
recovered (urine, lower respiratory, blood, CSF).
SNOMED
Required
Location
Patient care area where patient was located when
the laboratory specimen was collected. Use patient
location obtained from administrative data system
(ADT).
CDC
Location
Codes
Required

January 2024 Antimicrobial Use and Resistance Module
AUR
14-68
Organism and Antimicrobial Susceptibility Testing Results sections
Name
Description of Field
Code Value
List
Data
element
required for
CDA file?
“NA” allowed?
Isolate
identifier
Isolate identifier unique for each isolate
within laboratory based upon the
isolate being reported with its own AST
results.
For example, a urine specimen yields
an E. coli isolate and a K.
pneumoniae isolate and both have AST
performed and reported; each isolate
should be reported with a unique
isolate identifier.
Y
N
Organism
Organism identified from specimen
(Appendix F).
SNOMED
Y
N
Antimicrobial
Antimicrobial(s) tested for
susceptibility (Appendix F defines
agents by organism and specimen
source)
LOINC
Y
N
PBP2a-
agglutination
Result for PBP2a-agglutination (only if
SA)
Positive,
Negative,
or
Unknown
Y
(Required
only for
Staph
aureus)
N
PCR mec-gene
Result for PCR mec-gene (only if SA)
Positive,
Negative,
or
Unknown
Y
(Required
only for
Staph
aureus)
N
E-test sign
d
E-test sign
Note: Instead of “NA”, use “=” to
express an exact value.
Y
Y (Recommend
reporting sign
if test value is
reported)
E-test
value/units of
measure
E-test (Value in micrograms/liter). Use
'.' as decimal delimiter, for example,
0.25
Y
Y
(Recommend
reporting value
if test sign is
reported)
Interpretation
of E-test
Interpretation result of the E-test
susceptibility test performed
Y
Y

January 2024 Antimicrobial Use and Resistance Module
AUR
14-69
MIC sign
d
MIC sign
Note: Instead of “NA”, use “=” to
express an exact value.
Y
Y
(Recommend
reporting sign
if test value is
reported)
MIC
value/units of
measure
MIC (Value in micrograms/liter). Use '.'
as decimal delimiter, for example, 0.25
Y
Y
(Recommend
reporting value
if test sign is
reported)
Interpretation
of MIC test
Interpretation result of the MIC
susceptibility test performed
Y
Y
Disk diffusion
(KB) sign
d
Disk diffusion (KB) sign
Note: Instead of “NA”, use “=” to
express an exact value.
Y
Y
(Recommend
reporting sign
if test value is
reported)
Disk diffusion
(KB)
value/units of
measure
Disk diffusion (KB) value in millimeters
Y
Y
(Recommend
reporting value
if test sign is
reported)
Interpretation
of Disk
diffusion (KB)
test
Interpretation result of the disk
diffusion (KB) susceptibility test
performed
Y
Y
Final
Interpretation
result
Final interpretation result of all
different susceptibility tests performed
Y
Y
a
Facilities interested in submitting data to NHSN via CDA must obtain a Facility OID (object identifier).
More information on how to obtain an OID for your facility can be found on the
CDA Submission Support
Portal.
b
AR CDA files are required to include a Vendor (Application) OID (object identifier) as part of the AR
Option Synthetic Data Set initiative. More information on how to obtain a Vendor (Application) OID can
be found on the Vendor (Application) Object Identifier
page.
c
More detailed information about the AR Synthetic Data Set validation process can be found on the CDA
Submission Support Portal's Innovation Tools page.
d
Refer to the HL7 Implementation Guide for specifics on how to code these values in the CDA report.
Note: While many of these specific test results (specifically, E-test, MIC, Disk diffusion [KB]) are required
in the CDA report, facilities unable to electronically obtain these results may still participate by using
‘NA’ to signify ‘Not Tested’. Facilities should not employ manual means of data collection.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-70
Appendix H. Denominator Data Variables
Name Description of Field
Level of
Requirement
Facility OID
a
Must be assigned to facility and included in the importation file prior
to submission to NHSN.
