
HHS Action Plan to Reduce
Racial and Ethnic
Health Disparities:
Implementation
Progress Report
2011-2014
November 2015
About This Report
This document is an implementation progress report of the U.S. Department of Health and Human
Services (HHS) Action Plan to Reduce Racial and Ethnic Health Disparities (HHS Disparities Action
Plan). The HHS Disparities Action Plan represents an ongoing commitment by HHS to coordinate
efforts and assess the nation’s progress toward addressing racial and ethnic disparities in health and
health care. This report outlines the HHS Disparities Action Plan’s goals and strategies, describes a
sample of the specific actions being taken across HHS agencies to reduce these disparities, and
highlights major accomplishments to date.
Suggested citation: U.S. Dept. of Health and Human Services, Office of the Secretary, Office of the
Assistant Secretary for Planning and Evaluation and Office of Minority Health. HHS Action Plan to
Reduce Racial and Ethnic Health Disparities Implementation Progress Report. Washington, DC:
Office of the Assistant Secretary for Planning and Evaluation, 2015.
ii

Contents
HHS Action Plan to Reduce Racial and Ethnic Health Disparities: Implementation
Progress Report — Executive Summary ......................................................................................... 1
HHS Action Plan to Reduce Racial and Ethnic Health Disparities: Implementation
Progress Report—Full Report ......................................................................................................... 6
Background ................................................................................................................................. 6
Addressing the Major Dimensions of Racial and Ethnic Health Disparities .............................. 6
HHS Action Plan to Reduce Racial and Ethnic Health Disparities ............................................ 8
Goal I: Transform Health Care ............................................................................................................. 11
Goal II: Strengthen the Nation’s Health and Human Services Infrastructure and
Workforce ...................................................................................................................................... 15
Goal III: Advance the Health, Safety, and Well-Being of the American People ................................. 19
Goal IV: Advance Scientific Knowledge and Innovation .................................................................... 23
Goal V: Increase Efficiency, Transparency, and Accountability of HHS Programs ............................ 25
Conclusion ............................................................................................................................................ 27
References ............................................................................................................................................. 28
Appendix A: Glossary of Acronyms................................................................................................... A.1
Appendix B: Overview of HHS Action Plan to Reduce Racial and Ethnic Health
Disparities .................................................................................................................................... B.1
iii
HHS Action Plan to Reduce Racial and
Ethnic Health Disparities: Implementation
Progress Report — Executive Summary
Introduction
The U.S. Department of Health and Human Services Action Plan to Reduce Racial and Ethnic
Health Disparities (HHS Disparities Action Plan) is the most comprehensive federal commitment
to date for reducing, and eventually eliminating disparities in health and health care. Through the
HHS Disparities Action Plan, the Department of Health and Human Services (HHS) provides a
coordinated framework for departmental agencies and offices to streamline and institutionalize
programmatic and policy efforts, as well as promote integrated approaches and evidence-based
programs, so that all Americans have the chance to live the healthiest lives possible. This report
provides an overview of the four Secretarial priorities and five goals that make up this strategic
plan. The report also describes some of the major actions and activities that agencies have
undertaken to implement the HHS Disparities Action Plan since its original publication in April
2011. The implementation progress report is not meant to be an exhaustive list of all of the current
research, policies, and programs the Department is supporting to improve minority health, but
rather provide several illustrative examples of important work in this area.
Secretarial Priorities
The overarching Secretarial priorities represent the cross-cutting issues that the HHS Disparities
Action Plan addresses to ensure the coordination of HHS programmatic and policy efforts to
effectively advance health equity. Presented below are the four priorities and examples of
corresponding activities.
1. Assess and heighten the impact of all HHS policies, programs, processes, and resource
decisions to reduce health disparities. This priority supports monitoring HHS agencies’ stra-
tegic plans, programs, and regulations to ensure that the HHS Disparities Action Plan goals,
strategies, and actions are included to the fullest extent possible in the agencies’ work.
• In FY 2013, the Substance Abuse and Mental Health Services Administration (SAMHSA)
incorporated health disparity impact statements into all new Requests for Applications for
grant programs. These statements helped grantees build their capacity to collect and use data
to develop strategies addressing differential access, utilization, and outcomes of behavioral
health interventions among diverse populations.
1

2.
Increase the availability, quality, and use of data to improve the health of minority populations.
High-quality data is fundamental to HHS’s ability to understand the causes of health disparities,
design effective responses, and evaluate progress in reducing disparities.
• As called for by Section 4302 of the Affordable Care Act, HHS adopted new standards for the
collection of data by race, ethnicity, primary language, sex, and disability status within major
self-reported population health surveys. The new standards provide additional granularity for
the Asian race category and Hispanic ethnicity, and distinguish Native Hawaiian from Pacific
Islander race categories. The specificity provided by the new standards will allow for
improved demographic data collections and tracking of health differences among these
populations, as well as an increased ability to target interventions appropriately.
3. Measure and provide incentives for better health care quality for minority populations. As
racial and ethnic minorities often receive a poorer quality of care and face more barriers to
seeking care than Whites, providing incentives for quality care in these populations is critical
for improvement in patient outcomes.
• From 2011-2014, the Centers for Medicare & Medicaid Services (CMS) Disparities National
Coordinating Council (DNCC) offered technical assistance to Quality Improvement
Organizations (QIOs) to improve care provided to Medicare beneficiaries within underserved
populations. For example, QIOs in Arkansas, California, and Michigan engaged in the
Cardiac Health Disparities Project, which focused on prevention of cardiovascular disease
among racial and ethnic minorities. QIOs in West Virginia, New York, and Texas engaged
in the Everyone with Diabetes Counts (EDC) special innovation project. During this project,
Medicare and Dually Eligible beneficiaries from rural and minority underserved populations
were enrolled in diabetes self-management education (DSME) classes to maximize patient
engagement and improve health literacy, with the goal of decreasing the disparity in diabetes
care provided to these populations.
4. Monitor and evaluate the Department’s success in implementing the HHS Disparities Action
Plan. The HHS Health Disparities Council, co-chaired by the Assistant Secretary for Health
and the Assistant Secretary for Planning and Evaluation (ASPE), is composed of senior-level
HHS agency representatives and serves as the venue to share information, coordinate activities,
oversee implementation, and track progress of the strategies and actions of the HHS Disparities
Action Plan.
Goal I: Transform Health Care
Creating an equitable health system requires efforts to (1) expand opportunities for racial and
ethnic minorities to obtain and understand how to use insurance coverage; (2) expand access to
health care services; and (3) improve the quality of care provided to racial and ethnic minority
populations. To achieve these aims, Goal I of the HHS Disparities Action Plan includes the
specific actions below, among others:
Expansion of Medicaid and Introduction of the Health Insurance Marketplace. The Affordable
Care Act offers an opportunity for millions of racial and ethnic minorities to gain affordable and
quality health insurance coverage. At the time of this report, 29 states, including the District of
Columbia, have expanded Medicaid eligibility so that all individuals up to 133 percent of the
federal poverty level (FPL) qualify for coverage. The new Health Insurance Marketplace is
2

making coverage available to others who do not qualify for Medicaid, with tax credits available
to help defray the premium cost for those that qualify.
From Coverage to Care (C2C) Initiative. The CMS Office of Minority Health (OMH) launched
the From Coverage to Care (C2C) Initiative in June 2014. The C2C Initiative is designed to
answer consumer questions about new health coverage opportunities, provide information
about new benefits, including primary care and preventive services, and provide resources for
health care providers to promote patient engagement in care. The C2C launch marked the
release of the new Roadmap to Better Care and a Healthier You, which includes eight steps to
help consumers and health care providers be informed about the diverse benefits available
through their coverage and how to use it appropriately to access primary care and preventive
services. The Roadmap is available in English, as well as seven secondary languages. The
CMS OMH also developed an Enrollment Toolkit: Helping Consumers Choose the Health Plan
That’s Right for Them, to support the C2C Initiative.
The Health Resources and Services Administration’s (HRSA) National Health Service Corps
(NHSC). The NHSC offers loan repayment and scholarships to primary care providers and
students for serving at NHSC sites in communities with shortages of health professionals. In FY
2013, 8,899 NHSC clinicians provided care to more than 9.3 million Americans with otherwise
limited access to health services.
Goal II: Strengthen the Nation’s Health and Human
Services Infrastructure and Workforce
Strengthening the nation’s health and human services infrastructure and workforce involves
increasing the number and diversity of health care professionals, and incorporating cultural and
linguistic knowledge among the health care workforce. Goal II of the HHS Disparities Action Plan
supports the following actions, among others:
National Standards for Culturally and Linguistically Appropriate Services in Health and Health
Care (National CLAS Standards). The Office of Minority Health (OMH) released the enhanced
National CLAS Standards in April 2013, marking the first update since the original standards
were published in 2000. The enhanced National CLAS Standards are intended to advance health
equity, improve quality, and help eliminate health disparities by providing a blueprint for
individuals and health and health care organizations to implement culturally and linguistically
appropriate services.
Health Profession Opportunity Grants (HPOG). Authorized by the Affordable Care Act and
administered by the Administration for Children and Families (ACF), HPOG provides edu-
cation and training to Temporary Assistance to Needy Families (TANF) recipients and other
low-income individuals to help them pursue jobs in health care. As of December 2013, there
were 20,382 enrolled individuals in HPOG health care and occupation training programs, and
12,384 individuals had completed such programs.
3

