
CMS Manual System
Department of Health & Human
Services (DHHS)
Pub 100-04 Medicare Claims
Processing
Centers for Medicare &
Medicaid Services (CMS)
Transmittal 771 Date: DECEMBER 2, 2005
Change Request 4181
SUBJECT: Revisions to Pub. 100-04, Medicare Claims Processing Manual in
Preparation for the National Provider Identifier (NPI)
I. SUMMARY OF CHANGES: This Change Request creates a new section in chapter 1
of the manual which defines institutional provider indentifiers as they will be used over
the period of the NPI transition. It removes all other references to the Online Survey
Certification & Reporting system (OSCAR) numbers except in those cases where an
OSCAR number will continue to be used in the CMS internal processes.
NEW/REVISED MATERIAL
EFFECTIVE DATE: January 3, 2006
IMPLEMENTATION DATE: January 3, 2006
Disclaimer for manual changes only: The revision date and transmittal number apply
only to red italicized material. Any other material was previously published and
remains unchanged. However, if this revision contains a table of contents, you will
receive the new/revised information only, and not the entire table of contents.
II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual is not updated)
R = REVISED, N = NEW, D = DELETED
R/N/D CHAPTER/SECTION/SUBSECTION/TITLE
R
1/Table of Contents
R
1/80.3.2.2/FI Consistency Edits
N
1/160/Identifying Institutional Providers
R
3/20/Payment Under Prospective Payment System (PPS)
Diagnosis Related Groups (DRGs)
R
3/20.8/Payment to Hospitals and Units Excluded from IPPS
for Direct Graduate Medical Education (DGME) and
Nursing and Allied Health (N&AH) Education for Medicare
Advantage (MA) Enrollees
R
3/30.1/Requirements for CAH Services, CAH Skilled
Nursing Care Services and Distinct Part Units
R
3/30.1.2/Payment for Post-Hospital SNF Care Furnished by a

CAH
R
3/60/Swing-Bed Services
R
3/140.2.6/Outlier Payments: Cost-to-Charge Ratios
R
3/150.3/Affected Medicare Providers
R
3/150.13/Billing Requirements Under LTCH PPS
D
3/Addendum/Hospital Reclassifications and Redesignations
by Individual Hospital FY-2003
R
4/30.1/Coinsurance Election
R
4/141/Maryland Waiver Hospitals
R
4/250.2.2/Zip Code Files
R
4/260.1/Special Partial Hospitalization Billing Requirements
for Hospitals, Community Mental Health Centers, and
Critical Access Hospitals
R
4/260.1.1/Bill Review for Partial Hospitalization Services
Provided in Community Mental Health Centers (CMHC)
R
5/10/Part B Outpatient Rehabilitation and Comprehensive
Outpatient Rehabilitation Facility (CORF) Services-General
R
8/10.9/Dialysis Provider Number Series
R
8/60.8/Shared Systems Changes for Medicare Part B Drugs
for ESRD Independent Dialysis Facilities
R
9/10.2/Federally Qualified Health Centers (FQHCs)
R
10/40.1/Request for Anticipated Payment (RAP)
R
10/40.2/HH PPS Claims
R
11/20.1.2/Completing the Uniform (Institutional Provider)
Bill (Form CMS-1450) for Hospice Election
R
11/40.1.3.1/Care Plan Oversight
III. FUNDING:
No additional funding will be provided by CMS; Contractor activities are to be
carried out within their FY 2006 operating budgets.
IV. ATTACHMENTS:
Business Requirements
Manual Instruction
*Unless otherwise specified, the effective date is the date of service.

Attachment - Business Requirements
Pub. 100-04 Transmittal: 771 Date: December 2, 2005 Change Request 4181
SUBJECT: Revisions to Pub. 100-04, Medicare Claims Processing Manual in Preparation for the
National Provider Identifier (NPI)
I. GENERAL INFORMATION
A. Background: The Health Insurance Portability and Accountability Act (HIPAA) of 1996 requires
issuance of a unique NPI to physicians, suppliers, and other providers of health care. The implementing
regulation for that requirement can be found in 45 CFR Part 162, Subpart D (162.402-162.414). Several
articles referencing this initiative have been issued to educate physicians, suppliers, and other providers on
the NPI.
The Medicare Claims Processing Manual contains numerous references to legacy identifiers which have
been used prior to the NPI. In particular, many chapters in this manual refer to the use of the Online
Survey Certification & Reporting system (OSCAR) numbers to identify institutional providers. In
preparation for the NPI, the Medicare Claims Processing Manual has been revised to amend the sections
referencing the 6-digit alpha-numeric provider number (OSCAR) to conform to the future use of a 10 digit
numeric NPI provider number. This Change Request creates a new section in chapter 1 of the manual
which defines institutional provider identifiers as they will be used over the period of the NPI transition.
It removes all other references to OSCAR numbers except in those cases where an OSCAR number will
continue to be used in CMS internal processes.
B. Policy: The implementation of NPIs is required by HIPAA.
II. BUSINESS REQUIREMENTS
“Shall" denotes a mandatory requirement
"Should" denotes an optional requirement
Requirement
Number
Requirements Responsibility (“X” indicates the
columns that apply)
Shared System
Maintainers
F
I
R
H
H
I
C
a
r
r
i
e
r
D
M
E
R
C
F
I
S
S
M
C
S
V
M
S
C
W
F
Other
4181.1 Contractors shall be aware of the revisions to
the Medicare Claims Processing Manual in
regard to the implementation of the NPI as
required by HIPAA.
XX

III. PROVIDER EDUCATION
Requirement
Number
Requirements Responsibility (“X” indicates the
columns that apply)
Shared System
Maintainers
F
I
R
H
H
I
C
a
r
r
i
e
r
D
M
E
R
C
F
I
S
S
M
C
S
V
M
S
C
W
F
Other
None.
IV. SUPPORTING INFORMATION AND POSSIBLE DESIGN CONSIDERATIONS
A. Other Instructions: N/A
X-Ref Requirement # Instructions
B. Design Considerations: N/A
X-Ref Requirement # Recommendation for Medicare System Requirements
C. Interfaces: N/A
D. Contractor Financial Reporting /Workload Impact: N/A
E. Dependencies: N/A
F. Testing Considerations: N/A
V. SCHEDULE, CONTACTS, AND FUNDING
Effective Date*: January 3, 2006
Implementation Date: January 3, 2006
Pre-Implementation Contact(s): Yvonne Young,
(410) 786-1886,
Wil Gehne (410) 786-6148,
Post-Implementation Contact(s): Regional Office
No additional funding will be
provided by CMS; contractor
activities are to be carried out
within their FY 2006 operating
budgets.
*Unless otherwise specified, the effective date is the date of service.

Medicare Claims Processing Manual
Chapter 1 - General Billing Requirements
Table of Contents
(Rev. 771, 12-02-05)
160 - Identifying Institutional Providers
80.3.2.2 - FI Consistency Edits
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
In order to be processed correctly and promptly, a bill must be completed accurately. FIs
edit all Medicare required fields as shown below. If a bill fails these edits, FIs return it to
the provider for correction. If bill data is edited online, the edits are included in the
software. When FIs receive magnetic tape or paper bills, either directly or through a
billing service, they must ensure that these edits are made. Depending upon special
services billed, FIs may require additional edits.
FL 4. Type of Bill
a. Must not be spaces
b. Must be a valid code for billing. Valid codes are:
First Digit - Type of Facility:
1 - Hospital
NOTE: Hospital-based multi-unit complexes may also have use for
the following first digits when billing non-hospital services:
2 - Skilled Nursing
3 - Home Health
4 - Religious Non-Medical (Hospital)
7 - Clinic or Renal Dialysis Facility (requires special information in
second digit below)
8 - Special Facility or Hospital ASC Surgery (requires special information
in second digit, see below)
Second Digit - Classification (if first digit is 1-5):
1 - Inpatient (Part A)
2 - Hospital-Based or Inpatient (Part B) (includes HHA visits under a Part
B plan of treatment)
3 - Outpatient (includes HHA visits under a Part A plan of treatment and
use of HHA DME under a Part A plan of treatment)
4 - Other (Part B) (includes HHA medical and other health services not
under a plan of treatment, hospital and SNF for diagnostic clinical
laboratory services for “nonpatients”)
8 - Swing bed (used to indicate billing for SNF level of care in a hospital
with an approved swing bed agreement)
Second Digit - Classification (first digit is 7):
1 - Rural Health Clinic (RHC)
2 - Hospital-Based or Independent Renal Dialysis Facility
3 - Free-Standing Provider-Based Federally Qualified Health Center
(FQHC)
4 - Other Rehabilitation Facility (ORF)
5 - Comprehensive Outpatient Rehabilitation Facility (CORF)
6 - Community Mental Health Center (CMHC)
Second Digit - Classification (first digit is 8):
1 - Hospice (Nonhospital-based)
2 - Hospice (Hospital-based)
3 - Ambulatory Surgical Center Service to Hospital Outpatients
4 - Free Standing Birthing Center
5 - Critical Access Hospital (CAH)
Third Digit - Frequency:
A - Admission/Election Notice
B - Hospice/Medicare Coordinated Care Demonstration/Religious Non-
Medical Health Care Institution-Termination/Revocation Notice
C - Hospice Change of Provider
D - Hospice/Medicare Coordinated Care Demonstration/Religious Non-
Medical Health Care Institution-Void/Cancel
E - Hospice Change of Ownership
F - Beneficiary Initiated Adjustment Claim (For FI use only)
G - CWF Initiated Adjustment Claim (For FI use only)
H - CMS initiated Adjustment Claim (For FI use only)
I - FI Adjustment Claim (Other than QIO or Provider) (For FI use only)
J - Initiated Adjustment Claim-Other (For FI use only)
K - OIG Initiated Adjustment Claim (For FI use only)
M - MSP Initiated Adjustment Claim (For FI use only)
P - QIO Adjustment Claim (For FI use only)
0 - Nonpayment/zero claims
1 - Admit Through Discharge Claim
2 - Interim - First Claim
3 - Interim – Continuing Claims (Not valid for PPS bills. Exception: SNF
PPS bills)
4 - Interim – Last Claim (Not valid for PPS bills. Exception: SNF PPS
bills)
5 - Late charge
7 - Correction
8 - Void/Cancel
9 - Final Claim for a Home Health PPS Episode
FL 6. Statement Covers Period (From - Through)
a. Cannot exceed eight positions in either “From” or “Through” portion allowing for
separations (nonnumeric characters) in the third and sixth positions.
b. The “From” date must be a valid date that is not later than the “Through” date.
c. The “Through” date must be a valid date that is not later than the current date.
d. The number of days represented by this period must equal the sum of the covered
days (FL 7) and noncovered days (FL 8), if the type of bill is 11X, 18X, 21X, or
41X.
e. With the exception of Home Health PPS claims, the statement covers period may
not span 2 accounting years.
FL 7. Covered Days
FIs do not need to edit the provider’s bill. They determine the proper number of covered
days in their bill process.
FL 8. Noncovered Days
FIs do not need to edit the provider’s bill. They determine the proper number of
noncovered days in their bill process.
FL 9. Coinsurance Days
FIs do not need to edit the provider’s bill. They determine the proper number of
coinsurance days in their bill process.
FL 10. Lifetime Reserve Days
FIs do not need to edit the provider’s bill. They determine the proper number of lifetime
reserve days in their bill process.
FL 13. Patient’s Address
a. The address of the patient must include:
City
State (P.O. Code)
ZIP
b. Valid ZIP code must be present if the type of bill is 11X, 13X, 18X, 83X or
85X.
c. Cannot exceed 62 positions.
FL 14. Birthdate
a. Must be valid if present.
b. Cannot exceed 10 positions allowing for separations (nonnumeric characters)
in the third and sixth positions.
FL 15. Sex
a. One alpha position.
b. Valid characters are “M” or “F.”
c. Must be present.
FL 17. Admission Date
a. Must be valid if present.
b. Cannot exceed eight positions allowing for separations (nonnumeric characters)
in the third and sixth positions.
c. Present only if the type of bill is 11X, 12X, 18X, 21X, 22X, 32X, 33X, 41X,
81X or 82X.
d. Cannot be later than the “From” portion of Item 6.
FL 19. Type of Admission/Visit
a. One numeric position.
b. Required only if the type of bill is 11X, 12X, 18X, 21X, 22X, or 41X.
c. Valid codes are:
1 - Emergency
2 - Urgent
3 - Elective
4 - Newborn
5 - Trauma Center
9 - Information unavailable
FL 20. Source of Admission.
a. One numeric position
b. Must be present
c. Valid codes are:
1 - Physician referral
2 - Clinic referral
3 - HMO referral
4 - Transfer from a hospital
5 - Transfer from a SNF
6 - Transfer from another health care facility
7 - Emergency room
8 - Court/Law enforcement
9 - Information not available
A - Transfer from a Critical Access Hospital (CAH)
B - Transfer from another Home Health Agency (HHA)
C - Readmission to same Home Health Agency (HHA)
d. Valid codes for Newborns are:
1 - Normal Delivery;
2 - Premature Delivery;
3 - Sick Baby; and
4 - Extramural Birth.
FL 22. Patient Status.
a. Two numeric positions
b. Present on all Part A inpatient, SNF, hospice, home health agency, and
outpatient hospital services. Types of bill: 11X, 12X, 13X, 14X, 18X, 21X,
22X, 23X, 32X, 33X, 34X, 41X, 71X, 73X, 74X, 75X, 76X, 81X, 82X, 83X, or
85X.
c. Valid codes for hospitals, SNFs, HHAs and RNHCIs are:
01 - Discharged to home/self care (routine charge)
02 - Discharged/transferred to other short-term general hospital
03 - Discharged/transferred to SNF
04 - Discharged/transferred to ICF
05 - Discharged/transferred to a non-Medicare PPS children’s hospital or non-
Medicare PPS cancer hospital for inpatient care
06 - Discharged/transferred to home care of organized home health service
organization
07 - Left against medical advice
08 - Discharged/transferred to home under care of a home IV drug therapy
provider
09 - Admitted as an inpatient to this hospital
20 - Expired
30 - Still patient or expected to return for outpatient services
43 - Discharged/transferred to a Federal hospital (effective for discharges on
and after October 1, 2003)
50 - Discharged/transferred to Hospice - home
51 - Discharged/transferred to Hospice - medical facility
61 - Discharged/transferred to a hospital-based Medicare approved swing bed
62 - Discharged/transferred to an inpatient rehabilitation facility including
distinct part units of a hospital
63 - Discharged/transferred to a long-term care hospital (LTCH)
64 - Discharged/transferred to a nursing facility certified under Medicaid but
not certified under Medicare
65 - Discharged/transferred to a psychiatric hospital or psychiatric part unit of a
hospital (effective April 1, 2004)
71 - Discharged/transferred/referred to another institution for outpatient
services as specified by the discharge plan of care (deleted October 1,
2003)
72 - Discharged/transferred/referred to this institution for outpatient services as
specified by the discharge plan of care (deleted October 1, 2003)
d. Valid codes for hospice (81X or 82X) are:
01 - Discharged (left this hospice)
30 - Still patient
40 - Expired at home
41 - Expired in a medical facility such as a hospital, SNF, ICF, or freestanding
hospice
42 - Expired - place unknown
FL 23. Medical Record Number
a. If provided by the hospital, must be recorded by the FI for the QIO.
b. Must be left justified in CWF record for QIO.
FLs 24, 25, 26, 27, 28, 29, and 30. Condition Codes.
a. Each code is two numeric digits.
b. Valid codes are 01, 02, 03, 04, 05, 06, 07, 08, 09, 10, 11, 12, 13, 14, 15, 16, 17,
18, 19, 20, 21, 22, 23, 24, 25, 26, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39,
40, 41, 42, 43, 44, 45, 46, 48, 55, 56, 57, 58, 59, 61, 62, 63, 64, 65, 66, 70, 71,
72, 73, 74, 75, 76, 77, 78, 79, A5-A9, AA-AN, B0-B4, D0-D9, EO, GO, HO.
c. If code 07 is entered, type of bill must not be hospice 81X or 82X.
d. If codes 36, 37, 38, or 39 are entered, the type of bill must be 11X and the
provider must be a non-PPS hospital or exempt unit.
e. If code 40 is entered, the “From” and “Through” dates in FL 6 must be equal,
and there must be a “0” or “1” in FL 7 (Covered Days).
f. Only one code 70, 71, 72, 73, 74, 75, or 76 can be on an ESRD claim.
g. Code C1, C3, C4, C5, or C6 must be present if type of bill is 11X or 18X.
FLs 32, 33, 34, and 35. Occurrence Codes and Dates
a. All dates must be valid.
b. Each code must be accompanied by a date.
c. All codes are two alphanumeric positions.
d. Valid codes are 01-33, 35-37, 40-99, and A0-Z9.
e. If code 20 or 26 is entered, the type of bill must be 11X or 41X. If code 21 or
22 is entered, the type of bill must be 18X or 21X.
f. If code 27 is entered, the type of bill must be 81X or 82X.
g. If code 28 is entered, the first digit in FL 4 must be a “7” and the second digit a
“5.”
h. If code 42 is entered, the first digit in FL 4 must be “8” and the second digit
“1” or “2” and the third digit “1 or 4.”
i. If 01 - 04 is entered, Medicare cannot be the primary payer, i.e., Medicare-
related entries cannot appear on the “A” lines of FLs 58-62.
j. If code 20 is entered:
• Must not be earlier than “Admission” date (FL 17) or later than
“Through” date (FL 6).
• Must be less than 13 days after the admission date (FL 17) if “From”
date is equal to admission date (less than 14 days if billing dates cover
the period December 24 through January 2).
k. If code 21 is entered:
• Cannot be later than “Statement Covers Period” Through date; or
• Cannot be more than 3 days prior to the “Statement Covers Period”
From date.
l. If code 22 is entered, the date must be within the billing period shown in FL 6.
m. If code 31 is entered, the type of bill must be 11X, 21X, or 41X.
n. If code 32 is entered, the type of bill must be 13X, 14X, 23X, 32X, 33X, 34X,
71X, 72X, 73X, 74X, 75X, 81X, or 82X.
FL 36. Occurrence Span Codes and Dates
a. Dates must be valid.
b. Code entry is two alphanumeric positions.
c. Code must be accompanied by dates.
d. Valid codes are 70-79, M0-M5, and WZ-ZZ.
e. If code 70 is entered, the type of bill must be 11X, 18X, 21X, or 41X.
f. If code 71 is entered, the first digit of FL 4 must be “1,” “2,” or “4” and the
second digit must be “1.”
g. If code 72 is entered, the type of bill must be 13X, 14X, 32X, 33X, 34X, 71X,
73X, 74X, or 75X.
h. If code 74 is entered, the type of bill must be 11X, 13X, 14X, 18X, 21X, 34X,
41X, 71X, 72X, 74X, 75X, 81X, or 82X.
i. If code 75 is entered, the first digit of FL 4 must be “1” or “4” and the second
digit must be “1.”
j. If code 76 is entered, occurrence code 31 must be present (inpatient only).
k. If code 76 is entered, occurrence code 32 must be present (outpatient only).
l. If code 76, 77, or M1 is present, the bill type must be 11X, 13X, 14X, 18X,
21X, 34X, 41X, 71X, 72X, 73X, 74X, 75X, 81X, 82X, or 85X.
m. Neither the “From” nor the “Through” portion can exceed eight positions
allowing for separations (nonnumeric characters) in the third and sixth
positions of each field.
n. If code M2 is present, the bill type must be 81X or 82X.
o. Code 79 is for payer use only. Providers do not report this code.
FLs 39, 40, and 41. Value Codes and Amounts.
a. Each code must be accompanied by an amount.
b. All codes are two alphanumeric digits.
c. Amounts may be up to ten numeric positions. (00000000.00)
d. Valid codes are 01-99 and A0-ZZ.
e. If code 06 is entered, there must be an entry for code 37.
f. If codes 08 and/or 10 are entered, there must be an entry in FL 10.
g. If codes 09 and/or 11 are entered, there must be an entry in FL 9.
h. If codes 12, 13, 14, 15, 41, 43, or 47 are entered as zeros, occurrence codes 01,
02, 03, 04, or 24 must be present.
i. Entries for codes 37, 38, and 39 cannot exceed three numeric positions.
j. If the blood usage data is present, code 37 must be numeric and greater than
zero.
FL 42. Revenue Codes.
a. Four numeric positions.
b. Must be listed in ascending numeric sequence except for the final entry, which
must be “0001” for hardcopy claims only.
c. There must be a revenue code adjacent to each entry in FL 47.
d. For hospitals not subject to the outpatient prospective payment system (OPPS)
with types of bill 13X or 83X, the following revenue codes require a 5-position
HCPCS code:
0274, 030X, 031X, 032X, 034X, 035X, 040X, 046X, 0471, 0481, 0482, 061X,
0730, 0732, or 074X.
e. For bill types 32X and 33X the following revenue codes require a 5-position
HCPCS code:
0274, 029X, 042X, 043X, 044X, 055X, 056X, 057X, 0601, 0602, 0603, and 0604.
f. For bill type 34X, the following revenue codes require a 5-position HCPCS
code:
0271-0274, 42X, 43X, 44X, and 0601-0604.
g. For bill type 21X, 32X, 33X, or 11X (IRF facilities) the following revenue
codes require a 5-position HIPPS code:
0022 (SNF only), 0023 (HH only), 0024 (IRFs only).
FL 44. HCPCS Codes.
For bill type 13X or 83X, the HCPCS codes below must be reported with the specific
revenue code shown. These revenue codes can also be reported with other HCPCS
codes.
046X 94010, 94060, 94070, 94150, 94160, 94200, 94240, 94250,
94260, 94350, 94360, 94370, 94375, 94400, 94450, 94620,
94680, 94681, 94690, 94720, 94725, 94750, 94760, 94761,
94762, 94770
0471 92504, 92511, 92541, 92542, 92543, 92544, 92545, 92546,
92547, 92548, 92551, 92552, 92553, 92555, 92556, 92557,
92562, 92563, 92564, 92565, 92567, 92568, 92569, 92571,
92572, 92573, 92575, 92576, 92577, 92579, 92582, 92583,
92584, 92585, 92587, 92588, 92596
0480 93303, 93304, 93307, 93308, 93312, 93314, 93315, 93317,
93320, 93321, 93325, 93350, 93600, 93602, 93603, 93607,
93609, 93610, 93612, 93615, 93616, 93618, 93619, 93620,
93624, 93631, 93640, 93641, 93642, 93501, 93505, 93510,
93511, 93514
0481 93524, 93526, 93527, 93528, 93529, 93539, 93540, 93541,
93542, 93543, 93544, 93545, 93555, 93556, 93561, 93562,
Q0035
0482 93017
0636 Revenue code 0636 relates to the HCPCS code for drugs
requiring detailed coding.
0730 93005, 93024, 93041
0731 93024, 93041, 93225, 93226, 93231, 93232, 93236
0732 93012
074X 95805, 95807, 95808, 95810, 95812, 95813, 95816, 95819,
95822, 95824, 95827, 95829, 95920, 95933, 95950, 95951,
95953, 95954, 95955, 95956, 95957, 95958, 95961, 95962
075X 91000, 91010, 91011, 91012, 91020, 91030, 91034, 91035,
91052, 91055, 91060, 91065, 91122
0920 51736, 51741, 51792, 51795, 51797, 54250, 59020, 59025,
92060, 92065, 92081, 92082, 92083, 92235, 92240, 92250,
92265, 92270, 92275, 92283, 92284, 92285, 92286
0921 54240, 93721, 93731, 93732, 93733, 93734, 93735, 93736,
93737, 93738, 93740, 93770, 93875, 93880, 93882, 93886,
93888, 93922, 93923, 93924, 93925, 93926, 93930, 93931,
93965, 93970, 93971, 93975, 93976, 93978, 93979, 93980,
93981, 93990
0922 95858, 95860, 95861, 95863, 95864, 95867, 95868, 95869,
95872, 95875, 95900, 95903, 95904, 95921, 95922, 95923,
95925, 95926, 95930, 95934, 95936, 95937
0924 95004, 95024, 95027, 95028, 95044, 95052, 95056, 95060,
95065, 95070, 95071, 95078
For bill type 13X or 83X and revenue codes 0360-0369, a 5-position HCPCS code of
10000 - 69979 must be present unless diagnosis code V64.1, V64.2, or V64.3 is present.
For bill type 21X, 32X, 33X, or 11X (IRF facilities), HIPPS field for revenue codes
specific to SNF/HHA/IRF PPS (see item g in FL 44 above).
FL 45. Service Date
a. Six numeric positions, MMDDYY.
b. A single line item date of service (LIDOS) is required on every revenue code
present on outpatient types of bill 13X, 14X, 23X, 24X, 32X, 33X, 34X, 71X,
72X, 73X, 74X, 75X, 76X, 81X, 82X, 83X, and 85X and on inpatient Part B
types of bill 12X and 22X. Exception (LIDOS not required) for CAHs, Indian
Health Service hospitals, and hospitals located in American Samoa, Guam, and
Saipan.
c. When a particular service is rendered more than once during the billing period,
the revenue code and HCPCS code must be entered separately for each service
date.
FL 46. Units of Service
a. Up to seven numeric positions.
b. Must be present for all services with the exception of the HIPPS line item
service. (Exception: Units are required on the HIPPS line for SNF claims)
c. Accommodation units must equal covered days (FL 7) with the exception of the
R No-Pay.
FL 47. Total Charges
a. Up to 10 numeric positions (00000000.00).
b. There must be an entry adjacent to each entry in FL 42.
c. The “0001” amount must be the sum of all the entries for hardcopy only.
FLs 50A, B, and C. Payer Identification
a. "Medicare” must be entered on one of these lines depending upon whether it is
the primary, secondary or tertiary payer.
b. If value codes 12, 13, 14, 15, 16, 41, 42, 43, or 47 are present, data pertaining
to Medicare cannot be entered in Line A of FLs 50-62.
FL 51. Medicare Provider Number
a. A 6-position alpha/numeric field (for CMS use only, effective May 23, 2007,
providers are required to submit only their NPI).
b. Left justified.
FLs 58A, B, and C. Insured’s Name
a. Must be present. Cannot be all spaces.
FLs 60A, B, and C. Certificate/Social Security Number/HI Claim/Identification Number
a. Must be present.
b. Must contain nine numeric characters and at least one alpha character as a
suffix. The first alpha suffix is entered in position 10, the second in position
11, etc. The first three numbers must fall within the range of 001 through 680
or 700 through 728.
c. The alpha suffix must be A through F, H, J, K, M, T, or W. Alpha suffixes A
and T must not have a numeric subscript. Alpha suffixes B, C, D, E, F, M, and
W may or may not have a numeric subscript.
d. If the alpha suffix is H, it must be followed by A, B or C in position eleven.
The numeric subscript (position twelve) must conform with the above for the
A, B, or C suffix to be used.
e. RRB claim numbers must contain either six or nine numeric characters, and
must have one, two, or three character alpha prefix.
f. For prefixes H, MH, WH, WCH, PH and JA only a 6-digit numeric field is
permissible. For all other prefixes, a six or nine numeric field is permissible.
g. Nine numeric character claim numbers must have the same ranges as the SSA
9-position claim numbers.
FL 67. Principal Diagnosis Code.
a. Must be four or five positions left justified with no decimal points. FIs validate
with MCE and OCE programs.
b. Must be valid ICD-9-CM code.
FLs 68-75. Other Diagnosis Codes.
a. If present, must be four or five positions, left justified with no decimal points.
FIs validate with MCE and OCE programs.
FL 80 Principal Procedure Code and Date
a. If present, must be valid ICD-9-CM procedure code. FIs validate with MCE
program.
b. If code is present, date must be present and valid.
c. Date must fall before the “Through” date in FL 6. (In some cases it may be
before the admission date, i.e., where complications and admission ensue from
outpatient surgery.)
FL 81. Other Procedure Codes and Dates.
a. If present, apply edits for FL 80
FL 82. Attending/Referring Physician I.D.
• The UPIN must be present on inpatient Part A bills with a “Through” date of
January 1, 1992, or later. For outpatient and other Part B services, the UPIN
must be present if the “From” date is January 1, 1992, or later. This
requirement applies to all provider types and all Part B bill types.
° Number, last name, and first initial must be present;
° First three characters must be alpha or numeric; and
° If first three characters of UPIN are INT, RES, VAD, PHS, BIA, OTH,
RET, or SLF, exit. Otherwise, the 4th through 6th positions must be
numeric.
FL 83. Other Physician I.D
a. Must be present if:
•
•
•
•
•
•
Bill type is 11X and a procedure code is shown in FLs 80-81;
Bill type is 83X or 13X and a HCPCS code is reported that is subject to the
ASC payment limitation or is on the list of codes the QIO furnishes that
require approval; or
Bill type is 85X and HCPCS code is in the range of 10000 through 69979.
b. If required:
First three characters must be alpha or numeric:
Number, last name and first initial must be present; and
Left justified:
o If first three characters of UPIN are INT, RES, VAD, PHS, BIA,
OTH, RET, or SLF, exit. Otherwise the 4th through 6th positions
must be numeric.