Required
Vendor
(Application)
OID
b
Must be assigned to a vendor’s software application and included in
the AR CDA data file prior to submission to NHSN. The Vendor
(Application) OID should be obtained by the software vendor and is
distinct from the Facility OID.
Required
SDS
Validation
ID
b
The Synthetic Data Set (SDS) Validation ID will be provided to the AR
CDA vendor by the AUR Module Team upon confirmation that the AR
SDS Excel files pass validation as part of the AR SDS initiative.
c
Required
Vendor
Software
Name
Vendor software name is the name of the software application that
generates the AR CDA file. NHSN collects this information to more
effectively troubleshoot CDA files when needed.
Optional
Software
Version
Software version is the version of the software application that
generates the AR CDA file. NHSN collects this information to more
effectively troubleshoot CDA files when needed.
Optional
Vendor
Name
Vendor name is the name of the vendor that owns the software
application that generates the AR CDA file. NHSN collects this
information to more effectively troubleshoot CDA files when needed.
Optional
Location
FacWideIN, ED, Pediatric ED, 24-hour Observation Area
Required
Month
2-Digit month
Required
Year
4-Digit year
Required
Patient Days
For facility wide inpatient locations enter the total number of patient
days collected at the same time each day combined for the month.
All the facility’s inpatient acute care locations should be included
where denominators can be accurately collected.
Required for
FacWideIN
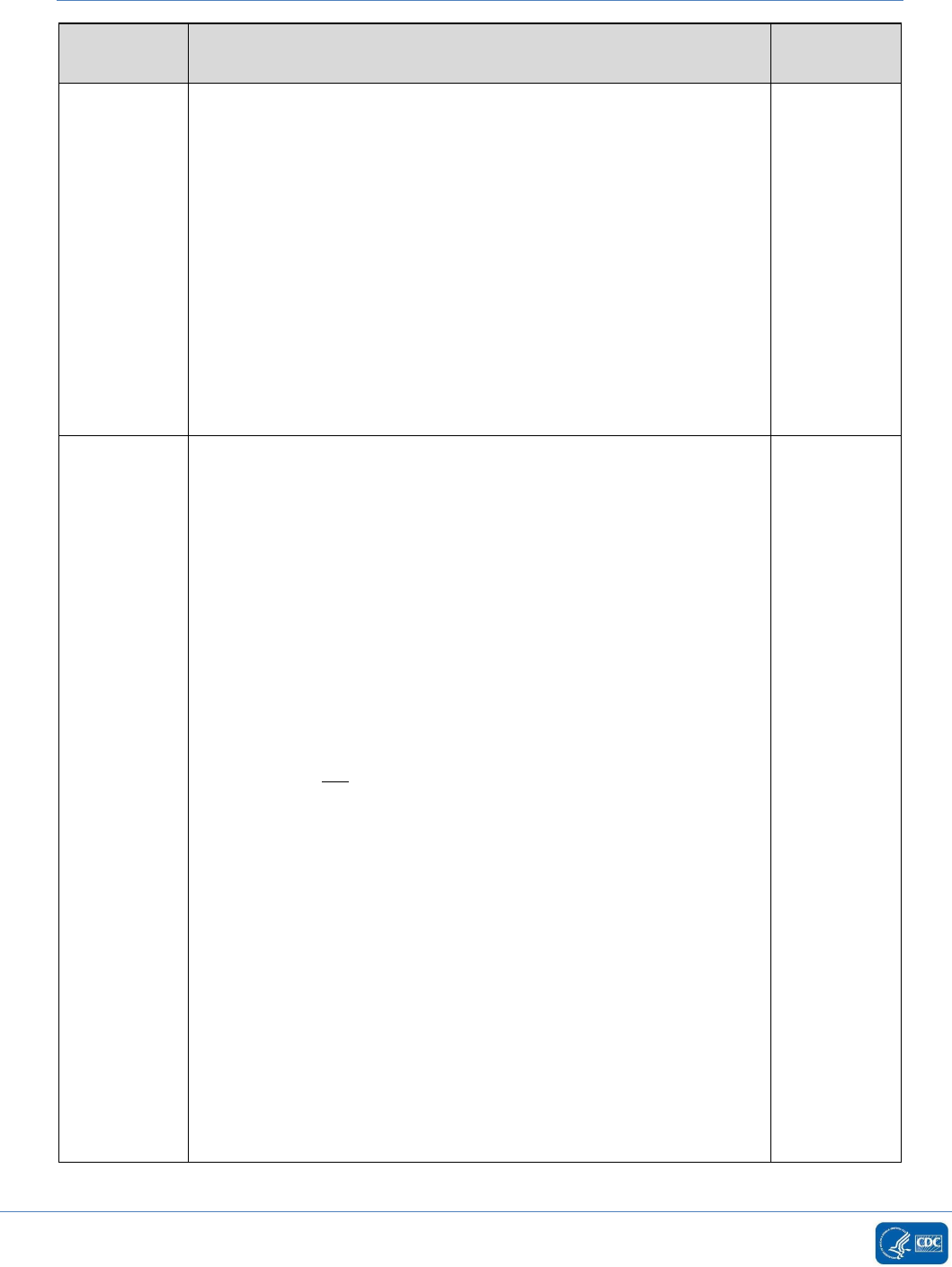
January 2024 Antimicrobial Use and Resistance Module
AUR
14-71
Name
Description of Field
Level of
Requirement
Admission
Count
Enter the total number of admissions for all facility inpatient
locations combined for the month.
• A patient is counted as an admission when they arrive in an
NHSN designated inpatient location regardless of patient
status (for example, inpatient, observation).
• A patient admitted to an inpatient unit would be counted as