Goal III: Advance the Health, Safety, and Well-Being
of the American People
Health disparities are also driven by community and environmental factors beyond those
embedded in the health care system. Strategies that create healthy and safe environments promote
healthy behaviors to improve the well-being of the American people. The following actions
support Goal III:
Public-Private Partnerships to Improve Vaccination Rates. For the 2010–2011 influenza
season, OMH established the Walgreens-HHS Co-Sponsorship Agreement, which provides
uninsured individuals with free seasonal influenza vaccination. Walgreens has committed over
$10 million annually to support this effort, and the partnership has successfully vaccinated more
than half a million individuals who otherwise would not receive the influenza vaccination due to
cost. Between April 2012 and September 2013, the National Vaccine Program Office (NVPO)
offered grants to support community-level efforts to deliver culturally appropriate immunization
interventions and developed a web tool to map flu vaccine disparities.
Community Transformation Grants (CTG) Program. The CTG Program, which had been
supported by the Prevention and Public Health Fund created by the Affordable Care Act,
enabled awardees to design and implement community-level prevention programs that placed
special emphasis on reaching people who experience the greatest burden of death, disability,
and suffering from chronic conditions. The CDC Community Transformation Grants Program
implemented, evaluated, and disseminated evidence-based community preventive health
activities. Funded communities worked across multiple sectors to reduce heart attacks, cancer,
and strokes by addressing a broad range of risk factors and conditions including poor nutrition
and physical inactivity, tobacco use, and others. By promoting healthy lifestyles, especially
among population groups experiencing the greatest burden of chronic disease, these grants
improved health, reduced health disparities, and controlled health care spending.
Goal IV: Advance Scientific Knowledge and
Innovation
To inform initiatives for increasing health equity, Goal IV promotes the collection of race and
ethnicity data and strengthening of information systems to improve the quality of health care and
biomedical research through the following actions, among others:
Native Hawaiian/Pacific Islander National Health Interview Survey. This landmark project,
launched by the CDC’s National Center for Health Statistics (NCHS) and OMH, aims to
enhance the availability and quality of data on health outcomes and health care utilization of
Native Hawaiian and Pacific Islanders (NHPIs). To support participation in the survey and
increase response rates, NCHS, OMH, and the Census Bureau collaborated to provide outreach
and education on the project to NHPI stakeholders. Policymakers, community leaders, and
others will use these findings for designing policies and programs to improve NHPI health and
well-being.
Community Networks Program Centers (CNPCs). To address cancer and other related
4

co-morbidities with documented health disparities, the National Institutes of Health/National
Cancer Institute (NIH/NCI) funded 23 Community Networks Program National and Regional
Centers for Reducing Cancer Health Disparities (CNPCs). CNPCs use community-based par-
ticipatory research (CBPR) methods to increase knowledge of, access to, and use of preventive
screening, diagnosis, and treatment in communities, and thus reduce cancer disparities among
racial and ethnic minority populations.
Goal V: Increase Efficiency, Transparency, and
Accountability of HHS Programs
To ensure that programs and policies are efficient, transparent, and accountable, HHS supports
information sharing across agencies to minimize duplication of efforts. These processes include
tracking existing performance measures and other government data on health system indicators
and making them available to the public.
Health System Measurement Project. The ASPE Health System Measurement Project provides
public access to data that track trends in racial and ethnic health and health care disparities. Data
can be accessed and used by individuals and organizations inside and outside of government to
track changes in these health system characteristics over time and identify areas that require
improvement.
Conclusion
Agencies contributing to the HHS Disparities Action Plan have developed an extensive, mul-
tifaceted set of activities that span a wide range of populations, address a multitude of individual
and system-level barriers to health and quality health care, and support the growth of a more
diverse health care workforce. Guided by the HHS Secretary’s priority to eliminate health
disparities and the HHS Disparities Action Plan, HHS agencies have demonstrated their com-
mitment to reducing racial and ethnic health disparities, and built their capacity to address these
disparities. HHS efforts related to implementation of the HHS Disparities Action Plan have
generated ideas, materials, and data that will help the Department advance toward its vision of a
nation free from disparities in health and health care.
5

HHS Action Plan to Reduce Racial and Ethnic
Health Disparities: Implementation Progress
Report 2011-2014—Full Report
Background
The United States (U.S.) continues to face significant and persistent racial and ethnic health disparities,
with racial and ethnic minority populations
1
bearing a disproportionate burden of illness, disability, and
premature death.
2, 3, 4
Healthy People 2020, which identifies and monitors 10-year national objectives for
improving the health of all Americans, defines a health disparity as “a particular type of health difference
that is closely linked with social, economic, and/or environmental disadvantage”.
5
Extensive research
shows that populations that have systematically experienced this kind of disadvantage, such as racial and
ethnic minorities, face greater obstacles to optimal health.
6
These obstacles include difficulty in accessing
health insurance and quality health care, as well as differential access to high-quality education,
employment, housing, and income—factors known as the social determinants of health.
7
These social
determinants of health are often the underlying causes of health disparities.
Many leading health indicators, such as those from the Healthy People 2010 Final Review and the Agency
for Healthcare Research and Quality (AHRQ) National Healthcare Disparities Report, have shown little
reduction in racial and ethnic health disparities over the past decade.
8
As such, a significant and
well-coordinated effort to reduce and eventually eliminate health disparities is necessary to ensure that all
Americans have the chance to live the healthiest lives possible. The U.S. Department of Health and
Human Services (HHS) Action Plan to Reduce Racial and Health Disparities (HHS Disparities Action
Plan) is an integral part of this effort. Through the HHS Disparities Action Plan, HHS promotes integrated
approaches, evidence-based programs, and promising practices to reduce racial and ethnic health
disparities.
Addressing the Major Dimensions of Racial and Ethnic
Health Disparities
Addressing disparities in health and health care requires a multifaceted approach, including the following:
Expanding access to quality health care. The Institute of Medicine’s 2002 report Unequal Treatment:
Confronting Racial and Ethnic Disparities in Health Care and AHRQ’s annual National Healthcare
Disparities Report have identified the lack of health insurance as a significant driver of health care
disparities. These reports have consistently documented the lower rates of health insurance and receipt
of recommended care among racial and ethnic minorities as compared to non-Hispanic Whites.
9, 10, 11, 12
Furthermore, these reports demonstrate disparities in the quality of care provided to different
populations, even when access to care is ensured through adequate health insurance coverage. The
Institute of Medicine has noted that even when racial and ethnic minority patients have the same types
of health insurance as White patients, they tend to receive a lower quality of care.
13
6

Addressing diversity and cultural competence in the health care workforce. Racial and ethnic diversity
in the health care workforce is associated with improved access to care. Providers who are culturally
competent provide care directly related to greater consumer satisfaction among racial and ethnic
minorities.
14
The diversity of the public health and health care workforces, however, continues to lag
behind the growing racial and ethnic diversity of the U.S. population.
15, 16
For example, Latinos and
African-Americans comprise nearly one-third of the nation’s population, but they account for only
slightly more than one-tenth of U.S. physicians.
17
Further, physician shortages in underserved areas
often inhabited by racial and ethnic minority populations can also contribute to inequities in health care.
Supporting population health. Many racial and ethnic minority populations experience higher rates of
disease and premature death than Whites. For example:
– Non-Hispanic African-American adults are at least 50 percent more likely than non-Hispanic
Whites to die prematurely from heart disease or stroke.
18
– Asian/Pacific Islander adults are 60 percent more likely to have acute Hepatitis B, a major cause of
liver disease, than non-Hispanic Whites.
19
– African-American, Native Hawaiian/Other Pacific Islander (NHPI), and Hispanic adults all have
rates of HIV infection diagnosis that range from three to nine times the rate of non-Hispanic
Whites.
20
– Hispanics, non-Hispanic Blacks, and those of mixed race all have higher rates of diabetes than
non-Hispanic Whites.
21
– The mortality rates for non-Hispanic Black infants and American Indian/Alaska Native infants are
far higher than those of non-Hispanic White infants.
22
Enhancing data collection and research. Incomplete and poor quality data on race, ethnicity, and
language prevent a comprehensive and accurate characterization of health disparities, factors
contributing to these disparities, and results from actions taken to address them.
23
Establishing and
implementing standards for data collection, reporting, and tracking can generate knowledge that can be
used to inform policy and programmatic decision making.
HHS Infrastructure to Address Racial and Ethnic Health Disparities
The HHS Office of Minority Health (OMH) was established in 1986, one year after the Report of the
Secretary’s Task Force on Black and Minority Health (the Heckler Report) outlined the tremendous
racial and ethnic minority health inequities in the United States. OMH is dedicated to improving the
health of racial and ethnic minority populations through the development of health policies and
programs that will help eliminate health disparities. OMH was reauthorized under the Patient
Protection and Affordable Care Act of 2010. OMH is led by the Deputy Assistant Secretary for
Minority Health who reports directly to the Secretary of HHS.
The Affordable Care Act established Offices of Minority Health within six agencies, including the
Agency for Healthcare Research and Quality (AHRQ), the Centers for Disease Control and Prevention
(CDC), the Food and Drug Administration (FDA), the Health Resources and Services Administration
(HRSA), the Centers for Medicare & Medicaid Services (CMS), and the Substance Abuse and Mental
Health Services Administration (SAMHSA).
The Affordable Care Act elevated the National Center on Minority Health and Health Disparities to an
7

