
Report to Congressional Committees
March 1989
MEDICAID
Recoveries From
Nursing Home
Residents’ Estates
Could Offset
Program Costs
GAO/HRD-89-56

Human Resources Division
B-226448
March 7, 1989
The Honorable Lloyd Bentsen
Chairman, Committee on Finance
United States Senate
The Honorable Henry A. Waxman
Chairman, Subcommittee on Health
and the Environment
Committee on Energy and Commerce
House of Representatives
This report discusses the potential for estate recovery programs to help offset state and
federal Medicaid nursing home costs while removing an inequity in the program. The
inequity involves some nursing home residents with homes having to contribute less toward
the cost of their care than recipients with more liquid assets. The report discusses the need
for the Congress to consider making mandatory the establishment of estate recovery
programs.
Copies of this report are being sent to the Secretary of Health and Human Services; the
Director, Office of Management and Budget; and other interested parties.
This report was prepared under the direction of Michael Zimmerman, Director, Medicare and
Medicaid Issues. Other major contributors are listed in appendix X.
Lawrence H. Thompson
Assistant Comptroller General

Executive Summ~
Purpose
An increasing proportion of Medicaid funds finance nursing home care
for people who become eligible because high medical expenses deplete
their financial resources. Such recipients, known as the medically needy,
must deplete their available financial resources before turning to Medi-
caid, but they are generally allowed to keep their homes for as long as
they or certain of their dependents need them.
Concerns about the treatment of the recipients’ assets have included:
l
that the elderly will dispose of their assets for less than their real value
in order to become eligible for Medicaid, and
l
that the elderly whose assets include a home may not have to contribute
as much toward the cost of their care as those whose assets are more
liquid.
Such actions cause the taxpayers to shoulder a greater portion of the
cost of care than would otherwise be required. These actions also create
an inequity between those with and without homes as part of their
assets.
The Congress has taken a series of actions to address the first concern,
recently requiring states to impose penalties on recipients found to have
transferred assets for less than their value within 30 months of apply-
ing for Medicaid. Also, states have been authorized, but not required, to
establish estate recovery programs to address the second concern.
Through asset recovery programs, states can recover from the estates of
nursing home recipients or their survivors a portion of the expenses the
state incurs in providing nursing home care. Estate recovery programs
require Medicaid recipients whose primary assets are their homes to
contribute toward the cost of their nursing home care in the same man-
ner required of recipients whose assets are in the form of stocks, bonds,
and cash. Unlike the payments made from liquid assets, however, pay-
ments from the home’s equity are deferred until the recipient and his or
her spouse and dependent children no longer need the home.
GAO
studied Medicaid nursing home programs in eight states, focusing
particular attention on the estate recovery program operated by Oregon.
The objective was to discover the potential financial impact of such pro-
grams on Medicaid and whether they provide a mechanism that is
acceptable to the elderly for sharing the costs of nursing home care.
Page 2 GAO/HBDs(Mg Medicaid Estate Recoveries

Executive Summary
Background
The Congress intends that all assets, including home equity, available to
Medicaid nursing home residents be used to help pay for their care.
However, to lessen the hardship on the family, the home-the primary
asset of most elderly
Americans
-is exempt in determining eligibility as
long as there is a spouse, dependent child, or certain other relatives liv-
ing in the home or the nursing home resident expects to return home.
By restricting transfers of the home and other assets to other than the
recipient’s spouse and/or placing a lien on a recipient’s house, states can
help ensure that a Medicaid recipient’s assets remain available to defray
Medicaid costs. Transfer-of-assets restrictions such as those recently
mandated through the Medicare Catastrophic Coverage Act of 1988
apply, however, only while the recipient is alive. Similarly, liens provide
only a mechanism for impeding improper transfers. Unless the state also
has an estate recovery program, it has no means to recover assets that
remain at the time of the recipient’s death or, if there is a surviving
spouse, at the time of the spouse’s death. (See pp. 17 to 19.)
In July 1988 the Department of Health and Human Services’
(HHS)
Inspector General reported
that
only 21 states and the District of Colum-
bia had established programs to recover correctly paid benefits from
recipients’ estates.
Results in Brief
Estate recovery programs provide a cost effective way to offset state
and federal costs, while promoting more equitable treatment of Medicaid
recipients. Oregon recovers about $10 for every $1 spent administering
the program, state officials estimate. Programs such as Oregon’s are a
logical extension of transfer-of-assets and lien provisions, providing the
mechanism for recovering those assets preserved through those
measures.
In the eight states studied, as much as two-thirds of the amount spent
for nursing home care for Medicaid recipients who owned a home could
be recovered from their estates or the estates of their spouses. If imple-
mented carefully, estate recovery programs can achieve savings, while
treating the elderly equitably and humanely. Advocacy groups for the
elderly in Oregon-
the state with the most effective program-told
GAO
that they had not heard any complaints about the program, and that the
state has been flexible in cases where recovery would cause a hardship
to the recipient’s family.
.
Page 3
GAO/ERD@%6 Medicaid Estate Recoveries

Executive Summary
Principal Findings
Potential Recoveries Are
Significant
About 14 percent of the Medicaid nursing home residents in the eight
states
GAO
reviewed owned a home with an average value of about
$31,000, based on county records.
GAO
based this estimate on examina-
tion of Medicaid applications filed for random samples of residents
admitted to nursing homes during fiscal year 1986 in the eight states.
(see pp.
19-2Q)
By using home equity to defray Medicaid costs as Oregon does, the six
states that now lack recovery programs could recover about $85 million
from recipients admitted to nursing homes in fiscal year 1986. This rep-
resents 68 percent of the approximately $126 million cost to Medicaid of
nursing home care for those recipients who owned homes. (See pp.
20-22.)
In Pennsylvania and Michigan, attempts to establish estate recovery
programs through administrative procedures were blocked by legal chal-
lenges, state officials told
GAO.
Oregon avoided such problems by enact-
ing legislation specifically authorizing estate recoveries. (See p. 35.)
Recoveries From Spouses’
Because about one-third of Medicaid nursing home residents who own a
Estates
home have a spouse living in the community, a significant portion of
potential recoveries is lost unless a state authorizes recoveries from the
estates of surviving spouses. For example,
GAO
estimates that California
will recover about $15.8 million from the estates of Medicaid recipients
admitted to nursing homes in 1985 under its existing recovery program.
But it could recover an additional $11 million if the state enacts legisla-
tion to authorize recoveries from the estates of the surviving spouse
when he or she, in turn, dies. (See pp. 22 and 37.)
Limited HHS Role
HHS, responsible at the federal level for administering the Medicaid pro-
gram, has little information on effective recovery programs. Moreover,
the wording of regulations has contributed to confusion over whether
the law permits recoveries from the estates of Medicaid recipients who
were under age 65 when they were admitted to a nursing home. As a
result, both Oregon and California have limited their recovery programs
to recipients 65 or older. (See pp. 23-25.)
Page 4
GAO/HBD8966 Medicaid Estate Recoveries

Executive Summary
Matters for
GAO
believes the Congress should consider making mandatory the estab-
Consideration by the
lishment of programs to recover the cost of Medicaid assistance pro-
vided to nursing home residents of all ages either from their estates or
Congress
from the estates of their surviving spouses. Establishment of such pro-
grams would be a logical extension of the transfer-of-assets provisions
recently mandated through the Medicare Catastrophic Coverage Act of
1988. Estate recovery programs would help ensure that the assets pre-
served through the new transfer-of-assets provisions are eventually
used to defray state and federal Medicaid costs. (See p. 41.)
Agency Comments
HHS
and officials from the seven states that provided comments (Califor-
nia, Michigan, Ohio, Oregon, Pennsylvania, Washington, and Wisconsin)
generally agreed that estate recovery programs could offset Medicaid
costs. Several state officials identified actions they plan to take to
encourage expansion of such programs. (See pp. 41-47.)
Page 6
GAO/HBD8966 Medicaid Estate Recoveries
-
Contents
Executive Summary
2
Chapter 1
8
Introduction
Medicaid
Medicaid Eligibility Criteria
Box-en-Long Amendment Limits Transfers
TEFRA Further Restricts Transfers and Authorizes
Greater Use of Liens and Estate Recoveries
Medicare Catastrophic Coverage Act of 1988
Objectives, Scope, and Methodology
8
9
10
10
13
14
Chapter 2
Significant Recovery
States Need Both Transfer-of-Assets and Recovery
of Nursing Home Costs
Programs
From Estates Possible
About 14 Percent of Medicaid Nursing Home Recipients
Own a Home
17
17
19
Medicaid Pays Millions in Nursing Home Bills for
Homeowners
20
Medicaid Recovers Little of Its Nursing Home Costs From
Recipients’ Estates
21
Expanding Programs to Recover From Estates of
Institutionalized Recipients Under Age 66 Would
Increase Recoveries
23
Chapter 3
Oregon Recovery
HCFA Provides Limited Technical Assistance
Program an Example
The Recovery Process in Oregon
for Other States
Key Elements of Oregon’s Recovery Program
25
25
26
35
Chapter 4
40
Conclusions, Matters
Conclusions
40
for Consideration by
Matters for Consideration by the Congress 41
HHS Comments and Our Evaluation
41
the Congress, and
State Officials’ Comments and Our Evaluation
44
Agency and State
Comments
Page 6 GAO/IlRDWWl
Medicaid Estate Recoveries

-~-
Contents
Appendixes
Appendix I: Methodology Used to Determine Potential
Recovery for Medicaid Recipients Who Own Real
Property
48
Appendix II: Comments From the Department of Health
and Human Services
53
Appendix III: Comments From the State of California
Appendix IV: Comments From the State of Michigan
Appendix V: Comments From the State of Ohio
Appendix VI: Comments From the State of Oregon
Appendix VII: Comments From the Commonwealth of
Pennsylvania
58
60
61
63
64
Appendix VIII: Comments From the State of Washington
66
Appendix IX: Comments From the State of Wisconsin
67
Appendix X: Major Contributors to This Report
68
Tables
Table 1.1: Annual Medicaid Estate Recoveries
Table 2.1: Projected Number and Value of Real Properties
Owned by Medicaid Recipients in Eight States (1985)
Table 2.2: Estimated Medicaid Payments for Nursing
Home Residents in Eight States Who Owned Real
Property ( 1985)
13
20
21
Table 2.3: Projected Recoveries From Estates of Medicaid
Recipients Admitted to Nursing Homes in Eight
States (1985)
22
Figures
Figure 3.1: Oregon’s Recovery Process: Identifying Assets
Figure 3.2: Oregon’s Recovery Process: Tracking and
Preserving Assets
28
30
Figure 3.3: Oregon’s Recovery Process: Recovering When
Assets Become Available
33
Abbreviations
American Association of Retired Persons
Aid to Families With Dependent Children
HCFA
Health Care Financing Administration
HHS
Department of Health and Human Services
SSI
Supplemental Security Income
TEFRA
Tax Equity and Fiscal Responsibility Act of 1982
Page 7
GAO/HB.D-W56 Medicaid Estate Recoveries

Chapter 1
Introduction
A Medicaid applicant’s ownership of a home does not usually make him
or her ineligible for Medicaid. Even though the home represents a poten-
tial resource to the individual that, upon sale or transfer, could be used
to defray the costs of medical care, the original Medicaid statute
severely limited states’ ability to restrict transfers, impose liens, or
recover correctly paid benefits from recipients’ estates. Specifically, the
Social Security Act prohibited states from imposing liens against any
recipient’s property before his or her death for Medicaid claims cor-
rectly paid on the individual’s behalf. In effect, the act generally prohib-
ited states from placing restrictions on the applicant’s ability to transfer
assets for the purpose of establishing Medicaid eligibility.
The law permitted states to recover Medicaid funds from the estates of
those recipients aged 66 or over but only after the death of the surviv-
ing spouse and only if there was no surviving child under the age of 21
or blind or disabled. Estate recovery programs were hard to administer,
however, because of the limits placed on the use of liens and transfer
restrictions. States were unable to identify and place liens on property
before the recipient’s death to ensure that the asset remained for future
recovery. This enabled an elderly individual to transfer his or her home
to a family member or friend and thereby assure that the home would
not be part of his or her estate and, therefore, would not be subject to
any recovery action initiated after the death of the individual.
In 1982, the Congress enacted measures to help prevent such practices
and ensure that all resources available to an institutionalized individual
not needed for support of a spouse or dependent child are applied
toward the cost of care. The Tax Equity and Fiscal Responsibility Act of
1982 (TEFRA) made it easier for states to restrict transfers, impose liens,
and recover the costs of provided services from the estates of Medicaid
recipients. This report focuses primarily on estate recovery programs.
Medicaid
Medicaid is a federally aided, state-administered medical assistance pro-
gram that served about 22 million needy people in fiscal year 1985. It
became effective on January 1, 1966, under authority of title XIX of the
Social Security Act, as amended (42 U.S.C. 1396). Within broad federal
limits, states set the scope and reimbursement rates for medical services
offered and make payments directly to the providers who render
services.
The Health Care Financing Administration
(HCFA),
within the Depart-
ment of Health and Human Services
(HHS),
has overall responsibility for
Page 8
GAO/HBDs956 Medicaid Estate Recoveries

Chapter 1
Introduction
administering the Medicaid program at the federal level. This includes
developing program policies, setting standards, and ensuring compliance
with federal Medicaid legislation and policies. The nature and scope of a
state’s Medicaid program are contained in a state plan, which, after
approval by
HHS,
provides the basis for federal funding.
Medicaid Eligibility
Criteria
Medicaid eligibility criteria are among the most complex of all assistance
programs. At a minimum, states must provide Medicaid coverage to all
persons who receive cash payments from the Aid to Families With
Dependent Children (AF’DC) program and almost all persons covered by
the Supplemental Security Income (SSI) pr0gram.l These Medicaid recipi-
ents are called categorically needy.
At their option, states can extend Medicaid coverage to certain groups,
including (1) institutionalized individuals with incomes up to 300 per-
cent of the
SSI
payment level (42 C.F.R. 436.231) and (2) those who
would be eligible for cash assistance if they were not in an institution
(42 C.F.R. 435.211).
States also can extend Medicaid coverage to individuals who are ineligi-
ble for cash assistance on the basis of income but whose income and
resources are considered insufficient to meet their medical needs. Pro-
grams for these medically needy persons accommodate individuals who
meet all the criteria for categorical assistance except for income and
who have incurred relatively large medical bills. Persons or families
with incomes above the medically needy income standard can deduct
certain incurred medical expenses for purposes of determining their
countable income to determine eligibility for Medicaid. In fiscal year
1986,34 states and the District of Columbia had medically needy
programs.
In addition to meeting income limits, Medicaid applicants’ assets must be
within specified limits. For example, to qualify for Medicaid as an SSI
recipient in 1988, an applicant could have a home of any value but could
not have liquid assets worth more than $1,900 for an individual and
‘Fourteen states limit Medicaid coverage of SSI recipients by requiring them to meet more restrictive
eligibility standards in effect before the January 1,1972, implementation of SSI, the Congressional
Research Service reported in July 19%‘. States choosing this option must allow applicants to deduct
medical expenses from income to establish eligibility. The 14 states (Connecticut, Hawaii, Illinois,
Indiana, Minnesota,
Missouri,
Nebraska, New Hampshire, North Carolina, North Dakota, Ohio,
Oklahoma, Utah, and Virginia) are referred to commonly as “209 (b) states.”
Page 9
GAO/HI@B69 Medicaid Estate Recoveries