160 - Identifying Institutional Providers
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
Effective January 3, 2006, the six position alpha-numeric provider number will begin
transitioning to the ten position numeric “National Provider Identifier” (NPI). The
following provides instructions on how the provider number (OSCAR) will be
transitioned to the NPI:
May 23, 2005 through January 2, 2006 Providers continue to submit the current
six position alpha-numeric provider
number. Any claims submitted with only
the NPI number will be returned as
unprocessable.
January 3, 2006 through October 1, 2006 Providers continue to submit the current
six position alpha-numeric provider
number. The NPI number may also be
submitted but must be present with the
current provider number.
October 2, 2006 through May 22, 2007 Providers may submit the current six
position alpha numeric provider number
and/or the NPI number.
Beginning May 23, 2007 Providers must only submit the NPI
number.
References to the six position alpha-numeric number or OSCAR number found
throughout the chapters of the Medicare Claims Processing Manual, on an ongoing
basis, are supplied only for the purpose of CMS internal processing. Therefore, these
references are documented as “for CMS use only”.
NOTE: All other references to “provider number” in the chapters that follow refer to
the usage of identifiers per the table above.
20 - Payment Under Prospective Payment System (PPS) Diagnosis
Related Groups (DRGs)
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
A General
The Social Security Amendments of 1983 (P.L. 98-21) provided for establishment of a
prospective payment system (PPS) for Medicare payment of inpatient hospital services.
(See
§20.4 for corresponding information for PPS capital payments and computation of
capital and operating outliers for FY 1992.) Under PPS, hospitals are paid a
predetermined rate per discharge for inpatient hospital services furnished to Medicare
beneficiaries. Each type of Medicare discharge is classified according to a list of DRGs.
These amounts are, with certain exceptions, payment in full to the hospital for inpatient
operating costs. Beneficiary cost-sharing is limited to statutory deductibles, coinsurance,
and payment for noncovered items and services. Section 4003 of OBRA of 1990 (P.L.
101-508) expands the definition of inpatient operating costs to include certain
preadmission services. (See
§40.3.)
The statute excludes children's hospitals and cancer hospitals, hospitals located outside
the 50 States. In addition to these categorical exclusions, the statute provides other
special exclusions, such as hospitals that are covered under State reimbursement control
systems. These excluded hospitals and units are paid on the basis of reasonable costs
subject to the target rate of increase limits.
In accordance with Section 1814 (b) (3) of the Act, services provided by hospitals in
Maryland subject to the Health Services Cost Review Commission (provider numbers
21000-21099) are paid according to the terms of the waiver, that is 94% of submitted
charges subject to any unmet Part B deductible and coinsurance.
For discharges occurring on or after April 1, 1988, separate standardized payment
amounts are established for large urban areas and rural areas. Large urban areas are
urban areas with populations of more than 1,000,000 as determined by the Secretary of
HHS on the basis of the most recent census population data. In addition, any New
England County Metropolitan Area (NECMA) with a population of more than 970,000 is
a large urban area.
The OBRA 1987 required payment of capital costs under PPS effective with cost
reporting periods that began October 1, 1991, or later. A 10-year transition period was
provided to protect hospitals that had incurred capital obligations in excess of the
standardized national rate from major disruption. High capital cost hospitals are known
as "hold harmless" hospitals. The transition period also provides for phase-in of the
national Federal capital payment rate for hospitals with capital obligations that are less
than the national rate. New hospitals that open during the transition period are exempt
from capital PPS payment for their first 2 years of operation. Hospitals and hospital
distinct part units that are excluded from PPS for operating costs are also excluded from
PPS for capital costs.
Capital payments are based on the same DRG designations and weights, outlier
guidelines, geographic classifications, wage indexes, and disproportionate share
percentages that apply to operating payments under PPS. The indirect teaching
adjustment is based on the ratio of residents to average daily census. The hospital split
bill, adjustment bill, waiver of liability and remaining guidelines that have historically
been applied to operating payments also apply to capital payments under PPS.
B Hospitals and Units Excluded
The following hospitals and distinct part hospital units (DPU) are excluded from PPS and
are paid on a reasonable cost or other basis:
• Pediatric hospitals whose inpatients are predominately under the age of 18.
• Hospitals located outside the 50 States.
• Hospitals participating in a CMS-approved demonstration project or State
payment control system.
• Nonparticipating hospitals furnishing emergency services have not been affected
by the PPS statute (P.L. 97-21). They are paid under their existing basis.
C Situations Requiring Special Handling
1 - Sole Community Hospitals are paid in accordance with the methods used to
establish the operating prospective rates for the first year of the PPS transition for
operating costs. The appropriate percentage of hospital-specific rate and the
Federal regional rate is applied by the Pricer program in accordance with the
current values for the appropriate fiscal year.
2 - Hospitals have the option to continue to be reimbursed on a reasonable cost basis
subject to the target ceiling rate or to be reimbursed under PPS if the following
are met:
• Recognized as of April 20, 1983, by the National Cancer Institute as
Comprehensive Cancer Centers or Clinical Research Centers;
• Demonstrating that the entire facility is organized primarily for treatment
of, and research on, cancer; and
• Having a patient population that is at least 50 percent of the hospital's total
discharges with a principal diagnosis of neoplastic disease.
The hospital makes this decision at the beginning of its fiscal year. The choice
continues until the hospital requests a change. If it selects reasonable cost subject
to the target ceiling, it can later request PPS. No further option is allowed.
3 - Regional and national referral centers within short-term acute care hospital
complexes. Rural hospitals that meet the criteria have their prospective rate
determined on the basis of the urban, rather than the rural, adjusted standardized
amounts, as adjusted by the applicable DRG weighting factor and the hospital's
area wage index.
4 - Hospitals in Alaska and Hawaii have the nonlabor related portion of the wage
index adjusted by their appropriate cost-of-living factor. These calculations are
made by the Pricer program and are included in the Federal portion of the rate.
5 - Kidney, heart, and liver acquisition costs incurred by approved transplant centers
are treated as an adjustment to the hospital's payments. These payments are
adjusted in each cost reporting period to compensate for the reasonable expenses
of the acquisition and are not included in determining prospective payment.
6 - Religious Nonmedical Health Care Institutions are paid on the basis of a
predetermined fixed amount per discharge. Payment is based on the historical
inpatient operating costs per discharge and is not calculated by "Pricer."
7 - Transferring hospitals with discharges assigned to DRG 385 (Neonates, Died or
Transferred) or DRG 504-511 (burns, transferred to another acute care facility)
have their payments calculated by the Pricer program on the same basis as those
receiving the full prospective payment. They are also eligible for cost outliers.
8 - Nonparticipating hospitals furnishing emergency services are not included in PPS.
9 - Veterans Administration (VA) Hospitals are generally excluded from
participation. Where payments are made for Medicare patients, the payments are
determined in accordance with 38 U.S.C. 5053(d).
10 - A hospital that loses its urban area status as a result of the Executive Office of
Management and Budget redesignation occurring after April 20, 1983, may
qualify for special consideration by having its rural Federal rate phased-in over a
2-year period. The hospital will receive, in addition to its rural Federal rate in the
first cost reporting period, two-thirds of the difference between its rural Federal
rate and the urban Federal rate that would have been paid had it retained its urban
status. In the second reporting period, one-third of the difference is applied. The
adjustment is applied for two successive cost reporting periods beginning with the
cost-reporting period in which CMS recognizes the reclassification.
11 - The payment per discharge under the PPS for hospitals in Puerto Rico is the sum
of:
• 50 percent of the Puerto Rico discharge weighted urban or rural
standardized rate.
• 50 percent of the national discharge weighted standardized rate.
(The special treatment of referral centers and sole community hospitals does not
apply to prospective payment hospitals in Puerto Rico.)
There are special criteria that facilities must meet in order to obtain approval for
payment for heart transplants and special processing procedures for these bills.
(See
§90.2.) Facilities that wish to obtain coverage of heart transplants for their
Medicare patients must submit an application and documentation showing their
initial and ongoing compliance with the criteria. For facilities that are approved,
Medicare covers under Part A all medically reasonable and necessary inpatient
services.
12 - Hospitals with high percentage of ESRD discharges may qualify for additional
payment. These payments are handled as adjustments to cost reports.
13 - Exception payments are provided for hospitals with inordinately high levels of
capital obligations. They will expire at the end of the 10-year transition period.
Exception payments ensure that for FY 1992 and FY 1993:
• Sole community hospitals receive 90 percent of Medicare inpatient capital costs:
• Urban hospitals with 100 or more beds and a disproportionate share patient
percentage of at least 20.2 percent receive 80 percent of their Medicare inpatient
capital costs; and
• All other hospitals receive 70 percent of their Medicare inpatient capital costs.
A limited capital exception payment is also provided during the 10-year capital transition
period for hospitals that experience extraordinary circumstances that require an
unanticipated major capital expenditure. Events such as a tornado, earthquake,
catastrophic fire, or a hurricane are examples of extraordinary circumstances. The capital
project must cost at least $5 million to qualify for this exception.
D DRG Classification
The DRGs are a patient classification system which provides a means of relating types of
patients a hospital treats (i.e., its case mix) to the costs incurred by the hospital. Payment
for inpatient hospital services is made on the basis of a rate per discharge that varies
according to the DRG to which a beneficiary's stay is assigned. All inpatient
transfer/discharge bills from both PPS and non-PPS facilities, including those from
waiver States, long-term care facilities, and excluded units are classified by the Grouper
software program into one of 489 diagnosis related groups (DRGs).
The following DRGs receive special attention:
• DRG No. 468 - Represents a discharge with valid data but where the surgical
procedure is unrelated to the principal diagnosis. This DRG has a weight
assigned and will be paid. The hospital must review the record on each DRG in
the remittance record and where either the principle diagnosis or surgical
procedure was reported incorrectly, prepare an adjustment bill. The FI may elect
to avoid the adjustment bill by returning the bill to the hospital prior to payment.
Further, Quality Improvement Organizations (QIOs) will review all DRG 468
cases.
• DRG No. 469 - Represents a discharge with a valid diagnosis in the principle
diagnosis field, but one not acceptable as a principal diagnosis. Examples include
a diagnosis of diabetes mellitus or an infection of the genitourinary tract during
pregnancy, both unspecified as to episode of care. These diagnoses may be valid,
but they are not sufficient to determine the principal diagnosis for DRG
assignment purposes. FIs will return the claims. The hospital must enter the
corrected principal diagnosis for proper DRG assignment and resubmit the claim.
• DRG No. 470 - Represents a discharge with invalid data. FIs return the claims
for correction of data elements affecting proper DRG assignment. The hospital
resubmits the corrected claim.
When the bills are processed in conjunction with the MCE (see
§20.2.1) coding
inconsistencies in the information and data are identified.
The MCE must be run before Grouper to identify inconsistencies before the bills are
processed through the Grouper.
E Difference in Age/Admission Versus Discharge
HO-415.4
When a beneficiary's age changes between the date of admission and date of discharge,
the DRG and related payment amount are determined from the patient's age at admission.
20.8 - Payment to Hospitals and Units Excluded from IPPS for Direct
Graduate Medical Education (DGME) and Nursing and Allied Health
(N&AH) Education for Medicare Advantage (MA) Enrollees
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
During the period January 1, 1998 through December 31, 1998, hospitals received 20
percent of the fee-for-service DGME and operating IME payment. This amount increased
by 20 percentage points each consecutive year until it reached 100 percent in calendar
year (CY) 2002.
Non-IPPS hospitals and units may submit their MA claims to their respective FIs to be
processed as no-pay bills so that the MA inpatient days can be accumulated on the
Provider Statistics & Reimbursement Report (PS&R) (report type 118) for DGME
payment purposes through the cost report.
This applies to the following hospitals and units excluded from the IPPS:
• Rehabilitation units
• Psychiatric units
• Rehabilitation hospitals
• Psychiatric hospitals
• Long-term Care hospitals
• Children’s hospitals
• Cancer hospitals
In addition, this applies to all hospitals that operate a nursing or an allied health (N&AH)
program and qualify for additional payments related to their MA enrollees under 42 CFR
§413.87(e). These providers may similarly submit their MA claims to their respective FIs
to be processed as no-pay bills so that the MA inpatient days can be accumulated on the
PS&R (report type 118) for purposes of calculating the MA N&AH payment through the
cost report.
Non-IPPS hospitals, hospitals with rehabilitation and psychiatric units, and hospitals that
operate an approved N&AH program must submit claims to their regular FI in UB-92
format, with condition codes 04 and 69 present on record type 41, fields 4-13, (Form
Locator 24-30). The provider uses Condition code 69 to indicate that the claim is being
submitted as a no-pay bill to the PS&R report type 118 for MA enrollees in non-IPPS
hospitals and non-IPPS units to capture MA inpatient days for purposes of calculating the
DGME and/or N&AH payment through the cost report.
The FI submits the claim to the Common Working File (CWF). The CWF determines if
the beneficiary is a MA enrollee and what his/her plan number and effective dates are.
The plan must be a MA plan, per 42 CFR §422.4. Upon verification from CWF that the
beneficiary is a MA enrollee, the FI adds the MA plan number and an MA Pay Code of
“0” to the claim. For fee-for-service claims that were previously paid and posted to
history for the same period (due to late posting of MA enrollment data), an L-1002
Automatic Cancellation Adjustment Report will be sent to the FI when a DGME-only or
a N&AH-only claim from a non-IPPS hospital or unit is accepted for payment by CWF.
No deductible or coinsurance is to be applied against this claim nor is the beneficiary's
utilization updated by CWF for this stay. If CWF enrollment records do not indicate that
the beneficiary is a MA enrollee, CWF rejects the claim and the FI notifies the hospital of
this reason. The hospital may resubmit the claim after 30 days to see if the enrollment
data has been updated. No interim bills should be submitted for DGME-only or N&AH-
only claims and no Medicare Summary Notices should be prepared for these claims.
The DGME payments are made using the same interim payment calculation FIs currently
employ. Specifically, FIs must calculate the additional DGME payments using the
inpatient days attributable to MA enrollees. As with DGME and N&AH education
payments made under fee-for-service, the sum of these interim payment amounts is
subject to adjustment upon settlement of the cost report. Note that these DGME and/or
N&AH payments apply both to IPPS and non-IPPS hospitals and units.
Teaching hospitals that operate GME programs (see 42 CFR §413.86) and/or hospitals
that operate approved N&AH education programs (see 42 CFR §413.87) must submit
separate bills for payment for MA enrollees. The MA inpatient days are recorded on
PS&R report type 118. For services provided to MA enrollees by hospitals that do not
have a contract with the enrollee’s plan, non-IPPS hospitals and units are entitled to any
applicable DGME and/or N&AH payments under these provisions. Therefore, such
hospitals and units should submit bills to their FI for these cases in accordance with this
section’s instructions. In addition to submitting the claims to the PS&R report type 118,
hospitals must properly report MA inpatient days on the Medicare cost report, Form
2552-96, on worksheet S-3, Part I, line 2 column 4, and worksheet E-3, Part IV, lines
6.02 and 6.06.
30.1 - Requirements for CAH Services, CAH Skilled Nursing Care
Services and Distinct Part Units
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
A CAH may provide acute inpatient care for a period that does not exceed, as determined
on an annual average basis, 96 hours per patient. The CAH's length of stay will be
calculated by their FI based on patient census data and reported to the CMS regional
office (RO). If a CAH exceeds the length of stay limit, it will be required to develop and
implement a corrective action plan acceptable to the CMS RO, or face termination of its
Medicare provider agreement.
Items and services that a CAH provides to its inpatients are covered if they are items and
services of a type that would be covered if furnished by an acute care hospital to its
inpatients. A CAH may use its inpatient facilities to provide post-hospital SNF care and
be paid for SNF-level services if it meets the following requirements:
1. The facility has been certified as a CAH by CMS;
2. The facility operates up to 25 beds for either acute (CAH) care or SNF swing
bed care (any bed of a unit of the facility that is licensed as a distinct-part SNF is not
counted under paragraph (1) of this section); and
3. The facility has been granted swing-bed approval by CMS.
A CAH that participated in Medicare as a rural primary care hospital (RPCH) on
September 30, 1997, and on that date had in effect an approval from CMS to use its
inpatient facilities to provide post-hospital SNF care, may continue in that status under
the same terms, conditions, and limitations that were applicable at the time those
approvals were granted.
A CAH may establish psychiatric and rehabilitation distinct part units effective for cost
reporting periods beginning on or after October 1, 2004. The CAH distinct part units
must meet the following requirements:
1. The facility distinct part unit has been certified as a CAH by CMS;
2. The distinct part unit meets the conditions of participation requirements for
hospitals;
3. The distinct part unit must also meet the requirements, other than conditions of
participation requirements, that would apply if the unit were established in an acute care
hospital;
4. Services provided in these distinct part units will be paid under the payment
methodology that would apply if the unit was established in an acute care (non-CAH)
hospital paid under the hospital inpatient PPS; Inpatient Rehabilitation Facilities in
CAHs are paid under the Inpatient Rehabilitation Facility PPS (see Pub 100-04, Chapter
3, Section 140 for billing requirements) and the Inpatient Psychiatric Units in CAHs are
paid on a reasonable cost basis until a prospective payment system is created (expected
in 2005);
5. Beds in these distinct part units are excluded from the 25 bed count limit for
CAHs;
6. The bed limitations for each distinct part unit is 10; and
If a distinct part unit does not meet applicable requirements with respect to a cost
reporting period, no payment may be made to the CAH for services furnished in the unit
during that period. Payment may resume only after the CAH has demonstrated that the
unit meets applicable requirements.
30.1.2 - Payment for Post-Hospital SNF Care Furnished by a CAH
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
The SNF-level services provided by a CAH, are paid at 101% of reasonable cost. Since
this is consistent with the reasonable cost principles, FIs will now pay for those services
at 101% reasonable cost. Hospitals must follow the rules for payment in
§60 for swing-
bed services.
Coinsurance and deductible are applicable for inpatient CAH payment.
All items on Form CMS-1450 are completed in accordance with Chapter 25.
60 - Swing-Bed Services
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
Swing-bed services require the provider to bill inpatient hospital services and SNF
services separately. The provider must meet the 3-day hospital stay requirement and the
timely transfer requirement. (See Pub. 100-02, Medicare Benefit Policy Manual, Chapter
8.)
Swing-bed hospitals use one provider number when billing for hospital services to
identify hospital swing-bed SNF bills. The following alpha letters identify hospital
swing-bed SNF bills (for CMS use only, effective May 23, 2007, providers are required to
submit only their NPI. NOTE: The swing-bed NPI will be mapped to the 6-digit alpha-
numeric legacy (OSCAR) number.):
• "U" = short-term/acute care hospital swing-bed;
• "W" = long-term hospital swing-bed; and
• "Y" = rehabilitation hospital swing-bed.
A Inpatient Hospital Services in a Swing-Bed
Where there is no change to a SNF level of care, hospitals bill services in accordance
with hospital billing instructions. Where the beneficiary's level of care changes from
hospital to SNF level, the provider shows patient status code 03 on the hospital bill in FL
22 to indicate transfer to a SNF level of care. (This constitutes a discharge for purposes
of Medicare payment for inpatient hospital services under PPS.) The FI indicates in FL 6
the last day of care at the hospital level.
B SNF Services in a Swing-Bed
Services are billed, in accordance with Chapter 25 with the following exceptions:
• The date of admission on the swing-bed SNF bill is the date the patient began to
receive SNF level of care services;
• State level agreements may call for varying types of bill coding in FL 4. CMS
does not perform edits on type of bill coding on bills with 8 in the 2nd digit (bill
classification), in FL 18 of the CWF inpatient record if the record is identified in
FL 1 as hospital or SNF. Therefore, the FI accepts, with subsequent conversion,
any bill type agreed to at the State level to identify swing-bed billing, e.g., 18X,
28X, 11X, 21X. It must be sure the record identification of CWF FL 1 is
consistent with the provider number shown; and
• If the hospital has 50-99 beds, the following additional processing rules apply:
° The hospital may not be paid for more than the number of capped days for
swing bed stays. See subsection
C for determining the limitation.
° When the hospital is notified that a SNF bed is available, the hospital is not
paid for services furnished after the 5-day transfer period (excluding
weekends and holidays). This rule does not apply if the patient's physician
certified within the 5-day period that a transfer to a SNF was not medically
necessary.
° If the physician certified the transfer, occurrence code 26 must be shown.
This code identifies the date a SNF bed became available on or after the date
the patient was healthy enough for transfer.
The FI is responsible for review to ensure that the provider has considered availability of
a SNF bed and obtained appropriate certification. The FI assumes that payment is
appropriate on initial bills and is subject to the cap limitation. The QIO may later deny
the bill and notify the FI.
See Pub. 100-02, Medicare Benefit Policy Manual, Chapter 8 for additional coverage
policy information.
C Application of Capped Amount (50-99) Bed Provider
Payment is limited to swing bed providers of 50 - 99 beds. The cap is determined by
multiplying .15 times the product of the number of days in the cost reporting period and
the average number of licensed beds at the hospital for the period. From its State
licensing agency, the FI determines the number of licensed beds at the beginning of a cost
reporting period or from the date of the swing-bed approval, if later.
In States that do not license beds, hospitals use the total number of hospital beds reported
on their most recent Certificate of Need (CON) (excluding bassinets). If during the cost
reporting period there is an increase or decrease in the number of licensed beds, the FI
multiplies the number of licensed beds for each part of the period by the number of days
for which that number of licensed beds was available. After totaling the results, it
computes 15 percent of the total available licensed bed days to determine the payment
limitation.
The FI maintains a record for each swing-bed provider of 50-99 beds. This record must
contain the following information:
• The number of days that may be paid under the cap;
• The SNF days paid for the period (or the days remaining if the FI prefers); and
• The date the cap is met (not the date the FI records it).
The FI notifies the hospital if a beneficiary's extended care stay cannot be covered
because the cap has been reached. In such a case, the law prohibits payment under Part
A. However, payment may be made under Part B for certain medical and other health
services. (See Chapter 1.)
On each bill from a provider with 50-99 beds, the FI determines whether the provider had
already met the cap limit before the date of admission to the SNF level of care. If an
admission occurs prior to the date the capped days are exhausted, the entire stay is paid
(if otherwise covered) even though the cap is met during the stay.
140.2.6 - Outlier Payments: Cost-to-Charge Ratios
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
This section describes the appropriate data sources for computing an overall Medicare
facility-specific cost-to-charge ratio (CCR) for the purpose of determining outlier
payments under the IRF PPS. For discharges beginning on or after October 1, 2003, FIs
will use a CCR from the most recent tentative settled cost report or the most recent settled
cost report (whichever is the later period). FIs will use the cost report and the associated
data in determining a facility’s overall Medicare CCR specific to freestanding IRFs of for
IRFs that are distinct part units of acute care hospitals.
The Medicare cost reporting forms contain information on both Medicare inpatient costs
and charges. In addition, Medicare charges should be contained in the provider statistical
and reimbursement (PS&R) report associated with a specific cost reporting period. If the
overall Medicare CCR appears to be substantially out-of-line with similar facilities, the FI
should ensure that the underlying costs and charges are properly reported.
Effective October 1, 2003, an IRF will be assigned the appropriate national average CCR
that falls above three standard deviations from the national mean (upper threshold). CMS
will not use a lower threshold and an IRF will receive their actual CCR, no matter how
low their ratio falls.
For discharges occurring on or after October 1, 2003 and before October 1, 2004, the
upper threshold is 1.461 and the national CCRs are 0.597 for rural IRFs and 0.554 for
urban IRFs. For discharges occurring on or after October 1, 2004, and before October 1,
2005, the upper threshold is 1.461, and the national CCR are 0.636 for rural IRFs and
0.531 for urban IRFs.
The IRF PPS covers operating and capital-related costs and excludes medical education
and nurse anesthetist costs paid for on a reasonable cost basis. Therefore, total Medicare
charges for IRFs will consist of the sum of the inpatient routine charges and the sum of
inpatient ancillary charges (including capital). Total Medicare costs will consist of the
sum of inpatient routine costs (net of private room differential and swingbed) plus the
sum of ancillary costs plus capital-related pass-through costs only.
The provider specific file contains a field for the operating CCR (Field 25; file position
102-105) and for the capital CCR (Field 42; file position 203-206). Because the CCR
computed for the IRF PPS includes routine, ancillary, and capital costs, the CCR for
freestanding IRFs, units, and new providers described below will be entered on the
provider specific file only in field 25; file position 102-105. Field 42; file position 203-
206 of the provider specific file must be zero-filled.
A Calculating Medicare CCRs for Freestanding IRFs
For freestanding IRFs, Medicare charges will be obtained from Worksheet D-4, Column
2, lines 25 through 30 plus line 103 from the cost report (where possible, these charges
should be confirmed with the PS&R data). For freestanding IRFs, total Medicare costs
will be obtained from Worksheet D-1, Part II, line 49 minus (Worksheet D, Part III, col.
8, lines 25 through 30 plus Worksheet D, Part IV, col., line 101). Divide the Medicare
costs by the Medicare charges to compute the CCR.
B - Calculating Medicare CCRs for IRF Distinct Part Units
For IRF distinct part units, total Medicare inpatient routine and ancillary charges will be
obtained from the PS&R report associated with the latest settled cost report. [If PS&R
data is not available, estimate Medicare routine charges by dividing Medicare routine
costs on Worksheet D-1, Part II, line 41, by the result of Worksheet C, Part I, line 31,
column 3 divided by line 31, column 6. Add this amount to Medicare ancillary charges on
Worksheet D-4, column 2, line 103 to arrive at total Medicare charges.] To calculate the
total Medicare costs for distinct part units, data will be obtained from Worksheet D-1,
Part II, line 49 minus (Worksheet D, Part III, col. 8, line 31 plus Worksheet D, Part IV,
col. 7, line 101). Divide the total Medicare costs by the total Medicare charges to
compute the cost-to-charge ratio.
C - Calculating Medicare CCRs for New IRFs
As stated in the final rule, new facilities may receive outlier payments even though they
will not have the historical cost report information needed to compute the estimated cost
that determines if a case is an outlier. Therefore, a national CCR based on the facility
location of either urban or rural will be used. Specifically, for FY 2005, CMS has
estimated a national CCR of 0.636 for rural IRFs and 0.531 for urban IRFs. Unless
otherwise notified, FIs use these national ratios until the facility's actual CCR can be
computed using the first tentative settled or final settled cost report data which will then
be used for the subsequent cost report period.
The CMS will continue to set forth the upper threshold (i.e., 3 standard deviations above
the national geometric mean CCR) and the national CCRs applicable to IRFs in each
year’s annual notice of prospective payment rates published in the Federal Register.
D - Use of More Recent Data for Determining CCRs
In order to arrive at a CCR to be used in the PSF based on tentative settlement data, the
intermediary should review previous adjustments used (if any) in the tentative settlement
and take into consideration the impact of prior audit adjustments on prior period CCR to
determine if they had an impact on the CCR. If these tentative settlement adjustments
have no impact on the CCR, or if no adjustments were made, the tentative settled CCR
will equal the CCR from the IRF’s as-filed cost report. If the adjustments made at
tentative settlement would have an impact on the CCR, the intermediary should compute
a new CCR based on the tentative settlement. (NOTE: If the tentative settlement
adjustments result in a difference in the CCR from the as filed cost report of 20% or less,
then no adjustment to the CCR at tentative settlement is necessary.)
Following the initial update of the CCR for all IRFs for discharges on or after October 1,
2003, FIs should continue to update an IRF’s CCR each time a more recent cost report is
tentatively settled. Revised CCRs must be entered into the PSF not later than 45 days
after the date of the tentative settlement or final settlement used in calculating the CCRs.
Subject to the approval of CMS, CCRs may be revised more often if a change in a
hospital’s operations occurs which materially affects a hospital’s costs or charges.
Revised CCRs will be applied prospectively to all IRF PPS claims processed after the
update.
The CMS may direct FIs to use an alternative CCR to the CCR from the later of the latest
settled cost report or latest tentative settled cost report, if CMS believes this will result in
a more accurate CCR. In addition, if the FI finds evidence that indicates that using data
from the latest settled or tentatively settled cost report would not result in the most
accurate CCR, the FI should contact CMS to seek approval to use a CCR based on
alternative data. Also, a facility will have the opportunity to request that a different CCR
be applied in the event it believes the CCR being applied is inaccurate. The IRF is
required to present substantial evidence supporting its request. Such evidence should
include documentation regarding its costs and charges that demonstrate its claim that an
alternative ratio is more accurate. The regional office must approve any such request
after evaluation by the fiscal intermediary of the evidence presented by the IRF.
E - Reconciling Outlier Payments for IRFs
For discharges occurring in cost reporting periods beginning on or after October 1, 2003,
FI s are to reconcile IRF PPS outlier payments at the time of cost report final settlement
if:
1) Actual CCR is found to be plus or minus 10 percentage points from the CCR used
during that time period to make outlier payments, and
2) Outlier payments exceed $500,000 in that cost reporting period.
The return codes from the PRICER software may be used to identify the cases for which
outlier payments were made in a cost reporting period. These criteria for the IRF PPS
will be reevaluated periodically to assess whether they should be revised.
In the event that these criteria do not identify facilities that are being overpaid (or
underpaid) significantly for outliers, then, based on an analysis of the facility’s most
recent cost and charge data that indicates that the CCR for those facilities are
significantly inaccurate, FIs also have the administrative discretion to reconcile cost
reports of those IRFs. However, FIs must seek approval from their regional office in the
event they intend to reconcile outlier payments for an IRF that does not meet the above-
specified criteria. The CMS will be issuing separate instructions detailing procedures to
follow regarding this reconciliation process and the application of the adjustment for the
time value of money.
F - Notification to Facilities Under the IRF PPS
The FIs are to notify a facility whenever they make a change to its CCR. When a CCR is
changed as a result of a tentative settlement or a final settlement, the change to the CCR
should be included in the notice that is issued to each provider after a tentative or final
settlement is completed.
150.3 - Affected Medicare Providers
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
LTCHs are certified under Medicare as short-term acute care hospitals and, for
Medicare payment purposes, are generally defined as having an average inpatient length
of stay of greater than 25 days.
Veterans Administration Hospitals, hospitals that are reimbursed under state cost control
systems approved under
42 CFR Part 403, and hospitals that are reimbursed in
accordance with demonstration projects authorized under §402(a) of Public Law 90-248
(42 U.S.C. 1395b-1) or §222(a) of Public Law 92-603 (42 U.S.C. 1395b-1) are not
included in the LTCH PPS. (See 42 CFR §412.22(c).) Payment to foreign hospitals will
be made in accordance with the provisions set forth in
42 CFR 413.74. Currently, two of
the four Maryland LTCHs included on CMS' OSCAR database are presently paid in
accordance with demonstration projects (i.e., the Maryland "Waiver") and therefore not
subject to payments under the LTCH PPS: Levindale Hebrew Geriatric Center and
Deaton Hospital and Medical Center (now known as University Specialty Hospital).
150.13 - Billing Requirements Under LTCH PPS
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
Billing LTCH PPS Services
Effective with cost reporting periods beginning on or after October 1, 2002, LTCHs are
to incorporate the following so that FIs accurately price and pay a claim under the
LTCH PPS. These claims must be submitted on Type of Bill 11X.
This is a DRG- based payment system; therefore the LTCH DRG is determined by the
grouping of ICD-9-CM codes based on the principal diagnosis, up to eight additional
diagnoses, and up to six procedures performed during the stay, as well as age, sex, and
discharge status of the patient on the claim. Grouper software will determine DRG
assignment.
Each bill from a LTCH must contain the complete diagnosis and procedure coding for
purposes of the GROUPER software. Normal adjustments will be allowed. LTCH
providers submit one admit through discharge claim for the stay. Final PPS payment is
based upon the discharge bill.