institute level at the National Institutes of Health (NIH).
The HHS Health Disparities Council is composed of the Deputy Assistant Secretary for Minority
Health, the directors of the agency OMHs, the director of the National Institute on Minority Health and
Health Disparities, and senior staff in other agencies. The HHS Health Disparities Council coordinates
the efforts of HHS operating and staff divisions on a cohesive set of strategies to reduce health
disparities and advance health equity.
HHS Action Plan to Reduce Racial and Ethnic Health
Disparities
Recognizing the complex and multiple approaches necessary to address health disparities, in April 2011
HHS released the first strategic plan to eliminate health disparities—the HHS Action Plan to Reduce
Racial and Ethnic Health Disparities (HHS Disparities Action Plan). This plan complements the 2011
National Stakeholder Strategy for Achieving Health Equity; a product of the National Partnership for
Action to End Health Disparities.
24
The National Stakeholder Strategy, was developed from the input of
thousands of individuals and organizations across the country in an effort to mobilize a nationwide,
community-driven approach to combating health disparities and achieving health equity.
The HHS Disparities Action Plan is the most comprehensive federal commitment to addressing health
disparities to date. Its vision is to help create “a nation free of disparities in health and health care.” This
unprecedented strategic plan provides a coordinated framework and guide for all HHS agencies. The HHS
Disparities Action Plan is designed to streamline and unify programmatic and policy efforts to reduce
racial and ethnic minorities health and social disparities.
25
The HHS Disparities Action Plan builds upon
the foundation of the Affordable Care Act, which includes a number of provisions that strive to improve
the health of racial and ethnic minorities and other underserved or vulnerable populations by addressing
many of the factors long associated with health disparities. For example, the Affordable Care Act includes
permanent reauthorization of the Indian Health Care Improvement Act, which extends current law and
authorizes new programs and services within the Indian Health Service. For American Indians and Alaska
Natives, the Affordable Care Act helps to address health disparities by investing in prevention and
wellness and increasing access to health coverage.
The HHS Disparities Action Plan contains four overarching Secretarial priorities and five specific goals.
As shown in figure 1, Goals I−IV include one or more related strategies subdivided into actions. Actions
are composed of activities undertaken by federal agencies to address racial and ethnic minority health
disparities. Subsequent sections of this report describe progress toward the Secretarial priorities and five
goals of the HHS Disparities Action Plan by highlighting some of the major actions and activities
undertaken since April 2011.
8
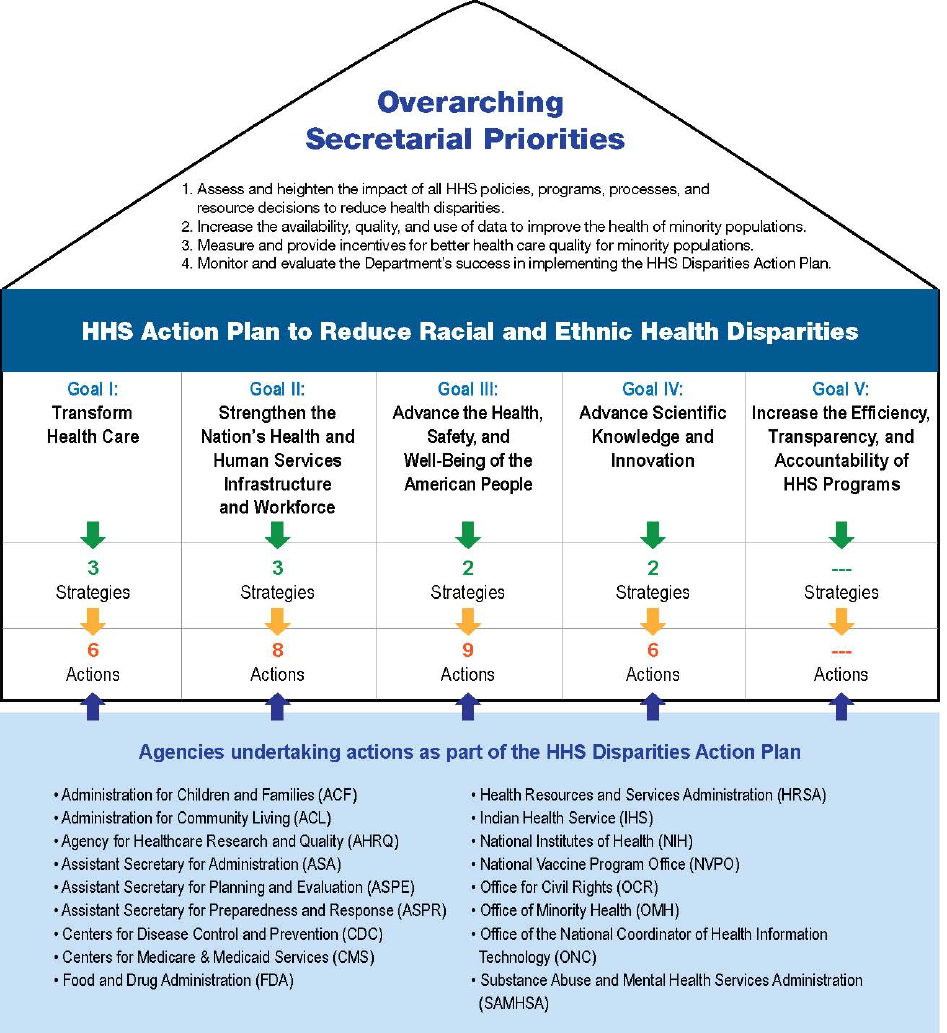
Figure 1.
Progress on the Overarching Secretarial Priorities
The overarching Secretarial priorities to reduce racial and ethnic minorities’ health disparities represent
the cross-cutting issues that the HHS Disparities Action Plan addresses. They are intended to ensure the
coordination of existing and new HHS programmatic and policy efforts so they will be used effectively to
advance health equity. Ultimately, the combination of goals, strategies, and actions that are implemented
should result in meeting these priorities. Below are the four priorities and examples of activities
corresponding to them.
9
1. Assess and heighten the impact of all HHS policies, programs, processes, and resource decisions
to reduce health disparities. This priority supports ongoing monitoring and assessment of HHS
agencies’ strategic plans, programs, and regulations to ensure that the goals, strategies, and actions in
the HHS Disparities Action Plan are included to the fullest extent possible. This priority also requires
program grantees, as applicable, to submit health disparity impact statements and supports the use of
this information to score grant applications and inform HHS programmatic and policy efforts. It also
supports ongoing assessment of the effects of proposed programs and policies on health disparities,
such that these disparities are monitored and addressed.
• The Substance Abuse and Mental Health Services Administration (SAMHSA) incorporated
health disparity impact statements into its Requests for Applications for four grant programs in
fiscal year 2012. These statements helped grantees build their capacity to collect and use data
to develop strategies addressing differential access, utilization, and outcomes of behavioral
health interventions among diverse populations. Because of the success of this pilot, in fiscal
year 2013, SAMHSA expanded the health disparity impact statement pilot to all new Requests
for Applications.
2. Increase the availability, quality, and use of data to improve the health of minority populations.
Collecting and analyzing high-quality data is fundamental to HHS’s ability to understand the causes of
health disparities, design effective responses, and evaluate progress in reducing disparities. Strong
surveillance systems must monitor trends in health and quality of care measures, as well as
patient-centered research activities.
• As called for by Section 4302 of the Affordable Care Act, in October 2011, HHS developed and
adopted new standards for the collection of data by race, ethnicity, sex, primary language, and
disability status within major self-reported population health surveys.
26, 27
The new standards
provide additional granularity for the Asian race category and Hispanic ethnicity, and also
distinguish Native Hawaiian from Pacific Islander race categories. In addition, for the first time,
HHS surveys will provide uniform self-reported data on primary language and disability status. The
specificity provided by the new standards will allow for improved demographic data collections and
tracking of health differences among these populations, as well as an increased ability to target
interventions appropriately.
3. Measure and provide incentives for better health care quality for minority populations. Racial
and ethnic minorities often receive a poorer quality of care and face more barriers to seeking care than
non-Hispanic Whites. Providing incentives for quality care for these populations is critical for
improving patient outcomes and creating a high-value health care system that promotes equity.
• Toward this end, the Centers for Medicare & Medicaid Services (CMS) Disparities National
Coordinating Council (DNCC) supported efforts by Quality Improvement Organizations (QIOs)
between 2011 and 2014 to improve the quality of care provided to Medicare beneficiaries within
underserved populations. The DNCC offered technical assistance and consultation to QIOs,
analyzed data related to special innovative disparities projects, and worked with QIOs to ensure
that Medicare providers and practitioners were supported and incentivized to provide high-quality
health services for all beneficiaries, regardless of race, ethnicity, or gender. For example, QIOs in
Arkansas, California, and Michigan engaged in the Cardiac Health Disparities Project, which
focused on prevention of cardiovascular disease among racial and ethnic minorities.
• QIOs in West Virginia, New York, and Texas engaged in the Everyone with Diabetes Counts
(EDC) special innovation project. During this project, Medicare and Dually Eligible
10