Chapter 1
introduction
-
$2,850 for a couple. Under certain circumstances, states can impose
more stringent asset limits for SSI beneficiaries.
Asset limits for medically needy programs vary by state, but must be
(1) at least as liberal as the highest limits allowed for cash assistance
recipients in the state and (2) the same for all covered groups. The liquid
asset limits for a family of two ranged from $2,250 to $6,450 as of the
second quarter of 1987.
According to the Congressional Research Service, the majority of elderly
persons who become eligible for Medicaid’s nursing home benefit do so
only after they have spent down to Medicaid income and asset limits.
Generally, they enter the nursing home as a private pay patient and con-
vert to Medicaid after having spent their “excess” income and resources
on nursing home care.
Middle-income nursing home residents with sizeable assets may find it
difficult to qualify for Medicaid. This creates an incentive to transfer or
otherwise dispose of assets for less than fair market value in order to
establish Medicaid eligibility.
Boren-Long
Amendment Limits
Transfers
In an attempt to limit the ability of individuals to get around Medicaid
asset limits by transferring assets, the Congress passed the Roren-Long
Amendment of 1980, which permitted states to restrict transfers of non-
exempt assets. This amendment had limited effect, however, because
home equity-an exempt asset-represents the primary asset of most
elderly. Under the Boren-Long Amendment, a home can be transferred
to a son or daughter or other person at any time without affecting Medi-
caid eligibility.
TEFRA Further
Restricts Transfers
and Authorizes
Greater Use of Liens
To further limit the ability of individuals with assets that could be used
to pay for their nursing home care to give those assets away in order to
establish Medicaid eligibility, the Congress enacted section 132 of
TEFRA.
The act modified provisions of the Social Security Act (section 1917) by
authorizing states to place further restrictions on asset transfers, thus
and Estate Recoveries
making it easier to impose liens against the assets. TEFRA also established
the conditions under which states can undertake estate recovery. The
changes in the lien and transfer-of-assets provisions should enhance
states’ ability to operate effective programs.
HHS
noted in its implement-
ing regulations that the
TEFRA
provisions are
Page 10
GAO/HRD-89-66 Medicaid Estate Recoveries

Chapter 1
Introduction
$6
.
intended to assure that all of the resources available to an institutionalized
individual, including equity in a home, which are not needed for the support of a
spouse or dependent children, will be used to defray the costs of supporting the
individual in the institution. In doing so, it seeks to balance government’s legitimate
interest in recovering its Medicaid costs against the individual’s need to have the
home available in the event discharge from the institution becomes feasible.”
The original transfer-of-assets provisions of TEFRA permitted states to
deny Medicaid assistance to any individual who otherwise became eligi-
ble because he or she disposed of resources for less than fair market
value within 2 years of applying for Medicaid or at any time after this
period. The time period was subsequently extended to 30 months by the
Medicare Catastrophic Coverage Act of 1988 (see p. 13). A Medicaid
recipient may be declared ineligible if the home, an excludable asset, is
transferred for less than fair market value to anyone other than the
spouse, child under 21 years of age, or child who is blind or disabled
while the recipient is in a nursing home. Transfer-of-assets policies have
been adopted by 49 states.
TEFRA allows a state to place a lien against a recipient’s real property for
the purpose of recovering correctly paid Medicaid benefits if the state
can reasonably determine that the recipient is not expected to return
home. A state may not place a lien on an individual’s home if his or her
spouse or dependent child is lawfully residing in the home. In addition, a
lien must be removed if the recipient returns home. Liens are not self-
executory, but merely impede the ability of the property holder to con-
vey the property. If a lien exists, the property holder must satisfy the
lien before the property may be sold or transferred. The lien holder-in
this case the state Medicaid agency-does not have to wait until the
property is sold or transferred to recover; it can itself force the sale of
the property to satisfy its claim. Only Alabama and Maryland intention-
ally place liens prior to death to recover correctly paid benefits provided
to Medicaid nursing home residents, according to the
HHS
Inspector Gen-
eral’s June 1988 report.
Finally, TEFRA established conditions under which states can defray the
costs of Medicaid assistance paid on behalf of nursing home residents
through estate recovery. Under an estate recovery program, the state
files a claim against the estate for the cost of Medicaid assistance pro-
vided.’ As in the prior statutes, recovery cannot be made until (1) the
death of the recipient’s spouse and (2) the recipient has no surviving
‘If the estate is not settled in probate court, the state can seek reimbursement from the executor of
the estate.
Page 11
GAO/lIlUHWS6
Medicaid Estate Recoveries
Chapter 1
Introduction
-
child who is either under 21 or who is blind or disabled. In addition,
TEFRA provided that recovery cannot be undertaken based on a lien
imposed on the home if certain relatives have resided there since the
Medicaid recipient moved into the institution.3 Despite these limitations,
designed to prevent estate recoveries from creating undue hardship on
the Medicaid recipient’s family, TEFRA enhanced states’ abilities to oper-
ate effective recovery programs by helping ensure that assets were not
disposed of for less than fair market value in order to establish Medicaid
eligibility or preserve an inheritance.
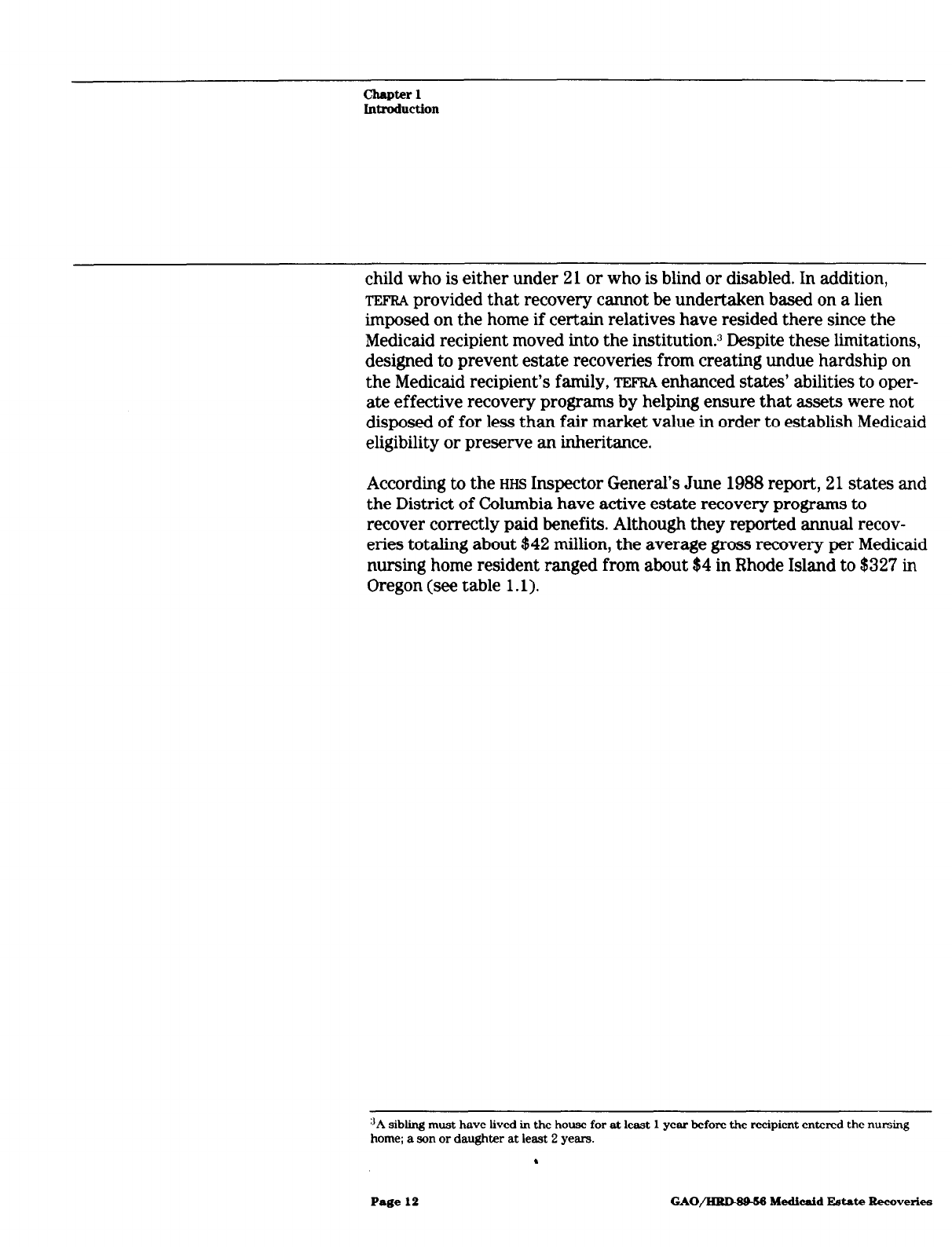
According to the
HHS
Inspector General’s June 1988 report, 21 states and
the District of Columbia have active estate recovery programs to
recover correctly paid benefits. Although they reported annual recov-
eries totaling about $42 million, the average gross recovery per Medicaid
nursing home resident ranged from about $4 in Rhode Island to $327 in
Oregon (see table 1.1).
“A sibling must have lived in the house for at least 1 year before the recipient entered the nursing
home; a son or daughter at least 2 years.
.
Page 12
GAO/llRMSM Medicaid Estate Recoveries

-r
Chapter 1
Inboduction
Table 1.1: Annual Medicaid Eatate
Recoveries
State
Alabama
California
Connecticut
2.100900
250,000 67.55
Amount of cost of
recovery’ recovery
$202,000 $55,000
12.000900 625600
Average gross
recovery per
Medicaid nursing
home resident
$9.74
91.37
District of Columbia 300,000 129,408 95.39
%ridab 640,941 c 17.00
Georgiab 1,089,358 c 30.35
Hawaii 68,208 8,280 16.78
Illinois 1,620,OOO 70,400 22.08
Indianad 400,000 c 9.86
Maryland 1,230,071 104,000 45.91
Massachusetts 4.800.000 93.450 109.05
Minnesota 4,722,895
‘
100.80
Missouri 453,000 21,391 15.53
Montana 150,000 lF900 29.93
New Hampshire 900,ooo 66,000 160.11
New Jersev 435.000 150,000 13.51
New Yorkb
North Dakota
5,942,995
c
53.62
316,955 34,200
5176
Oregon
Rhode Island
4,000,OOO 306,000
327.44
45.000 26.000
4.24
Utah 230,000
45,000
40.74
Vermont
TOtal
69,326 5,667
20.34
$41,715,749
$2,005,396
Source: Medicard Estate Recoveries, Office of Inspector General, HHS OAI-69-86-06678, June 1966,
p, 27.
aThe Inspector General’s report does not state the trme frame for reported recoveries except where
noted.
‘Amounts listed as recovenes are those reported to HCFA as “probate recoveries” in federal fiscal year
1985.
‘Unknown.
dlndrana no longer tracks estate recoveries. This figure is a projection based on past recovery perform-
ance.
Medicare Catastrophic
The Medicare Catastrophic Coverage Act of 1988 amended TEFRA provi-
Coverage Act of 1988
sions pertaining to Medicaid estate recoveries. The act extends (to 30
months) and makes mandatory the restrictions on transfers of assets for
less than fair market value. This should help ensure that resources
remain available for later recovery. Second, the act makes it easier for a
.
Page 13
GAO/Hl?DW-66 Medicaid Estate Recoveries

Chapter 1
Introduction
couple to qualify for Medicaid by requiring states to exclude more
income and resources in determinin
g eligibility if there is a noninstitu-
tionalized spouse. Because not as much of a couple’s income must be
applied toward the cost of care, these provisions will make it easier for
middle-income elderly to spend down to qualify for Medicaid and this
should increase recovery potential. Finally, the act requires the Secre-
tary of
HHS
to study the means for recovering the amounts from the
estates of deceased beneficiaries (or the estates of spouses of deceased
beneficiaries) to pay for nursing home services furnished under Medi-
caid. The Secretary was required to report to the Congress no later than
December 3 1, 1988, and to include appropriate recommendations for
changes.
Methodology
efforts to reduce program costs
by using the estates of Medicaid
nursing
home recipients or their surviving spouses to recover all or part of the
costs of care paid for by Medicaid. Our specific objectives concerning
estate recovery programs were to
l
identify key elements of effective programs,
l
estimate potential savings from establishment or expansion of
programs,
. identify barriers to the establishment of programs, and
. evaluate policy implications of programs.
We chose the Oregon program to identify the key elements of a success-
ful estate recovery program because it reported annual recoveries per
nursing home recipient more than twice those reported by any other
state. In addition, Oregon has been mentioned by
HCFA
as a model pro-
gram. In Oregon, we (1) reviewed pertinent laws, regulations, and proce-
dures supporting the estate recovery program, (2) obtained the views of
state officials on the elements of their program that they believed were
most important to its success, and (3) obtained the views of representa-
tives of advocacy groups for the elderly, such as the Gray Panthers, the
American Association of Retired Persons
(AARP),
United Seniors, and the
Senior Law Center.
To determine the potential for Medicaid cost savings from the establish-
ment or expansion of estate recovery programs, we reviewed the Medi-
caid applications for 200 randomly selected nursing home residents
from Oregon and seven other states. We selected six states (Michigan,
Ohio, Pennsylvania, Texas, Washington, and Wisconsin) because they
Page 14 GAO/IllUM946 Medicaid Estate Recoveriea

Chapter 1
Introduction
did not have recovery programs and had among the largest Medicaid
nursing home programs. We selected California because it (1) operates
an estate recovery program but was recovering significantly less per
recipient than Oregon when we began our review and (2) accounts for
about 8 percent of all Medicaid nursing home payments.
In each state, we reviewed the Medicaid application (or
SSI
application if
Medicaid eligibility was established based on
SSI
eligibility) for 200 ran-
domly selected Medicaid recipients 66 years of age or older who were
first admitted to nursing homes in calendar year 19EK4 We selected
1986 as a sampling time frame rather than 1986 or 1987, to enable us to
obtain actual Medicaid cost data on as many recipients as possible.
Using the applications, we identified recipients who declared real prop-
erty ownership. In 13 counties in seven states, we reviewed county
records at the offices of the county assessors and treasurers to deter-
mine whether recipients (1) owned real property that was not declared
on their applications or (2) transferred property for less than fair mar-
ket value within 2 years of or after applying for Medicaid. Because our
work in the 13 counties did not identify many instances of home owner-
ship or transfers not disclosed on the applications, we decided to limit
our evaluation to home ownership disclosed on the Medicaid and/or
SSI
application.
For recipients with real property, we contacted the county assessor’s or
treasurer’s office to determine the value of the property. We then esti-
mated potential recoveries from the estates of recipients with real prop-
erty based on the policies and procedures followed in the Oregon
recovery program. Finally, we projected recoveries to the universes for
each of the eight states. Our methods for estimating potential recoveries
are discussed in more detail in appendix I.
To identify barriers to the establishment or expansion of estate recovery
programs, we (1) interviewed Medicaid officials in the eight states;
(2) attended a legislative hearing in the state of Washington on proposed
estate recovery legislation; (3) interviewed
HCFA
headquarters and
regional office officials to determine
HCFA’S
role in assisting states in
establishing recovery programs; and (4) interviewed representatives
from
AARP,
the Gray Panthers, and advocacy groups for the elderly in
Oregon about the Oregon program.
‘We limited our review to recipients 65 or older
because
HHS, in publishing its implementing regula-
tions, appeared to limit recoveries to that age
group.
Page 16
GAO/HRD-S956 Medicaid Estate Recoveries

Chapter 1
Introduction
-
Our work was done between September 1986 and August 1987 in
accordance with generally accepted government auditing standards.
Page 16 GAO/IIRD-WM Medicaid Estate Recoveries