30.1 - Coinsurance Election
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
The transition to the standard Medicare coinsurance rate (20 percent of the APC payment
rate) will be gradual. For those APC groups for which coinsurance is currently a
relatively high proportion of the total payment, the process will be correspondingly
lengthy. The law offers hospitals the option of electing to reduce coinsurance amounts
and advertise their reduced rates for all OPPS services. They may elect to receive a
coinsurance payment from Medicare beneficiaries that is less than the wage adjusted
coinsurance amount per APC. That amount will apply to all services within that APC.
This coinsurance reduction must be offered to all Medicare beneficiaries.
Hospitals should review the list of APCs and their respective coinsurance amounts that is
published in the Federal Register for the applicable year as a final rule. After adjusting
those coinsurance amounts for the wage index applicable to their MSA, hospitals must
notify their FIs if they wish to charge their Medicare beneficiaries a lesser amount. The
election remains in effect until the following calendar year. The first election must be
filed by July 1, 2000, for the period August 1, 2000, through December 31, 2000. Future
calendar year elections must be made by December 1st of the year preceding the calendar
year for which the election is being made.
Because the final rule on OPPS payment rates for 2002 was not published until March 1,
2002, providers were unable to make election decisions for 2002 by December 1
preceding the year the payment rates became effective, the typical deadline for making
such elections. The deadline for providers to make elections to reduce beneficiary
copayments for 2002 was extended until April 1, 2002. The elections are effective for
services furnished on or after April 1, 2002.
The lesser amount elected:
• May not be less than 20 percent of the wage adjusted APC payment amount;
• May not be greater than the inpatient hospital deductible for that calendar year
($812 for 2002); and
• Will not be wage adjusted by the FI or CMS.
Once an election to reduce coinsurance is made, it cannot be rescinded or changed until
the next calendar year. National unadjusted and minimum unadjusted coinsurance
amounts will be posted each year in the addenda of the OPPS final rule (Form
CMS-1005FC) on CMS’ Web site
(http://www.cms.hhs.gov).
This coinsurance election does not apply to partial hospitalization services furnished by
CHMCs, vaccines provided by a CORF, vaccines, splints, casts, and antigens provided by
HHAs, or splints, casts, and antigens provided to a hospice patient for the treatment of a
non-terminal illness. It also does not apply to screening colonoscopies, screening
sigmoidoscopies, or screening barium enemas, or to services not paid under OPPS.
Hospitals must utilize the following format for notification to the FI:
Provider number
1122334455
Provider name XYZ Hospital Effective from 8/1/2000 -
12/31/2000
Provider contact Joe Smith Phone # 123-456-7890
XYZ Hospital elects to reduce coinsurance to the amount shown for the following APCs:
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
APC____ Coinsurance___.__ APC____ Coinsurance___.__
Return to:
Provider Audit & Reimbursement Dept.
Attn: John Doe
FI Address
The FI must validate that the reduced coinsurance amount elected by the hospital is not
less than 20 percent of the wage adjusted APC amount nor more than the inpatient
deductible for the year of the election, and must send an acknowledgment to the hospital
that the election has been received, within 15 calendar days of receipt.
141 – Maryland Waiver Hospitals
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
In accordance with §1814 (b)(3) of the Act, services provided by hospitals in Maryland
subject to the Health Services Cost Review Commission are paid according to the terms
of the waiver, that is 94% of submitted charges subject to any unmet Part B deductible
and coinsurance. Payment should not be made under a fee schedule or other payment
method for outpatient items and services provided except the following situations:
• Non-patient laboratory specimens are paid under the clinical diagnostic laboratory
fee schedule (bill type 14X); and
Ambulance services which are subject to the ambulance fee schedule.
250.2.2 - Zip Code Files
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
The CMS shall provide a file of zip codes for payment for the primary care and specialty
physician scarcity bonus. The file will be effective for claims with dates of service on or
after January 1, 2005. Contractors will be notified by e-mail of the name of the file and
when it will be available for downloading.
Prior to January 1, 2005, CMS will post on its Web site zip codes that are eligible for the
bonus payment. Through regularly scheduled bulletins and list serves, intermediaries
must notify the CAH to verify their zip code eligibility via the CMS Web site.
Effective January 1, 2005, the HPSA bonus designations will be updated annually and
will be effective for services rendered with dates of service on or after January 1 of each
calendar year beginning January 1, 2005 through December 31, 2005. Once the annual
designations are made, no interim changes will be made to account for HRSA updates to
designations throughout the year. (Effective January 1, 2005, CAHs will no longer have
to notify the FI of their HPSA designation). Designations of new HPSAs during a
calendar year will be included in the next annual update. However, should a CAH
become designated as a HPSA area after the annual update through the HRSA Web site
or other method of notification, the bonus payment can be made for qualified physician
services. The CAH will have to notify the intermediaries of their change in status.
The contractors and standard systems will be provided with a file at the appropriate time
prior to the beginning of the calendar year for which it is effective. This file will contain
zip codes that fully and partially fall within a HPSA bonus area for both mental health
and primary care services. After the implementation of this new process, a recurring
update notification will be issued for each annual update. Contractors will be informed
of the availability of the file and the file name via an email notice.
Contractors will automatically pay bonuses for services rendered in zip code areas that:
1) fully fall within a designated primary care or mental health full county HPSA; 2) are
considered to fully fall in the county based on a determination of dominance made by the
United States Postal Service (USPS); or 3) are fully within a non-full county HPSA area.
Should a zip code fall within both a primary care and mental health HPSA, only one
bonus will be paid on the service. Bonuses for mental health HPSAs will only be paid
when performed by psychiatrists.
For services rendered in zip code areas: 1) that do not fall within a designated full county
HPSA; 2) are not considered to fall within the county based on a determination of
dominance made by the USPS; or 3) are partially within a non-full county HPSA, the
CAH must still submit a QB or QU modifier to receive payment for claims with dates of
service prior to January 01, 2006. Effective for claims with dates of service on or after
January 01, 2006, the modifier AQ, Physician providing a service in a Health
Professional Shortage Area (HPSA), must be submitted. To determine whether a
modifier is needed, the CAH must review the information provided on the CMS Web site
for HPSA designations to determine if their location is, indeed, within a HPSA bonus
area.
For service rendered in zip code areas that cannot automatically receive the bonus, it will
be necessary to know the census tract of the area to determine if a bonus should be paid