beneficiaries from rural and minority underserved populations were enrolled in diabetes
self-management education (DSME) classes to maximize patient engagement and improve health
literacy, with the goal of decreasing the disparity in diabetes care provided to these populations.
4. Monitor and evaluate the Department’s success in implementing the HHS Disparities Action
Plan. HHS is committed to ensuring program integrity, effective program performance, and
responsible stewardship of federal funds. Monitoring implementation and assessing progress are
important steps in ensuring that HHS is moving toward achieving the vision and goals of the HHS
Disparities Action Plan. Assessing progress on action steps in the HHS Disparities Action Plan allows
the Department to track implementation and observed outcomes, identify achievements and challenges
across agencies, and make midcourse corrections to improve agencies’ effectiveness in the long term.
Furthermore, the HHS Health Disparities Council serves as the venue to share information, coordinate
activities, and oversee implementation of the strategies and actions. The Council is co-chaired by the
Assistant Secretary for Health and the Assistant Secretary for Planning and Evaluation (ASPE), and
comprises senior-level HHS agency representatives, including the Deputy Assistant Secretary for
Minority Health, the directors of the individual OMHs, and the director of the National Institute on
Minority Health and Health Disparities.
Goal I: Transform Health Care
Creating an equitable health system requires efforts to ensure that all Americans have access to
high-quality health care services. This involves transformative strategies that will (1) expand
opportunities for members of racial and ethnic minority populations to obtain and understand how to use
preventative services provided by high-quality, affordable insurance coverage; (2) expand access to
needed health care services; and (3) improve the quality of care provided to racial and ethnic minority
populations. To achieve these aims, Goal I of the HHS Disparities Action Plan includes the strategies and
specific agency actions listed below.
Reduce disparities in health insurance coverage and access to care
Health insurance coverage is a critical part of any effort to remove financial barriers to care.
28, 29
Research
shows that uninsured individuals are less likely to receive needed health care services.
30, 31
The expansion
of health insurance availability and affordability made possible because of the Affordable Care Act, offers
an opportunity to address disparities in insurance coverage, which in turn can be used to promote
enrollment, access, and utilization of care.
32
Expansion of Medicaid and Introduction of the Health Insurance Marketplace. The Affordable Care
Act offers an opportunity for millions of racial and ethnic minorities to gain affordable and quality
health insurance coverage. As part of this work, the Centers for Medicare & Medicaid Services (CMS)
is overseeing the implementation of the Health Insurance Marketplace (Marketplace). At the time of
this report, 29 states, including the District of Columbia, have expanded Medicaid eligibility so that all
individuals up to 133 percent of the federal poverty level (FPL) qualify for coverage.
33
For states that
chose to expand Medicaid, this newly covered group includes childless adults who were previously
ineligible for Medicaid in most states prior to the Affordable Care Act. For those not eligible for
Medicaid, the new Marketplace is making coverage available to those who previously could not access
private insurance, with tax credits to help defray the cost for qualified individuals with incomes
11
between 100 and 400 percent of FPL.
From Coverage to Care (C2C) Initiative. The CMS Office of Minority Health (OMH) launched the
From Coverage to Care (C2C) Initiative in June 2014. The C2C Initiative is designed to answer
consumer questions about new health coverage opportunities, provide information about new benefits,
including primary care and preventive services, and provide resources for health care providers to
promote patient engagement in care. The C2C launch marked the release of the new Roadmap to Better
Care and a Healthier You, which includes eight steps to help consumers and health care providers be
informed about the diverse benefits available through their coverage and how to use it appropriately to
access to primary care and preventive services. The Roadmap is available in English, as well as seven
secondary languages. The CMS OMH also developed an Enrollment Toolkit: Helping Consumers
Choose the Health Plan That’s Right for Them, to support the C2C Initiative.
Figure 2.
Estimated number of Americans who have preventive services coverage with zero cost sharing
1
White Latino Black Asian American and Pacific Islanders American Indian/Alaska Native
111 million 17 million 15 million 8 million 1 million
Note: The numbers presented in Figure 2 sum to more than the total number of Americans with preventative services with no cost sharing because
individuals reporting Latino ethnicity also reported a race category.
Source: ASPE Data Point. The Affordable Care Act is Improving Access to Preventive Services for Millions of Americans. May 2015.
http://aspe.hhs.gov/health/reports/2012/ACA-Research/index.cfm
Figure 3.
Estimated number of uninsured racial and ethnic minorities eligible for Medicaid, Children’s Health
Insurance Program (CHIP), or Marketplace premium tax credits, beginning January 1, 2014
African Americans American Indian/Alaska Natives Asian Americans and
Pacific Islanders
Latinos
6,800,000 579,000 2,000,000 10,200,000
Sources: ASPE Issue Brief. Eligible uninsured African Americans: 6 in 10 could receive health insurance Marketplace tax credits, Medicaid, or CHIP.
http://aspe.hhs.gov/health/reports/2013/UninsuredAfricanAmericans/ib_UninsuredAfricanAmericans.cfm
. Published December 2013.
HHS.gov/HealthCare Fact Sheet. The Affordable Care Act and American Indian and Alaska Native People.
http://www.hhs.gov/healthcare/facts/factsheets/2011/03/americanindianhealth03212011a.html
. Published 2013.
HHS.gov/HealthCare Fact Sheet. The Affordable Care Act and Asian Americans and Pacific Islanders.
http://www.hhs.gov/healthcare/facts/factsheets/2012/05/asian-americans05012012a.html. Published 2013.
ASPE Issue Brief. Eligible uninsured Latinos: 8 in 10 could receive health insurance Marketplace tax credits, Medicaid, or CHIP.
http://aspe.hhs.gov/health/reports/2013/UninsuredLatinos/rb_uninsuredLatinos.pdf. Published February 11, 2014.
1
ASPE Data Point. The Affordable Care Act is Improving Access to Preventive Services for Millions of Americans. May 2015.
http://aspe.hhs.gov/health/reports/2012/ACA-Research/index.cfm
12

Reduce disparities in access to primary health care service
Racial and ethnic minority populations continue to face major barriers in accessing health care.
34
Although having a medical home increases the chance that people receive the preventive and other
services they need to stay healthy, approximately 23 percent of Hispanic or Latino adults do not have a
usual source of medical care, as compared to less than 12 percent of non-Hispanic or Latino adults.
35
Moreover, even as access to insurance increases, many parts of the country still lack the provider capacity
to offer needed primary health care services. The Health Resources and Services Administration (HRSA)
is addressing this issue by increasing the number of providers offering care in health professional shortage
areas, as well as expanding the ability of health centers to care for more patients. Of the 21.7 million
patients served by community health centers in 2013, nearly two out of three patients were members of
racial and ethnic minority populations.
36
HRSA’s National Health Service Corps (NHSC). For 40 years, the NHSC has supported primary health
care providers dedicated to serving areas with limited access to health care. Recognizing the need to
further expand access to primary care, the Affordable Care Act is investing $1.5 billion to support the
NHSC. In fiscal year 2013, 8,899 NHSC clinicians—including primary care physicians, physician
assistants, dentists, dental hygienists, nurse practitioners, certified nurse midwives, and behavioral
health professionals—provided needed health services to more than 9.3 million Americans.
37
The
program has more than doubled since 2008, when approximately 3,600 clinicians participated. NHSC
clinicians also provide needed primary care services to American Indian/Alaska Native populations,
with 620 Tribal health programs across the country approved as NHSC service sites as of October
2013. This represents a tenfold increase since 2010, when 60 Tribal health programs served as NHSC
sites.
38
Linking Low-Income Men to Medicaid. The Office of Minority Health (OMH), Assistant Secretary for
Planning and Evaluation (ASPE), and the Administration for Children and Families (ACF) are funding
research to identify promising outreach, enrollment, and messaging strategies to connect low-income
men to health insurance and care. A major component of the study is to identify strategies for key
subpopulations of low-income men, including racial and ethnic minorities.
HRSA’s New Access Point Awards. In 2012 and 2013, HRSA awarded nearly $150 million in New
Access Point awards to support 251 health center sites across the country. These centers provide
culturally competent and comprehensive primary care services to medically underserved communities.
HRSA’s new awards will promote health care access by providing primary health care services for an
additional 1.25 million patients.
39
The Indian Health Service (IHS) Improving Patient Care (IPC) Program. The IPC Program works to
transform the Indian health care system by developing high-performing, innovative health care teams
to improve the quality of and access to care by utilizing a patient-centered medical home model.
Participating IHS/Tribal/Urban Indian health programs receive training to deliver comprehensive
services through coordinated care across all elements of the health system to improve continuity of
care, enhance access, and partner with community-based health programs and Tribal organizations.
Using evidence-based medicine in guiding shared decision making with patients and families, a
positive relationship among the health system, care team, individual, family, community, and tribe is
strengthened. Currently, 172 federal, tribal and urban sites have participated in or are currently
13

participating in the Improving Patient Care (IPC) Program.
Reduce disparities in the quality of health care
Though quality of care for racial and ethnic minority populations is slowly improving, significant
disparities persist between the quality of care received by Whites and that received by many racial and
ethnic minorities.
40
For example, African Americans are far more likely than non-Hispanic Whites to be
hospitalized for heart failure. Within the state of Hawaii, Native Hawaiians and Other Pacific Islanders
also have higher rates of hospital admissions for heart failure than Whites.
41
Although some
hospitalizations for heart failure are considered unavoidable, rates of hospitalization can be linked to the
quality of outpatient care received.
42
Other disparities exist in the quality of care received; for example,
Asian Americans are less likely than Whites to receive recommended hospital care for pneumonia.
43
In
another example, African American mothers are less likely than White mothers to receive adequate
prenatal care.
44
The quality and quantity of prenatal care pregnant women receive may influence a range
of birth outcomes, including low birth weight and preterm birth.
HHS is taking a range of actions to address such disparities in quality, including promoting the
development of interventions to prevent the leading causes of premature death among racial and ethnic
minority populations.
Million Hearts
TM
Initiative. Million Hearts™ is a multifaceted public-private partnership that aims to
prevent one million heart attacks and strokes by 2017. The initiative has brought together 86 partners to
implement programs, policies, and campaigns to promote cardiovascular health.
45
Specific activities
have included use of quality improvement strategies to increase the quality of care provided for high
blood pressure and high cholesterol, as well as broader public health education campaigns to reduce
smoking and sodium intake. In 2013, Million Hearts™ launched its Hypertension Control Challenge to
reward health systems and clinicians who are successful in working with their patients to achieve 70
percent hypertension control rates.
46
100 Congregations for Million Hearts
The 100 Congregations for Million Hearts initiative was launched in February 2013. Its goal is to
encourage faith-based organizations to increase awareness and action around heart disease prevention and
blood pressure control. As part of the initiative, congregations:
Designate a Million Hearts Advocate who serves as a resource for heart health information and links
individuals to needed services;
Establish and/or strengthen relationships with community pharmacists, health centers, and health
workers;
Distribute messages about the importance of controlling high blood pressure and action steps taken to
promote this control;
Promote the Heart Health Mobile App that helps determine and reduce an individual's heart attack and
stroke risk; and
Distribute blood pressure tracking wallet cards.
14

Since its inception, 51 congregations have committed to the 100 Congregations for Million Hearts
initiative.
Goal II: Strengthen the Nation’s Health and
Human Services Infrastructure and Workforce
Patient-provider relationships are shaped by the experiences, culture, values, and expectations of both the
provider and the patient. Racial and ethnic minority patients tend to have more mistrust of health care
professionals and perceive more discrimination in the health care system than do non-Hispanic Whites.
47
Further, a lack in providers’ knowledge about the culture and language of their patients can lead to
misunderstandings in patient and provider interactions. Patients from racial and ethnic minority
populations often report greater satisfaction with health care from providers of the same race, ethnicity, or
culture. That commonality makes a provider more successful at gaining patients’ trust and improves the
ability to communicate in a more culturally and linguistically competent manner.
48
This evidence
underscores the need for health professionals with diverse backgrounds and improved competencies to
care for and serve racial and ethnic minority populations. Currently, the racial and ethnic makeup of the
health care workforce lags behind that of the U.S. population. For example, although 13 percent of
Americans are Black and 16 percent are Latino, only 6 percent of physicians are Black and 5 percent
Latino.
49, 50
Increasing the number of health professionals from racial and ethnic minority populations may
help increase the quality of patient-provider interactions, thereby helping to improve these populations’
patient experiences.
Thus, strengthening the nation’s health and human services infrastructure and workforce involves both
incorporating cultural and linguistic knowledge among the health care workforce, and increasing the
number and diversity of health care professionals. Goal II of the HHS Disparities Action Plan supports the
following strategies and actions:
Increase the ability of all health professions and the healthcare system to identify and
address racial and ethnic health disparities
HHS agencies are engaged in several activities to promote provision of care and services respectful of and
responsive to the cultural and linguistic needs of diverse communities. These include developing tools to
help health and health care organizations identify the cultural and linguistic needs of the communities they
serve, and enhancing standards for culturally and linguistically appropriate services in health and health
care.
National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care
(National CLAS Standards). OMH released the enhanced National CLAS Standards in April 2013,
marking the first update since the original standards were published in 2000.
51
The enhanced National
CLAS Standards are intended to advance health equity, improve quality, and help eliminate health care
disparities by providing a blueprint for individuals and health and health care organizations to
implement culturally and linguistically appropriate services. The enhancements to the National CLAS
Standards reflect the nation’s increasing diversity and the tremendous growth in the fields of cultural
and linguistic competency over the past decade, and help to ensure relevance to new national policies
and legislation, such as the Affordable Care Act.
Medical Schools Curriculum Initiative. Through this Initiative, the Office for Civil Rights’ (OCR)
15