Significant Recovery of Nursing Home Costs
From Estates Possible
Many elderly who
own
a home when they enter a nursing home still own
it when they die. States that do not operate effective estate recovery
programs lose the opportunity to use this primary asset of about
one-
fourth of Medicaid recipients-their
home
equity-to defray Medicaid
costs. This is because transfer-of-assets provisions do not apply to assets
remaining at the time of the Medicaid recipient’s death, and liens are not
self-executing.
Of elderly Medicaid recipients admitted to nursing homes during calen-
dar year 1986 in the eight states reviewed, about 14 percent owned a
home or other real property (such as a farm) at the time they applied
for Medicaid. The average value of the real property they held based on
county assessment records was about $31,000. We estimate that
although Medicaid will pay an average $12,000 in nursing home bills for
those recipients, only about $1,360 of those payments is likely to be
recovered because
l
six of the eight states had no programs to recover their Medicaid nursing
home costs from
the
estates of Medicaid recipients and their spouses,
and
l
one state (California) had a recovery program but was not recovering
from the estates of surviving spouses.
If the seven states had had programs similar to Oregon’s, we estimate
that an additional $6,716 on average could have been recovered per
recipient.
Another opportunity for recoveries was lost in all eight states because
HCFA
regulations did not clearly indicate that recoveries were permitted
for institutionalized recipients under age 66. We did not estimate poten-
tial recoveries for this group, but believe
they
could be significant based
on
the
extent of home ownership in younger age groups.
States Need Both
Estate recoveries are an essential component of state efforts to ensure
Transfer-of-Assets
and
that Medicaid recipients’ assets are used to defray Medicaid costs. In
effect, a state that has a transfer-of-assets policy but
no
recovery pro-
Recovery Programs
gram ensures
that
the home remains available to defray Medicaid costs
while
the
recipient is alive, but fails to recover upon
the
death of the
recipient, even if there is
no
surviving spouse. The absence of an estate
recovery program also creates inequities in the treatment of Medicaid
recipients and their heirs, allowing recipients who still own a home at
the time of death to leave an estate, while requiring those
that
do not
Page 17 GAO/HRD-89-56 Medicaid Estate Recoveries

Chapter 2
Significant Recovery of Nursing Home Costa
From Estates Possible
own a home to apply most of their liquid assets toward the cost of their
care before they become Medicaid-eligible.
The Congress intended to enable states to require that all of an institu-
tionalized recipient’s available resources be used to defray the costs of
institutionalization (section 1917, Social Security Act). As we discuss on
pages 10-12, such resources include equity in a home. These and certain
other resources, however, are not available to help pay for institutional
costs while the assets are needed to support a spouse or dependent child
or if there is a chance that the recipient will return home. Each of the
states we reviewed had established a transfer-of-assets policy to prevent
an individual from transferring assets to other than the spouse or
dependent child in order to establish Medicaid eligibility. But six of the
eight states (Michigan, Ohio, Pennsylvania, Texas, Washington, and Wis-
consin) had not, at the time of our review, established an estate recov-
ery program.
Without a recovery program, a transfer-of-assets policy leaves the
states without a mechanism to use assets remaining at the time of death
to defray Medicaid costs. Also, any such assets revert to the recipient’s
estate and can be transferred to the recipient’s nondependent children
or other heirs without first being used to defray Medicaid costs. The
following hypothetical example illustrates the inequities that could
result.
Example 1-A widow who had been living alone in her $40,000 home
enters a nursing home, but expects to return home. The widow’s home is
exempt in determining Medicaid eligibility. If the woman died after 1
year in the nursing home without selling the home, her heirs would
inherit the home and none of the proceeds from its sale would be used to
repay the Medicaid program for the $16,000 in nursing home payments.
However, if the home had been sold before she died, the widow would
be ineligible for Medicaid benefits until the remainder from the sale of
the home had been spent down to the $1,600 Medicaid asset limit. In
addition, proceeds from the sale could have been used to repay the
Medicaid program for the nursing home costs already incurred if the
state had placed a lien on her property before she died. The woman’s
heirs would have received only those funds remaining at the time of
death that were not needed to pay for the parent’s nursing home care.
Finally, if the widow had $40,000 in savings but did not own a home,
she would have been required to spend down to the Medicaid asset limit
($1,600) as a private pay patient before she could become eligible for
Page 18
GAO/IiRBWM Medicaid Estate Recoveries

-
Chapter 2
Significant Recovery
of
Nursing Home Costa
Prom Estates Podble
Medicaid. After about 2 years as a private pay patient, she could have
established Medicaid eligibility. During those 2 years, the Medicaid pro-
gram would have avoided about $30,000 in nursing home payments. The
adult child would be left with no inheritance.
The above example shows that a recipient who does not own a home or
sells a home while in a nursing home must apply his or her assets
toward the cost of nursing home care. On the other hand, the recipient
who still owns a home at the time of death need not apply those assets
toward the cost of care, unless the state has established an estate recov-
ery program.
About 14 Percent of
In the eight states reviewed, the percentage of nursing home recipients
Medicaid Nursing
in our sample who owned a home or other real property when they
applied for Medicaid ranged from 8.6 percent in Pennsylvania to 21 per-
Home Recipients Own
cent in Wisconsin (see table 2.1). An average of 14 percent of Medicaid
a Home
nursing home recipients sampled in the eight states owned real prop-
erty. Of the property owners, only about 7 percent indicated they were
still making mortgage payments (see p. 48 for a more detailed discus-
sion). In each state, our random sample consisted of 200 individuals 66
years or older, whose Medicaid applications we reviewed to identify
whether they owned a home or other real property at the time of
application.
The average value of real property owned by Medicaid nursing home
recipients sampled in the eight states was $30,712, ranging from about
$23,000 in Michigan to $39,000 in Washington (see table 2.1). We deter-
mined the value of the properties from county records (see p, 49 for a
discussion of these sources).
Page 19
GAO/HID&t%
lkdicaid Estate Recoveries

Chapter 2
Significant Recovery of Nursing Home Costa
From Estates Possible
Table 2.1: Projected Number and Value
of Real Properties Owned by Medicaid
Recipients in Eight States
(1985)
State
California
Recipients
Projected home
admitted to
ownership
Average
value of real
nursing homes Number
Projected total
Percent
wwerty~
value of property
29,416
3,677 12.5
$36,168
$132.989.736
Michigan
9,711
874 9.0 23,287
203352,838
Ohio
13,000
2,340 18.0 28,214
66,020,760
Oreaon
3,018
453 15.0 37.234
16.867.002
Pennsylvania
17,374
1,477 8.5 26,035
38,453,695
Texas
14,980
2,846 19.0 25,476
72.504.696
Washington
7,122
783 11.0 39,162
30,663,846
Wisconsin
9,520
1,999 21 .o 32,012
63,991,988
Total
104,141
14,449 (14.01 $30.712
5441.844.561 b
%epresents the average value of real property for the 228 recipients in the eight state samples
bThls figure IS accurate withln plus or minus $64,662.650 at the 95-percent confidence level
We estimate that 14,449 Medicaid recipients admitted to nursing homes
in 1985 in the eight states at the time of admission owned real property
valued at about $442 million.
Medicaid Pays Millions
For each of our sample recipients who owned a home or other real prop-
in Nursing Home Bills
erty, we estimate that Medicaid will pay nursing home costs ranging
from $10,281 in Texas to $14,745 in Washington over the duration of his
for Homeowners
or her nursing home stay (see table 2.2). For the eight states we
reviewed, we project total Medicaid payments of about $176 million for
the estimated 14,449 recipients admitted to nursing homes in 1985 who
owned real property. We based our estimates on actual Medicaid pay-
ments in 1985 and 1986, and projected payments for those who were
still in the homes at the beginning of 1987.
Page 20
GAO/HRD&L56 Medicaid Estate Recoveries

chapter 2
Significant Recovery of Nursing Home C.&a
Prom Estates Possible
Table 2.2: Estimated Medicaid Payments
for Nursing Home Residents in Eight
Average Estimated total
States Who Owned Real Property
(1985)
Projected recipients Medicaid Medicaid
State
owning real property payments
payments
California
3,677 $12,523 -$46,047,071
Michigan 874 13,409 11,719,466
Ohio
2,340 12,649
29,598,660
Oregon 453 9,674 4,382,322
Pennsylvania 1,477 10,463 15,453,851
Texas 2,846 10,281 29,259,726
Washington 783 14,745 11,545,335
Wisconsin 1,999 13,802 27,590,198
Total
14,449
$12,193 $175,596,62g8
aThis figure is accurate wlthln plus or minus $X4,912,950 at the 95-percent confidence level
Medicaid Recovers
Little of Its Nursing
Home Costs From
Recipients’ Estates
A state cannot use a Medicaid recipient’s home equity to defray Medi-
caid costs unless the home is either (1) sold before the recipient dies or
(2) the state operates an estate recovery program (see pp. 10-12). At the
time we completed our field work, 95 of the 228 recipients in our sam-
ples who owned a home at the time they entered the nursing home were
deceased. Of those 95 recipients, 91 owned their homes at the time of
death. Because Medicaid recipients in the eight states generally retained
ownership of their homes until death, only Oregon and California-the
two states with recovery programs-could use recipients’ home equity
to defray Medicaid costs.
In the eight states reviewed, only about $19.5 million of the estimated
$176 million in Medicaid payments for recipients admitted to nursing
homes in 1985 who owned real property will be recovered (see table
2.3). To determine the potential effect of a recovery program on Medi-
caid costs, we applied the recovery procedures used by Oregon to the
cases in all eight states. Oregon recovers up to the actual cost of Medi-
caid services provided from the recipient’s estate, or, if there is a surviv-
ing spouse, from the spouse’s estate. (See app. I for a more detailed
discussion of the methods used to estimate potential recovery.)
Page 21 GAO/HRD8%56 Medicaid Estate Recoveries

Chapter 2
Significant Recovery of Nursing Home Costa
From Estates Possible
Table 2.3: Projected Recoveries From
Estates of Medicaid Recipients Admitted
Estimated
to Nurring Homes in Eight States
(1985)
Projected
recoveries under recoveries based
State 1986 state law on Oregon law Increase
California
$15,801,100
$26,740,760
$10,939,660
Michigan 0
9,869,386 9,869,386
Ohio
0
21,226,600 21,226,604
Oregon
3,779,427 3,779,427
0
Pennsylvania
0
8,447,847
8,447,847
Texas
0 20.297900
20.297900
Washington
Wisconsin
Total
0
6,890,606 6,890,606
$19.580,52~
18,368,170 18,368,170
$115,620,696”
$96,040,169
aThis figure is accurate within plus or minus $23,835,640 at the 95-percent confidence level
By establishing recovery programs patterned after Oregon’s, the six
states without recovery programs could defray about $85 million of the
estimated $125 million in Medicaid nursing home payments they will
incur for recipients owning a home. Although California operates a
recovery program, it does not attempt to recover from the estates of
surviving spouses because state law does not authorize such recoveries.
We estimate that California could increase recoveries by about $11 mil-
lion by recovering from the estates of surviving spouses. Overall, in the
eight states we sampled, about one-third of the recipients who owned
property had a surviving spouse, making recoveries from their estates
an important component of states’ efforts to defray Medicaid costs.
During the course of our review, Texas and Washington enacted legisla-
tion establishing recovery programs. However, neither program offers
the recovery potential of the Oregon program. Specifically:
. Texas’s law does not authorize recovery from spouses’ estates. About
$6 million of the approximately $20 million in projected recoveries in
Texas would be from spouses’ estates.
. Washington’s law, enacted in 1987, does not allow recovery from real
property sold for less than $50,000 if there are any surviving children,
even if they have reached adulthood. For real property sold for over
$50,000, recovery is limited to 35 percent of the value if there is an
adult child. These provisions reduce projected recoveries in Washington
from about $7 million to about $218,000.
.
Page 22 GAO/HRD43H56 Medicaid Estate Recoveries

Chapter 2
S&i&ant Recovery of Nursing Home Coetu
Prom Eetates Possible
Expanding Programs
Neither Oregon nor California attempts to recover from the estates of
to Recover From
institutionalized recipients under age 66. Officials from both states told
us that they believed that recoveries from recipients under age 66 were
Estates of
authorized by section 1917 only if a lien were placed before the death of
Institutionalized
the recipient. But our analysis of the law and discussions with
HCFA
offi-
Recipients Under Age
cials indicate that recoveries from the estates of permanently institu-
tionalized recipients under 66 are permitted. Because the rate of home
65 Would Increase
ownership is higher for individuals under age 66 and about 14 percent
Recoveries
of skilled nursing home residents were under 66 in fiscal year 1983,’
recoveries could be significant.
Section 1917(b) reads, in pertinent part,
“( 1) No adjustment or recovery of any medical assistance correctly paid on behalf of
an individual under the State plan may be made, except-
“(A) in the case of an individual described in subsection (a)( l)(B) of this section
[which refers to permanently institutionalized individuals whom states require to
pay most of their income for medical care], from his estate or upon sale of the prop-
erty subject to a lien imposed on account of medical assistance paid on behalf of
such individual. and
“(B) in the case of any other individual who was 66 years of age or older when he
received such assistance, from his estate.”
California’s Department of Health Services interprets section (b)(l)(A)
as applying only to institutionalized recipients whose estate or property
is subject to a lien, Department officials told us. Their recovery program,
they said, is operated under section (b)(l)(B), which limits recovery to
estates of recipients 66 years of age or older.
Officials from Oregon’s Estate Administration Unit also believed section
1917 precluded recoveries for recipients under age 66, but for a differ-
ent reason. They interpreted the section as requiring that
both
“A” and
“B” must be satisfied in order to recoyer. In other words, they believed
the individual had to be both institutionalized and over 66 years of age
before estate recovery could be done.
HHS
may have contributed to the confusion by its statement in the Fed-
eral Register notice
that
published the final regulations to implement the
lien and estate recovery provisions of TEFRA:
‘HCFA, Program Statistics, Medicare and
Medicaid Data Books, 1986, p. 86.
.
Page 23
GAO/HlUMM6 Medicaid E&ate Recoveries
Chapter 2
Significant Recovery of Nursin~~ Home Costa
Prom Estates Possible
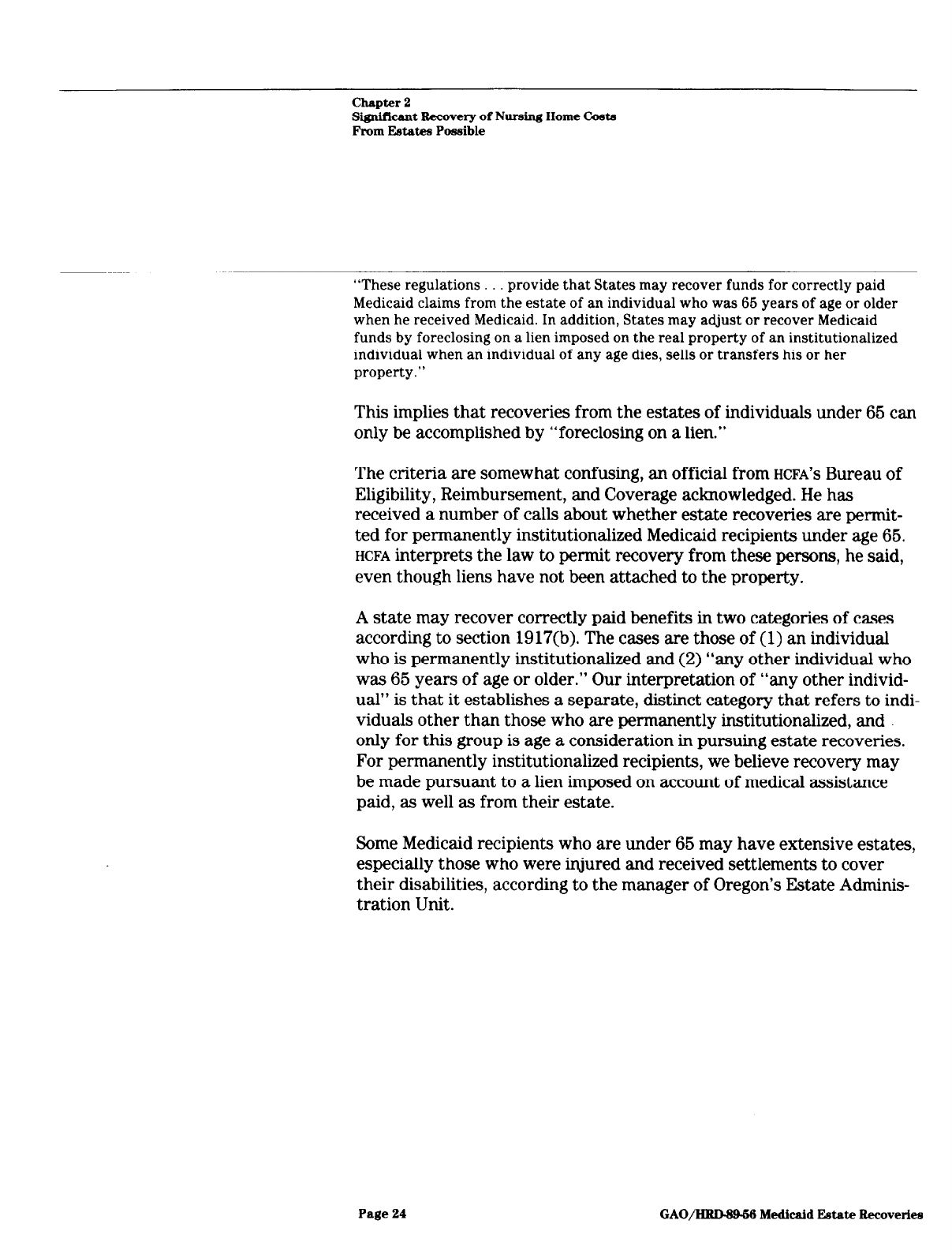
“These regulations. provide that States may recover funds for correctly paid
Medicaid claims from the estate of an individual who was 66 years of age or older
when he received Medicaid. In addition, States may adjust or recover Medicaid
funds by foreclosing on a lien imposed on the real property of an institutionalized
individual when an individual of any age dies, sells or transfers his or her
property.”
This implies
that
recoveries from the estates of individuals under 66 can
only be accomplished by “foreclosing on a lien.”
The criteria are somewhat confusing, an official from
HCFA’S
Bureau of
Eligibility, Reimbursement, and Coverage acknowledged. He has
received a number of calls about whether estate recoveries are permit-
ted for permanently institutionalized Medicaid recipients under age 66.
HCFA
interprets the law to permit recovery from these persons, he said,
even though liens have not been attached to the property.
A state may recover correctly paid benefits in two categories of cases
according to section 1917(b). The cases are those of (1) an individual
who is permanently institutionalized and (2) “any other individual who
was 66 years of age or older.” Our interpretation of “any other individ-
ual” is
that
it establishes a separate, distinct category that refers to indi-
viduals other than those who are permanently institutionalized, and
only for this group is age a consideration in pursuing estate recoveries.
For permanently institutionalized recipients, we believe recovery may
be made pursuant to a lien imposed on account of medical assistance
paid, as well as from their estate.
Some Medicaid recipients
who
are under 66 may
have
extensive estates,
especially those who were injured and received settlements to cover
their disabilities, according to the manager of Oregon’s Estate Adminis-
tration Unit.
Page 24
GAO/HRLWk% Medicaid Estate Recoverlea