and a modifier submitted. Census tract data can be retrieved by visiting the U.S. Census
Bureau Web site at
www.Census.gov.
For services with dates of service prior to January 1, 2005, CAHs must indicate that the
services were provided in an incentive-eligible rural or urban HPSA by using one of the
following modifiers:
• QB - physician providing a service in a rural HPSA; or
• QU - physician providing a service in an urban HPSA.
The required format for the quarterly report:
Quarterly HPSA and Scarcity Report for CAHs
Provider Number Beneficiary
HICN
DCN Rev.
Code
HCPCS LIDOS Line
Item
Payment
Amount
10% of
Line
Payment
Amount
5% of
Line
Payment
Amount
123456 (Effective
May 23, 2007 this
number will be
f
or CMS use only.
FIs are required
to use the
providers NPI.)
1122334455
Abcdefghijk xxxxxxxxx xxx 12345 3/2/03 $1000.00 $100.00 $50.00
789012 (Effective
May 23, 2007 this
number will be
f
or CMS use only.
FIs are required
to use the
providers NPI.)
2233445566
Lmnopqrstu xxx 67890 10/30/0
2
$5378.22 $537.82 $268.91
Use the information in the Professional Component/Technical Component (PC/TC)
indicator field of the CORF extract of the Medicare Physician Fee Schedule
Supplementary File to identify professional services eligible for HPSA and physician
scarcity bonus payments. The following are the rules to apply in determining whether to
pay the bonus on services furnished within a geographic HPSA billed with a QB or QU
modifier for dates of service prior to January 01, 2006 or the AQ modifier for services on
or after January 01, 2006, and/or whether to pay the bonus on services furnished within a
Physician Scarcity Area with the AR modifier effective for dates of service on or after
January 01, 2005.
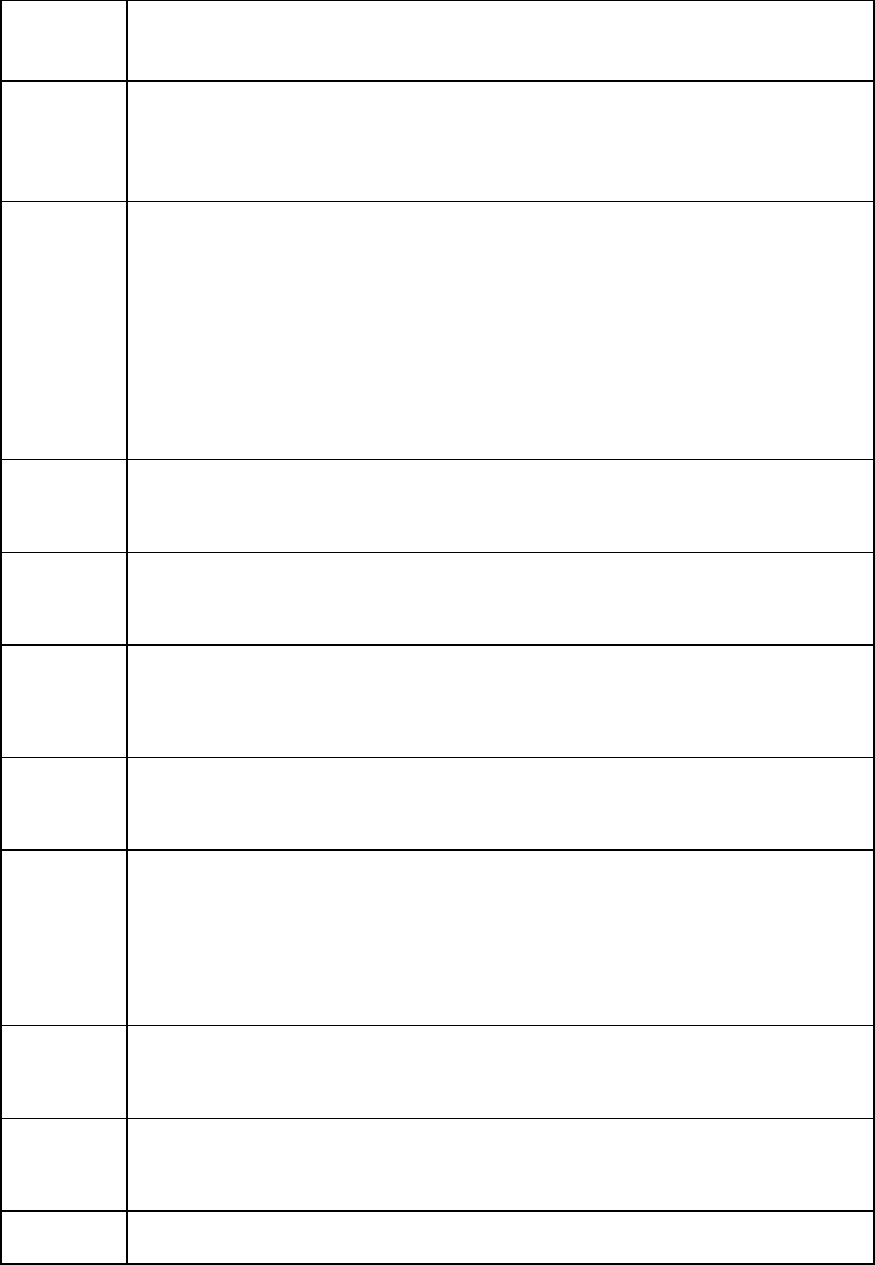
(Field 20 on the full MPFS file layout)
PC/TC
Indicator
Bonus Payment Policy
0 Physician services. The concept of PC/TC does not apply since physician
services cannot be split into professional and technical components.
ACTION: Pay the bonus
1 Globally billed. Only the professional component of this service qualifies
for the bonus payment. The bonus cannot be paid on the technical
component of globally billed services.
ACTION: Return the service as unprocessable and notify the CAH that the
professional component must be re-billed if it is performed within a
qualifying bonus area. If the technical component is the only component
of the service that was performed in the bonus area, there wouldn’t be a
qualifying service.
1 Professional Component (modifier 26).
ACTION: Pay the bonus.
1 Technical Component (modifier TC).
ACTION: Do not pay the bonus.
2 Professional Component only.
ACTION: Pay the bonus.
3 Technical Component only.
ACTION: Do not pay the bonus.
4 Global test only. Only the professional component of this service qualifies
for the bonus payment.
ACTION: Return the service as unprocessable. Instruct the provider to re-
bill the service as separate professional and technical component procedure
codes.
5 Incident to codes.
ACTION: Do not pay the bonus.
6 Laboratory physician interpretation codes.
ACTION: Pay the bonus
7 Physical therapy service.

PC/TC
Indicator
Bonus Payment Policy
ACTION: Do not pay the bonus.
8 Physician interpretation codes.
ACTOIN: Pay the bonus.
9 Concept of PC/TC does not apply.
ACTION: Do not pay the bonus.
NOTE: Codes that have a status of “X” on the CORF extract Medicare Physician Fee
Schedule Database (MFSDB) have been assigned PC/TC indicator 9 and are not
considered physician services for MFSDB payment purposes. Therefore, neither the
HPSA bonus nor the physician bonus payment (5 percent) will be paid for these codes.

260.1 - Special Partial Hospitalization Billing Requirements for
Hospitals, Community Mental Health Centers, and Critical Access
Hospitals
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
Medicare Part B coverage is available for hospital outpatient partial hospitalization
services.
A. Billing Requirement
Section
1861 of the Act defines the services under the partial hospitalization benefit in a
hospital.
Section
1866(e)(2) of the Act recognizes CMHCs as “providers of services” but only for
furnishing partial hospitalization services. See
§261.1.1 for CMHC partial
hospitalization bill review directions.
Hospitals and CAHs report condition code 41 in FLs 24-30 (or electronic equivalent) to
indicate the claim is for partial hospitalization services. They must also report a revenue
code and the charge for each individual covered service furnished. In addition, hospital
outpatient departments are required to report HCPCS codes. CAHs are not required to
HCPCS code for this benefit.
Under component billing, hospitals are required to report a revenue code and the charge
for each individual covered service furnished under a partial hospitalization program. In
addition, hospital outpatient departments are required to report HCPCS codes.
Component billing assures that only those partial hospitalization services covered under
§1861(ff) of the Act are paid by the Medicare program.
All hospitals are required to report condition code 41 in FLs 24-30 to indicate the claim is
for partial hospitalization services. Hospitals use bill type 13X and CAHs use bill type
85X. The following special procedures apply.
Bills must contain an acceptable revenue code. They are as follows:
Revenue Code Description
0250 Drugs and Biologicals
043X Occupational Therapy
0900 Behavioral Health Treatment/Services
0904 Activity Therapy
0910 Psychiatric/Psychological Services (Dates of Service prior to
October 16, 2003)
0914 Individual Therapy
0915 Group Therapy
Revenue Code Description
0916 Family Therapy
0918 Testing
0942 Education Training
Hospitals other than CAHs are also required to report appropriate HCPCS codes as
follows:
Revenue Code Description HCPCS Code
043X Occupational Therapy *G0129
0900 Behavioral Health Treatment/Services 90801, 90802, 90899
0904 Activity Therapy (Partial
Hospitalization)
**G0176
0910 Psychiatric General Services (Dates
of Service prior to October 16, 2003)
90801, 90802, 90899
0914 Individual Psychotherapy 90816, 90817, 90818,
90819, 90821, 90822,
90823, 90824, 90826,
90827, 90828, or 90829
0915 Group Therapy 90849, 90853, or 90857
0916 Family Psychotherapy 90846, 90847, or 90849
0918 Psychiatric Testing 96100, 96115 or 96117
0942 Education Training ***G0177
The FI will edit to assure that HCPCS are present when the above revenue codes are
billed and that they are valid HCPCS codes. The FI will not edit for matching the
revenue code to HCPCS.
*The definition of code G0129 is as follows:
Occupational therapy services requiring skills of a qualified occupational
therapist, furnished as a component of a partial hospitalization treatment program,
per day,
**The definition of code G0176 is as follows:
Activity therapy, such as music, dance, art or play therapies not for recreation,
related to care and treatment of patient’s disabling mental problems, per session
(45 minutes or more).