enhances medical school instruction by helping future medical practitioners appreciate their role in
reducing health disparities. The curriculum, “Stopping Discrimination Before It Starts: The Impact of
Civil Rights Laws on Health Care Disparities,” was developed with funding and support from the
National Institutes of Health and the Stanford University School of Medicine. The curriculum is
published in the Association of American Medical Colleges’ (AAMC) MedEdPORTAL. Currently,
Emory University, the University of Colorado, and the University of Kansas have incorporated the
curriculum into their medical school programs. Most recently, OCR introduced the curriculum to
nearly 1,000 students at 12 medical and dental schools participating in the AAMC’s Summer Medical
and Dental Education Program (SMDEP).
Promoting Effective Communication in Health Care Organizations. OCR conducted compliance
reviews of 45 Critical Access Hospitals (CAH), one hospital in each of the 45 states served by the CAH
program. The purpose of the reviews was to improve language access services in rural communities for
individuals with limited English proficiency. OCR reviewed service area data; evaluated language
access policies and procedures; conducted on-site visits; interviewed hospital staff and community
stakeholders; provided technical assistance; and secured corrective actions for compliance issues.
Additionally, OCR, in collaboration with the American Hospital Association, provided technical
assistance to hospital associations in 17 states to help hospital administrators and staff understand the
applicable federal anti-discrimination laws, and implement practices that ensure meaningful access to
individuals who are limited English proficient (LEP) or deaf or hard of hearing.
Promoting effective communication in healthcare organizations
The Office for Civil Rights (OCR) and the South Dakota Association of Healthcare Organizations,
together with the Centers for Medicare & Medicaid Services (CMS), distributed “I Speak” language cards
to health care organizations throughout the state. The cards include both Native American languages and
foreign languages spoken in the state, and explain individuals’ rights to free interpretation and translation
services.
Promote the use of community health workers and promotores de salud
Community health workers (CHWs) and promotores de salud increase access to and utilization of care by
providing health insurance enrollment assistance and health education to their communities.
52, 53, 54
They
act as a bridge between the community and the health care system, providing community members with
social support and education, and facilitating access to care as needed. In recognition of their critical role,
HHS agencies are using multiple approaches to utilize CHWs and promotores de salud to increase the
health system’s ability to provide culturally and linguistically competent care to diverse communities.
National Hispanic Council on Aging (NHCOA) Portal e-Comunidad. OMH supported NHCOA in the
development of Portal e-Comunidad, an e-learning platform to provide promotores de salud with an
easy-to-use and accessible platform to learn about and promote health literacy among Latino seniors in
their communities. The platform currently consists of five modules of 20 to 40 minute lessons given via
narrated PowerPoint presentations, “managing medications at home” and “how to get the most out of a
doctor’s visit” are examples of the topics presented. Tools like the Portal e-Comunidad help connect
promotores de salud who serve hard-to-reach audiences, such as Hispanic older adults, with relevant,
important, and necessary learning opportunities to which these audiences may not have easy access
through other channels.
16

Figure 4.
Increase the diversity of the health care and public health workforces
HHS has demonstrated a commitment to promoting medical and scientific educational opportunities for
individuals from racial and ethnic minority populations that are underrepresented in the public health and
health care professions. Such opportunities aim to increase the proportion of health and human services
providers with the same linguistic and cultural backgrounds as the individuals they serve, thereby
increasing the provision of culturally and linguistically appropriate care and services. One of the largest
and longest-standing programs reflecting HHS efforts under this strategy is the NHSC, administered by
HRSA, which provides scholarships and loan repayment support to health care professionals who enter
into service in underserved areas. More than half of the 1,100 NHSC Scholars in the pipeline are members
of racial and ethnic minority populations.
55
Additional HHS programs and activities that strive to
increase diversity in the public health, health care,
and research workforces are highlighted below.
Centers for Disease Control and Prevention
(CDC) Undergraduate Public Health Scholars
(CUPS) Program. This program, funded through a
cooperative agreement with CDC, supports four
academic institutions in their efforts to increase
interest in public health and biomedical sciences
among students from underrepresented racial and
ethnic minority populations. The program consists
of a 10-week summer internship at state and local
health departments, hospitals, community-based
organizations, or CDC, complemented by
employment guidance and support for considering
public health as a career choice. It is expected that
exposure to public health practice will heighten
awareness of, and interest in, public health careers
and thus increase the diversity of the workforce. In
the first three years of the program, 8,407 students
applied to the program, and 578 students were
accepted and completed the CUPS program.
Historically Black Colleges and Universities
(HBCUs) Center for Excellence in Behavioral
Health. This center, overseen by the Substance
Abuse and Mental Health Services Administration
(SAMHSA), supports HBCUs in promoting
behavioral health education, expanding behavioral
health service capacity, and facilitating workforce
development. It aims to increase the diversity and
cultural competence of the behavioral health
workforce by training teams of clinicians, faculty,
and students from HBCUs on best practices in
behavioral health promotion and prevention,
screening and referral services, and intervention
.
17
Improving the Cultural Competency and Diversity of the Behavioral Health
Workforce
In FY 2013, the Historically Black Colleges and Universities (HBCUs) Center for Excellence in
Behavioral Health:
– Awarded 86 Behavioral Health Capacity Expansion mini-grants to institutions that established
more than 550 behavioral health internships for undergraduate and graduate students;
– Trained 477 faculty, 572 students, and 120 military veterans via the Kognito At-Risk online behav-
ioral health training tool;
– Provided internship opportunities to 89 undergraduate and graduate students: 10 interns were
offered extended employment opportunities;
– Hosted webinars with more than 675 participants on topics such as addiction; bullying; and work-
ing with lesbian, gay, bisexual, transgender, and queer youth; and
– Trained 970 students, 134 faculty/staff, 155 peer educators, and 160 other campus community
individuals in behavioral health suicide prevention and mental health skills.
• Health Profession Opportunity Grants (HPOG). Authorized by the Affordable Care Act and
administered by the Administration for Children and Families (ACF), HPOG provides education and
training to Temporary Assistance to Needy Families (TANF) recipients and other low-income
individuals to pursue jobs in health care. ACF has awarded 32 five-year grants to organizations in 23
states. These organizations—including community colleges, community-based organizations, and
Tribal organizations—offer training and credentials for nurse aides, home health aides, registered
nurses, medical assistants, and pharmacy technicians.
Increasing Training and Education Opportunities for Low-Income Individuals in
Health Care Occupations
As of December 2013:
– 20,382 individuals had enrolled in Health Profession Opportunity Grants (HPOG) health care
occupation training programs
– 12,384 individuals had completed HPOG health care occupation training programs
Increasing Training and Education Opportunities for American Indians and Alaska
Natives in Health Care Occupations
Through the HPOG program, five demonstration project grants were awarded to Tribal organizations and
colleges in 2010 to increase American Indian and Alaska Native (AI/AN) representation in the health care
workforce. Funded entities offer courses for health care careers, including certified nursing assistant
(CNA), licensed practical nurse (LPN), registered nurse (RN), emergency medical technician (EMT), and
medical billing and coding. In the first two years of the program:
– All sites have enrolled participants into training programs, with enrollment ranging from 36−208
students
– 25−41 percent of program participants have obtained employment after program completion
18