Oregon Recovery Program an Example for
Other States
Although 21 states and the District of Columbia have active estate
recovery programs to recover correctly paid benefits, none has recov-
ered more per recipient than the Oregon program. Additional states are
in the process of implementing estate recovery programs. Still others,
according to the
HHS
Inspector General’s June 1988 report, are consider-
ing establishing or expanding such programs.
Despite the increasing interest in estate recovery programs,
HCFA
has lit-
tle information on them and, until recently, has provided limited techni-
cal assistance to states interested in establishing or improving a
recovery program. As a result, states have asked Oregon for technical
assistance. To get a better idea of why Oregon has been more successful
than other states in obtaining estate recoveries, we discussed with Ore-
gon officials and advocacy groups for the elderly the elements of the
Oregon program that they think are key to its success. The key elements
cited were (1) establishing enabling legislation, (2) maintaining flexibil-
ity in dealing with hardship cases, (3) securing recoveries from estates
of surviving spouses, (4) establishing a central recovery unit,
(6) appointing a conservator to handle incompetent recipients’ assets,
and (6) establishing an effective transfer-of-assets policy.
HCFA Provides
Limited Technical
Assistance
HCFA
headquarters and regional office officials have not obtained or ana-
lyzed data on estate recovery programs and, therefore, provide limited
technical assistance to states in establishing or improving recovery pro-
grams. HCFA'S
Central Office does not obtain information on the pro-
grams or take a proactive role in encouraging states to establish or
improve programs, according to an official from
HCFA'S
Bureau of Eligi-
bility, Reimbursements, and Coverage.
Similarly, officials from the five
HCFA
regional offices we visited said
that they knew which states had established recovery programs, but
lacked detailed knowledge of the scope and structure of the programs.
Although
HCFA'S
Seattle regional office conducted a study in 1986 of the
potential for estate recoveries in Idaho, the region had made no further
efforts as of December 1988 to encourage the establishment of recovery
programs.
As the implementation of the section 1917 provisions are optional,
HCFA
headquarters and regional office officials told us during the course of
our review that they do not believe it is
HCFA'S
responsibility to help,
encourage, or provide information to states regarding recovery pro-
grams. States should be on their own to set up programs and should
Page 26 GAO/HRD-SM6 Medicaid Estate Recoveries

Chapter 3
Oregon Recovery Program an Example for
Other States
obtain information on successful programs from each other, the officials
said.
In commenting on a draft of this report, however,
HHS
said that it plans
to take advantage of every appropriate opportunity to encourage states
not pursuing estate recoveries, or pursuing them ineffectively, to insti-
tute effective recovery programs.
HCFA'S
May 1988 State Agency Suc-
cessful Practices Guide contains a chapter on estate recoveries profiling
five states that have successful programs,
HHS
noted. The guide was dis-
tributed to all state agency heads, Medicaid directors, third-party liabil-
ity managers, the National Conference of State Legislatures, the
National Governors’ Association, and all
HCFA
regional offices, according
to
HHS.
In addition,
HCFA
has encouraged estate recoveries and the use of
the guide in several national meetings during 1988,
HHS
stated.
Other actions taken during 1988 to improve estate recoveries include
distribution of the
HHS
Inspector General’s comprehensive study on
states’ estate recovery programs to all state Medicaid agencies and
establishment of a departmental task force to evaluate the administra-
tive and regulatory changes needed to improve states’ estate recovery
programs,
HHS
noted.
These recent actions are a step in the right direction and should help
expand estate recovery programs. The successful practices guide, how-
ever, is, in our opinion, of limited usefulness to states wishing to estab-
lish or improve estate recovery programs. Specifically, the guide
discusses few of the key elements that help account for the success of
the Oregon program, and points out ways that the five “profiled” states
could improve their programs, such as by recovering from the estates of
(1) surviving spouses and (2) recipients who were under age 66 when
admitted to the nursing home. The Inspector General’s report, in our
opinion, provides more useful guidance to states wanting to establish or
improve recovery programs.
The Recovery Process
Oregon enacted legislation in 1949 authorizing the state to recover the
in Oregon
cost of state-provided cash assistance to the elderly. In 1976, legislation
was enacted authorizing recovery of the cost of medical assistance pro-
vided to persons 66 and older. In 1986, Oregon recovered $3.7 million,
and spent about $376,000 to operate the recovery program-a benefit-
to-cost ratio of 10 to 1.
Page 26 GAO/HRD-W56 Medicaid Estate Recoveries

chapter 3
Oregon Recovery Program an Example for
Other Statea
The recovery process can be broken into three parts: (1) identifying an
applicant’s assets, (2) tracking and preserving assets while assistance is
provided, and (3) recovering from the recipient’s estate.
Identifying Applicants’
Assets
A
recovery program depends on good information to identify assets held
or transferred by public assistance recipients. Oregon’s information
gathering
process routinely begins with the caseworker at the time indi-
viduals apply for food stamps or financial, medical, or social services
assistance (see fig. 3.1). During the application process, applicants or
their representatives are asked for information on real property, bank
accounts, or other assets currently held or disposed of within 2 years of
applying for assistance.
Page 27
GAO/HRDNM6 Medicaid Estate l&cove&a

Chapter 3
Oregon Reeovery Program an Example for
Other States
Figure 3.1: Oregon’s Recovery Process:
Identifying Assets
Persons apply for public assistance, including Medicaid, at branch offices of the
state’s Department of Human Resources. As part of the process, applicants or
their representatives fill out an application asking them to identify any property
(real property, bank accounts, and other assets) the applicants own or have
recently transfened.
Caseworkers in the branch offices review the applications and determine whether
applicants are eligible. The caseworker may verify
asset
information through
contacts with
l
applicant’s bank or banks
l
county assessor’s office (real property ownership)
l
county recorder’s office (real property transfers)
The applicant/recipient is required to notify the branch office or Area Agency on
1 could affe;ibillty . 1
Aging Dfffce within 10 days of any change in income, property, and the like, that
Each year, the applicant/recipient must complete
a
redetermination of eligibility
(same form
as
an application). The caseworker uses the form to determine
whether the applicant remains eligible.
The caseworkers screen each application to make sure that the neces-
sary information is provided and to determine whether the applicant
qualifies for assistance. The caseworkers may also follow up and verify
the information provided. For example, the caseworker might
contact
the county assessor’s office
to
verify information the applicant provided
on real property ownership. The data are then sent to Oregon’s Central
Recovery Unit, which uses the information for estate recovery purposes.
Page 28
GAO/IiRDWM Medicaid Estate Recoveries

chapter 3
Oregon Recovery Program an Ebmpie
for
other State6
Tracking and Preserving
Assets
Once identified, assets should be tracked to ensure that they are being
used to pay for the recipients’ care and not being given away to others.
In Oregon, caseworkers complete a property referral form and forward
it to the central state recovery unit when they identify applicants/recip-
ients who own or have recently transferred assets (see fig. 3.2). The
form contains information on real property, mobile homes, cars, boats,
and other assets, such as trust funds that the individual owns or has
transferred. Involving the recovery unit early helps the unit to better
track applicant&/recipients’ assets. If an individual is unable to manage
his or her own affairs, the state petitions the court to appoint a conser-
vator to assist the recipient.
Page
29 GAO/liBDWM Medicaid Estate Recawerh

Chapter 3
Oregon Recovery Program an Example for
Other States
Figure 3.2:
Oregon’s Recovery
Process:
Tracking and Preserving Assets
Caseworkers in the branch offices send property referral forms to the
Department’s centralized Estate Administration Unit when applications or case
reviews show the following:
l
The applicant/recipient has real property or other assets (such as a mobile
home, car, or trust fund) that may be lost or wasted due to the applicant’s
inability to manage them or confinement to a nursing home
a
The applicant/recipient has transferred real property to someone else within
2 years of applying for assistance
l
The applicant/recipient has a situation that the caseworker is unsure how to
handle
The Estate Administration Unit takes one or more of the following actions:
l
It files the information for later use in estate recovery efforts
l
If the applicant/recipient is unable to manage his or her own financial affairs,
it petitions the court to appoint
a
conservator to do so
l
If the applicant/recipient has transferred property without adequate
compensation, it offers these options to the affected parties:
- The applicant can be paid for the transferred property
-- The property holder can give the property back
-- The new property owner can sign an “open-end” mortgage giving the state
the right to recover assistance payments from the property after the
recipient dies
-- The state can determine that the applicant/recipient is ineliyible for
assistance for a period of time based on the value of the transferred
property
l
It advises the caseworker on an appropriate course of action
1
The caseworkers and estate administrators also want to prevent appli-
cants/recipients from giving away their assets without adequate com-
pensation. When they find that applicants or recipients have given away
assets at less than fair market value within 2 years of applying for
Medicaid or at any time after applying, Oregon gives the parties
involved three options to avoid a period of ineligibility:
Page 30
GAO/llMN&W Medicaid Estate Recoveries