an admission even if they were discharged that same
calendar day.
• A patient transfer from an inpatient to an outpatient location
then back to an inpatient location is counted as two separate
admissions.
• Please note, the admissions definition used in the AUR
Module is different than the definition used in the NHSN
MDRO/CDI Module.
Required for
FacWideIN
Encounters
for
outpatient
locations
Enter the total number of patient visits to the given outpatient
location (specifically: ED, Pediatric ED, 24-hour Observation Area). A
visit to an eligible outpatient location counts as a single encounter.
• If the patient’s stay in any eligible outpatient location
continues into subsequent calendar days, that patient should
still be counted as 1 encounter. For example:
o If the patient arrives in the ED on Monday and remains in
the ED until Wednesday, that patient should be counted
as 1 encounter within the ED.
• If the patient transfers from one outpatient location to
another within the same facility, that patient should be
counted as 1 encounter for the first outpatient location and
should not be counted as an encounter for the receiving
location (specifically, a patient should not contribute two
encounters when transferring between outpatient locations
in the same facility). For example:
o If the patient arrives in the ED on Monday, then is
transferred to the 24hr Observation Area on Tuesday, the
patient should be counted only as 1 encounter within the
ED and zero encounters within the 24hr Observation
Area.
• If the patient is discharged, or leaves, then returns to that
outpatient unit, that patient should be counted as 2
encounters, even when the movements were during the
same calendar day. For example:
o If the patient arrives in the ED at 07:00 on Monday, is
discharged at 11:00 on Monday then returns to the ED at
Required for
ED, Pediatric
ED, and 24-
hour
Observation
Area

January 2024 Antimicrobial Use and Resistance Module
AUR
14-72
Name
Description of Field
Level of
Requirement
18:00 on Monday, that patient counts as two separate
encounters for the ED.