***The definition of code G0177 is as follows:
Training and educational services related to the care and treatment of patient’s
disabling mental health problems, per session (45 minutes or more).
Codes G0129, G0176, and G0177 are used only for partial hospitalization programs.
Revenue code 250 does not require HCPCS coding. However, Medicare does not cover
drugs that can be self-administered.
Edit to assure that HCPCS are present when the above revenue codes are billed and that
they are valid HCPCS codes. Do not edit for the matching of revenue code to HCPCS.
B.
Professional Services
The professional services listed below when provided in all hospital outpatient
departments are separately covered and paid as the professional services of physicians
and other practitioners. These professional services are unbundled and these practitioners
(other than physician assistants (PA) bill the Medicare Part B carrier directly for the
professional services furnished to hospital outpatient partial hospitalization patients. The
hospital can also serve as a billing agent for these professionals by billing the Part B
carrier on their behalf under their billing number for their professional services. The
professional services of a PA can be billed to the carrier only by the PAs employer. The
following direct professional services are unbundled and not paid as partial
hospitalization services.
• Physician services that meet the criteria of 42 CFR 415.102, for payment on a fee
schedule basis;
• Physician assistant (PA) services as defined in §1861(s)(2)(K)(i) of the Act;
• Nurse practitioner and clinical nurse specialist services, as defined in
§1861(s)(2)(K)(ii) of the Act; and
• Clinical psychologist services as defined in §1861(ii) of the Act.
The services of other practitioners (including clinical social workers and occupational
therapists), are bundled when furnished to hospital patients, including partial
hospitalization patients. The hospital must bill you for such nonphysician practitioner
services as partial hospitalization services. Make payment for the services to the hospital.
PA services can only be billed by the actual employer of the PA. The employer of a PA
may be such entities or individuals such as a physician, medical group, professional
corporation, hospital, SNF, or nursing facility. For example, if a physician is the
employer of the PA and the PA renders services in the hospital, the physician and not the
hospital would be responsible for billing the carrier on Form CMS-1500 for the services
of the PA.
C.
Outpatient Mental Health Treatment Limitation
The outpatient mental health treatment limitation
may apply to services to treat mental,
psychoneurotic, and personality disorders when furnished by physicians, clinical
psychologists, NPs, CNSs, and PAs to partial hospitalization patients. However, the
outpatient mental health treatment limitation
does not apply to such mental health

treatment services billed to the intermediary by a CMHC or hospital outpatient
department as partial hospitalization services.
D. Reporting of Service Units
Hospitals report number of times the service or procedure, as defined by the HCPCS
code, was performed. CAHs report the number of times the revenue code visit was
performed.
You must RTP claims that contain more than one unit for HCPCS codes G0129 per day.
NOTE: Service units are not required to be reported for drugs and biologicals (Revenue
Code 250).
E.
Line Item Date of Service Reporting
Hospitals other than CAHs are required to report line item dates of service per revenue
code line for partial hospitalization claims. This means each service (revenue code)
provided must be repeated on a separate line item along with the specific date the service
was provided for every occurrence. Line item dates of service are reported in FL 45
“Service Date” (MMDDYY). See
§260.5 for a detailed explanation.
F.
Payment
Beginning with services provided on or after August 1, 2000, for hospital outpatient
departments, make payment under the hospital outpatient prospective payment system for
partial hospitalization services.
Apply Part B deductible, if any, and coinsurance.
G.
Data for CWF and PS&R
Include revenue codes, HCPCS/CPT codes, units, and covered charges in the financial
data section (fields 65a - 65j), as appropriate. Report the billed charges in field 65h,
"Charges," of the CWF record.
Include in the financial data portion of the PS&R UNIBILL, revenue codes, HCPCS/CPT
codes, units, and charges, as appropriate.
260.1.1 - Bill Review for Partial Hospitalization Services Provided in
Community Mental Health Centers (CMHC)
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
A General
Medicare Part B coverage for partial hospitalization services provided by CMHCs is
available effective for services provided on or after October 1, 1991.
B Special Requirements
Section
1866(e)(2) of the Act recognizes CMHCs as “providers of services” but only for
furnishing partial hospitalization services.
C Billing Requirements
The CMHCs bill for partial hospitalization services on Form CMS-1450 or electronic
equivalent under bill type 76X. The FIs follow bill review instructions in Chapter 25
except for those listed below.
The acceptable revenue codes are as follows:
Code Description
0250 Drugs and Biologicals
043X Occupational Therapy
0900 Behavioral Health Treatments/Services
0904 Activity Therapy
0910 Psychiatric/Psychological Services (Dates of Service prior to
October 16, 2003)
0914 Individual Therapy
0915 Group Therapy
0916 Family Therapy
0918 Testing
0942 Education Training
The CMHCs are also required to report appropriate HCPCS codes as follows:
Revenue Codes Description HCPCS Code
043X Occupational Therapy
(Partial Hospitalization)
*G0129
0900 Behavioral Health
Treatments/Services
90801, 90802, 90899
0904 Activity Therapy (Partial
Hospitalization)
**G0176
0910 Psychiatric General Services
(Dates of Service prior to
October 16, 2003)
90801, 90802, 90899
Revenue Codes Description HCPCS Code
0914 Individual Psychotherapy 90816, 90817, 90818, 90819, 90821,
90822, 90823, 90824, 90826, 90827,
90828, or 90829
0915 Group Psychotherapy 90849, 90853, or 90857
0916 Family Psychotherapy 90846, 90847, or 90849
0918 Psychiatric Testing 96100, 96115, or 96117
0942 Education Training ***G0177
FIs edit to assure that HCPCS are present when the above revenue codes are billed and
that they are valid HCPCS codes. They do not edit for the matching of revenue codes to
HCPCS.
*The definition of code G0129 is as follows:
Occupational therapy services requiring the skills of a qualified occupational
therapist, furnished as a component of a partial hospitalization treatment program,
per day.
**The definition of code G0176 is as follows:
Activity therapy, such as music, dance, art or play therapies not for recreation,
related to the care and treatment of patient’s disabling mental health problems, per
session (45 minutes or more).
***The definition of code G0177 is as follows:
Training and educational services related to the care and treatment of patient’s
disabling mental health problems, per session (45 minutes or more).
Codes G0129, G0176, and G0177 are used only for partial hospitalization programs.
Revenue code 0250 does not require HCPCS coding. However, drugs that can be self-
administered are not covered by Medicare.
HCPCS includes CPT-4 codes. CMHCs report HCPCS codes in FL44, “HCPCS/Rates.”
HCPCS code reporting is effective for claims with dates of service on or after April 1,
2000.
FIs are to advise their CMHCs of these requirements. CMHCs should complete the
remaining items on Form CMS-1450 in accordance with the bill completion instructions
in Chapter 25.
The professional services listed below are separately covered and are paid as the
professional services of physicians and other practitioners. These professional services
are unbundled and these practitioners (other than physician assistants (PAs)) bill the
Medicare Part B carrier directly for the professional services furnished to CMHC partial
hospitalization patients. The CMHC can also serve as a billing agent for these

professionals by billing the Part B carrier on their behalf for their professional services.
The professional services of a PA can be billed to the carrier only by the PAs employer.
The following professional services are unbundled and not paid as partial hospitalization
services:
• Physician services that meet the criteria of 42 CFR 415.102, for payment on a fee
schedule basis;
• PA services, as defined in §1861(s)(2)(K)(i) of the Act;
• Nurse practitioner and clinical nurse specialist services, as defined in
§1861(s)(2)(K)(ii) of the Act; and,
• Clinical psychologist services, as defined in §1861(ii) of the Act.
The services of other practitioners (including clinical social workers and occupational
therapists) are bundled when furnished to CMHC patients. The CMHC must bill the FI
for such nonphysician practitioner services as partial hospitalization services. The FI
makes payment for the services to the CMHC.
The PA services can be billed only by the actual employer of the PA. The employer of a
PA may be such entities or individuals as a physician, medical group, professional
corporation, hospital, SNF, or nursing facility. For example, if a physician is the
employer of the PA and the PA renders services in the CMHC, the physician and not the
CMHC would be responsible for billing the carrier on Form CMS-1500 for the services
of the PA.
D Outpatient Mental Health Treatment Limitation
The outpatient mental health treatment limitation may apply to services to treat mental,
psychoneurotic, and personality disorders when furnished by physicians, clinical
psychologists, NPs, CNSs, and PAs to partial hospitalization patients. However, the
outpatient mental health treatment limitation does not apply to such mental health
treatment services billed to the FI as partial hospitalization services.
E Reporting of Service Units
Visits should no longer be reported as units. Instead, CMHCs report in Form Locator
(FL) 46, “Service Units,” the number of times the service or procedure, as defined by the
HCPCS code, was performed when billing for partial hospitalization services identified
by revenue code in subsection C.
EXAMPLE
A beneficiary received psychological testing (HCPCS code 96100, which is defined in 1
hour intervals) for a total of 3 hours during 1 day. The CMHC reports revenue code 0918
in FL 42, HCPCS code 96100 in FL 44, and “3” units in FL 46.
When reporting service units for HCPCS codes where the definition of the procedure
does not include any reference to time (either minutes, hours or days), CMHCs should
not bill for sessions of less than 45 minutes.
The FI returns to the provider claims that contain more than one unit for HCPCS code
G0129 or that does not contain service units for a given HCPCS code.

NOTE: The CMHC need not report service units for drugs and biologicals (Revenue
Code 0250)
F Line Item Date of Service Reporting
Dates of service per revenue code line for partial hospitalization claims that span two or
more dates. This means each service (revenue code) provided must be repeated on a
separate line item along with the specific date the service was provided for every
occurrence. Line item dates of service are reported in FL 45 “Service Date”
(MMDDYY). See examples below of reporting line item dates of service. These
examples are for group therapy services provided twice during a billing period.
For the UB-92 flat file as well as the HIPAA 837, FIs report as follows:
Record
Type
Revenue
Code
HCPCS Dates of
Service
Units Total
Charges
61 0915 90849 19980505 1 $80
61 0915 90849 19980529 2 $160
For the hardcopy UB-92 (Form CMS-1450), FIs report as follows:
FL 42 FL 44 FL 45 FL 46 FL 47
0915 90849 050598 1 $80
0915 90849 052998 2 $160
For the Medicare A 837 Health Care Claim version 3051 implementations 3A.01 and
1A.C1, FIs report as follows:
LX*1~
SV2*0915*HC:90849*80*UN*1~
DTP*472*D8*19980505~
LX*2~
SV2*0915*HC:90849*160*UN*2~
DTP*472*D8*19980529~
The FIs return to provider claims that span two or more dates if a line item date of service
is not entered for each HCPCS code reported or if the line item dates of service reported
are outside of the statement covers period. Line item date of service reporting is effective
for claims with dates of service on or after June 05, 2000.
G Payment
Section
1833(a)(2)(B) of the Act provides the statutory authority governing payment for
partial hospitalization services provided by a CMHC. FIs made payment on a reasonable
cost basis until OPPS was implemented. The Part B deductible and coinsurance applied.
Payment principles applicable to partial hospitalization services furnished in CMHCs are
contained in §2400 of the Medicare Provider Reimbursement Manual. FIs are to furnish
each CMHC with one copy of that manual.
The FIs make payment on a per diem basis under the hospital outpatient prospective
payment system for partial hospitalization services. CMHCs must continue to maintain
documentation to support medical necessity of each service provided, including the
beginning and ending time.
NOTE: Occupational therapy services provided to partial hospitalization patients are not
subject to the prospective payment system for outpatient rehabilitation services, and
therefore the financial limitation required under §4541 of the Balanced Budget Act
(BBA) does not apply.
H Medical Review
The FIs follow medical review guidelines in Pub. 100-08, Medicare Program Integrity
Manual.
I Coordination With CWF
See Chapter 27.

10 - Part B Outpatient Rehabilitation and Comprehensive Outpatient
Rehabilitation Facility (CORF) Services - General
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
Section 4541(a)(2) of the Balanced Budget Act (BBA) (P.L. 105-33), which added
§1834(k)(5) to the Social Security Act (the Act), required that all claims for outpatient
rehabilitation, certain audiology services and comprehensive outpatient rehabilitation
facility (CORF) services, be reported using a uniform coding system. The CMS chose
HCPCS (Healthcare Common Procedure Coding System) as the coding system to be used
for the reporting of these services. This coding requirement is effective for all claims for
outpatient rehabilitation services including certain audiology services and CORF services
submitted on or after April 1, 1998.
The BBA also required payment under a prospective payment system for outpatient
rehabilitation services including audiology and CORF services. Effective for claims with
dates of service on or after January 1, 1999, the Medicare Physician Fee Schedule
(MPFS) became the method of payment for outpatient physical therapy (which includes
outpatient speech-language pathology) services furnished by:
• Comprehensive Outpatient Rehabilitation Facilities (CORFs);
• Outpatient Physical Therapy Providers (OPTs);
• Other Rehabilitation Facilities (ORFs);
• Hospitals (to outpatients and inpatients who are not in a covered Part A stay);
• Skilled Nursing Facilities (SNFs) (to residents not in a covered Part A stay and to
nonresidents who receive outpatient rehabilitation services from the SNF); and
• Home Health Agencies (HHAs) (to individuals who are not homebound or
otherwise are not receiving services under a home health plan of care (POC)).
The MPFS is used as a method of payment for outpatient rehabilitation services furnished
under arrangement with any of these providers.
In addition, the MPFS is used as the payment system for audiology and CORF services
identified by the HCPCS codes in §20 Assignment is mandatory.
The Medicare allowed charge for the services is the lower of the actual charge or the
MPFS amount. The Medicare payment for the services is 80 percent of the allowed
charge after the Part B deductible is met. Coinsurance is made at 20 percent of the lower
of the actual charge or the MPFS amount. The general coinsurance rule (20 percent of
the actual charges) does not apply when making payment under the MPFS. This is a final
payment.
The MPFS does not apply to outpatient rehabilitation services furnished by critical access
hospitals (CAHs). CAHs are to be paid on a reasonable cost basis.
Fiscal Intermediaries (FIs) process outpatient rehabilitation claims from hospitals,
including CAHs, SNFs, CORFs, outpatient rehabilitation agencies, and outpatient
physical therapy providers for which they have received a tie in notice from the RO.
Carriers process claims from physicians, certain nonphysician practitioners (NPPs), and
physical and occupational therapists in private practice (PTPPs and OTPPs). A
physician-directed clinic that bills for services furnished incident to a physician’s service
(see Chapter 15 in Pub. 100-02, Medicare Benefit Policy Manual for a definition of
“incident to”) bills the carrier.
There are different fee rates for nonfacility and facility services. Chapter 23 describes the
differences in these two rates. (See fields 28 and 29 of the record therein described).
Facility rates apply to professional services performed in a facility other than the
professional’s office. Nonfacility rates apply when the service is performed in the
professional’s office. The nonfacility rate (that is paid when the provider performs the
services in its own facility) accommodates overhead and indirect expenses the provider
incurs by operating its own facility. Thus it is somewhat higher than the facility rate.
FIs pay the nonfacility rate for services performed in the provider’s facility. Carriers may
pay the facility or nonfacility rate depending upon where the service is performed (place
of service on the claim), and the provider specialty.
Carriers pay the codes in §20 under the MPFS regardless of whether they may be
considered rehabilitation services. However, FIs must use this list to determine whether
to pay under outpatient rehabilitation rules or whether payment rules for other types of
service may apply, e.g., OPPS for hospitals, reasonable costs for CAHs.
Note that because a service is considered an outpatient rehabilitation service does not
automatically imply payment for that service. Additional criteria, including coverage,
plan of care and physician certification must also be met. These criteria are described in
Pub. 100-02, Medicare Benefit Policy Manual, Chapters 1 and 15.
Payment for rehabilitation services provided to Part A inpatients of hospitals or SNFs is
included in the respective PPS rate. Also, for SNFs (but not hospitals), if the beneficiary
has Part B, but not Part A coverage (e.g., Part A benefits are exhausted), the SNF must
bill the FI for any rehabilitation service (except audiologic function services).
Independent audiologists may bill the carrier directly for services rendered to Part B
Medicare entitled beneficiaries residing in a SNF, but not in a SNF Part A covered stay.
Payment is made based on the MPFS, whether by the carrier or the FI. For beneficiaries
not in a covered Part A SNF stay, who are sometimes referred to as beneficiaries in a Part
B SNF stay, audiologic function tests are payable under Part B when billed by the SNF as
type of bill 22X, or when billed directly to the carrier by the provider or supplier of the
service. For tests that include both a professional component and technical component,
the SNF may elect to bill the technical component to the FI, but is not required to bill the
service. (The professional component of a service is the direct patient care provided by
the physician or audiologist, e.g., the interpretation of a test.)
Payment for rehabilitation services provided by home health agencies under a home
health plan of care is included in the home health PPS rate. HHAs may submit bill type
34X and be paid under the MPFS if there are no home health services billed under a
home health plan of care at the same time, and there is a valid rehabilitation POC (e.g.,
the patient is not homebound).
An institutional employer (other than a SNF) of the PTPPs, OTPPs, or physician
performing outpatient services, (e.g., hospital, CORF, etc.), or a clinic billing on behalf of
the physician or therapist may bill the carrier on Form CMS-1500.

The MPFS is the basis of payment for outpatient rehabilitation services furnished by
PTPPs and OTPPs, physicians, and certain nonphysician practitioners or for diagnostic
tests provided incident to the services of such physicians or nonphysician practitioners.
(See Pub. 100-02, Medicare Benefit Policy Manual, Chapter 15, for a definition of
“incident to.") Such services are billed to the Part B carrier. Assignment is mandatory.
The following table identifies the provider types or physician/nonphysician and to which
contractor they may submit bills.
“Provider/Service” Type Bill to Bill Type Comment
Inpatient hospital Part A FI 11X Included in PPS
Inpatient SNF Part A FI 21X Included in PPS
Inpatient hospital Part B FI 12X Hospital may obtain services
under arrangements and bill, or
rendering provider may bill.
Inpatient SNF Part B except for
audiology function tests.
FI 22X SNF must provide and bill, or
obtain under arrangements and
bill.
Inpatient SNF Part B audiology
function tests only.
FI 22X SNF may bill the FI or provider
of service may bill the carrier.
Outpatient hospital FI 13X Hospital may provide and bill
or obtain under arrangements
and bill, or rendering provider
may bill
Outpatient SNF FI 23X SNF must provide and bill or
obtain under arrangements and
bill
HHA billing for services
rendered under a Part A or Part
B home health plan of care.
FI 32X Service is included in PPS rate.
CMS determines whether
payment is from Part A or Part
B trust fund.
HHA billing for services not
rendered under a Part A or Part
B home health plan of care, but
rendered under a therapy plan of
care.
FI 34X Service not under home health
plan of care.
Other Rehabilitation Facility
(ORF)
FI 74X Paid MPFS for outpatient
rehabilitation services effective
January 1, 1999, and all other

“Provider/Service” Type Bill to Bill Type Comment
services except drugs effective
July 1, 2000. Starting April 1,
2002, drugs are paid 95% of the
AWP. For claims with dates of
service on or after July 1, 2003,
drugs and biologicals do not
apply in an OPT setting.
Therefore, FIs are to advise
their OPTs not to bill for them.
Comprehensive Outpatient
Rehabilitation Facility (CORF)
FI 75X Paid MPFS for outpatient
rehabilitation services effective
January 1, 1999, and all other
services except drugs effective
July 1, 2000. Starting April 1,
2002, drugs are paid 95% of the
AWP.
Physician, NPPs, PTPPs,
OTPPs, and, for diagnostic tests
only, audiologists (service in
hospital or SNF)
Carrier See Chapter 26
for place of
service, and
type of service
coding.
Payment may not be made for
therapy services to Part A
inpatients of hospitals or SNFs,
or for Part B SNF residents.
Otherwise, carrier billing.
Note that physician/
NPP/PTPP/OTPP employee of
facility may assign benefits to
the facility, enabling the facility
to bill for physician/therapist to
carrier
Physician/NPP/PTPP/OTPP
office, independent clinic or
patient’s home
Carrier See Chapter 26
for place of
service, and
type of service
coding.
Paid via Physician fee
schedule.
Practicing audiologist for
services defined as diagnostic
tests only
Carrier See Chapter 26
for place of
service, and
type of service
coding.
Some audiologists tests
provided in hospitals are
considered other diagnostic
tests and are subject to HOPPS
instead of MPFS for outpatient
therapy fee schedule.
Critical Access Hospital -
inpatient Part A
FI 85X Rehabilitation services are paid
cost.