Chapter 3
Oregon Recovery Program an Example for
Other States
l
The applicant/recipient can be paid an adequate amount for the assets.
This would make the money received available to pay for care before
the individual could become Medicaid-eligible.
. The property holder can void the transfer and give the assets back. This
step makes the assets available to pay for care before Medicaid eligibil-
ity is established or, in the case of exempt property, available for possi-
ble recovery of costs at a later date.
. In the case of real property, the property holder can sign an “open-end
mortgage” with the state. This mortgage allows the property holder to
keep the property. But under its terms, after the Medicaid recipient dies,
the property holder pays the state (up to the value of the property) for
the cost of care provided.
If the applicant/recipient and property holder do not agree to one of the
above actions, the applicant/recipient is declared ineligible to receive
Medicaid assistance for a period of time. At the time we completed our
review, if the fair market value of the asset minus the amount of com-
pensation received by the applicant/recipient is less than or equal to
$24,000, the period of ineligibility is 24 months. Should the uncompen-
sated value exceed $24,000, the number of months the individual is inel-
igible for assistance equals the uncompensated value divided by $1,000.
For example, if property worth $30,000 was sold for $2,000, then the
uncompensated value was $28,000. The period of ineligibility would be
28 months, or $28,000 divided by $1,000.
Recovering
Provided
for Care
Recovering From Living
Recipients
A process to recover from recipients’ assets the cost of care provided is
the final step in an effective recovery program. In Oregon, recoveries
can take place while the individual is receiving assistance or after the
individual dies. In addition, Oregon law allows recovery from the
spouse’s estate if the state did not recover from the recipient’s estate.
The state may recover from living recipients for care provided. This
generally occurs when a recipient owns a home but is living in a nursing
home and is not expected to return home, the recovery unit manager
said. If the home is sold, the proceeds are used to reimburse the state for
past care provided. Any remaining assets are held in trust and used to
pay for the recipient’s present and future care. When the recipient dies,
any money not used to defray Medicaid costs remains part of the estate
to go to the recipient’s heirs, according to the manager.
Page 31 GAO/HRD-3%56 Medicaid Estate Recoveries
Chapter 3
Oregon Recovery Program an Example for
Other States
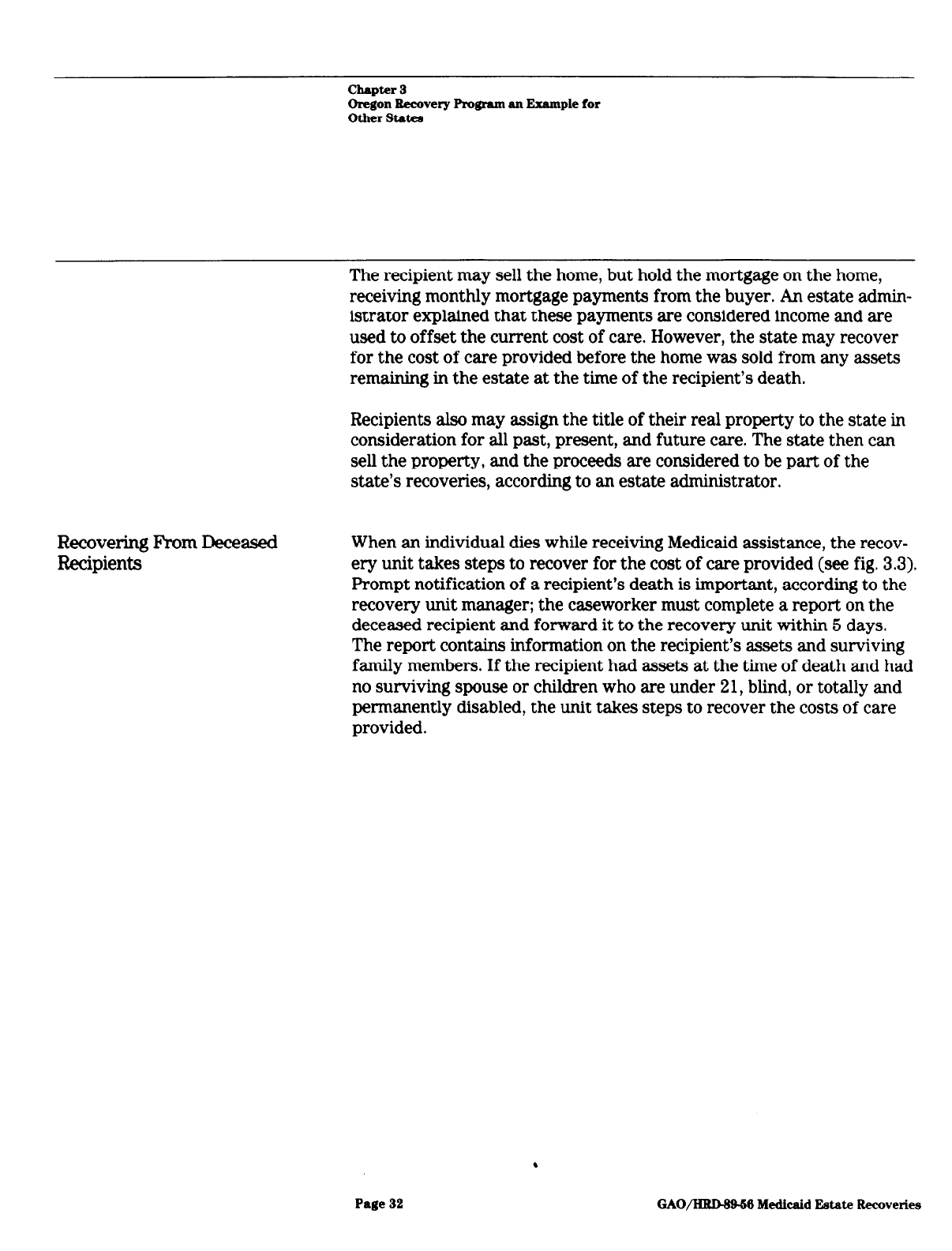
Recovering From Deceased
Recipients
The recipient may sell the home, but hold the mortgage on the home,
receiving monthly mortgage payments from the buyer. An estate admin-
istrator explained that these payments are considered income and are
used to offset the current cost of care. However, the state may recover
for the cost of care provided before the home was sold from any assets
remaining in the estate at the time of the recipient’s death.
Recipients also may assign the title of their real property to the state in
consideration for all past, present, and future care. The state then can
sell the property, and the proceeds are considered to be part of the
state’s recoveries, according to an estate administrator.
When an individual dies while receiving Medicaid assistance, the recov-
ery unit takes steps to recover for the cost of care provided (see fig. 3.3).
Prompt notification of a recipient’s death is important, according to the
recovery unit manager; the caseworker must complete a report on the
deceased recipient and forward it to the recovery unit within 5 days.
The report contains information on the recipient’s assets and surviving
family members. If the recipient had assets at the time of death and had
no surviving spouse or children who are under 2 1, blind, or totally and
permanently disabled, the unit takes steps to recover the costs of care
provided.
Page 32
GAO/ISWMBM Medicaid Estate Recoveries

Chapter 3
Oregon Remvery Program an
Example for
Other States
Recovering When Aasets Become
Available
Estates of persons on public Estates of persons not on public
assistance at the time of death assistance at the time of death
Caseworker sends a report on
deceased persons to the Estate
Administration Unit
l
notifylng the unit of
the recipient’s death
l
providing information
on available assets
l
providing information on
surviving spouse or children
If assets are available and no such
survivors remain, the Unit proceeds
If the estate is
not probated,
the Estate Ad-
ministration Unit
asks for pay-
ment from the
manager of the
estate or from
others who may
be holding the
recipient’s
assets
If the estate is
probated, the
Estate Admin-
istration Unit
files a claim
against the
estate for the
cost of care
provided
Branch offices submit monthly lists
of probate actions to the Estate
Estate Administration Unit reviews
the lists to identify deceased
persons who were
l
Former recipients. but not
receiving assistance at the
time of their death
l
Spouses of deceased recipients
Estate Administration Unit determines
whether
l
assets are available
l
the person is survived by a
spouse or by a child who is
under 21, blind, or totally
and permanently disabled.
If assets are available and no such
survivors remain, the Unit files
a
claim against the estate for
the cost of care provided.
I I
The recovery procedure the unit follows depends on
the amount
and
type of assets the recipient owned. If it appears that the estate will not
.
Page 33 GAO/HRDW56 Medicaid J2atat.e Recoveries

chapter 3
Oregon Recovery Program an JSxample
for
Other States
Recovering From Former
Recipients or Spouses
be probated because of the small value of the assets, the unit requests
reimbursement from the individual responsible for managing the recipi-
ent’s estate. Letters are also sent to the recipient’s banks and the nurs-
ing home, requesting that the recipient’s funds be forwarded to the
state. If a claim with a higher priority than medical expenses (funeral
expenses, for example) is filed against the estate, the state reimburses
the appropriate amount to the claimant from the money it receives.
If a recipient had assets of substantial value, the recovery unit asks the
recipient’s family to either repay the state for the public assistance pro-
vided (up to the value of the recipient’s assets) or probate the estate. If
the estate is probated, an estate administrator files a claim against the
estate in the county probate court for the value of the public assistance
provided. The state’s claim for public assistance would be paid from the
estate after the costs of administering the estate, the expenses of a
funeral (up to $1 ,OOO), and federal taxes are paid. The claims of heirs
are paid only after state claims are satisfied. According to Oregon’s
Estate Administration Unit, if there are sufficient assets in the estate
but no person with a higher preference is willing to become the personal
representative of the estate, the unit will petition the court to nominate
a personal representative.
Oregon also has a system to identify and recover from individuals who
received Medicaid or other assistance in the past, even if they were not
receiving assistance at the time of death. To identify these former recip
ients, the unit reviews monthly lists of probate court actions sent by
each branch office. If a former recipient is found and has no surviving
spouse or a child who is under 21, blind, or disabled, the unit calculates
the amount of public assistance and files a claim against the individual’s
estate in the probate court.
The state is also authorized to recover from the estate of a deceased
recipient’s spouse if both the recipient and the spouse are deceased and
there are no surviving children under 21, blind, or disabled. For exam-
ple, when a recipient dies but is survived by a spouse, the unit takes no
action to recover any funds at that time. Instead, the unit fills out a data
card on the spouse as a basis for later recovering from the spouse’s
estate when he or she dies. Each month, the county probate lists are
reviewed and compared with the list of spouses to see if any have died.
If there is a match, the state files a claim against the estate for public
assistance provided to the husband, wife, or both.
Page 34
GAO/HRDM-M Medicaid Estate Recoveries

-
chapter 3
Oregon Recovery Program an Example for
Other States
Key Elements of
Oregon’s Recovery
Program
There are several features of the Oregon program
that
help account for
its success and acceptance by Medicaid recipients. These elements are
discussed below.
Element 1: Oregon Enacted
Oregon enacted laws specifically authorizing
the
recovery program and
Laws Authorizing Estate
establishing the conditions under which recoveries will be authorized.
Recoveries -
Two of the states included in our review, Pennsylvania and Michigan,
said that their attempts to operate estate recovery programs administra-
tively were blocked by legal challenges. In Pennsylvania, a state attor-
ney told us that a class action suit brought against
the
state caused the
state to disband its recovery program because recovery was not permit-
ted under existing state law, and that, under section 1917, recovery was
optional, not required. Similarly, Michigan discontinued its estate recov-
ery program because of a binding opinion issued by the state’s Attorney
General concluding that the state could not recover because state laws
did not specifically authorize it.
As discussed on page 26, Oregon law has authorized estate recoveries
since 1949; specific legislation authorizing recoveries from the estates of
Medicaid recipients 65 years of age or older was enacted in 1975. Other
Oregon laws authorize recovery of cash assistance provided by Oregon’s
Adult and Family Services Division and certain assistance provided to
the blind or disabled. Other laws give the state a priority claim against
the estate, authorize
the
appointment of a conservator to ensure
the con-
tinued availability of assets, and authorize recoveries from
the
estates
of surviving spouses.
Element 2: Oregon
Maintains Flexibility in
Dealing With Hardship
Cases
Oregon has allowed sufficient flexibility to ensure
that estate
recoveries
do
not
create undue hardships on the recipient’s heirs, according to
advocacy groups for the elderly in the state.
In designing their Medicaid programs, states should strike a balance
between the needs of Medicaid recipients and their heirs and the needs
of the government to contain Medicaid spending. Officials from Michi-
- gan and Pennsylvania told us that
they
had not considered establishing
recovery programs by law because of expected political pressure from
special interest groups concerned about the effect recovery legislation
would have
on
the desire of
the
elderly to leave an estate. For example,
.
Page 36
GAO/llRMB-M Medicaid Estate Recoveries

chapter 3
Oregon Recovery Program an Example for
Other States
a Pennsylvania official told us that legal services and welfare rights
advocacy groups were active in the state and that the legislature was
not likely to approve such a program. Similarly, an Ohio official told us
that the Ohio legislature did not fund a recovery program.
Although Washington enacted recovery legislation in 1987, the scope of
the program was narrowed because of political sensitivity during delib-
erations. An early proposal would have permitted recovery from the
estates of any deceased Medicaid recipient without a surviving spouse
or dependent child. However, after hearings on the bill, it was amended
to exempt recoveries for property valued below $50,000 if there are any
children, regardless of age.
We contacted several organizations in Oregon that provide services to
senior citizens or act as advocates for seniors, including the Gray
Panthers, United Seniors, and the Legal Aid Service-Senior Law Project.
A volunteer for the Gray Panthers, who serves as the vice chairperson
for United Seniors, a coalition of senior service groups, said he had
never heard anyone complain about the estate recovery effort. Accord-
ing to the staff attorney for the Senior Law Project in Portland, the state
has been flexible in cases where recovery would cause a hardship for
recipients’ adult children or siblings.
We also discussed estate recovery with national representatives of
AARP
and the Gray Panthers.
AARP
has not established a formal policy position
on estate recoveries, a legislative representative said, but is not opposed
to the concept. She said that the program should be administered in a
way that it does not intimidate people, minimizes confusion, and pro-
tects the interests of caretakers of the elderly. The concept of liens
frightens people, she added.
The Gray Panthers do not have a national policy on estate recoveries
under Medicaid, an official said, but she had serious questions about
having long-term care coverage provided under Medicaid. As long as
long-term care is provided under Medicaid, however, it should be uni-
form in all states, she said. It is not fair, in her view, that some adult
children inherit from their parents and others do not.
As discussed above, advocacy groups for the elderly within Oregon
think that the Oregon program allows sufficient flexibility to protect the
interests of caretakers and the program has accomplished recoveries
without the use of liens.
Page 36 GAO/l%l?DS9-56 Medicaid Estate Recoveries

Chapter 3
Oregon Recovery Program an Example for
Other States
Element 3: Oregon
Authorized Recoveries
From the Estates of
Surviving Spouses
Oregon increased its recoveries by enacting a law to authorize recoveries
from the estates of surviving spouses.
Because about one-third of Medicaid nursing home residents we sampled
who owned a home had a spouse, and recoveries are allowed only when
there is no surviving spouse, a significant portion of potential recoveries
is lost unless a state authorizes recoveries from the estates of surviving
spouses.
A state can recover from the estate of the surviving spouse only if it has
enacted a law authorizing such recovery. Nothing in the federal Medi-
caid statute explicitly authorizes or forbids recovery from the estate of
the surviving spouse. Section 1917(b) prohibits recovery of correctly
paid Medicaid benefits except from the estate of the Medicaid recipient
and provides that recovery “may be made only after the death of the
individual’s surviving spouse.” Although the statute does not provide a
clear basis for a state to proceed against the surviving spouse’s estate,
one state court-the only court we found that has addressed an issue
relevant to this question- construed section 1917(b) as not prohibiting
recovery from the estate of a surviving spouse.’
Oregon law allows the state to recover from the estate of the spouse
after both the recipient and the spouse are deceased and there are no
children under age 21, blind, or disabled. Of the $3.8 million in potential
recoveries we identified for recipients admitted to Oregon nursing
homes in 1986, we estimate that about $600,000 will come from the
estates of married recipients. In the other seven states, we identified
about $46.4 million in potential recoveries from the estates of married
recipients.
Element 4: Oregon
Established a Central
Recovery Unit
To facilitate recoveries and reduce administrative costs, Oregon estab-
lished a central unit to administer estate recoveries for all programs.
One concern expressed in nonrecovery states was the cost effectiveness
of recovery programs. For example, an Ohio official believed that the
administrative costs of recovery would outweigh any recoveries. One
‘Matter of Estate of Imburgia, 487 N.Y.S. 2d 263 (SW. Ct. 1984). In this case, the State of New York
had a statute authorizing recovery from the estate of a responsible relative (such as the surviving
spouse). The court, faced with the question of whether the New York statute was invalid because it
conflicted with section 1917(b), found no conflict. The executors of the estate had argued that since
section 1917(b) provided no recovery except against the estate of the recipient, it implicitly prohib
ited recovery against the estate of a responsible relative.
Page 37 GAO/~S# Medicaid Estate Recoveries

Chapter 3
Oregon Recovery Program an Example for
Other States
Wisconsin official was hesitant to establish an estate recovery program,
she said, because such programs do not always receive prompt notice of
a Medicaid recipient’s death and would have difficulty submitting
claims in time for probate.
Oregon established a central recovery unit, known as the Estate Admin-
istration Unit. The unit recovers for services provided through the Men-
tal Health Division, the Adult and Family Services Division, and the
Senior Services Division. Approximately 96 percent of the recoveries are
for services provided to those 66 years of age or older through the
Senior Services Division, according to the program manager. By estab-
lishing a central unit, the state avoids the expense of operating separate
units for each recovery program.
The Estate Administration Unit has a staff experienced in legal, prop
erty, and probate transactions. A manager heads the unit and is assisted
in carrying out the estate recovery process by three estate administra-
tors. All four positions require a law degree or an equivalent back-
ground in law and experience in real property transfers, probate laws,
and interpreting wills and assets. A clerical staff of five and a resource
coordinator assist the administrators.
Element 5: Oregon
To protect both the interests of the recipient and the state, Oregon peti-
A ---:-Cm “ons&vators for tkypurr LL3 b
tions the court to appoint conservators to manage the financial affairs
Incompeter It Recipients
of recipients who are mentally or physically unable to manage their own
affairs.
Oregon law allows the state to petition the court for the appointment of
a conservator to assist a recipient if the individual is unable to handle
his or her affairs due to physical or mental illness. The individual’s
caseworker, with the assistance of the physician, nurse, or nursing home
administrator, determines whether a recipient is competent to manage
his or her own affairs. The property referral form provides the recovery
unit with the information, such as the amount and type of assets,
needed to file the court petition.
Page 38 GAO/‘HUNWM Medicaid Estate Recoveries

Chapter 3
Oregon ltemvery Program an Example for
Other States
Element 6: Oregon
To help ensure that a recipient’s assets are not sold or given away
Maintains an Effective
before the state can recover, Oregon established an effective transfer-of-
Transfer-of-Assets Policy
assets
policy.
Oregon has enacted laws that empower the state to void transfers of
real or personal property when the recipient did not receive adequate
payment. As discussed on pages 30 and 31, Oregon provides recipients
several options when an illegal transfer has occurred. These options
help ensure that the recipient’s available resources remain available to
pay for his or her care.
Page 39
GAO/ERD-69-56
Medicaid Estate Recoveries