– Many CNA participants have continued their education at two- or four-year nursing programs
Building Infrastructure Leading to Diversity (BUILD) Initiative. The BUILD initiative aims to increase
the diversity of the National Institutes of Health (NIH) funded workforce by supporting collaborative
programs that include novel approaches for enhancing undergraduate education, training, and
mentorship, as well as infrastructure support and faculty development to facilitate those approaches. In
2013, BUILD planning grants were awarded to 15 colleges and universities to help these institutions
develop the necessary partnerships and infrastructure needed to be competitive for the BUILD
initiative.
National Disaster Medical System (NDMS). Disasters affect communities unequally. Low-income,
minority populations often live and work near risk-prone locations; for example, areas prone to
flooding, landslides, and industrial hazards; areas with non-compliant building code housing and
buildings; and places with greater dependence on public transportation. Areas with fewer economic
resources can be predicted to be less resilient when faced with a disaster. Examples of this include
low-income, minority individuals and families may be less resilient when facing the adverse effects of
disasters due to challenges in storing emergency food and supplies or having the capacity to evacuate to
safety. During a response well-meaning outside, responders cannot necessarily understand the
challenges and needs of these communities. The Office of Assistant Secretary for Preparedness and
Response (ASPR) has developed an action plan that includes strategies to increase representation of
racial and ethnic minorities in the public health emergency preparedness and response workforce. This
plan includes conducting outreach about the NDMS at HBCU medical and nursing schools, sponsoring
workshops at key professional meetings, and offering public-private community disaster graduate
fellowships. ASPR also promotes cultural competency among ASPR staff and NDMS personnel by
providing online training in Psychological First Aid, a disaster-specific behavioral health intervention
for providers offered through the National Association of City & County Health Officials (NACCHO)
that helps providers meet the needs of diverse populations.
Building the Capacity of the Preparedness and Response Workforce
As of January 2013, 53 languages/dialects were represented among staff members of the National Disaster
Medical System (NDMS).
As of September 2012, more than 2,800 NDMS and U.S. Public Health Service personnel had taken an
online Psychological First Aid training course as part of wider cultural competency efforts. This
70-minute online training is offered through the National Association of City & County Health Officials
(NACCHO).
Goal III: Advance the Health, Safety, and
Well-Being of the American People
Health disparities are an outcome of community and environmental factors, not just those in the health
care system. These factors, sometimes referred to as the social determinants of health, are conditions in the
environments in which people are born, live, learn, work, play, worship, and age that affect a wide range
of health, functioning, and quality-of-life outcomes and risks.
56
Resources that enhance quality of life,
such as access to safe and affordable housing, education, public safety, healthy foods, and health services,
19
can have a significant influence on population health outcomes.
57
Therefore, approaches that go beyond
the health care system are needed to reduce health disparities and promote health equity among racial and
ethnic minority populations. Community-based and ecological approaches that support the creation of
healthy and safe environments, that promote healthy behaviors, and that are implemented in the
community, at the workplace, and through policy are promising strategies for advancing the health, safety,
and well-being of the American people.
58, 59
Figure 5.
Recognizing the potential of community-based and ecological approaches to eliminate health disparities,
Goal III supports building community capacity to develop and implement health initiatives that reach
racial and ethnic minority populations. Specifically, Goal III supports the following two strategies:
Reduce disparities in population health by increasing the availability and
effectiveness of community-based programs and policies
HHS agencies support a wide range of community-based programs to promote healthy behaviors and
prevent disease among racial and ethnic minority populations. These programs focus on providing health
education, enabling access to services, and linking individuals to community resources. They target a
variety of health problems, including chronic disease prevention and management, tobacco cessation,
maternal and child health, and mental health.
Public Awareness Campaign to Increase Patient Participation in Health Decision Making. In the
Toma las Riendas (Take the Reins) campaign, AHRQ is partnering with organizations that primarily
serve the Hispanic community to promote Spanish-language resources that encourage consumers to
become more active partners in their health care. These materials convey information on the benefits
and risks of treatment options for multiple conditions, and encourage shared decision making between
patients and their health teams. Information is available in print through condition-specific consumer
20

guides, brochures, and postcards, and is disseminated via the AHRQ website, Facebook and Twitter,
radio advertisements, and placement of print materials in public venues.
Tips From Former Smokers Tobacco Education Campaign. In March, 2012, Centers for Disease
Control and Prevention’s Office on Smoking and Health launched the first ever paid national tobacco
education campaign called Tips From Former Smokers (Tips). The development of the Tips campaign
was based on evidence from both national and international literature, which shows that graphic ads
linking smoking to health damage and that evoke strong negative emotions, are the most effective in
promoting tobacco use cessation among adults and reducing initiation in youth. The primary target
audience of the campaign is low SES smokers, ages 18 to 54 and secondary audiences include parents;
family members; health care providers; and the faith-based community.
Since it began in 2012, the Tips campaign has reached diverse population groups including those
groups experiencing the highest rates of tobacco use disparities. Most recently, the 2014 Tips campaign
reached diverse groups through its national media buy, including running Spanish language TV ads on
Spanish-language stations. The national reach to African American audiences was augmented in local,
high smoking prevalence markets by emphasizing media placements that focused on African American
audiences in markets where they were predominant. The national reach to lesbian, gay, bisexual, and
transgender (LGBT) audiences was enhanced through focused digital and print advertising in media
properties that specialize in reaching them. Tips print ads also ran in Asian-language newspapers across
the country. The ads included Chinese, Vietnamese and Korean-language executions, promoted
asiansmokersquitline.org and offered free nicotine replacement therapy. Local radio, magazines and
newspapers that serve reservations and American Indian and Alaska Native communities also ran Tips
ads.
In an article published in The Lancet in September, 2013, CDC reported on main outcomes from our
evaluation of the Tips 2012 Campaign. Among the findings were that an estimated 1.6 million
Americans tried to quit smoking because of the 2012 Tips Campaign and, at a minimum, more than
100,000 Americans quit smoking long-term because of Tips. The campaign is also incredibly cost
effective: As reported in the American Journal of Preventive Medicine, the 2012 campaign prevented
at least 17,000 premature deaths and saved nearly 180,000 quality adjusted life years.
Consortium of National Networks to Impact Populations Experiencing Tobacco-Related and Cancer
Health Disparities. Since FY 2013, CDC has provided funding for a consortium of population-specific,
public health-oriented, national networks to impact tobacco-related and cancer health disparities
among specific target populations. The networks enhance the quality and performance of specific
public health programs, public health data and information systems, public health practice and services,
public health partnerships, and public health resources that focus on tobacco-related and cancer health
disparities in specific populations. The target populations are: 1) African Americans; 2) American
Indians/Alaskan Natives; 3) Asian Americans/Pacific Islanders/Hawaiian Natives; 4)
Latinos/Hispanics; 5) Lesbian, Gay, Bisexual and Transgender persons; 6) persons with low
socioeconomic status; 7) persons with mental health and substance abuse disorders; and 8)
geographically defined populations with high commercial tobacco use and related health disparities.
Encouraging Spanish speakers to be active partners in their health care
Since the Toma las Riendas campaign launch in November 2011:
– The Spanish-language Facebook page has received 14,425 unique page visits.
21

– 89 media outlets have published the press release.
– Nearly 3,000 versions of placards have been placed in public venues, including buses, transit
shelters, and malls, reaching a potential audience of more than 36 million people.
Population Assessment of Tobacco and Health Study (PATH). In 2013, the Food and Drug
Administration (FDA) and NIH launched a five-year study of more than 50,000 people ages 12 and
older to examine tobacco use attitudes and behaviors across racial and ethnic minority populations, and
investigate the effectiveness of interventions aimed at reducing tobacco use, such as tobacco-free
policies, quitline promotion, and various tobacco cessation programs. Results from the PATH study
will inform educators about how to tailor prevention and cessation programs to diverse communities.
Public-Private Partnerships to Improve Vaccination Rates. Immunization disparities are a persistent
public health problem that require targeted intervention at both the community and national levels.
Some causes of these disparities include cost factors, lack of access, perceived lack of susceptibility to
vaccine-preventable diseases, and a lack of culturally appropriate education. OMH initially established
for the 2010−2011 influenza season the Walgreens-HHS Co-Sponsorship Agreement, which provides
uninsured individuals with free seasonal influenza vaccination. Walgreens has committed over $10
million annually to support this effort; since 2010, the partnership has successfully vaccinated more
than half a million individuals who otherwise would not receive the influenza vaccination due to cost.
Utilizing Walgreens’ local pharmacies and pharmacists, HHS provides linkages to underserved
communities through its Regional Health Administrators and Regional Minority Health Consultants
for the coordination of community health education and vaccination clinics and events.
HHS-collaborating agencies include the National Vaccine Program Office (NVPO), CDC, the
Administration for Community Living (ACL), and the Office of the Assistant Secretary of Health
(OASH) regional offices. NVPO coordinates and ensures collaboration between federal agencies and
private organizations involved in vaccination and immunization activities. Between April 2012 and
September 2013, NVPO offered grants to support community-level efforts to deliver culturally
appropriate immunization interventions. NVPO also has developed a real-time web tool to map flu
vaccine disparities across geographic regions.
Improving vaccination rates
Between April 2012 and September 2013, the National Vaccine Program Office (NVPO):
Partnered with the National Institute on Minority Health and Health Disparities (NIMHD) to fund three
grants to increase influenza vaccine coverage. Funded interventions included the following:
– A virtual patient advocate system, with communication tailored to pregnant African American
women and their primary care providers;
– An evidence-based demonstration to increase influenza vaccination rates among low-income
pregnant women who receive health care at Federally Qualified Health Centers (FQHCs) in Puerto
Rico; and
– Evidence-based approaches to increase influenza and pertussis vaccination among low-income
racial and ethnic minority adults with diabetes.
22

Conduct and evaluate pilot tests of health disparity impact assessments of selected
proposed national policies and programs
HHS supports the use of health disparity impact assessments as a method for creating and disseminating
information about the likelihood of proposed policies and programs for increasing or decreasing health
and healthcare disparities among racial and ethnic minority populations.
Equity in All Policies. The National Partnership for Action to End Health Disparities (NPA) is
implemented at the federal level through the activities of the Federal Interagency Health Equity Team
(FIHET). The FIHET currently comprises 12 federal agencies, including HHS and other agencies, such
as the Departments of Justice, Veterans Affairs, Transportation, and Agriculture. The FIHET convenes
on the central theme of health equity and is intended to increase dialogue between traditionally siloed
programs in ways that enhance cross-agency coordination, maximally leverage existing resources, and
ultimately increase the impact of federal resources in communities. The FIHET has identified “Equity
in All Policies that Affect Health and the Social Determinants of Health” as one of its project areas. The
overarching objective for this project area is to “promote the consideration of equity in the development
and implementation of all policies and programs of public and private organizations, in recognition
that all policies and programs have the potential to impact health and the social determinants of
health.” In selecting this project area and overarching objective, the FIHET aims to provide leadership
on health equity through several activities, including those that (a) identify promising practices and
opportunities to ensure the conditions for optimal health for all people; and (b) convene subject matter
experts and stakeholders to share knowledge, experience, and promising practices for promoting the
consideration of equity in programs, policies, and practices.
Promoting Equity in All Policies Among Internal and External Stakeholders
In September 2013, the Federal Interagency Health Equity Team (FIHET) Equity in All Policies work
group conducted a panel session at the National Health Impact Assessment conference in Washington, DC
on ongoing efforts to integrate or consider equity in policies and programs in the public health, private
health, and non-health sectors. The panel highlighted state-of-the-art strategies with respect to approaches
for considering equity in programs and policies, the role of partnerships in driving systemic change, and
practical applications of assessment tools and methods in efforts to consider and integrate equity. Featured
panelists represented federal, state, and local government organizations. The panel also highlighted
process, data, and methodology challenges, and research needs to inform a more robust evidence base for
integrating the social determinants of health into effective policies.
Goal IV: Advance Scientific Knowledge and
Innovation
Efforts to advance scientific knowledge and innovation can improve prevention and health care services
for all populations, and increase the quality of health, public health, and biomedical research. More
specifically, health disparities research can inform initiatives to improve the health of racial and ethnic
minorities by bridging the gap between knowledge and practice. However, the capacity of HHS to identify
health and health care disparities and monitor efforts to address them is limited by a lack of high-quality
health data that include details about race, ethnicity, and language, as well as a scarcity of research that
specifically addresses the health care needs of racial and ethnic minorities. For this reason, the HHS
23