“Provider/Service” Type Bill to Bill Type Comment
Critical Access Hospital -
inpatient Part B
FI 85X Rehabilitation services are paid
cost.
Critical Access Hospital –
outpatient Part B
FI 85X Rehabilitation services are paid
cost.
Complete Claim form completion requirements are contained in Chapters 25 and 26.
For a list of the outpatient rehabilitation HCPCS codes see §20.
If an FI receives a claim for one of the these HCPCS codes with dates of service on or
after July 1, 2003, that does not appear on the supplemental file it currently uses to pay
the therapy claims, it contacts its local carrier to obtain the price in order to pay the claim.
When requesting the pricing data, it advises the carrier to provide it with the nonfacility
fee.
NOTE: The list of codes in §20 contains commonly utilized codes for outpatient
rehabilitation services. FIs may consider other codes for payment under the MPFS as
outpatient rehabilitation services to the extent that such codes are determined to be
medically reasonable and necessary and those that could be performed within the scope
of practice of the therapist providing the service.
10.9 – Dialysis Provider Number Series
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
There are multiple facilities that provide dialysis services to ESRD beneficiaries. To
ensure that provider data is correct, facilities are required to use a Provider Number based
on facility type issued by CMS.
The Provider Number Series for Dialysis Providers are as follows (for CMS use only,
effective May 23, 2007, providers are required to submit only their National Provider
Identifier (NPI). The dialysis provider numbers will be mapped to the NPI):
2300-2499 Chronic Renal Dialysis Facilities (Hospital – Based)
2500-2899 Non – Hospital Renal Facilities
2900-2999 Independent Special Purpose Renal Dialysis Facility
3300-3399 Children’s Hospitals (Excluded from PPS)
3500-3699 Renal Disease Treatment Centers (Hospital Satellites)
3700-3799 Hospital Based Special Purpose Renal Dialysis Facilities
All facilities should use their appropriately assigned provider numbers on the 72x type of
bill. In the event that a facility changes from one type to another, the provider number
must reflect the facility’s present provider type.
60.8 - Shared Systems Changes for Medicare Part B Drugs for ESRD
Independent Dialysis Facilities
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
Section 303 of the Medicare Prescription Drug, Improvement, and Modernization Act of
2003 (MMA) provides that the payment limits for ESRD-related drugs billed by differing
types of facilities vary depending on the site of service. For calendar year 2005, the
payment limits for Medicare Part B drugs will be updated on a quarterly basis.
Therefore, Medicare Shared Systems (FISS) must be able to accommodate at least two
payment limits for HCPCS drug codes per quarter effective for dates of service on or
after January 1, 2005.
Fiscal intermediaries (FIs) shall use the 95 percent of the Average Wholesale Price
(AWP) payment amount provided solely to pay independent dialysis facilities with type
of bill (TOB) 72X for separately billable drugs furnished to ESRD beneficiaries.
Specifically, the ESRD drug payment limit shall be used to determine payment for TOB
72X, but only for independent dialysis facilities.