Chapter 4
Conclusions, Matters for Consideration by the
Congress, and Agency and State Comments
Conclusions
Estate recovery programs increase equity by requiring all Medicaid
nursing home recipients to apply their assets equally toward the cost of
their care. In those states without an estate recovery program, only
those recipients who own a home at the time of death are allowed to
leave an estate. Recipients with savings, but not a home, are forced to
apply those savings toward the cost of care. Several benefits offered by
estate recovery programs are that they
. help to keep the Medicaid program focused on its intent. In all 50 states,
a Medicaid recipient who sells assets while alive must use the proceeds
to pay for care. Forty-nine states have laws prohibiting recipients from
avoiding this requirement by transferring assets without compensation.
Without a recovery program, however, a state has no mechanism for
receiving compensation after a recipient has died leaving no spouse or
blind, disabled, or dependent child.
. can be structured so as to recover costs without placing undue hard-
ships on the elderly. A recovery program like Oregon’s demonstrates
that the interests of the state and the elderly and their heirs can be
served. Institutionalized recipients need not give up their homes to
receive benefits when they or their spouses are alive. In most cases,
recovery is initiated only after the death of the recipient and the recipi-
ent’s spouse.
l
can more than pay for themselves. In 1986 Oregon’s program recovered
$10 for every $1 spent on the program. From a financial standpoint, the
cost and effort involved in setting up a recovery program appear to be
justified.
l
help to meet future financial strains on the government’s health care
efforts. In the near future, the number of older Americans will grow
rapidly, and this growth likely will bring an increased demand for nurs-
ing home care. Recovery programs can help ease the strain on already
limited government resources.
HHS should do more to promote the establishment and improve the effec-
tiveness of estate recovery programs. Specifically, the Department, in
preparing the required report to the Congress on the means for recover-
ing the cost of Medicaid services from the estates of institutionalized
recipients, should develop a legislative proposal that would require
states to establish estate recovery programs. In addition, the report
should include information on effective estate recovery practices,
including recoveries from spouses’ estates and estates of recipients
under age 66 if they received Medicaid assistance.
.
Page 40
GAO/HRD-Sg-S6 Medicaid Estate Recoveries

Chupter 4
Conclusioos, Matters for Consideration by
the Congress, and Agency and
State Comments
Matters for
The Medicare Catastrophic Coverage Act of 1988 makes mandatory the
Consideration by the
provisions of the Tax Equity and Fiscal Responsibility Act of 1982 per-
taining to restrictions on transfers of assets for less than fair market
Congress
value and extends the restriction period on transfers from 24 to 30
months.
GAO
believes the Congress should consider making mandatory
the establishment of programs to recover the cost of Medicaid assistance
provided to nursing home residents of all ages, from either their estates
or the estates of their surviving spouses. The establishment of such pro-
grams would help to ensure that assets preserved through the new
transfer-of-assets provisions can be used to defray Medicaid costs.
HHS Comments and
Our Evaluation
HHS
said that it generally agreed that estate recovery programs
have
potential to offset Medicaid costs (see app. II). But it said our legislative
proposal should be more specific, better justified, and address the
appropriate balance between state flexibility and detailed federal
requirements.
While states should retain flexibility in designing their recovery pro-
grams, we believe certain minimum requirements should be established
at the federal level. As
HI-B
correctly notes in its comments, states have
not taken full advantage of the authority to establish estate recovery
programs that has existed for over 20 years. And, when recovery pro-
grams have been established, they have sometimes contained such
severe restrictions that only limited recoveries are possible. For exam-
ple, as discussed on pages 22 and 36, Washington’s estate recovery pro-
gram is structured to recover only a small fraction of the assets
available, the remainder going to the surviving children, even if they
have reached adulthood. Accordingly, we believe that estate recovery
programs should include provisions for (1) recovering Medicaid costs
from estates of recipients of all ages, not just those over 65, (2) recover-
ing from the estates of surviving spouses, and (3) establishing the Medi-
caid program as a creditor whose claims against the estate have priority
over those of heirs other than the surviving spouse or dependent child.
States should, in our opinion, retain the flexibility to design the recovery
process with
HCFA
oversight to help ensure that those processes are
effective in identifying, tracking, and recovering assets from recipients’
estates or the estates of their surviving spouses.
Mandating estate recoveries would,
HHS
said, amend national policy on
such fundamental issues as the disposal of homes of the elderly, the
intergenerational transfer of wealth, and the traditional authority of
states to set probate policy. Because of these fundamental public policy
Page 41
GAO/IBtD6966 Medicaid Estate Recoveries

Chapter 4
Conclusions, Matters for Consideration by
the Congress, and Agency and
State Comments
issues,
HHS
said that it favors a two-pronged approach. First,
HHS
would
encourage broad public discussion in the Congress and other appropri-
ate forums on the complex underlying issues affecting estate recovery
programs. Second,
HHS
would pursue limited legislative, regulatory, and
program management change to enhance program effectiveness. The
program management aspects are, according to
HHs,
being addressed by
HCFA,
and the legislative and regulatory aspects will be addressed in the
departmental study.
We agree that the issues surrounding estate recovery programs are
politically sensitive and that the Congress is an appropriate public
forum to debate those issues. We also believe, however, that
HHS, as
the
federal agency responsible for administering the Medicaid program,
should assume a leadership role in that debate.
Further, the fundamental issues to which
HHS
alludes were to a large
degree decided by the Congress through TEFF& As
HHS
noted in its imple-
menting regulations, the TFZRA provisions are “. . . intended to assure
that all of the resources available to an institutionalized individual,
including equity in a home, which are not needed for the support of a
spouse or dependent children, will be used to defray the costs of sup-
porting the individual in the institution.” Therefore the future debate
should focus more on the best way to (1) ensure that those resources are
used to defray Medicaid costs and (2) eliminate the inequity that exists
in those states that do not have effective recovery programs. Current
law generally allows the intergenerational transfer of wealth by Medi-
caid nursing home residents only in those states that do not have an
effective estate recovery program and then only if the recipient still
owns the home at the time of death. Mandating estate recoveries would,
in our opinion, address both issues.
With respect to
HHS'S
comment that mandating estate recoveries would
alter the traditional authority of the states to set probate policy, we are
proposing no fundamental change in this authority. The action we sug-
gest would give the Medicaid program the right to settle claims against
the estates like other creditors.
HIB said that we did not specially address the difficult issue of how to
recover Medicaid costs from surviving spouses’ estates, and said that
there will be instances where the spouse outlives the Medicaid recipient
by many years, moves to a different house or different state, or remar-
ries. As discussed on page 49, we recognized that Medicaid may not be
Page 42 GAO/HiUNB-SB Medicaid Estate Recoveries

Chapter 4
Conclusions, Matters for Consideration by
the
Congress, and
Agency and
State Comments
able to collect 100 percent of Medicaid costs in these cases, and in mak-
ing our savings estimates, we used only 50 percent of the value of the
real property available to offset Medicaid costs. An Oregon official said
that Oregon has successfully collected from the estates of surviving
spouses and some states, including California, see promise in expanding
or changing their programs to increase potential recoveries.
Potential recoveries are overstated because of changes in the transfer-
of-assets rules mandated by the Medicare Catastrophic Coverage Act,
HI-IS
maintains. Our estimates were based on home ownership at the time
of Medicaid application for a sample of recipients admitted to nursing
homes in 1985. Because the transfer-of-assets provisions of the Medi-
care Catastrophic Coverage Act apply only to resources disposed of on
or after July 1, 1988,
they
would
have
little effect on the savings projec-
tions for our sample population. For those admitted to nursing homes in
the future, however, we believe the act will increase, not decrease,
potential recoveries. First, as discussed on pages 13 and 14, the spousal
impoverishment provision of the act will make it easier for middle-
income elderly to qualify for Medicaid by requiring states to exclude
more income and resources in determining eligibility if there is a nonin-
stitutionalized spouse. Because home ownership generally increases
with income, the potential for estate recoveries should also increase.
Second, by extending the restriction on transfers of assets to 30 months,
the act should help ensure that more assets remain available for even-
tual recovery.
HHS also stated that our savings estimates are based on the assumption
that each state could perform as effectively as Oregon.
HHS
does not
believe that larger states could achieve the same percentage savings
that Oregon realized. Our savings estimates were based on actual cases
reviewed in each state, not on savings projections for Oregon. As shown
on pages 19 to 22,
the
potential recovery in
each
state was based on the
percentage of Medicaid recipients who owned homes, the average value
of the homes, and the estimated Medicaid payments for those recipients.
The potential percentage savings depends on those factors, not on the
size of the state. California, for example,
has
demonstrated
that
a large
state can operate an effective estate recovery program. Recoveries
under California’s program have increased from about $130,000 in 1981
to a projected $25 million in fiscal year 1989. As California recognizes in
its comments on this report, its recoveries could be increased if it
expanded its program to recover from
the
estates of recipients under
age 65 and from the estates of surviving spouses.
Page 43 GAO/HRD-W66 Medicaid Estate Recoveries
Chapter 4
Conclusions, Matters for Consideration by
the Congress, and Agency and
State Chnmenta
State Officials’
Comments and Our
Evaluation
Comments were received from seven (California, Michigan, Ohio, Ore-
gon, Pennsylvania, Washington, and Wisconsin) of the eight states
included in our review. Generally, the states agreed with our findings
and indicated that they would consider establishing or expanding estate
recovery programs. Comments had not been received from Texas at the
time this report was finalized.
California
The Deputy Director of Medical Care Services within California’s
Department of Health Services (see app. III) said that California prides
itself as being a leader in estate recoveries and expects our report to
help it in implementing some new processes. Specifically, the state is,
according to the deputy director, preparing legislation to enable it to
recover from the estates of (1) surviving spouses and (2) recipients who
received nursing home services before age 65. California also hopes to
further increase recoveries, which have grown from $130,128 in 1981 to
a projected $25 million in fiscal year 1989, by providing further training
at the county level to clarify the state’s authority to file property liens
against long-term-care beneficiaries (at any age) that declare no intent
of returning home under current state laws.
Michigan
Based on the facts and recovery potential, Michigan will, according to
the governor, (see app. IV) be exploring the possibility of implementing
an estate recovery program. Michigan has not, the governor noted, had a
statutory basis for a recovery program during the past 10 to 15 years.
How well Oregon has done by enacting legislation specifically authoriz-
ing estate recoveries is interesting to note, the governor said.
With the clarification of federal intent in TEFRA and the Medicare Cata-
strophic Coverage Act of 1988, it would appear, the governor said, that
many states will be addressing recovery potential. There is a potential
for recovery of $7 to $9 million after a program is developed and opera-
tional, according to the governor.
Ohio
Ohio (see app. V) substantially agrees with our conclusions that estate
recovery programs would increase equity, be cost effective, and help
meet future financial strains on the government’s health care efforts,
according to the Director of Ohio’s Department of Human Services.
HCFA
must take a more active leadership role in assisting the states with the
development of estate recovery programs and should, according to the
director, begin developing a legislative proposal that would provide a
Page 44
GAO/IUD&66 Medicaid Estate Recoveries

Chapter 4
Conch~~io~, Matters for Consideration by
the Congress, and Agency and
SW.82 Comments
more uniform program without the ambiguous language that currently
exists as illustrated in section 1917(b) (see p. 23).
The director said that Ohio foresees having many more problems in
implementing an estate recovery program than Oregon had. The Oregon
program has, she noted, been operational for 25 years. She saw this as
meaning that advocacy groups may have a different perspective on the
programs in Oregon than the advocacy groups in Ohio. In addition, Ohio
would face initial costs associated with development of an estate recov-
ery program. Finally, Oregon has a state-administered program that
allows it to administer the program from a centralized system, while
Ohio has a county-administered system that places much of the burden
on local county offices. These factors may, in the director’s opinion,
reduce the cost-benefit ratio.
We agree that the factors the director cites could reduce the cost-benefit
ratio. For example, we recognize on page 36 that when Washington
enacted recovery legislation in 1987, the scope of the program and
potential recoveries were reduced during the deliberations because of
the political sensitivity of the issue. We also discussed the views of
national representatives of
AARP
and the Gray Panthers, groups that
could help distill the political sensitivity of the issue if
HCFA
and the
states work with them in developing their programs.
While start-up costs may, as the director suggests, reduce the initial
cost-benefit ratio, the experience of California shows that an estate
recovery program can soon pay for itself. As California noted in its com-
ments, recoveries have grown from about $130,000 to an estimated $25
million during the first 8 years of the program. Finally, while having a
county-administered Medicaid program may make it more difficult to
administer certain aspects of an estate recovery program, it might facili-
tate other aspects, such as review of probate court actions and identifi-
cation of real property transfers. Other states with locally administered
Medicaid programs, such as New York, may be able to assist Ohio in
structuring an effective recovery program. And, as the director notes,
HCFA
should take a more active role in assisting states with the develop-
ment of estate recovery programs.
Oregon
The Governor of Oregon (see app. VI) said that Oregon looks forward to
the challenge of maintaining its national leadership in the area of estate
recoveries. Its goal, the governor said, is to increase estate recoveries
while protecting the personal and property rights of the people it serves.
.
Page 46
GAO/HBDs986 Medicaid Estate Recoveries
Chapter 4
Conclusions, Matters for Consideration by
the
Congress, and
Agency and
State Comments
The program aggressively corrects disqualifying transfers of assets and
is active in the preservation of assets so they may be available for the
current cost of care as well as the estate. The governor expressed a will-
ingness to continue to provide assistance to other states interested in
implementing estate recovery programs.
Pennsylvania
The Deputy Secretary for Administration of Pennsylvania’s Department
of Public Welfare (see app. VII) said that although Pennsylvania did not
agree with all the information in our report, it believes that establishing
an estate recovery program is a viable option that will be given further
consideration. Current state law does not, the deputy secretary said,
allow for recovery of properly received benefits. Medicaid should not,
he said, be forced to carry the burden of providing nursing home care
while enlarging the estates of some recipients.
While the Deputy Secretary agreed that there could be increased reve-
nues generated from operating an estate recovery program, he said that
Pennsylvania did not necessarily agree with some of the assumptions
used to calculate the probable dollar value of an estate recovery pro-
gram in Pennsylvania. Specifically, he questioned our assumption that
one-half of the market value of the home of married couples would sub-
sequently be available from the estate of the spouse living outside the
nursing home. The Deputy Secretary said that he suspects that this
assumption is not practical in Pennsylvania and that the dollars recov-
ered would probably be less than the $8.5 million we estimated.
As discussed on page 49, making accurate estimates of potential recov-
eries from spouses’ estates was a problem because we had
no
way of
knowing how much longer the spouse would live and what the estate
would be worth at the time of death. Based on the success in recovering
from spouses’ estates reported by Oregon, we continue to believe our
assumptions are reasonable, particularly considering the conservative
approach followed in estimating the percentage of the property value to
offset against Medicaid costs.
Washington
The Governor of Washington (see app. VIII) said that Washington is con-
fident that its recently enacted estate recovery program will develop
into a cost-effective program, although recoveries to date have been less
than originally projected. The scope of the program was, the governor
noted, limited to the filing of property liens or creditor claims after the
death of medical assistance recipients who were older than 65 years of
Page 46
GAO/HRD-8B-66 Medicaid Estate Recoveries
Chapter 4
Conclusion, Mattera for Chuidemtion by
the Congress, and Agency and
State Commenta
age and to estates valued in excess of $50,000 unless there were no close
surviving relatives. An amendment to reduce the $50,000 exemption to
$35,000 is, according to the governor, being proposed for the 1989 legis-
lative session.
As discussed on page 22, the limitations on the Washington recovery
provisions will reduce projected recoveries from $7 million to $218,000.
We believe Washington should consider making the Medicaid agency
coequal with other creditors of the estate by eliminating the $60,000
exemption for estate recovery.
Wisconsin
The Secretary of Wisconsin’s Department of Health and Social Services
(see app. IX) said that Wisconsin has done considerable research in the
area of estate recovery since we began our review and now believes that
an estate recovery program operated with flexibility and a high degree
of sensitivity to the needs of the elderly and their families can accom-
plish recovery goals without intimidation and confusion. Statutory lan-
guage has, the secretary said, been proposed that would permit the state
to recover Medicaid expenditures from an estate when there is no sur-
viving spouse, minors, or disabled children.
Page 47 GAO/HRD-&M Medicaid IZutrte Recoveries