Disparities Action Plan includes a goal to explicitly support the promotion of the collection of race and
ethnicity data, especially in a standardized format; evaluate existing and new biomedical and public health
approaches that reduce health disparities, thereby improving the evidence base; and strengthen
information systems to support dissemination and sharing of data and results.
Increase the availability and quality of data collected and reported on racial and
ethnic minority populations
To support efforts to identify effective strategies to reduce health disparities, agencies have conducted
activities to improve the availability, specificity, uniformity, and quality of data collection and reporting;
improve public access to HHS data on racial and ethnic minorities; and regularly publish estimates of
health outcomes for racial and ethnic minority populations.
Native Hawaiian/Pacific Islander (NHPI) National Health Interview Survey (NHIS). This project, led
by CDC’s National Center for Health Statistics (NCHS), aims to enhance the availability and quality of
data on the health outcomes and health care utilization of NHPIs. NHPIs comprise 0.4 percent of the
total U.S. population, which can make it difficult to include them in sufficient numbers in most
population-based health surveys. Although the limited data currently available on NHPIs indicate that
they experience significant health disparities, the lack of more reliable data has made it difficult to
monitor these disparities and plan interventions. To support participation in the survey and increase
response rates, NCHS, OMH, and the Census Bureau partnered to provide outreach and education on
the project to NHPI stakeholders. NHPI NHIS data collection began in February 2014, and findings
will be made available in mid-2015. These findings will be used by policymakers, community leaders,
and others to design policies and programs to improve NHPI health and well-being.
61
The National Healthcare Quality and Disparities Report (QDR). AHRQ plays a critical role in
increasing the availability and quality of data collected and reported on racial and ethnic minority
populations by annually producing the National Healthcare Disparities Report. AHRQ’s National
Healthcare Quality Report provides a comprehensive view of access to and the quality of health care in
the U.S. Both reports track more than 250 measures of health care quality and access among different
racial and ethnic populations. In 2014, AHRQ combined the National Healthcare Disparities Report
with the National Healthcare Quality report. This combined report provides a comprehensive picture of
the state of health care experienced by the general population and racial and ethnic minorities. To
support data queries by specific parameters the QDR unified web tool supports data searches utilizing
numerous social, race, and ethnic parameters.
Patient-Centered Outcomes Research (PCOR). PCOR can help providers and patients make sound
health care decisions by providing evidence on the effectiveness, benefits, and harms of different
treatment options. By working collaboratively with research and health care institutions, HHS is
working to develop, implement, and test strategies to increase the adoption and dissemination of
interventions based on PCOR among racial and ethnic minority populations. To advance this type of
research, AHRQ funded 21 three-year grants to research institutions that focused on content
customizations of comparative effectiveness research materials for populations underserved or
unserved by the health care system, including racial and ethnic minorities.
Conduct and support research to inform disparities reduction initiatives
To gather accurate data, understand the root causes of health disparities, and evaluate the effectiveness of
24

interventions aimed at reducing persistent racial and ethnic health disparities, HHS supports research in a
variety of areas, such as obesity, cancer, diabetes, and access to preventive services. It also promotes the
use of emerging methodologies, such as PCOR and community-based participatory research (CBPR)
methods. HHS encourages collaborative research across federal departments, promotes the dissemination
of evidence-based interventions, and expands training opportunities and supportive infrastructure among
institutes of higher education. Together, these activities are expected to bridge the gap between knowledge
and practice, and lead to the development of more effective interventions to help attain health equity.
Community Networks Program Centers (CNPCs) and Regional Centers for Reducing Cancer Health
Disparities. To address cancer and other related co-morbidities with documented health disparities, the
NIH/National Cancer Institute (NCI) funded 23 CNPCs. CNPCs use CBPR methods to increase
knowledge of, access to, and use of preventive screening, diagnosis, and treatment in communities, and
thus reduce cancer disparities among racial and ethnic minority populations. The CNPCs also provide
mentorship and training to new researchers—particularly those from underrepresented
backgrounds—in the fields of CBPR and cancer health disparities research.
Supporting Research and Training Opportunities for Reducing Cancer Disparities
Since October 2012:
23 Community Networks Program Centers (CNPCs) have been funded;
221 individuals have received training in community-based participatory research (CBPR) methods;
CNPCs have collaborated with more than 150 clinical partners to provide appropriate screening,
follow-up, and treatment services to underserved populations;
24% (871) of individuals who attended workshops and community presentations provided by CNPCs
reported increases in knowledge about cancer health disparities after the event; and
85% (2119) of individuals who attended workshops and community presentations provided by CNPCs
reported increases in their use of beneficial and behavioral biomedical procedures.
Goal V: Increase Efficiency, Transparency, and
Accountability of HHS Programs
Because of the complexity of health disparities, no one office or agency can solve the problem of health
disparities alone; thus, HHS promotes collaboration across the Department to maximize efforts and
optimize results. To ensure that programs and policies are efficient, transparent, and accountable, HHS
has established systems to support information sharing across agencies and minimize duplication of
efforts. HHS also has implemented processes to track, assess, and report on the impact of programmatic
and policy efforts to address health disparities. These processes include tracking existing performance
measures and other government data on health system indicators and making them available to the public
(such as those available via the Health System Measurement Project).
25

Figure 6.
Health System Measurement Project. The Assistant Secretary for Planning and Evaluation (ASPE)
Health System Measurement Project allows public access, via a website, to data that provide a picture
of the evolving status of the U.S. health system,
including trends in racial and ethnic health and health
care disparities. The project tracks measures in 10
topic areas, such as health care costs and affordability,
health care coverage, the health care workforce, and
population health. The data can be used by individuals
and organizations inside and outside of government to
track changes in these health system characteristics
over time and identify areas that require improvement.
Recognizing the importance of tracking changes in
disparities in health and health care, the project
includes a dashboard dedicated to “Vulnerable
Populations,” which tracks measures that consistently
have been associated with disparities across
populations.
The Health System Measurement Project:
Vulnerable Populations Dashboard
The dashboard tracks and allows public access to
measures known to reflect consistent health disparities,
including the following:
The percentage of people who have a usual source of
medical care;
The percentage of infants born at low birth weight;
The percentage of people with high blood pressure that is controlled;
The percentage of people who experience good communication with their health care provider; and
Website available at https://healthmeasures.aspe.hhs.gov/topic/I.
26
Conclusion
Agencies contributing to the HHS Disparities Action Plan have developed an extensive, multifaceted set
of activities that span a wide range of populations, address a multitude of individual and system-level
barriers to health and quality health care, and support the growth of a more diverse health care workforce.
Guided by the HHS Secretary’s strategic priority to eliminate health disparities and the HHS Disparities
Action Plan, HHS agencies have demonstrated their commitment to reducing racial and ethnic health
disparities, and built their capacity to address these disparities. Goal I activities have expanded access to
health insurance and health care for millions of racial and ethnic minorities through the Affordable Care
Act, while agencies working on Goal II have taken steps to increase access to a highly qualified, diverse,
and culturally competent public health and health care workforce. Public awareness campaigns conducted
under Goal III have employed culturally sensitive messaging techniques to promote healthy behaviors
among racial and ethnic minorities. Agencies working on Goal IV have conducted research to support the
development of innovative, evidence-based interventions to address health disparities and are monitoring
their effectiveness. With regard to Goal V, HHS agencies are tracking, evaluating, and reporting on efforts
to address health disparities so that results are optimized. HHS efforts related to implementation of the
HHS Disparities Action Plan have generated ideas, materials, and data that will help the Department
advance toward its vision of a nation free from disparities in health and health care.
27
References
1 Section 4302 of the Affordable Care Act defines new standards for the collection of race and ethnicity
data on population subgroups. The new standards have been formally adopted by the Secretary for
application in all HHS-sponsored population health surveys involving self-reporting. The new
standards include categories for five ethnicity populations: (1) Not of Hispanic, Latino/a, or Spanish
origin; (2) Mexican, Mexican American, Chicano/a; (3) Puerto Rican; (4) Cuban; and (5) Another
Hispanic, Latino/a, or Spanish origin. The new standards also include categories for 14 racial pop-
ulations: (1) White; (2) Black or African American; (3) American Indian or Alaska Native; (4) Asian
Indian; (5) Chinese; (6) Filipino; (7) Japanese; (8) Korean; (9) Vietnamese; (10) Other Asian; (11)
Native Hawaiian; (12) Guamanian or Chamorro; (13) Somoan; and (14) Other Pacific Islander.
2 Agency for Healthcare Research and Quality. 2012 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/index.html
. Accessed March 3, 2014.
3 Ko HK., Graham G, Glied SA. Reducing racial and ethnic disparities: the action plan from the Depart-
ment of Health and Human Services. Health Aff. 2011;30:1822-1829.
4 Centers for Disease Control and Prevention. Healthy People 2010: final review.
http://www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf. Published December 2012.
Accessed March 3, 2014.
5 HealthyPeople.gov. Disparities.
http://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities. Accessed March
7, 2014.
6 World Health Organization. Social determinants of health.
http://www.who.int/social_determinants/en/. Accessed March 3, 2014.
7 The World Health Organization defines the social determinants of health as “the circumstances in
which people are born, grow up, live, work and age, and the systems put in place to deal with illness.
These circumstances are in turn shaped by a wider set of forces: economics, social policies, and
politics.”
8 U.S. Department of Health and Human Services. Healthy People 2010: final review.
http://www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf. Accessed April 29, 2014.
9 Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care.
http://iom.nationalacademies.org/Reports/2002/Unequal-Treatment-Confronting-Racial-and-Ethnic-
Disparities-in-Health-Care.aspx. Published 2002. Accessed March 3, 2014.
10 Kaiser Family Foundation. State health facts: uninsured rates for the nonelderly by race/ethnicity,
2012. http://kff.org/uninsured/state-indicator/rate-by-raceethnicity/. Accessed March 3, 2014.
11 Agency for Healthcare Research and Quality. 2012 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/index.html. Accessed March 3, 2014.
12 Agency for Healthcare Research and Quality. 2008 National Healthcare Disparities Report.
http://www.ahrq.gov/research/findings/nhqrdr/index.html. Accessed March 3, 2014.
13 Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care.
http://iom.nationalacademies.org/Reports/2002/Unequal-Treatment-Confronting-Racial-and-Ethnic-
Disparities-in-Health-Care.aspx. Published 2002. Accessed March 3, 2014.
14 Institute of Medicine. In the nation’s compelling interest: ensuring diversity in the health care work-
force.
28