10.2 - Federally Qualified Health Centers (FQHCs)
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
The statutory requirements that FQHCs must meet to qualify for the Medicare benefit are
in
§1861(aa)(4) of the Social Security Act (the Act) and are described in Pub. 100-02,
Medicare Benefit Policy Manual, Chapter 13.
FQHC services consist of services that are similar to those provided in rural health clinics
(RHC) but also include preventive primary services, as described in Pub. 100-02,
Medicare Benefit Policy Manual, Chapter 13.
An RHC cannot be concurrently approved for Medicare as both an FQHC and an RHC.
40.1 - Request for Anticipated Payment (RAP)
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
The following data elements are required to submit a request for anticipated payment
under HH PPS. Effective for dates of service on or after October 1, 2000, home health
services under a plan of care are paid based on a 60-day episode of care. Payment for
this episode is usually made in two parts. To receive the first part of the HH PPS split
payment, the HHA must submit an RAP with coding as described below.
Each RAP must be based on a current OASIS based payment group represented by a
HIPPS code. In general, an RAP and a claim will be submitted for each episode period.
Each claim, usually following an RAP and at the end of an episode, must represent the
actual utilization over the episode period. If the claim is not received 120 days after the
start date of the episode or 60 days after the paid date of the RAP (whichever is greater),
the RAP payment will be canceled automatically by Medicare claims processing systems.
The full recoupment of the RAP payment will be reflected on the next remittance advice
(RA).
If care continues with the same provider for a second episode of care, the RAP for the
second episode may be submitted even if the claim for the first episode has not yet been
submitted. If a prior episode is overpaid, the current mechanism of generating an
accounts receivable debit and deducting it on the next RA will be used to recoup the
overpaid amount.
While an RAP is not considered a claim for purposes of Medicare regulations, it is
submitted using the same formats as Medicare claims. The Social Security Act at §1862
(a)(22) requires that all claims for Medicare payment must be submitted in an electronic
form specified by the Secretary of Health and Human Services, unless an exception
described at §1862 (h) applies. The electronic form required for billing HH episodes is
the ANSI X12N 837 Institutional claim transaction. Since the data structure of the 837
transaction is difficult to express in narrative form and to provide assistance to small
providers excepted from the electronic claim requirement, the instructions below are
given relative to the UB-92 (Form CMS-1450) hardcopy form. A table to crosswalk UB-
92 form locators to the 837 transaction is found in Chapter 25, §100.
Form Locator (FL) 1. (Untitled) Provider Name, Address, and Telephone Number
Required - The minimum entry is the agency’s name, city, State, and ZIP code. The post
office box number or street name and number may be included. The State may be
abbreviated using standard post office abbreviations. Five or nine-digit ZIP codes are
acceptable. This information is used in connection with the Medicare provider number
(FL 51) to verify provider identity.
FL 2. Not required for Medicare HH RAP billing.
FL 3. Patient Control Number
Optional - The patient’s control number may be shown if the HHA assigns one and
needs it for association and reference purposes.
FL 4. TOB Required - This 3-digit alphanumeric code gives three specific pieces of
information. The first digit identifies the type of facility. The second classifies the type
of care. The third indicates the sequence of this bill in this particular episode of care. It
is referred to as a “frequency” code. The types of bill accepted for HH PPS requests for
anticipated payment are any combination of the codes listed below:
Code Structure (only codes used to bill Medicare are shown).
lst Digit-Type of Facility
3 - Home Health
2nd Digit-Bill Classification (Except Clinics and Special Facilities)
2 - Hospital Based or Inpatient (Part B) (includes HHA visits under a Part B plan of care).
NOTE: While the bill classification of “3,” defined as “Outpatient (includes HHA visits
under a Part A plan of care and use of HHA DME under a Part A plan of care)” may also
be appropriate to an HH PPS claim depending upon a beneficiary’s eligibility, Medicare
encourages HHAs to submit all RAPs with bill classification “2.” Medicare claims
processing systems determine whether an HH claim should be paid from the Part A or
Part B trust fund and will change the bill classification digit on the electronic claim
record as necessary to reflect this.
3rd Digit-Frequency Definition
2-Interim-First Claim For HHAs, used for the submission of original or
replacement RAPs.
8-Void/Cancel of a Prior Claim Used to indicate this bill is an exact duplicate of an
incorrect bill previously submitted. A code “2” bill (a
replacement RAP) must be submitted for the episode
to be paid. If an RAP is submitted in error (for
instance, an incorrect HIPPS code is submitted), this
code cancels it so that a corrected RAP can be
submitted.
RHHIs will allow only provider-submitted cancellations of RAPs and claims to process
as adjustments against original RAPs. Provider may not adjust RAPs.
FL 5. Not required for Medicare HH RAP billing.
FL 6. Statement Covers Period (From-Through)
Required - Typically, these fields show the beginning and ending dates of the period
covered by a bill. Since the RAP is a request for payment for future services, however,
the ending date may not be known. The RAP contains the same date in both the “from”
and “through” date fields. On the first RAP in an admission, this date should be the date
the first service was provided to the beneficiary. On RAPs for subsequent episodes of
continuous care, this date should be the day immediately following the close of the
preceding episode (day 61, 121, etc.). All dates are in the format MM-DD-YY.
FL 7. Not required for Medicare HH RAP billing.
FL 8. Not required for Medicare HH RAP billing.
FL 9. Not required for Medicare HH RAP billing.
FL 10. Not required for Medicare HH RAP billing.
FL 11. Not required for Medicare HH RAP billing.
FL l2. Patient’s Name
Required - Patient’s last name, first name, and middle initial.
FL l3 Patient’s Address
Required - Patient’s full mailing address, including street number and name, post office
box number or RFD, City, State, and ZIP code.
FL 14. Patient’s Birthdate
Required - Month, day, and year of birth (MM-DD-YY) of patient.
Left blank if the full correct date is not known.
FL l5. Patient’s Sex
Required - “M” for male or “F” for female must be present. This item is used in
conjunction with FLS 67-81 (diagnoses and surgical procedures) to identify
inconsistencies.
FL 16. Not required for Medicare HH RAP billing.
FL l7. Admission Date
Required - Date the patient was admitted to home health care (MM-DD-YY). On the
first RAP in an admission, this date should match the statement covers “from” date in FL
6. On RAPs for subsequent episodes of continuous care, this date should remain
constant, showing the actual date the beneficiary was admitted to home health care. The
date on RAPs for subsequent episodes should, therefore, match the date submitted on the
first RAP in the admission.
FL 18. Not required for Medicare HH RAP billing.
FL 19. Not required for Medicare HH RAP billing.
FL 20. Source of Admission
Required - Indicates the source of this admission. Source of admission information will
be used by Medicare to correctly establish and track home health episodes.
Code Structure:
Code Definition
1 Physician Referral
2 Clinic Referral
3 HMO Referral
4 Transfer from a Hospital
5 Transfer from a SNF
6 Transfer from Another Health Care Facility
7 Emergency Room
8 Court/Law Enforcement
9 Information Not Available
A Transfer from a Critical Access Hospital (CAH)
B Transfer from Another HHA
C Readmission to Same HHA
On the first RAP in an admission, this code reflects the actual source of admission. On
RAPs for subsequent episodes of continuous care, the HHA reports code 1, physician
referral, since the beneficiary is not a new admission but continues to receive services
under a physician’s plan of care.
FL 21. Not required for Medicare HH RAP billing.
FL 22. Patient Status
Required - Indicates the patient’s status as of the “through” date of the billing period (FL
6). Since the “through” date of the RAP will match the “from” date, the patient will
never be discharged as of the “through” date. As a result only one patient status is
possible on RAPs.
Code structure
Code Definition
30 Still patient or expected to return for outpatient services
FL 23. Medical Record Number
Optional - This is the number assigned to the patient’s medical/health record. The RHHI
must carry information entered in this field through their system and return it to the biller.
FLs 24 - 30. Condition Codes
Conditional. The HHA enters any NUBC approved code to describe conditions that
apply to the RAP.
If canceling the RAP (TOB 3X8), the agency reports one of the following:
Claim Change Reasons
Code Title Definition
D5 Cancel to Correct HICN or
Provider ID
Cancel only to correct an HICN or Provider
Identification Number.
D6
Cancel Only to Repay a
Duplicate or OIG Overpayment
Cancel only to repay a duplicate payment or
OIG overpayment. Use when D5 is not
appropriate.
Enter “Remarks” in FL 84, indicating the reason for cancellation.
For a complete list of Condition codes, see Chapter 25.
FL 31. Not required for Medicare HH RAP billing.
FL 32, 33, 34, and 35. Occurrence Codes and Dates
Optional - Enter any NUBC approved code to describe occurrences that apply to the
RAP. Event codes are two alphanumeric digits, and dates are shown as eight numeric
digits (MM-DD-YY).
Fields 32A-35A must be completed before fields 32B-35B are used.
FL 35 contains the same occurrence span code as the code in FL 34, and the occurrence
span “through” date is in the date field.
Other codes may be required by other payers, and while they are not used by Medicare,
they may be entered on the RAP.
For a complete list of Occurrence Codes, see Chapter 25.
FL 36. Occurrence Span Code and Dates
Not Required - Since the statement covers period (FL 6) of the RAP is a single day,
occurrence spans cannot be reported.
FL 37. Internal Control Number (ICN)/ Document Control Number (DCN)
Required - If canceling an RAP, HHAs must enter the control number (ICN or DCN)
that the FI assigned to the original RAP here (reported on the remittance record).
ICN/DCN is not required in any other case. Show payer A’s ICN/DCN on line “A” in FL
37. Similarly, HHAs show the ICN/DCN for Payer’s B and C on lines B and C
respectively, in FL 37.
FL 38. Not required for Medicare HH RAP billing.
FLs 39-41. Value Codes and Amounts
Required - Home health episode payments must be based upon the site at which the
beneficiary is served. RAPs will not be processed without the following value code:
Code Title Definition
61 Location Where Service is
Furnished (HHA and Hospice)
MSA number (or rural state code) of the
location where the home health or hospice
service is delivered. The HHA reports the
number in dollar portion of the form locator
right justified to the left of the dollar/cents
delimiter, add two zeros to the cents field if
no cents.
A description of the MSA system and codes can be found at the following Web site:
http://www.census.gov/population/estimates/metro-city/a99mfips.txt
Optional - Any NUBC approved Value code to describe other values that apply to the
RAP. Value code(s) and related dollar amount(s) identify data of a monetary nature
necessary for the processing of this claim. The codes are two alphanumeric digits, and
each value allows up to nine numeric digits (0000000.00). Negative amounts are not
allowed except in FL 41. Whole numbers or nondollar amounts are right justified to the
left of the dollars and cents delimiter. Some values are reported as cents, so the biller
must refer to specific codes for instructions.
If more than one value code is shown for a billing period, codes are shown in ascending
numeric sequence. There are two lines of data, line “a” and line “b.” FLs 39a through
41a must be used before FLs 39b through 41b (i.e., the first line is used before the second
line).
For a complete list of value codes, see Chapter 25.
FL 42 and 43 Revenue Code and Revenue Description
Required - One revenue code line is required on the RAP. This line will be used to
report a single Health HIPPS code (defined below) that will be the basis of the
anticipated payment. The required revenue code and description for HH PPS RAPs
follows:
Revenue
Code.
Description
0023 Home Health Services
The 0023 code is not submitted with a charge amount.
Optional - HHAs may submit additional revenue code lines at their option, reporting any
revenue codes which are accepted on HH PPS claims (
see §40.2) except another 0023.
Purposes for doing so include the requirements of the other payers, or billing software
limitations that require a charge on all requests for payment.
NOTE: Revenue codes 058X and 059X are not accepted with covered charges on
Medicare home health RAPs under HH PPS. Revenue code 0624 (investigational
devices) is not accepted at all on Medicare home health RAPs under HH PPS.
HHAs may report a “Total” line, with revenue code 0001, in FL 42. The adjacent
charges entry in FL 47 may be the sum of the charges billed. However, Medicare claims
processing systems will overlay this amount with the total payment for the RAP.
FL 44. HCPCS/Rates
Required - On the 0023 revenue code line, the HHA reports the HIPPS code for which
anticipated payment is being requested.
Optional - If additional revenue code lines are submitted on the RAP, HHAs must report
HCPCS codes as appropriate to that revenue code. Coding detail for each revenue code
under HH PPS is defined in
§40.2.
FL 45. Service Date
Required - On the 0023 revenue code line, the HHA reports the date of the first billable
service provided under the HIPPS code reported on that line.
Optional - If additional revenue codes are submitted on the RAP, the HHA reports
service dates as appropriate to that revenue code. Coding detail for each revenue code
under HH PPS is defined in
§40.2.
FL 46. Units of Service
Optional - Units of service are not required on the 0023 revenue code line. If additional
revenue codes are submitted on the RAP, the HHA reports units of service as appropriate
to that revenue code. Coding detail for each revenue code under HH PPS is defined in
§40.2.
FL 47. Total Charges
Required - Zero charges must be reported on the 0023 revenue code line. Medicare
claims processing systems will place the payment amount for the RAP in this field on the
electronic claim record.
Optional - If additional revenue codes are submitted on the RAP, the HHA reports any
necessary charge amounts to meet the requirements of other payers or its billing software.
Medicare claims processing systems will not make any payments based upon submitted
charge amounts.
FL 48. Noncovered Charges
Not Required - The HHA does not report noncovered charges for Medicare on RAPs.
FL 49. Not required for Medicare HH RAP billing.
FLs 50A, B, and C. Payer Identification
Required - See Chapter 25.
Medicare does not make Secondary Payer payments on RAPs. This includes conditional
payments.
FL 51. Medicare Provider Number
Required - The HHA enters the six position alphanumeric “number” assigned by
Medicare (for CMS use only, effective May 23, 2007, providers are required to submit
only their NPI). It must be entered on the same line (A, B, or C) as “Medicare” in FL 50.
If a Medicare provider number changes within a 60-day episode, reflect this by closing
out the original episode with a claim under the original provider number, indicating
patient status 06. This claim will be paid a PEP adjustment. Submit a new RAP under
the new provider number to open a new episode under the new provider number. In such
cases report the new provider number in this field.
FLs 52A, B, and C. Release of Information Certification Indicator
Required - A “Y” code indicates the provider has on file a signed statement permitting
the provider to release data to other organizations in order to adjudicate the claim. An
“R” code indicates the release is limited or restricted. An “N” code indicates no release
on file.
FL 53. Not required for Medicare HH RAP billing.
FL 54. Not required for Medicare HH RAP billing.
FL 55. Not required for Medicare HH RAP billing.
FL 56. Not required for Medicare HH RAP billing.
FL 57. Not required for Medicare HH RAP billing.
FLs 58A, B, and C. Insured’s Name
Required - On the same lettered line (A, B, or C) that corresponds to the line on which
Medicare payer information is shown in FLs 50-54, record the patient’s name as shown
on the patient’s HI card or other Medicare notice.
FLs 59A, B,and C. Patient’s Relationship to insured, Not required for Medicare HH
RAP billing
FLs 60A, B, and C. Certificate/Social Security Number/HI Claim/Identification
Number Required.
See Chapter 25.
FL 61. Not required for Medicare HH RAP billing.
FL 62. Not required for Medicare HH RAP billing.
FL 63. Treatment Authorization Code
Required - The HHA enters the claim-OASIS matching key output by the Grouper
software. This data element links the RAP record to the specific OASIS assessment used
to produce the HIPPS code reported in FL 44. This is an eighteen-position code,
containing the start of care date (eight positions, from OASIS item M0030), the date the
assessment was completed (eight positions, from OASIS item M0090), and the reason for
assessment (two positions, from OASIS item M0100).
The elements in this code must be reproduced exactly as they appear on the OASIS
assessment, matching date formats used on the assessment. In cases of billing for denial
notice, using condition code 21, this code may be filled with eighteen ones.
The investigational device (IDE) revenue code, 0624, is not allowed on HH PPS claims.
Therefore, treatment authorization codes associated with IDE items must never be
submitted in this field.
FL 64. Not required for Medicare HH RAP billing.
FL 65. Not required for Medicare HH RAP billing.
FL 66. Not required for Medicare HH RAP billing.
FL 67. Principal Diagnosis Code
Required - The HHA enters the ICD-9-CM code for the principal diagnosis. The code
must be reported according to Official ICD-9-CM Guidelines for Coding and Reporting,
as required by the Health Insurance Portability and Accountability Act (HIPAA). The
code must be the full ICD-9-CM diagnosis code, including all five digits where
applicable. Where the proper code has fewer than five digits, the HHA does not fill it
with zeros.
The ICD-9 code and principle diagnosis reported in FL67 must match the primary
diagnosis code reported on the OASIS form item M0230 (Primary Diagnosis).
FLs 68-75. Other Diagnoses Codes
Required - The HHA enters the full ICD-9-CM codes for up to eight additional
conditions if they coexisted at the time of the establishment of the plan of care. None of
these other diagnoses may duplicate the principal diagnosis listed in FL 67 as an
additional or secondary diagnosis.
For other diagnoses, the diagnoses and ICD-9 codes reported in FLs 68-75 must match
the additional diagnoses reported on the OASIS, form item M0240 (Other Diagnoses). In
listing the diagnoses, the HHA places them in order to best reflect the seriousness of the
patient’s condition and to justify the disciplines and services provided in accordance with
the Official ICD-9-CM Guidelines for Coding and Reporting. The sequence of codes
should follow ICD-9 guidelines for reporting manifestation codes. Therefore, if a
manifestation code is part of the primary diagnosis, the first two diagnoses should match
and appear in the same sequence on both forms. Medicare does not have any additional
requirements regarding the reporting or sequence of the codes beyond those contained in
ICD-9 guidelines.
OASIS form items M0245a and M0245b, Payment Diagnosis, are not directly reported in
any field of the claim form. If under ICD-9 coding guidelines the codes reported in these
OASIS items must be reported as Other Diagnoses, the codes may be repeated in OASIS
form item M0240 and will be reported in FLs 68-75. In other circumstances, the codes
reported in M0245a and M0245b may not appear on the claim form at all.
FL 76. Not required for Medicare HH RAP billing.
FL 77. Not required for Medicare HH RAP billing.
FL 78. Not required for Medicare HH RAP billing.
FL 79. Not required for Medicare HH RAP billing.
FL 80. Not required for Medicare HH RAP billing.
FL 81. Not required for Medicare HH RAP billing.
FL 82. Attending/Requesting Physician I.D.
Required - The HHA enters the UPIN and name of the attending physician that has
established the plan of care with verbal orders.
FL 83. Not required for Medicare HH RAP billing.
FL 84. Remarks
Required - Remarks are necessary when canceling an RAP, to indicate the reason for the
cancellation.
FL 85. Not required for Medicare HH RAP billing.
FL 86. Not required for Medicare HH RAP billing.
40.2 - HH PPS Claims
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
The following data elements are required to submit a claim under home health PPS. For
billing of home health claims not under an HH plan of care (not under HH PPS), see
§90.
Effective for dates of service on or after October 1, 2000, home health services under a
plan of care will be paid based on a 60-day episode of care. Payment for this episode will
usually be made in two parts. After an RAP has been paid and a 60-day episode has been
completed, or the patient has been discharged, the HHA submits a claim to receive the
balance of payment due for the episode.
HH PPS claims will be processed in Medicare claims processing systems as debit/credit
adjustments against the record created by the RAP, except in the case of “No-RAP”
LUPA claims (see
§40.3). As the claim is processed the payment on the RAP will be
reversed in full and the full payment due for the episode will be made on the claim. Both
the debit and credit actions will be reflected on the remittance advice (RA) so the net
payment on the claim can be easily understood. Detailed RA information is contained in
Chapter 22.
The Social Security Act at §1862 (a)(22) requires that all claims for Medicare payment
must be submitted in an electronic form specified by the Secretary of Health and Human
Services, unless an exception described at §1862 (h) applies. The electronic form
required for billing HH episodes is the ANSI X12N 837 Institutional claim transaction.
Since the data structure of the 837 transaction is difficult to express in narrative form and
to provide assistance to small providers excepted from the electronic claim requirement,
the instructions below are given relative to the UB-92 (Form CMS-1450) hardcopy form.
A table to crosswalk UB-92 form locators to the 837 transaction is found in Chapter 25,
§100.
FL 1. (Untitled) Provider Name, Address, and Telephone Number
Required - The minimum entry is the agency’s name, city, State, and ZIP code. The post
office box number or street name and number may be included. The State may be
abbreviated using standard post office abbreviations. Five or nine-digit ZIP codes are
acceptable. Use this information in connection with the Medicare provider number (FL
51) to verify provider identity.
FL 2. Not required for Medicare HH PPS claim billing
FL 3. Patient Control Number
Required - The patient’s control number may be shown if the patient is assigned one and
the number is needed for association and reference purposes.
FL 4. TOB
Required - This 3-digit alphanumeric code gives three specific pieces of information.
The first digit identifies the type of facility. The second classifies the type of care. The
third indicates the sequence of this bill in this particular episode of care. It is referred to
as a “frequency” code. The types of bill accepted for HH PPS claims are any
combination of the codes listed below:
Code Structure (only codes used to bill Medicare are shown).
lst Digit-Type of Facility
3 - Home Health
2nd Digit-Bill Classification (Except Clinics and Special Facilities)
2 - Hospital Based or Inpatient (Part B) (includes HHA visits under a Part B plan
of treatment).
NOTE: While the bill classification of 3, defined as “Outpatient (includes HHA
visits under a Part A plan of treatment and use of HHA DME under a Part A plan
of treatment)” may also be appropriate to an HH PPS claim, Medicare encourages
HHAs to submit all claims with bill classification 2. Medicare claims system
determine whether a HH claim should be paid from the Part A or Part B trust fund
and will change the bill classification digit on the electronic claim record as
necessary to reflect this.
3rd Digit-Frequency - Definition
7 - Replacement of Prior Claim - HHAs use to correct a previously submitted bill.
Apply this code for the corrected or “new” bill. These adjustment claims must be
accepted at any point within the timely filing period after the payment of the
original claim.
8 - Void/Cancel of a Prior Claim - HHAs use this code to indicate this bill is an
exact duplicate of an incorrect bill previously submitted. A replacement RAP or
claim must be submitted for the episode to be paid.
9 - Final Claim for a HH PPS Episode - This code indicates the HH bill should be
processed as a debit/credit adjustment to the RAP. This code is specific to home
health and does not replace frequency codes 7, or 8.
HH PPS claims will be submitted with the frequency of “9.” These claims may be
adjusted with frequency “7” or cancelled with frequency “8.” FIs do not accept late
charge bills, submitted with frequency “5” on HH PPS claims. To add services within
the period of a paid HH claim, an adjustment must be submitted by the HHA.
FL 5. Not required for Medicare HH PPS claim billing.
FL 6. Statement Covers Period (From-Through)
Required - The beginning and ending dates of the period covered by this claim. The
“from” date must match the date submitted on the RAP for the episode. For continuous
care episodes, the “through” date must be 59 days after the “from” date. The patient
status code in FL 22 must be 30 in these cases. In cases where the beneficiary has been
discharged or transferred within the 60-day episode period, HHAs will report the date of
discharge in accordance with internal discharge procedures as the Through date. If a
discharge claim is submitted due to change of FI, see
FL 22 below. If the beneficiary has
died, the HHA reports the date of death in the through date. In such cases, the “through”
date field should represent the date of discharge or last billable service date. Any NUBC
approved patient status code may be used in these cases. The HHA may submit claims
for payment immediately after the claim “through” date. It is not required to hold claims
until the end of the 60-day episode unless the beneficiary continues under care.
All dates are submitted in the format MM-DD-YY.
FL 7. Not required for Medicare HH PPS claim billing.
FL 8. Not required for Medicare HH PPS claim billing.
FL 9. Not required for Medicare HH PPS claim billing.
FL 10. Not required for Medicare HH PPS claim billing.
FL 11. Not required for Medicare HH PPS claim billing.
FL 12. Patient’s Name
Required - Enter the patient’s last name, first name, and middle initial.
FL 13. Patient’s Address
Required - Enter the patient’s full mailing address, including street number and name,
post office box number or RFD, City, State, and ZIP code.
FL 14. Patient’s Birthdate
Required - Enter the month, day, and year of birth (MM-DD-YY) of patient. If the full
correct date is not known, leave blank.
FL 15. Patient’s Sex
Required - “M” for male or “F” for female must be present. This item is used in
conjunction with FLs 67-81 (diagnoses and surgical procedures) to identify
inconsistencies.
FL 16. Not required for Medicare HH PPS claim billing.
FL l7. Admission Date
Required - The HHA enters the same date of admission that was submitted on the RAP
for the episode (MM-DD-YY).
FL 18. Not required for Medicare HH PPS claim billing.
FL 19. Not required for Medicare HH PPS claim billing.
FL 20. Source of Admission
Required - Enter the same source of admission code that was submitted on the RAP for
the episode.
FL 21. Not required for Medicare HH PPS claim billing.
FL 22. Patient Status
Required - Enter the code that most accurately describes the patient’s status as of the
“Through” date of the billing period. Any applicable NUBC approved code may be used.
Code Definition
0l Discharged to home or self-care (routine charge)
02 Discharged/transferred to other short-term general hospital
03 Discharged/transferred to SNF
04 Discharged/transferred to an Intermediate Care Facility (ICF)
05 Discharged/transferred to a non-Medicare PPS children’s hospital or non-
Medicare PPS cancer hospital for inpatient care
06 Discharged/transferred to home care of organized home health service
organization, OR Discharged and readmitted to the same home health agency
within a 60-day episode period
07 Left against medical advice
20 Expired
30 Still patient or expected to return for outpatient services
43 Discharged/transferred to a Federal hospital (effective for discharges on and
after October 1, 2003)
50 Discharged/transferred to hospice - home
51 Discharged/transferred to hospice - medical facility
61 Discharged/transferred to a hospital-based Medicare approved swing bed
62 Discharged/transferred to an inpatient rehabilitation facility including distinct
part units of a hospital
63 Discharged/transferred to a long-term care hospital (LTCH)
Code Definition
64 Discharged/transferred to a nursing facility certified under Medicaid but not
certified under Medicare
65 Discharged/transferred to a psychiatric hospital or psychiatric part unit of a
hospital (effective April 1, 2004)
71 Discharged/transferred/referred to another institution for outpatient services
as specified by the discharge plan of care (deleted October 1, 2003)
72 Discharged/transferred/referred to this institution for outpatient services as
specified by the discharge plan of care (deleted October 1, 2003)
Patient status code 06 should be reported in all cases where the HHA is aware that the
episode will be paid as a partial episode payment (PEP) adjustment. These are cases in
which the agency is aware that the beneficiary has transferred to another HHA within the
60-day episode, or the agency is aware that the beneficiary was discharged with the goals
of the original plan of care met and has been readmitted within the 60-day episode.
Situations may occur in which the HHA is unaware at the time of billing the discharge
that these circumstances exist. In these situations, Medicare claims processing systems
will adjust the discharge claim automatically to reflect the PEP adjustment, changing the
patient status code on the paid claims record to 06.
In cases where an HHA is changing the intermediary to which they submit claims, the
service dates on the claims must fall within the provider’s effective dates at each
intermediary. To ensure this, RAPs for all episodes with “from” dates before the
provider’s termination date must be submitted to the intermediary the provider is leaving.
The resulting episode must be resolved by the provider submitting claims for shortened
periods, with “through” dates on or before the termination date. The provider must
indicate that these claims will be PEP adjustments by using patient status code 06.
Billing for the beneficiary is being “transferred” to the new intermediary.
In cases where the ownership of an HHA is changing which causes the Medicare
provider number to change, the service dates on the claims must fall within the effective
dates of the terminating provider number. To ensure this, RAPs for all episodes with
“from” dates before the termination date of the provider number must be resolved by the
provider submitting claims for shortened periods, with “through” dates on or before the
termination date. The provider must indicate that these claims will be PEP adjustments
by using patient status 06. Billing for the beneficiary is being “transferred” to the new
agency ownership. In changes of ownership which do not affect the Medicare provider