• If the patient transfers from outpatient to inpatient, then to
outpatient, the second outpatient stay (assuming it’s in an
eligible location) would be considered a new encounter
because there was time spent in an inpatient location. For
example:
o If the patient arrives in the ED on Monday, is admitted or
transferred to the medical ICU on Monday then is
transferred to the 24hr Observation Unit on Tuesday and
admitted or transferred back to the medical ward on
Tuesday, the patient would contribute 2 encounters (the
first in the ED and the second to the 24hr Observation
Unit) since there was time spent in an inpatient location
(medical ward) in between the outpatient stays.
• If the patient’s stay in the facility crosses calendar months,
the patient will contribute an encounter to the first month
the patient was in an outpatient location. For example:
o If patient is in outpatient location on January 31 and
February 1 then count as 1 encounter to January and zero
to February.
• Please note, the encounters count will not be a direct match
to the AU Option days present count for these location types.
a
Facilities interested in submitting data to NHSN via CDA must obtain a Facility OID (object identifier).
More information on how to obtain an OID for your facility can be found on the
CDA Submission Support
Portal.
b
AR CDA files are required to include a Vendor (Application) OID (object identifier) as part of the AR
Option Synthetic Data Set initiative. More information on how to obtain a Vendor (Application) OID can
be found on the Vendor (Application) Object Identifier
page.
c
More detailed information about the AR Synthetic Data Set validation process can be found on the CDA
Submission Support Portal's Innovation Tools page.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-73
Appendix I. NHSN AR Option Phenotype Definitions
Note: The phenotypes defined here for the AR Option only may not match phenotype definitions used in other NHSN Modules. Additionally, the drug
classes listed below are specific to laboratory testing and, in some cases, do not match to the specific class defined in the AU Option. The drugs
included in each phenotype definition are specific to those included in the reportable drug panel for that organism. Please refer to Appendix F of the
AUR Module Protocol for the complete list of drug panels for each organism.
Phenotype Name
Phenotype Code
Phenotype Definition
a
Methicillin-resistant Staphylococcus
aureus
b
MRSA_AR
Staphylococcus aureus that has tested Resistant (R) to at least one of the following:
oxacillin or cefoxitin
Carbapenem-resistant
Enterobacterales (expanded)
CREexpanded_AR
Any Citrobacter amalonaticus, Citrobacter braakii, Citrobacter freundii, Citrobacter
freundii complex, Citrobacter koseri, Citrobacter youngae, Enterobacter spp., E. coli,
Klebsiella aerogenes, Klebsiella oxytoca, Klebsiella pneumoniae, and Serratia
marcescens that has tested Resistant (R) to at least one of the following: imipenem,
meropenem, doripenem, ertapenem, meropenem/vaborbactam, or
imipenem/relebactam
OR
Any Proteus mirabilis, Proteus penneri, Proteus vulgaris, and Morganella morganii
that has tested Resistant (R) to at least one of the following: meropenem, doripenem,
ertapenem, or meropenem/vaborbactam
Carbapenem-resistant
Enterobacterales
b
(E. coli, Klebsiella,
or Enterobacter)
CREall_AR
Any Escherichia coli, Klebsiella aerogenes, Klebsiella oxytoca, Klebsiella pneumoniae,
or Enterobacter spp. that has tested Resistant (R) to at least one of the following:
imipenem, meropenem, doripenem, ertapenem, meropenem/vaborbactam, or
imipenem/relebactam
Carbapenem-resistant E. coli
CREecoli_AR
Any Escherichia coli that has tested Resistant (R) to at least one of the following:
imipenem, meropenem, doripenem, ertapenem, meropenem/vaborbactam, or
imipenem/relebactam

January 2024 Antimicrobial Use and Resistance Module
AUR
14-74
Phenotype Name
Phenotype Code
Phenotype Definition
a
Carbapenem-resistant Enterobacter
spp. and Klebsiella aerogenes
CREenterobacter_AR
Any Enterobacter spp. or Klebsiella aerogenes that has tested Resistant (R) to at least
one of the following: imipenem, meropenem, doripenem, ertapenem,
meropenem/vaborbactam, or imipenem/relebactam
Carbapenem-resistant Klebsiella
pneumoniae/oxytoca
CREklebsiella_AR
Any Klebsiella oxytoca or Klebsiella pneumoniae that has tested Resistant (R) to at
least one of the following: imipenem, meropenem, doripenem, ertapenem,
meropenem/vaborbactam, or imipenem/relebactam
Carbapenem-non-susceptible
Pseudomonas aeruginosa
carbNS_PA_AR
Pseudomonas aeruginosa that has tested either Intermediate (I) or Resistant (R) to at
least one of the following: imipenem, meropenem, doripenem or
imipenem/relebactam
Extended-spectrum cephalosporin-
resistant Enterobacterales
b
ESCEall_AR
Any Escherichia coli, Klebsiella aerogenes, Klebsiella oxytoca, Klebsiella pneumoniae,
or Enterobacter spp. that has tested Resistant (R) to at least one of the following:
cefepime, ceftriaxone, cefotaxime, ceftazidime, ceftazidime-avibactam, or
ceftolozane-tazobactam
Extended-spectrum cephalosporin-
resistant E. coli
ESCecoli_AR
Any Escherichia coli that has tested Resistant (R) or Intermediate (I) to at least one of
the following: cefepime, ceftriaxone, cefotaxime, ceftazidime, ceftazidime-avibactam,
or ceftolozane-tazobactam
Extended-spectrum cephalosporin-
resistant Klebsiella
pneumoniae/oxytoca
ESCklebsiella_AR
Any Klebsiella oxytoca or Klebsiella pneumoniae that has tested Resistant (R) or
Intermediate (I) to at least one of the following: cefepime, ceftriaxone, cefotaxime,
ceftazidime, ceftazidime-avibactam, or ceftolozane-tazobactam
Fluoroquinolone-resistant
Enterobacterales
b
FQE_AR
Any Escherichia coli, Klebsiella aerogenes, Klebsiella oxytoca, Klebsiella pneumoniae,
or Enterobacter spp. that has tested Resistant (R) to at least one of the following:
ciprofloxacin, levofloxacin, or moxifloxacin
Fluoroquinolone-resistant
Pseudomonas aeruginosa
b
FQPA_AR
Pseudomonas aeruginosa that has tested Resistant (R) to at least one of the following:
ciprofloxacin or levofloxacin

January 2024 Antimicrobial Use and Resistance Module
AUR
14-75
Phenotype Name
Phenotype Code
Phenotype Definition
a
Multidrug-resistant Pseudomonas
aeruginosa
b
MDR_PA_AR
Pseudomonas aeruginosa that has tested either Intermediate (I) or Resistant (R) to at
least one drug in at least three of the following six categories
c
:
1. Extended-spectrum cephalosporin (cefepime, ceftazidime, ceftazidime-
avibactam, ceftolozane-tazobactam)
2. Fluoroquinolones (ciprofloxacin, levofloxacin)
3. Aminoglycosides (amikacin, gentamicin, tobramycin)
4. Carbapenems (imipenem, meropenem, doripenem, imipenem/relebactam)
5. Piperacillin/tazobactam
6. Cefiderocol
Carbapenem-non-susceptible
Acinetobacter spp.
carbNS_Acine_AR
Any Acinetobacter spp. that has tested either Intermediate (I) or Resistant (R) to at
least one of the following: imipenem, meropenem, or doripenem
Multidrug-resistant Acinetobacter
spp.