Methodology Used to Determine Potential
Recovery for Medicaid Recipients Who Own
Real Property
This appendix explains the methodology we used to estimate potential
estate recoveries in eight states (California, Michigan, Ohio, Oregon,
Pennsylvania, Texas, Washington, and Wisconsin). We limited our
review to determining the Medicaid costs that could be defrayed using
recipients’ real property because
l
the home is the primary asset of most older individuals;
. the value of real property is public information obtainable from the
county assessor’s or treasurer’s offices; and
l
information on liquid assets, such as bank accounts, is difficult to obtain
because of privacy concerns.
For the first 200 recipients from a random sample of 500 Medicaid nurs-
ing home recipients in each of the eight states, we obtained their Medi-
caid applications and/or subsequent redetermination of eligibility.’ The
universe for our samples consisted of all Medicaid nursing home recipi-
ents who were 66 years of age or older in 1986 and from whom the first
Medicaid payment was for nursing home services provided in calendar
year 1985. We determined whether the recipient was deceased and if so
obtained the date of death. For recipients with real property we
obtained the number of days of care or dates showing when nursing
home care was provided and the actual Medicaid payments in 1985 and
1986.
We reviewed the data obtained for the 1,600 recipients (200 records in
each of the eight states). If the application indicated that the recipient
owned real property,” we contacted the appropriate county assessor’s or
treasurer’s office to obtain the value of the property. If we were unable
to determine clear property ownership or the value of the real property,
we excluded the case from our calculation of potential recoveries.
Where the recipient had a life estate, we also excluded the case. Life
estates occur when recipients have transferred their real property but
‘For recipients whose Medicaid eligibility was established as a result of SI eligibility, we obtained
the SSI application from the Social Security Administration.
‘Of the 228 property owners in our samples, 16 (7 percent) indicated on their Medicaid applications
that they were making mortgage payments. Nine of the 16 were from our Oregon sample. An Oregon
official said that the higher number of mortgages identified in the Oregon sample could be due either
to the thoroughness of the Medicaid application process in Oregon or to the reporting of payments for
state or federal loans for weatherproofing homes as mortgage
payments.
Because the projected value
of the property in our samples was over twice the estimated Medicaid payments, we assumed that the
homeowners had sufficient equity in the home to help defray Medicaid costs. Accordingly, we did not
attempt to determine the amount of the outstanding mortgage for the 16 homeowners. Rather, we
assumed that the entire value of the property was available to defray Medicaid costs.
Page 48
GAO/HRDJBM Medicaid Estate Recoveries

Appendix I
Methodology Used to Determine Potential
Recovery for Medicaid Recipienta Who Own
Real propem
retained the right to possess and use the property until death. While we
counted these recipients as property owners, we excluded
them
from
our recovery projections as they do not represent recovery potential.
To determine which property value to use for our estate recovery pro-
jections we developed the following priority order:
1. Actual sales price, as this should be
the most
accurate indication of
the fair market value.
2. Fair market value from the city or county assessor’s, treasurer’s, or
auditor’s office.
3. Appraised value as determined by a real estate appraisal company.
4. Assessed value from the office of the city or county assessor’s, trea-
surer’s, or auditor’s office. (In some locations this was the same as the
fair market value.)
5. Value based on discussions with the caseworker.
6. Value stated in the Medicaid application.
We estimated the recovery potential based on the laws and procedures
used for estate recovery in Oregon. When we had questions, we
con-
sulted
with
the manager of Oregon’s Estate Administration Unit. The
following assumptions were used in certain circumstances we
encountered:
1. With respect to married recipients, Oregon allows recovery from the
estate of a deceased recipient’s spouse, and we wanted to include this
potential amount in our projections. Yet making accurate estimates was
a problem, as we had
no way
of knowing how much longer the spouse
would live and what the estate would be worth at the time of death. We
decided to assume that in cases where a Medicaid recipient was married,
50 percent of the value of
the
real property would be available to offset
the cost of care. Our logic was that in some cases the full cost of the
Medicaid care would be recovered and in other cases nothing would be
recovered.
2. Where property was jointly owned by two unmarried individuals, we
also assumed that 50 percent of the value of the property would be
available to offset
the cost
of care.
Page 49 GAO/HRD-6956 Meditid Estate Recoveries
Appendix I
Methodology Used to Lkternhe Potential
Recovery for Medicaid Recipients Who Own
-Roperty
3. Where property was owned by more than two individuals, we did not
count the property as potentially recoverable. We decided that although
a state might be able to recover the property, if it was jointly owned by
more than two parties it should not be considered an available resource
for the recipient.
4. Where the deed included a “right of survivorship” clause, we did not
deem jointly owned property as a recoverable asset. In these cases,
when one of the owners died, the property would pass directly to the
other owner and would not be included as part of the decedent’s estate,
Oregon’s Estate Administration Unit manager said. As this property
would not be part of the decedent’s estate, it would not be available for
recovery.
After we determined the value of the recipient’s share of the real prop-
erty, we multiplied the value by 80 percent. We did this because a por-
tion of the estate would be used to pay such estate expenses as real
estate agent and attorney fees and, consequently, would not be available
to defray Medicaid costs. Oregon’s Estate Administration Unit manager
agreed with this approach.
Before we could make projections we had to determine the amount of
Medicaid claims paid for each recipient who owned real property.
Whenever possible, we attempted to use actual payment amounts. From
the states, we determined actual payments made in calendar years 1985
and 1986. We then compared the value of the real property available to
defray Medicaid costs (i.e., 80 percent of the recipient’s share of the
property) and the Medicaid payments, as follows.
1. If the recipient was deceased, the potential recovery was the lesser of
the value of the real property or the Medicaid claims paid.
Example: One recipient was a widower who owned real property valued
at $27,386, of which $21,908 was available for recovery after allowing
20 percent for real estate and attorney fees. The recipient died in May
1986. All the Medicaid costs, totaling $10,937, could have been recov-
ered from the recipient’s estate.
2. If the recipient was alive but no longer in a nursing home, we com-
pared the value of the real property and the Medicaid costs and took the
lesser of the two.
Page 60
GAO/HRD4&56 Medicaid Estate Recoveries

Appendix I
Methodology Used to Determine Potential
Recovery for Medicaid Reclpienta Who Own
Real property
3. If the recipient was alive and was in a nursing home for most of 1986,
we assumed that the individual would be in a nursing
home
the rest of
his or her life.
a. If the value of the real property was less than actual costs incurred,
we assumed the recoverable amount was equal to the value of the
wwW
b. If the value of
the
property was greater than actual Medicaid costs
paid in calendar years 1986 and 1986, we estimated the additional
potential recovery, using a computer program that incorporated life
expectancy tables. The additional potential recovery was calculated
from five factors:
recipient’s age on January 1,1987,
recipient’s sex,
actual Medicaid costs paid for him/her in 1986 and 1986,
average daily Medicaid cost for him/her in 1986, and
value of the recipient’s property available for recovery.
Example: One recipient in our sample was a widow who owned real
property valued at $43,630. After deducting 20 percent to pay for any
legal or real estate agent fees, the value of the property available to
defray Medicaid costs was $34,904. The recipient was in
the
nursing
home
on
Medicaid most of 1986 and all of 1986. Her Medicaid payments
totaled $17,370. It appeared
that
she would spend the rest of her life in
a nursing home. Because her Medicaid costs to date were less than the
value of her property, we needed to estimate the additional costs that
could be recovered. Using a computer program that factored in the
recipient’s age, sex, actual 1986 and 1986 Medicaid costs, daily cost in
1986, and value of property, we estimated that $14,674 more in Medi-
caid costs would be incurred that could later be recovered by the state.
The total projected recovery was $3 1,944.
After we identified the individuals who owned real property and calcu-
lated the recovery potential for each, we estimated the potential recov-
ery in each state. We also estimated
the
precision of the recovery
estimates based on a 95-percent confidence level. In addition, we used
stratified sampling procedures (each stratum consisted of the recoveries
from one state) to estimate the recovery potential for the eight states
combined with the precision of that estimate.
Page 51
GAO/EIBD89d6 Medicaid btate Recoveries

Appendix I
Methodology Used to Determine Potential
Recovery for Medicaid Reclpienta Who Own
~~perty
We did not take any steps to factor in inflation or to determine the pre-
sent value of the amount recoverable.
Page 62
GAO/HBD(f9MI
Medicaid E&ate Recoveries

Appendix II
Comments From the Department of Health and
Human Services
DEPARTMENT OF HEALTH & HUMAN SERVICES
@c grsee
Olke 01
Inspector General
Washfnglon. DC 20201
MC.
Lawrence H. Thompson
Assistant Comptroller General
U.S. General Accounting Office
Washington, D.C.
20548
Dear
Mr.
Thompson:
Enclosed are the Department's comments on your draft report,
"Recoveries From Nursing Home Residents'
Estates Could Offset
Program Costs."
The enclosed comments represent the tentative
position of the Department and are subject to reevaluation when
the final version of this report is received.
As you know,
the Office of Inspector
General (OIG)
has conducted
a comprehensive study on States'
estate recovery programs and has
provided this information to all Medicaid State agencies. In
addition,
in response to an OIG report on this same subject
earlier this year,
the Department formed a task force which is
evaluating administrative and regulatory changes to improve
States'
estate recovery programs.
The Department appreciates the opportunity to comment on this
draft report before its publication.
Sincerely yours,
Richard P. Kusserow
Inspector General
Enclosures
Page 53
GAO/HRD-SM Medicaid Estate Ftecoveries

Appendix II
Comments Prom the Department of Health
and Human Servicea
Comments of the Department of Health and Human Services
on the General Accounting Office Draft Report,
"Recoveries from Nursing Home Residents' Estates
Could Offset Program Costs"
Overview
GAO studied the Medicaid nursing home programs in eight States, focusing
particular attention on the estate recovery program operated by Oregon.
GAO sought to discover the potential financial impact of such a program on
Medicaid and whether it provides a mechanism for sharing the costs of
nursing home care in a way that is acceptable to the elderly.
According to GAO, States can recover a substantial portion of Medicaid
nursing home payments through establishment of effective estate recovery
programs.
GAO found that as much as two-thirds of the amount spent for
nursing home care for Medicaid recipients who owned a home in the eight
States studied could be recovered from their estates or the estates of
their spouses.
GAO believes that if implemented carefully, such programs
can achieve savings without treating the elderly, inhumanely. In
addition, advocacy groups for the elderly in Oregon (the State with the
most effective estate recovery program) have not expressed concerns about
the program.
Matters For Consideration
By The Congress
The recently enacted Medicare Catastrophic Coverage Act of 1988 (MCCA)
makes mandatory the transfer of assets provisions of the Tax Equity and
tiscal Responsibility Act of 1982 and extends the transfer period f rom 24
to
30
months. GAO believes the Congress should consider making mandatory
the establishment of programs to recover the cost of Medicaid assistance
provided to nursing home residents of all ages either form their estates
or from the estates of their surviving spouses. The establishment of such
programs would help to ensure that the assets preserved through the new
transfer of assets provisions can be used to defray Medicaid costs.
Department Comment
We would generally agree that estate recovery programs have potential as a
technique for assuring that a Medicaid recipient's assets, including a
home, are used to offset program costs. However, we believe that GAO's
recommendation to Congress needs to be more specific and better justified.
Page 54
GAO/IUD-8966
Medicaid Estate Recoveries

Appendix II
Comments P-rum the Department of Health
and Human Services
Page 2
The recommendation is stated in extremely general terms. It does not take
the next, more difficult step of examining what the basic elements of a
legislative proposal might be.
Two especially difficult issues that such
a viable proposal would have to address and on which the GAO report is
silent are:
--
the appropriate balance between State flexibility and detailed Federal
requirements; and
--
cases involving recoveries from the estates of recipients' spouses.
As to the former issue, by pointing out the shortfall in voluntary State
activity, GAO seems to imply that Federal requirements are necessary. By
contrast, the very general tone of the recarmendation seems to imply that
GAO would leave the States in the lead in designing estate recovery
programs,
an outcome that would not be much different from the situation
today.
As to the latter issue, it is conceivable that there will be instances
where the spouse outlives the Medicaid recipient by many years, moves to a
different house or different State, or remarries. Any of these events can
radically affect the spouse's estate and poses difficult questions about
the desirability and potential for recovering Medicaid costs from the
estates of spouses.
However, we would note that the Department has done a great deal to
encourage States to initiate estate recovery programs. First, it should
be noted that the Health Care Financing Administration (HCFA) has taken a
number of actions including:
-- In May 1988, HCFA published a State Agency Successful Practices Guide
which includes a chapter on estate recoveries. HCFA profiled five
States that have successful programs.
This Guide has been distributed to all single State agency heads,
Medicaid Directors, third party liability (TPL) managers, the National
Conference of State Legislatures,
the National Governors Association, and
all HCFA regional offices, among others.
-- We expect this effort to begin to show results in fiscal year (FY)
1989.
-- HCFA has encouraged estate recoveries and use of the Successful
Practices Guide in several national meetings this year; e.g. State
Medicaid Directors conference and National Conference of State
Legislatures.
-- HCFA included estate recoveries in its TPL marketing to selected
States in FY 1988.
.
Page 66 GAO/HBDs966 Medicaid Estate Recoveries

Appendix II
Commenta From the Llepartment of He&b
and Human Servicee
Page 3
--
We plan to take advantage of every appropriate opportunity to
encourage States not pursuing estate recoveries, or pursuing them
ineffectually, to institute a program and/or take a more aggressive
stance.
Secondly, the Office of Inspector General has conducted a comprehensive
study on States' estate recovery programs and has provided this
information to all Medicaid State agencies. Thirdly, we have developed a
departmental task force which is evaluating administrative and regulatory
changes to improve States estate recovery programs.
However, in promoting this program, we must keep in mind its political
sensitivity,
The GAO's recommendations to mandate this program would
amend national policy on such fundamental issues as the disposal of the
homes of the elderly, the intergenerational transfer of wealth, and the
traditional authority of States to set probate policy. For all of these
reasons, we would encourage a broad public discussion of these underlying
issues.
Finally, we would note that although the basic period of ineligibility
governing transfer of homes of institutionalized individuals specified in
the statute prior to MCCA was 24 months, this period could have been
greater depending upon the net amount of the uncompensated value of the
transferred home and the average amount payable under the State plan for
care in a nursing facility.
Other Matters
Impact of recent legislative chanqes and validity of GAO savings
estimates.
The recent enactment of the MCCA substantially changed Federal rules in
section 1917(c) regarding penalties that States impose on persons who
dispose of assets (including the home) for less that fair market value.
MCCA made no changes to the authority in section 1917(b) regarding
recoveries from the estates of deceased recipients or from the estates of
their spouses.
Consequently, GAO's estimates of potential recoveries may no longer be
valid; they almost certainly overstate the maximum potential for savings
from mandatory estate recovery programs by some amount that should be
determined and included in the report. GAO based its estimates on the
assumption that each State could perform as effectively as the State of
Oregon.
Oregon is a relatively small State with approximately
$76 million in nursing home expenditures in FY 1985. While additional
savings could be expected, we do not believe it is feasible to expect
larger States with large Medicaid expenditures to achieve the same
percentage of savings.
Page 56