number, billing for episodes is also unaffected.
In cases where an HHA is aware in advance that a beneficiary will become enrolled in a
Medicare Advantage (MA) Organization as of a certain date, the provider should submit
a claim for the shortened period prior to the MA Organization enrollment date. The
claim should be coded with patient status 06. Payment responsibility for the beneficiary
is being “transferred” from Medicare fee-for-service to MA Organization, since HH PPS
applies only to Medicare fee-for-service.
If HHAs require guidance on OASIS assessment procedures in these cases, refer them to
the appropriate state OASIS education coordinator.
FL 23. Medical Record Number
Required - Enter the number assigned to the patient’s medical/health record. The RHHI
must carry it through their system and return it on the remittance record.
FLs 24 - 30. Condition Codes
Optional - Enter any NUBC approved code to describe conditions that apply to the
claim.
Claim Change Reasons
Code Definition
D0 Changes to Service Dates (From and Through dates)
D1 Changes to Charges
D2 Changes to Revenue Codes/HCPCS/HIPPS Rate Codes
D7 Change to Make Medicare the Secondary Payer
D8 Change to Make Medicare the Primary Payer
D9 Any Other Change
E0 Change in Patient Status (Use D9 if multiple changes are necessary)
20 Demand Bill (See
§50)
21 No payment bill (See Chapter 1)
If adjusting the claim to correct a HIPPS code, HHAs use condition code D2 and enter
“Remarks” in FL 84 indicating the reason for the HIPPS code change. Use D9 if
multiple changes are necessary.
Required - If canceling the claim (TOB 3x8), HHAs report the condition codes D5 or D6
and enter “Remarks” in FL 84 indicating the reason for cancellation of the claim.
Code Definition
D5 Cancel to Correct HICN or Provider ID
D6 Cancel Only to Repay a Duplicate or OIG Overpayment
For a complete list of Condition Codes see Chapter 25.
FL. 31. Not required for Medicare HH PPS claims billing
FL 32, 33, 34, and 35. Occurrence Codes and Dates
Optional - The HHA enters any NUBC approved code to describe occurrences that apply
to the claim.
See Chapter 25.
FL 36. Occurrence Span Code and Dates
Optional - The HHA enters any NUBC approved Occurrence Span code to describe
occurrences that apply to the claim. Reporting of occurrence span code 74 is not required
to show the dates of an inpatient admission during an episode.
For a complete list of Occurrence Span codes see Chapter 25.
FL 37. Internal Control Number (ICN)/ Document Control Number (DCN)
Required - If submitting an adjustment (TOB 3X7) to a previously paid HH PPS claim,
the HHA enters the control number assigned to the original HH PPS claim here. The
HHA inserts the ICN/DCN of the claim to be adjusted here. The HHA shows payer A’s
ICN/DCN on line “A” in FL 37, and shows the ICN/DCN for Payer’s B and C on lines B
and C respectively, in FL 37.
Since HH PPS claims are processed as adjustments to the RAP, Medicare claims
processing systems will match all HH PPS claims to their corresponding RAP and
populate this field on the electronic claim record automatically. Providers do not need to
submit an ICN/DCN on all HH PPS claims, only on adjustments to paid claims.
FL 38. Not required for Medicare HH PPS claim billing.
FLs 39-41. Value Codes and Amounts
Required - See
§40.1, FL 39 - 41.
For episodes in which the beneficiary’s site of service changes from one MSA to another
within the episode period, HHAs should submit the MSA code corresponding to the site
of service at the end of the episode on the claim.
NOTE: FI value codes. Providers report code 61. The FI places codes 17 and 61 - 65 on
the claim in processing. They may be visible in CMS online history and on remittances.
Code Title Definition
17 Outlier Amount The amount of any outlier payment returned by the
Pricer with this code. (Always place condition
code 61 on the claim along with this value code.)
61 Location Where Service
is Furnished (HHA and
Hospice)
HHAs report the MSA number (or rural state code)
of the location where the home health or hospice
service is delivered. The HHA reports the number
in dollar portion of the form locator right justified
to the left of the dollar/cents delimiter, add two
zeros to the cents field if no cents.
62 HH Visits - Part A The number of visits determined by Medicare to be
payable from the Part A trust fund to reflect the
shift of payments from the Part A to the Part B trust
Code Title Definition
fund as mandated by §1812a)(3) of the Social
Security Act.
63 HH Visits - Part B The number of visits determined by Medicare to be
payable from the Part B trust fund to reflect the
shift of payments from the Part A to the Part B trust
fund as mandated by §1812 (a)(3) of the Social
Security Act.
64 HH Reimbursement -
Part A
The dollar amounts determined to be associated
with the HH visits identified in a value code 62
amount. This Part A payment reflects the shift of
payments from the Part A to the Part B trust fund as
mandated by §1812 (a)(3) of the Social Security
Act.
65 HH Reimbursement -
Part B
The dollar amounts determined to be associated
with the HH visits identified in a value code 63
amount. This Part B payment reflects the shift of
payments from the Part A to the Part B trust fund as
mandated by §1812 (a)(3) of the Social Security
Act.
If information returned from the Common Working File (CWF) indicates all visits on the
claim are Part A, the FI shared system must place value codes 62 and 64 on the claim
record, showing the total visits and total PPS payment amount as the values, change the
TOB on the claim record to 33X, and send the claim to CWF with RIC code V.
If information returned from CWF indicates all visits on the claim are Part B, the shared
system must place value codes 63 and 65 on the claim record, showing the total visits and
total PPS payment amount as the values, change the TOB on the claim record to 32X, and
send the claim to CWF with RIC code W.
If information returned from CWF indicates certain visits on the claim are payable from
both Part A and Part B, the shared system must place value codes 62, 63, 64, and 65 on
the claim record. The shared system also must populate the values for code 62 and 63
based on the numbers of visits returned from CWF and prorate the total PPS
reimbursement amount based on the numbers of visits to determine the dollars amounts
to be associated with value codes 64 and 65. The shared system will not change the TOB
and will return the claim to CWF with RIC code U.
FL 42 and 43 Revenue Code and Revenue Description
Required
See Chapter 25 for explanation of the varying third digit of the revenue code represented
by “X” in this section.
Claims must report a 0023 revenue code line matching the one submitted on the RAP for
the episode. If this matching 0023 revenue code line is not found on the claim, Medicare
claims processing systems will reject the claim. If there is a change in the HIPPS code,
refer to the SCIC chart located in
§10.1.20 to determine if the HIPPS code should be
reported. In the rare instance in which a beneficiary is assessed more then once in a day,
report only one 0023 revenue code, with the HIPPS code generated by the assessment
done latest in the day.
If the claim represents an episode in which the beneficiary experienced a significant
change in condition (SCIC), the HHA reports one or more additional 0023 revenue code
lines to reflect each change. Assessments that do not change the payment group (i.e., no
new HHRG) do not have to be reported as a SCIC adjustment. SCICs are determined by
an additional OASIS assessment of the beneficiary that changes the HHRG and HIPPS
code that applies to the episode and a change order from the physician to the plan of care.
Each additional 0023 revenue code line will show in FL 44 the new HIPPS code output
from the Grouper for the additional assessment, the first date on which services were
provided under the revised plan of care in FL 45 and zero charges in FL 46. See
§40.1,
FL 44
, for more detailed information on the HIPPS code.
Unlike RAPs, claims must also report all services provided to the beneficiary within the
episode. Each service must be reported in line item detail. Each service visit (revenue
codes 042X, 043X, 044X, 055X, 056X and 057X) must be reported as a separate line.
Any of the following revenue codes may be used:
027X
(NOTE:
Revenue
Codes 0275
through 0278
are not used
for Medicare
billing on
HH PPS
types of bills)
Medical/Surgical Supplies (Also see
062X, an extension of 027X)
Required detail: With the exception of revenue code 0274 (prosthetic
and orthotic devices), only service units and a charge must be reported
with this revenue code. If also reporting revenue code 0623 to
separately identify specific wound care supplies, not just supplies for
wound care patients, ensure that the charge amounts for revenue code
0623 lines are mutually exclusive from other lines for supply revenue
codes reported on the claim. Report only nonroutine supply items in
this revenue code or in 0623. Revenue code 0274 requires an HCPCS
code, the date of service units and a charge amount.
042X Physical Therapy
Required detail: HCPCS code G0151 (services of a physical therapist
under a home health plan of care, each 15 minutes), the date of service,
service units which represent the number of 15 minute increments that
comprised the visit, and a charge amount.
043X Occupational Therapy
Required detail: HCPCS code G0152 (services of an occupational
therapist under a home health plan of care, each 15 minutes), the date of
service, service units which represent the number of 15 minute
increments that comprised the visit, and a charge amount.
044X Speech-Language Pathology
Required detail: HCPCS code G0153 (services of a speech and language
pathologist under a home health plan of care, each 15 minutes), the date
of service, service units which represent the number of 15 minute
increments that comprised the visit, and a charge amount.
055X Skilled Nursing
Required detail: HCPCS code G0154 (services of a skilled nurse under a
home health plan of care, each 15 minutes), the date of service, service
units which represent the number of 15 minute increments that
comprised the visit, and a charge amount.
056X Medical Social Services
Required detail: HCPCS code G0155 (services of a clinical social
worker under a home health plan of care, each 15 minutes), the date of
service, service units which represent the number of 15 minute
increments that comprised the visit, and a charge amount.
057X Home Health Aide (Home Health)
Required detail: HCPCS code G0156 (services of a home health aide
under a home health plan of care, each 15 minutes), the date of service,
service units which represent the number of 15 minute increments that
comprised the visit, and a charge amount.
NOTE: FIs do not accept revenue codes 058X or 059X when submitted with covered
charges on Medicare home health claims under HH PPS. They also do not accept
revenue code 0624, investigational devices, on HH claims under HH PPS.
Revenue Codes for Optional Billing of DME
Billing of Durable Medical Equipment (DME) provided in the episode is not required on
the HH PPS claim. Home health agencies retain the option to bill these services to their
RHHI or to have the services provided under arrangement with a supplier that bills these
services to the DME Regional Carrier. Agencies that choose to bill DME services on
their HH PPS claims must use the revenue codes below. For additional instructions for
billing DME services see Chapter 20.
029X Durable Medical Equipment (DME) (Other Than Renal)
Required detail: the applicable HCPCS code for the item, a date of service
indicating the purchase date or the beginning date of a monthly rental, a
number of service units, and a charge amount. Monthly rental items should be
reported with a separate line for each month’s rental and service units of one.
060X Oxygen (Home Health)
Required detail: the applicable HCPCS code for the item, a date of service, a
number of service units, and a charge amount.
Revenue Code for Optional Reporting of Wound Care Supplies
062X Medical/Surgical Supplies - Extension of 027X
Required detail: Only service units and a charge must be reported with this
revenue code. If also reporting revenue code 027x to identify nonroutine
supplies other than those used for wound care, the HHA must ensure that the
charge amounts for the two revenue code lines are mutually exclusive.
HHAs may voluntarily report a separate revenue code line for charges for nonroutine
wound care supplies, using revenue code 0623. Notwithstanding the standard
abbreviation “surg dressings,” HHAs use this code to report charges for ALL nonroutine
wound care supplies, including but not limited to surgical dressings.
Chapter 7 of Pub. 100-02, Medicare Benefit Policy Manual defines routine vs. nonroutine
supplies. HHAs will continue to use that definition to determine whether any wound care
supply item should be reported in this line because it is nonroutine.
Information on patient differences in supply costs can be used to make refinements in the
home health PPS case-mix adjuster. The case-mix system for home health prospective
payment was developed from information on the cost of visit time for different types of
patients. If supply costs also vary significantly for different types of patients, the case-
mix adjuster may be modified to take both labor and supply cost differences into account.
Wound care supplies are a category with potentially large variation. HHAs can assist
CMS’ future refinement of payment rates if they consistently and accurately report their
charges for nonroutine wound care supplies under revenue center code 0623. HHAs
should ensure that charges reported under revenue code 027X for nonroutine supplies are
also complete and accurate.
HHAs may continue to report a “Total” line, with revenue code 0001, in FL 42. The
adjacent charges entry in FL 47 may sum charges billed. Medicare claims processing
systems will assure this amount reflects charges associated with all revenue code lines
excluding any 0023 lines.
FL 44. HCPCS/Rates
Required - On the earliest dated 0023 revenue code line, the HHA must report the
HIPPS code (See
§40.1 for definition of HIPPS codes) that was reported on the RAP. On
claims reflecting a SCIC, the HHA reports on each additional 0023 line the HIPPS codes
produced by the Grouper based on each additional OASIS assessment, unless the HIPPS
code change has no payment impact (same HHRG).
For revenue code lines other than 0023, which detail all services within the episode
period, the HHA reports HCPCS codes as appropriate to that revenue code.
FL 45. Service Date
Required - On each 0023 revenue code line, the HHA reports the date of the first service
provided under the HIPPS code reported on that line. For other line items detailing all
services within the episode period, it reports service dates as appropriate to that revenue
code. Coding detail for each revenue code under HH PPS is defined above under FL 43.
For service visits that begin in 1 calendar day and span into the next calendar day, report
one visit using the date the visit ended as the service date.
FL 46. Units of Service Required
The HHA should not report units of service on 0023 revenue code lines. For line items
detailing all services within the episode period, the HHA reports units of service as
appropriate to that revenue code. Coding detail for each revenue code under HH PPS is
defined above under FL 43. For the revenue codes that represent home health visits
(042X, 043X, 044X, 055X, 056X, and 057X), the HHA reports as units of service a
number of 15 minute increments that comprise the time spent treating the beneficiary.
Time spent completing the OASIS assessment in the home as part of an otherwise
covered and billable visit and time spent updating medical records in the home as part of
such a visit may also be reported. Visits of any length are to be reported, rounding the
time to the nearest 15-minute increment. Visits cannot be split into multiple lines.
Report covered and noncovered increments of the same visit on the same line.
FL 47. Total Charges
Required - Zero charges must be reported on the 0023 revenue code line (the field may
be zero or blank). Medicare claims processing systems will place the episode payment
amount for the claim in this field on the electronic claim record. For LUPA claims, the
per visit payment will be reported on individual line items.
For line items detailing all services within the episode period, report charges as
appropriate to that revenue code. Coding detail for each revenue code under HH PPS is
defined above under FL 43. Charges may be reported in dollars and cents (i.e., charges
are not required to be rounded to dollars and zero cents). Medicare claims processing
systems will not make any payments based upon submitted charge amounts.
FL 48. Noncovered Charges
Required - The total noncovered charges pertaining to the related revenue code in FL 42
are entered here. The HHA reports all noncovered charges, including no-payment
claims.
Claims with Both Covered and Noncovered Charges
The HHA reports (along with covered charges) all noncovered charges, related revenue
codes, and HCPCS codes, where applicable.
HHA Bills with All Noncovered Charges
The HHA submits claims when all of the charges on the claim are noncovered (no-
payment claim). The HHA completes all items on a no-payment claim in accordance
with instructions for completing claims for payment, with exceptions including all
charges reported as noncovered. See chapter 1, section 60 for further instructions on no-
payment bills.
FLs 50A, B, and C. Payer Identification
Required - See Chapter 25.
FL 51. Medicare Provider Number
Required - The HHA enters the six position alphanumeric “number” assigned by
Medicare (for CMS use only, effective May 23, 2007, providers are required to submit
only their NPI). It must be entered on the same line as “Medicare” in FL 50.
The HHA reflects a change in Medicare provider number within a 60-day episode by
closing out the original episode with a PEP claim under the original provider number and
opening a new episode under the new provider number. In this case, it reports the
original provider number in this field.
FLs 52A, B, and C. Release of Information Certification Indicator
Required - See Chapter 25.
FL 53. Not required for Medicare HH PPS claim billing.
FL 54. Not required for Medicare HH PPS claim billing.
FL 55. Not required for Medicare HH PPS claim billing.
FL 56. Not required for Medicare HH PPS claim billing.
FL 57. Not required for Medicare HH PPS claim billing.
FLs 58A, B, and C. Insured’s Name
Required only if MSP involved. See Pub. 100-05, Medicare Secondary Payer Manual.
Enter the beneficiary’s name as shown on the Health Insurance Claim card. The name
should be recorded on line A if Medicare is prime, line B if Medicare is secondary, and
line C if Medicare is the tertiary payer. This placement, A, B, or C, should correspond
with the line Medicare was recorded on in FL50.
FLs 59A, B, and C. Patient’s Relationship To Insured
Required only if MSP involved. See Pub. 100-05, Medicare Secondary Payer Manual.
FLs 60A, B, and C. Certificate/Social Security Number/HI Claim/Identification
Number
Required only if MSP involved. See Pub. 100-05, Medicare Secondary Payer Manual.
Enter the Medicare health insurance claim number as shown on the Medicare card. Place
this information on Line A, B, or C as consistent with FL 58.
FLs 61A, B, and C. Group Name
Required only if MSP involved. See Pub. 100-05, Medicare Secondary Payer (MSP)
Manual.
FLs 62A, B, and C. Insurance Group Number
Required only if MSP involved. See Pub. 100-05, Medicare Secondary Payer (MSP)
Manual.
FL 63. Treatment Authorization Code
Required - The HHA enters the claim-OASIS matching key output by the Grouper
software. This data element links the claim record to the specific OASIS assessment
used to produce the HIPPS code reported in FL 44. This is an eighteen-position code,
containing the start of care date (eight positions, from OASIS item M0030), the date the
assessment was completed (eight positions, from OASIS item M0090), and the reason for
assessment (two positions, from OASIS item M0100). The elements in this code must be
reproduced exactly as they appear on the OASIS assessment, matching date formats used
on the assessment.
In most cases the claims-OASIS matching key on the claim will match that submitted on
the RAP. In SCIC cases, however, the matching key reported must correspond to the
OASIS assessment that produced the HIPPS code on the latest dated 0023 revenue code
line on the claim.
FL 64. Employment Status Code
Required only if MSP involved. See Pub. 100-05, Medicare Secondary Payer (MSP)
Manual.
FL 65. Employer Name
Required only if MSP involved. See Pub. 100-05, Medicare Secondary Payer (MSP)
Manual.
Where the HHA is claiming a payment under the circumstances described under FLs
58A, B, or C, and there is involvement of WC or EGHP, it enters the name of the
employer that provides health care coverage for the individual.
FL 66. Employer Location
Required only if MSP involved. See Pub. 100-05, Medicare Secondary Payer (MSP)
Manual.
FL 67. Principal Diagnosis Code
Required - The HHA enters the ICD-9-CM code for the principal diagnosis. The code
must be reported according to Official ICD-9-CM Guidelines for Coding and Reporting,
as required by the Health Insurance Portability and Accountability Act (HIPAA). The
code may be the full ICD-9-CM diagnosis code, including all five digits where
applicable. Where the proper code has fewer than five digits, the HHA does not fill it
with zeros.
The ICD-9 code and principle diagnosis reported in FL 67 must match the primary
diagnosis code reported on the OASIS form item M0230 (Primary Diagnosis).
In most cases the principal diagnosis code on the claim will match that submitted on the
RAP. In SCIC cases, however, the principal diagnosis code reported must correspond to
the OASIS assessment that produced the HIPPS code on the latest dated 0023 revenue
code line on the claim.
FLs 68-75. Other Diagnoses Codes
Required - The HHA enters the full ICD-9-CM codes for up to eight additional
conditions if they coexisted at the time of the establishment of the plan of care. These
codes may not duplicate the principal diagnosis listed in FL 67 as an additional or
secondary diagnosis.
For other diagnoses, the diagnoses and ICD-9 codes reported in FLs 68-75 must match
the additional diagnoses reported on the OASIS, form item M0240 (Other Diagnoses). In
listing the diagnoses, the HHA places them in order to best reflect the seriousness of the
patient’s condition and to justify the disciplines and services provided in accordance with
the Official ICD-9-CM Guidelines for Coding and Reporting. The sequence of codes
should follow ICD-9 guidelines for reporting manifestation codes. Therefore, if a
manifestation code is part of the primary diagnosis, the first two diagnoses should match
and appear in the same sequence on both forms. Medicare does not have any additional
requirements regarding the reporting or sequence of the codes beyond those contained in
ICD-9 guidelines.
OASIS form items M0245a and M0245b, Payment Diagnosis, are not directly reported in
any field of the claim form. If under ICD-9 coding guidelines the codes reported in these
OASIS items must be reported as Other Diagnoses, the codes may be repeated in OASIS
form item M0240 and will be reported in FLs 68-75. In other circumstances, the codes
reported in M0245a and M0245b may not appear on the claim form at all.
FL 76. Not required for Medicare HH PPS claim billing.
FL 77. Not required for Medicare HH PPS claim billing.
FL 78. Not required for Medicare HH PPS claim billing.
FL 79. Not required for Medicare HH PPS claim billing.
FL 80. Not required for Medicare HH PPS claim billing.
FL 81. Not required for Medicare HH PPS claim billing.
FL 82. Attending/Requesting Physician I.D.
Required - The HHA enters the UPIN and name of the attending physician that has
signed the plan of care.
FL 83. Not required for Medicare HH PPS claim billing.
FL 84. Remarks
Optional - Remarks are required only in cases where the claim is cancelled or adjusted.
FL 85. Not required for Medicare HH PPS claim billing.
FL 86. Not required for Medicare HH PPS claim billing.
20.1.2 - Completing the Uniform (Institutional Provider) Bill (Form
CMS-1450) for Hospice Election
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
The following fields must be completed by the hospice on the Form CMS-1450 for the
Notice of Election:
Form Locator (FL) 1. (Untitled) - Provider Name, Address, and Telephone Number
The minimum entry for this item is the provider’s name, city, State, and ZIP code. The
post office box number or street name and number may be included. The State may be
abbreviated using standard post office abbreviations. Five or 9-digit ZIP codes are
acceptable. Use the information to reconcile provider number discrepancies. Phone
and/or FAX numbers are desirable.
FL 4. Type of Bill
Enter the 3-digit numeric type of bill code: 81A, B, C, D, E or 82A, B, C, D, as
appropriate. The first digit identifies the type of facility. The second classifies the type of
care. The third indicates the sequence of this bill in this particular episode of care. It is
referred to as a “frequency” code.
Code Structure
1st Digit - Type of Facility
8 - Special (Hospice)
2nd Digit - Classification (Special Facility)
1 - Hospice (Nonhospital-Based)
2 - Hospice (Hospital-Based)
3rd Digit - Frequency
A - Hospice benefit period initial election notice
B - Termination/revocation notice for previously posted hospice election
C - Change of provider
D - Void/cancel hospice election
E - Hospice Change of Ownership
FL 12. Patient’s Name
The patient’s name is shown with the surname first, first name, and middle initial, if any.
FL 13. Patient’s Address
The patient’s full mailing address including street name and number, post office box
number or RFD, city, State, and ZIP code.
FL 14. Patient’s Birth Date
(If available.) Show the month, day, and year of birth numerically as MM-DD-YYYY. If
the date of birth cannot be obtained after a reasonable effort, the field will be zero-filled.
FL 15. Patient’s Sex
Show an “M” for male or an “F” for female. This item is used in conjunction with FLs
67-81 (diagnoses and surgical procedures) to identify inconsistencies.
FL 17. Admission Date
Enter the admission date, which must be the same date as the effective date of the hospice
election or change of election. The date of admission may not precede the physician’s
certification by more than 2 calendar days, and is the same as the certification date if the
certification is not completed on time.
EXAMPLE
The hospice election date (admission) is January 1, 1993. The physician’s certification is
dated January 3, 1993. The hospice date for coverage and billing is January 1, 1993. The
first hospice benefit period ends 90 days from January 1, 1993.
Show the month, day, and year numerically as MM-DD-YY.
FLs 51A, B, and C. Provider Number
This is the 6-digit number assigned by Medicare (for CMS use only, effective May 23,
2007, providers are required to submit only their NPI). It must be entered on the same
line as “Medicare” in FL 50.
FLs 58A, B, C. Insured’s Name
Enter the beneficiary’s name on line A if Medicare is the primary payer. Show the name
exactly as it appears on the beneficiary’s HI card. If Medicare is the secondary payer,
enter the beneficiary’s name on line B or C, as applicable, and enter the insured’s name
on the applicable primary policy on line A.
FLs 60A, B, C. Certificate/Social Security Number and Health Insurance
Claim/Identification Number
On the same lettered line (A, B, or C) that corresponds to the line on which Medicare
payer information is shown in FL 58, enter the patient’s HICN. For example, if Medicare
is the primary payer, enter this information in FL 60A. Show the number as it appears on
the patient’s HI Card, Social Security Award Certificate, Utilization Notice, EOMB,
Temporary Eligibility Notice, etc., or as reported by the SSO.
FL 67. Principal Diagnosis Code
The full ICD-9-CM diagnosis code is required. The principal diagnosis is defined as the
condition established after study to be chiefly responsible for the patient’s admission.
The CMS accepts only ICD-9-CM diagnostic and procedural codes using definitions
contained in DHHS Publication No. (PHS) 89-1260 or CMS approved errata and
supplements to this publication. The CMS approves only changes issued by the Federal
ICD-9-CM Coordination and Maintenance Committee. Use full ICD-9-CM diagnoses
codes including all five digits where applicable.
FL 82. Attending Physician I.D.
Enter the UPIN and name of the physician currently responsible for certifying the
terminal illness. The UPIN is shown in the first six positions followed by two spaces, the
physician’s last name, one space, first name, one space, and middle initial.
Claims Where Physician Not Assigned a UPIN - Not all physicians are assigned UPINs.
Where the physician is an intern or resident, the number assignment may not be
complete. In addition, numbers are not assigned to physicians who limit their practice to
the Public Health Service, Department of Veterans Affairs or Indian Health Services. Use
the following UPINs to report those physicians not assigned UPINs:
• INT000 for each intern;
• RES000 for each resident;
• PHS000 for Public Health Service physicians, including the Indian Health
Services;
• VAD000 for Department of Veterans Affairs’ physicians;
• RET000 for retired physicians; and
• OTH000 for all other unspecified entities not included above. The OTH000 ID
may be audited.
FL 83. Other Physician I.D.
If the attending physician is a nurse practitioner, enter the UPIN and name of the
nurse practitioner. The UPIN is shown in the first six positions followed by two spaces,
the nurse practitioner’s last name, one space, first name, one space, and middle initial.
The word “employee” or “nonemployee” must be entered here to describe the
relationship the patient’s attending physician has with the hospice. “Employee” also
refers to a volunteer under the hospice jurisdiction.
FL 85-6. Provider Representative Signature and Date
A hospice representative must make sure the required physician’s certification, and a
signed hospice election statement are in the records before signing the Form CMS-1450.
A stamped signature is acceptable.
40.1.3.1 - Care Plan Oversight
(Rev.771, Issued: 12-02-05, Effective: 01-03-06, Implementation: 01-03-06)
The attending physician may bill for care plan oversight services for a hospice enrollee.
The physician must bill for these services using Form CMS-1500; these services are not
to be included on the hospice bill.
Care plan oversight (CPO) exists where there is physician supervision of patients under
care of hospices that require complex and multidisciplinary care modalities involving
regular physician development and/or revision of care plans. Implicit in the concept of
CPO is the expectation that the physician has coordinated an aspect of the patient’s care
with the hospice during the month for which CPO services were billed.
Claims for CPO must be submitted with no other services billed on that claim and may be
billed only after the end of the
month in which the CPO services were rendered. CPO
services may not be billed across calendar months. One unit of service is shown for the
month.
Services not countable toward the 30 minutes threshold that must be provided in order to
bill for CPO include, but are not limited to, time
associated with discussions with the
patient, his or her family or friends to adjust medication or treatment, time spent by staff
getting or filing charts, travel time, and/or physician’s time spent telephoning
prescriptions in to the pharmacist unless the telephone conversation involves discussions
of pharmaceutical therapies.
For CPO claims submitted on or after January
1, 1997, physicians must enter on the
Medicare claim form the Medicare provider number of the hospice providing Medicare
covered services to the beneficiary for the period during which CPO services were
furnished and for which the physician signed the plan of care. Physicians are
responsible for obtaining the hospice
Medicare provider numbers.
For additional information on CPO, see Pub. 100-02, Medicare Benefit Policy Manual,
Chapter 15.