MDR_Acine_AR
Any Acinetobacter spp. that has tested either Intermediate (I) or Resistant (R) to at
least one drug in at least three of the following seven categories
c
:
1. Extended-spectrum cephalosporin (cefepime, ceftazidime, ceftriaxone,
cefotaxime)
2. Fluoroquinolones (ciprofloxacin, levofloxacin)
3. Aminoglycosides (amikacin, gentamicin, tobramycin)
4. Carbapenems (imipenem, meropenem, doripenem)
5. Piperacillin/tazobactam
6. Ampicillin/sulbactam
7. Cefiderocol
Vancomycin-resistant Enterococcus
faecalis
VREfaecalis_AR
Enterococcus faecalis that has tested Resistant (R) to vancomycin
Vancomycin-resistant Enterococcus
faecium
VREfaecium_AR
Enterococcus faecium that has tested Resistant (R) to vancomycin

January 2024 Antimicrobial Use and Resistance Module
AUR
14-76
Phenotype Name
Phenotype Code
Phenotype Definition
a
Vancomycin-resistant Enterococcus
b
VREgeneral_AR
Any Enterococcus spp. that has tested Resistant (R) to vancomycin
Fluconazole-resistant Candida
albicans/auris/glabrata/parapsilosis
/tropicalis
FR_Candi_AR
Any Candida albicans, Candida auris, Candida glabrata, Candida parapsilosis, or
Candida tropicalis that has tested Resistant (R) to fluconazole
Drug-resistant Streptococcus
pneumoniae
DR_SP_AR
Streptococcus pneumoniae that has tested either Intermediate (I) or Resistant (R) to
at least one of the antimicrobials listed in the NHSN AR Option defined drug panel
a
Adapted from CLSI M100
b
A SRIR is available for these phenotypes.
c
The category names are for grouping purposes and are not inclusive of all drugs in that drug class.

January 2024 Antimicrobial Use and Resistance Module
AUR
14-77
Appendix J. List of SRIRs and pSIRs
Table 1. Hospital-onset SRIRs
SRIR
Specimen Source
SRIR Type in NHSN
Hospital-onset Carbapenem-resistant
Enterobacterales
Blood
HO_CREall_Blood
Lower Respiratory Tract
HO_CREall_LRT
Urine
HO_CREall_Urine
Hospital-onset Extended-spectrum
cephalosporin-resistant Enterobacterales
Blood
HO_ESCEall_Blood
Lower Respiratory Tract
HO_ESCEall_LRT
Urine
HO_ESCEall_Urine
Hospital-onset Fluoroquinolone-resistant
Enterobacterales
Blood
HO_FQE_Blood
Lower Respiratory Tract
HO_FQE_LRT
Urine
HO_FQE_Urine
Hospital-onset Vancomycin-resistant
Enterococcus
Blood
HO_VRE_Blood
Lower Respiratory Tract
HO_VRE_LRT
Urine
HO_VRE_Urine
Hospital-onset Fluoroquinolone-resistant
Pseudomonas aeruginosa
Blood
HO_FQPA_Blood
Lower Respiratory Tract
HO_FQPA_LRT
Urine
HO_FQPA_Urine
Hospital-onset Multidrug-resistant
Pseudomonas aeruginosa
Blood
HO_MDR_PA_Blood
Lower Respiratory Tract
HO_MDR_PA_LRT
Urine
HO_MDR_PA_Urine
Hospital-onset Methicillin-resistant
Staphylococcus aureus
Blood
HO_MRSA_Blood
Lower Respiratory Tract
HO_MRSA_LRT
Urine
HO_MRSA_Urine
Table 2. Hospital-onset pSIRs
pSIR
Specimen Source
pSIR Type in NHSN
Hospital-onset
Enterobacterales
Blood
HO_Enterobacterales_Blood
Lower Respiratory Tract
HO_Enterobacterales_LRT
Urine
HO_Enterobacterales_Urine
Hospital-onset
Enterococcus
Blood
HO_Enterococcus_Blood
Lower Respiratory Tract
HO_Enterococcus_LRT
Urine
HO_Enterococcus_Urine
Hospital-onset
Staphylococcus aureus
Blood
HO_SA_Blood
Lower Respiratory Tract
HO_SA_LRT
Urine
HO_SA_Urine
Hospital-onset
Pseudomonas aeruginosa
Blood
HO_PA_Blood
Lower Respiratory Tract
HO_PA_LRT
Urine
HO_PA_Urine