Comments From the tkpvbnent of Health
and H- Services
Page 4
Errors in description of legislative history.
The GAO report erroneously traces legislative authority for liens, estate
recoveries, and penalties against uncompensated transfers of assets only
back to the Tax Equity and Fiscal Responsibility Act of 1982 (TEFRA). In
fact, authority for estate recoveries and transfer of assets penalties
pre-dates TEFRA.
-- State authority to recover from the estates of deceased recipients
existed in the original Medicaid statute enacted in 1965
(P.L. 89-97).
All that TEFRA did was move this authority from section
1902(a)(18) to section 1917(b)(l).
This raises the difficult question
which, it seems to us, would be a reasonable issue for the GAO report
to address; i. e.,
few States have taken full advantage of the
authority they have had for over twenty years.
In conclusion, fundamental public policy issues that are embedded in
estate recoveries will continue to arise in the long-term care discussions
being addressed at the departmental and congressional levels. Discussions
will presumably include the interface between traditions of inheritance
and repayment of public assistance,
Federal requirements vs. State
flexibility, and nature and levels of income and resources the individual
may exempt and protect. Therefore, we favor a two-pronged approach.
First, we would encourage
a
broad public discussion in Congress and other
appropriate forums on the complex underlying issues affecting Medicaid
estate recovery programs.
Secondly, we would pursue limited legislative,
regulatory, and program management change to enhance program
effectiveness. HCFA is addressing the program management aspects, and the
departmental study, which the GAO mentions in its report, will address the
legislative and regulatory aspects.
Page 57
GAO/ERD&NM Medicaid Estate Recoveries

Appendix III
Comments From the State of CaWornia
STAR ff CAU~NIA-NEALTH Aw) WWAE ACHIC”
‘.XO”cK ONIWIAN, ODrrna
DEPARTMENT OF HEALTH SERVICES
714/7u P SRE”
C.O. Box 912732
SACMNTO, CA 9*34-7310
(916) 322-5824
November 17, 1983
Mr. Lawrence H. Thompson
Assistant Comptroller General
United States General
Accounting Office
Human Resources Division
Washington, DC 20548
Dear Mr. Thompson:
We have been asked to respond to and thank you for your letter of
October 21,
1988 to Governor Deukmejian regarding the draft
report "Recoveries from Nursing Home Residents' Estates Could
Offset Program CostsB'. This report studied Medicaid nursing home
programs in eight states (including California) and has concluded
that the States can recover a substantial portion of Medicaid
nursing home payments through establishment of effective estate
recovery programs. California prides itself as being a leader
among Medicaid programs in this endeavor and certainly agrees
with this approach. We do not find any discrepancies of data in
the references to California.
California's generalized Estate Recovery Program began in 1981
with a
collection program of $130,128 and has grown in 7 years
to 9 Droiected recovery of ~ZS.OOO.OOQ for 1988-89 fiscal year.
Hopefully, this report will aid us in implementing some new
processes in California.
As acknowledged in the study, our State
is unable to effect recovery in cases where there is a surviving
spouse and/or where the nursing patient received services prior
to age 65 due to current State laws and regulations. We are
currently preparing enabling State legislation
to address these
issues.
We are also hoping to increase recoveries by providing
further training at the county level to clarify the State's
authority to file property liens against long term care
beneficiaries (at any age) that declare no intent of returning
home under current State laws and 42 USC 1396p(a).
Page 58
GAO/w Medicaid Estate Recoveries

Appendix III
Commenta Prom the Stat.42 of CalUornh
Mr.
Lawrence H. Thompson
Page 2
If you need further information regarding this matter, please
feel free to contact, Gerald B. Rohlfes, Chief, Recovery Branch
at (916) 445-0416.
Sincerely,
g;:$d
Medical Care Services
Page 59
GAO/llRDWW
MedIcaid Estate Recovedea

Appendix IV
Comments From the State of Michigan
J*MES J. BLANCHIRO
GOYERNOR
STATE 0~ YICHIQAN
OfFICE oc THE GOVERNOR
LANBINO
January 10, 1989
M r .
Lawrence H. Thompson
Assistant Comptroller General
General Accounting Office
Human Resources Division
Washington, D.C.
29548
Dear Mr.
Thompson:
The proposed report to the Secretary of Health and Human Services
has been reviewed.
Although we do not have specific comments on
the contents of
the report,
potential for Michigan.
the concept certainly may have
During the past 10 to 15 years, Michigan has not had a statutory
base upon which to subrogate against estates of deceased Medicaid
recipients. It is interesting to note how well Oregon has done
by
enacting
legislation specifically
recoveries.
authorizing estate
Also,
with the clarification of federal intent in the Tax Equity
and Fiscal Responsibility Act of 1982 (TEFRA) and the Medicare
Catastrophic Coverage Act of 1988, it would appear that many
states will be addressing the recovery potential.
We,
in Michigan, are of the opinion that there is a potential for
recovery of some $7 to $9 million dollars after a program is
developed and operational.
Based upon the facts and recovery potential, Michigan will be
exploring the possibility of implementing such a program.
.
Page 60
GAO/HRD-9960
Medicaid If&ate Recoveries

Appendix V
Comments From the State of Ohio
Richard F. Cd&e
Governor
Ohio Department of Human Services
30 East Broad Street. Columbus, Ohio 43X6-0423
December 13, 1988
United States
General Accounting Office
Human Resource Divlsion
Attention Laurence H. Thompson
Suitzer Building Roa 1126
330 C Street94
Washington D.C. 20201
Dear Mr. Thompson:
On behalf of the Honorable Richard F. Celesk, Governor of Ohio, I am
responding to your October 21,
1988 letter concerning the Draft Report
*Recoveries Fwn Rursfng Home Residents' Estates Could Offset Program Costs".
Ye substantially agree with the conclusions reached in this report.
We agree
state recovery prograss would fncrrase equity, be cost effective, and would
help wet future financial strains on the govemsent's health cara effort.
We
do, however, have sane reservations on the amounts projected in the cost
benefit analysis. Me also foresee that Ohio nqy
have
more problems
implementing this program than Oregon.
Gill Bagel from the Oregon Department of Human Services' unit in charge of
this program stated that part of the reason the progra is so successful in
Oregon is that the program has been In exfstence, along with the enablfng
legislatfon, for 25 years. This means that advocacy groups in Ohio may have a
different perspective on the program than the advocacy groups in Oregon.
Also, because Oregon has an established progrius and Ohio does not, Ohfo would
face the fnftial cost associated with the development of the program.
Another advantage that Oregon has fs that ft is a state admfnistered program
which allows them to atifnfster the program fra a centralized system.
Thus,
R;{, ara able to send out attorneys from their district offices to fmpose the
This greatly incraases thefr efficfency and provfdes better control of
the irogram. Ohio has a county adnfnistered system uhfch places much of the
atiinistrative burden on the local county offices. This
q
qy also increases
the administrative costs thus reducing the cost benefit ratio.
Page 6 1
GAO- MedkaidE&at.eRecoveries

Commente From the State of Ohio
Lawrence H.
Thompson
Assfstant Comptroller General
Page 2
We do agree that the Health Care Financing Administration (HCFA) of the
Department of Health and Human Servfces (HHS) must take a more active
leadershfp role in assfstfng the states with the development of
such
In addition HCFA should begin developing a legislative proposal
$$'~~id provide a more uniform program without the ambiguous language which
currently exists
as
illustrated In Section 1917(b).
Thank you for the Opportunfty to respond to your report. If you have any
questfon please feel free to contact my office. Please send us the results of
this report along with conments from the other states,
Sincerely
Patricia Barry
Director
PG/dk
cc: Governor Rfchard F. Celeste
Page 62
GAO/HRD439-56 Medicaid Eatate Recoveries

knments From the State of Oregon
December 5, 1958
Lawrence H. Thompson
Assistant Comptroller Ceneral
U.S. General Accounting Office
Human Resources Division
Washington, D.C. 20548
Dear Mr. Thompson:
Thank you for the copy of your report, Recoverie mRursfnq
&RJR Res'dents' ,wI;puld Offset Proaram&. We are
pleased lo learn that Oregon's estates program ranks number one
nationally for Medicaid estate recoveries.
We project that Medicaid estate recoveries in Oregon for the
current bienniumwill total $10,508,000. Our program
aggressively corrects disqualifying transfers of assets, and is
active in the preservation of assets sotheymay be available
for the current cost of care as well as the estate. Our goal
is to increase estate recoveries while protecting the personal
and property rights of the people we serve.
I have attached a colrment from the Estate Administration Unit
staff for your consideration. We are happy to have been able
to provide your office with assistance in preparing the report.
Cregon has frequently been cal?ed upon to assist other states
in implementing Medicaid estate recovery programs. We will
continue to provide assistance to other states and antfcfpate
inquiries to increase following the release of your report. We
look forwardtothe challenge of maintaining our national
leadership in this area.
NG:wrl
Enclosure
Page 63
GAO/HBD%(Mg
Medicaid Jbtate Recoveries

Appendix VII
Comments From the Commonwealth
of Pennsylvania
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF PUBLIC WELFARE
P.O. BOX 2675
HARRISBURG. PENNSYLVANIA 17105-2675
Mr. Lawrence H. lhompson
Assistant Comptroller General
U.S. General Accounting Office
441 G Street,
Northwest
mczin 6064
Washington, D.C.
20548
fg:
Review of Wsdicaid Estate Recovery
programs
(cxo/Rm-88-95)
Dear Mr. Ihanpson:
Since the Departmsnt of Public Welfare (Department) is the Single
State &gency which tiinisters the Medicaid Program in the Cacnnonwealth of
Pennsylvania, Ciovernor Casey has asked the Dspartmsnt to respond to this
report on Medicaid Estate Pecovery Programs.
Secretary White has
asked
that
I respond for the Dspartsmnt.
Ibe Department agrees that there could bs increased
revenues
generated frau operating an estate recovery program: however, current
Pennsylvania state law &ss not allow for recovery of properly received
benefits.
Federal regulations permit recovery
of
correctly paid Medicaid
funds fran the estate
of
an individual who was 65 years of age or older
Aen
he or she received Wedicaid only:
1) after the death of the individual’s surviving spouse, and
2) when the individual
has
no surviviq child who is
under
age 21, or who is blind or disabled.
If the Ccsraonvealth wants to consider recipients’ estates as a
source of recovering Wsdicaid fur&, steps would have to be taken to
introduce legislation which mandates estate recowry.
We do not necessarily agree with scans of the assumptions used to
calculate the probable dollar value of an estate recovery progrmn in
Pennsylvania. Ihe report data concluded that
a.5
percent of the recipient
sm@e relevant to Pennsylvania owned real property that could bs used to
help defray the cost of their Medicaid care. They also concluded that the
progran would have yielded $8.5 million in gross recovery if such a program
had bsen in place affecting the Wsdicaid nursing hams caseload during 1985.
Your extrapolations did not totally exclude married nursirq home recipients
from the dollar projections,
but
rather assumed that one-half the market
Page 64
GAO/ERD&Mf
Medicaid Estate Recoveries

NW* WJ
C4~mmentaFromthecommOnweal~
of Pennaylv~
-2-
value would subsequently bs available from the estate of the spouse living
outside the nursing bane.
We
suspect that
this assunption is nut practical
in Pennsylvania, and must conclude that the probable dollars recovered uxld
be less than the $8.5 million.
Although we do not agree witi all the information contained in
your report, we believe that establishirq an estate recovery program in the
Canaonwealth of Pennsylvania could be a viable option which will bs given
further consideration by the Department.
-Xs do not believe that Medicaid
should be forced tc carry the burden of providing nursing bane care while
enlarging the estates of sane recipients.
Thank you for giving us the opportunity to respond to this replrt.
Sincerely,
cc: Governor Robert P. Casey
.
Page 66

Appendix VIII
Comments From the State of Washington
BOOTH GARDNER
ClOVERNOR
STATE OF WASHINGTON
wFlcE OF M GOVERWOR
OLYMPIA
WKU-2413
November 10. 1988
United States General Accounting Office
Mr. Lawrence Thompson. Assistant Comptroller General
Human Resources Division
Washington. D.C. 20548
RE: Medicaid Estate Recovery Program
Dear Mr. Thompson:
We have reviewed the proposed report to the Secretary of Health and Human
Services on the recent review of Medicaid estate recovery programs.
The slate of Washington, Department of Social and Health Services (DSHSl.
began an Estate Recovery Program with the enactment of legislation in 198’7.
The scope of the program selected by DSHS was limited lo the filing of
property liens or creditor claims after the death of medical assistance
recipients who were older than 65 years of age.
Recovery was further lia-
ited in the enacting legislation to estates valued below $50,000, unless
there were no close surviving relatives.
An amendment to reduce the
$50,000 exemption to $35,000 is being proposed for the 1989 legislative
session.
It is too soon to assess the overall effectiveness of the DSHS Estate
Recovery Program. To dale, recoveries are less than originally projected:
however. many of the properties involved have not yet been probated or
sold. We are confident this will develop into a cost effective program.
Thank you for the opportunity to review and comment on the proposed report.
Sincerely,
BOOTH GARDNER
Governor
Page 06
GAO/HRM9-56 Medicaid Estate Recoveries

Appendix IX
Comments From the State of Wisconsin
State of Wisconsin \
DEPARTMENT OF HEALTH AND SOCIAL SERVICES
1 West Wilson Street, Madtson, Wisconsm 53702
Twnmy G. rhompum
Cover”“‘
November 25, 1988
Lawrence H. Thompson
Assistant Comptroller General
United States General Accounting Office
Human Resources Division
WASHINGTON, D.C. 20548
Dear Mr. Thompson:
Thank you for the opportunity to review and comment on the GAO draft
report concerning Medicaid Estate Recovery Programs.
The statistical
projections contained therein correspond well with the data originally
provided by Wisconsin during the research phase of this project.
Since
providing the GAO with those data, Wisconsin has done considerable research in
the area of estate recovery. Due to its outstanding recovery rate, as well as
the
apparent efficiency with which its program is administered, Oregon’s
estate recovery program has been studied in detail, as have programs currently
operating in several other states. As a result of this study, statutory
language has been proposed which would permft Wisconsin to recover Medicaid
expenditures from an estate when there is no surviving spouse, minors, or
disabled children. Recovery of such monies would be allowed when a home was
exempted from consideration as an asset during the eligibility determination
process because the institutionalized individual expected to return home.
Additionally, recovery would not take place until the home was sold in
settlement of the estate.
It is my belief that an estate recovery program, operated with
flexibility and a high degree of sensitivity to the needs of the elderly and
their families, can accomplish recovery goals without intimidation and
confusion.
Should you be interested in the details of Wisconsin’s proposed
estate recovery program, please feel free to contact me.
Again, thank you for
sharing this report with us.
Sincerelv.
Secretary -
Page 67
GAO/ERD&fUM
Medicaid E&ate Recoveries

Appendix X
Major Contributors to This Report
Human Resources
Division, Washington,
(202) 275-6195
James R. Linz, Assistant Director
D.C.
Seattle Regional Office
Randall Williamson, Assignment Manager
Susan L. Pazina, Evaluator-in-Charge
Magdalene T. Siew, Evaluator
Janet E. Frisch, Evaluator
Suzanne T. Jackson, Evaluator
Debra Jean Evick, Evaluator
(101109)
Page 68