http://iom.nationalacademies.org/Reports/2004/In-the-Nations-Compelling-Interest-Ensuring-Divers
ity-in-the-Health-Care-Workforce.aspx. Published February 2004. Accessed March 3, 2014.
15 Institute of Medicine. In the nation’s compelling interest: ensuring diversity in the health care work-
force.
http://iom.nationalacademies.org/Reports/2004/In-the-Nations-Compelling-Interest-Ensuring-Divers
ity-in-the-Health-Care-Workforce.aspx. Published February 2004. Accessed March 3, 2014.
16 Agency for Healthcare Research and Quality. 2011 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhqrdr11/qrdr11.html
. Accessed March 20, 2014.
17 Association of American Medical Colleges. Diversity in the physician workforce: facts & figures 2010.
https://members.aamc.org/eweb/upload/Diversity%20in%20the%20Physician%20Workforce%20Fa
cts%20and%20Figures%202010.pdf. Published 2010. Accessed March 3, 2014.
18 Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report – United
States, 2013. http://www.cdc.gov/mmwr/pdf/other/su6203.pdf. Published November 22, 2013.
Accessed March 3, 2014.
19 U.S. Department of Health and Human Services Office of Minority Health. Hepatitis and Asian
Americans. http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=50
. Accessed March 20,
2014.
20 Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report – United
States, 2013. http://www.cdc.gov/mmwr/pdf/other/su6203.pdf. Published November 22, 2013.
Accessed March 3, 2014.
21 Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report – United
States, 2013. http://www.cdc.gov/mmwr/pdf/other/su6203.pdf. Published November 22, 2013.
Accessed March 3, 2014.
22 Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report – United
States, 2013. http://www.cdc.gov/mmwr/pdf/other/su6203.pdf. Published November 22, 2013.
Accessed March 3, 2014.
23 Institute of Medicine. Race, ethnicity, and language data: standardization for health care quality
improvement. http://iom.nationalacademies.org/Reports/2009/RaceEthnicityData.aspx. Published
August 31, 2009. Accessed March 3, 2014.
24 National Partnership for Action to End Health Disparities. National stakeholder strategy for achieving
health equity. http://minorityhealth.hhs.gov/npa/templates/content.aspx?lvl=1&lvlid=33&ID=286.
Published April 2011. Accessed March 3, 2014.
25 U.S. Department of Health and Human Services. HHS action plan to reduce racial and ethnic dispar-
ities: a nation free of disparities in health and health care.
http://www.minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf. Published April
2011. Accessed March 3, 2014.
26 U.S. Department of Health and Human Services Office of Minority Health. Final data collection
standards for race, ethnicity, primary language, sex, and disability status required by section 4302 of
the Affordable Care Act. http://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=2&lvlid=23
.
Accessed March 25, 2014.
27 Dorsey R, Graham G, Glied S, Meyers D, Clancy C, Koh H. Implementing health reform: improved
data collection and the monitoring of health disparities. Annu Rev Public Health. 2014;18(35):123-38.
28 Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing
racial/ethnic disparities in access to care. Health Serv Res. 2003;38:809-829.
29

29 Brown ER, Ojeda V, Wyn R, Levan R. Racial and ethnic disparities in access to health insurance and
health care. Los Angeles, CA: UCLA Center for Health Policy Research and the Henry J. Kaiser
Family Foundation; April 2000.
30 Hadley J, Holahan J. The cost of care for the uninsured: what do we spend, who pays, and what would
full coverage add to medical spending? Washington, DC: The Kaiser Commission on Medicaid and
the Uninsured; May 2004.
31 Agency for Healthcare Research and Quality. 2012 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/index.html. Accessed March 3, 2014.
32 Long SK. What is the evidence on health reform in Massachusetts and how might the lessons from
Massachusetts apply to national health reform?
http://www.urban.org/research/publication/what-evidence-health-reform-massachusetts-and-how-mi
ght-lessons-massachusetts-apply-national-health-reform. Published June 2012. Accessed March 1,
2014.
33 Kaiser Family Foundation. Status of state action on the Medicaid expansion decision, 2014.
http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affor
dable-care-act/. Accessed March 1, 2014.
34 Agency for Healthcare Research and Quality. 2012 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/index.html. Accessed March 3, 2014.
35 Centers for Disease Control and Prevention. 2012 National Health Interview Survey: Percentage of
People Who Have a Usual Source of Medical Care. https://healthmeasures.aspe.hhs.gov/measure/1.
Accessed August 5, 2014.
36 Health Resources and Services Administration. The Affordable Care Act and health centers.
http://bphc.hrsa.gov/about/healthcenterfactsheet.pdf. Accessed March 1, 2014.
37 Association of American Medical Colleges. National Health Services Corp (NHSC).
https://www.aamc.org/advocacy/meded/176378/national_health_service_corps_nhsc.html.
Accessed July 2015.
38 Health Resources and Services Administration. HRSA and American Indians and Alaska Natives.
http://www.hrsa.gov/publichealth/community/indianhealth/tribalconsoverview080513.pdf. Accessed
March 21,2014.
39 U.S. Department of Health and Human Services. HHS awards Affordable Care Act funds to expand
access to care. http://www.hhs.gov/news/press/2013pres/11/20131107a.html. Published November 7,
2013. Accessed March 1, 2014.
40 Agency for Healthcare Research and Quality. 2012 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/index.html. Accessed March 3, 2014.
41 Agency for Healthcare Research and Quality. 2012 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/index.html. Accessed March 3, 2014.
42 Agency for Healthcare Research and Quality. 2012 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/index.html. Accessed March 3, 2014.
43 Agency for Healthcare Research and Quality. AHRQ-funded research on health care for Asian Amer-
icans/Pacific Islanders.
http://www.ahrq.gov/research/findings/factsheets/minority/aapifact/index.html. Accessed March 24,
2014.
44 Agency for Healthcare Research and Quality. 2012 National Healthcare Disparities Report.
http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/index.html. Accessed March 3, 2014.
30
45 Million Hearts: the initiative. http://millionhearts.hhs.gov/aboutmh/overview.html. Accessed March 3,
2014.
46 Million Hearts: hypertension control champions.
http://millionhearts.hhs.gov/aboutmh/htn_champions.html
. Accessed March 3, 2014.
47 Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care.
http://iom.nationalacademies.org/Reports/2002/Unequal-Treatment-Confronting-Racial-and-Ethnic-
Disparities-in-Health-Care.aspx. Published 2002. Accessed March 3, 2014.
48 Ngo-Metzger Q, Telfair J, Sorkin DH, Weidmer B, Weech-Maldonado R, Hurtado M, Hays RD.
Cultural competency and quality of care: obtaining the patient’s perspective. http://www.com-
monwealthfund.org/usr_doc/Ngo-Metzger_cultcompqualitycareobtainpatientperspect_963.pdf.
Accessed March 20, 2014
49 American Community Survey. http://quickfacts.census.gov/qfd/states/00000.html. Accessed April 9,
2014.
50 Association of American Medical Colleges. Diversity in the physician workforce: facts & figures 2010.
https://members.aamc.org/eweb/upload/Diversity%20in%20the%20Physician%20Workforce%20Fa
cts%20and%20Figures%202010.pdf. Published 2010. Accessed March 3, 2014.
51 U.S. Department of Health and Human Services Office of Minority Health. Think cultural health:
advancing health equity at every point of contact. https://www.thinkculturalhealth.hhs.gov/.
Accessed March 20, 2014.
52 Kaiser Family Foundation. Optimizing Medicaid enrollment: perspectives on strengthening
Medicaid’s reach under health care reform.
http://kff.org/health-reform/issue-brief/optimizing-medicaid-enrollment-perspectives-on-strengtheni
ng-medicaids. Published April 2010. Accessed March 5, 2014.
53 Centers for Disease Control and Prevention. Community health workers/promotores de salud: critical
connections in communities. http://www.cdc.gov/diabetes/projects/pdfs/comm.pdf. Accessed March
24, 2014.
54 Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care.
http://iom.nationalacademies.org/Reports/2002/Unequal-Treatment-Confronting-Racial-and-Ethnic-
Disparities-in-Health-Care.aspx. Published 2002. Accessed March 3, 2014.
55 Health Resources and Services Administration. Testimony of Rebecca Spitzgo, before the Committee
on Health, Education, Labor and Pensions Subcommittee on Primary Health and Aging
United States Senate. http://www.hhs.gov/asl/testify/2014/04/t20140409.html. Published April 2014.
Accessed May 15, 2015.
56 U.S. Department of Health and Human Services. Healthypeople.gov: social determinants of health.
http://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health?topicid=39.
Accessed March 24, 2014.
57 U.S. Department of Health and Human Services. Healthypeople.gov: social determinants of health.
http://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health?topicid=39.
Accessed March 24, 2014.
58 Wallerstein NB, Duran B. Using community-based participatory research to address health disparities.
Health Promotion Practice. 2006;7(3):312-323.
59 Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial
and environmental concepts. Environ Health Perspect. 2004;112(17):1645.
60 Centers for Disease Control and Prevention. New project aimed at collecting health data for Native
31

Hawaiian and Pacific Islander populations.
http://www.cdc.gov/media/releases/2013/p1217-pacific-islanders.html.
61 Centers for Disease Control and Prevention. National Health Interview Survey: Native Hawaiian and
Pacific Islander (NHPI) National Health Interview Survey (NHIS).
http://www.cdc.gov/nchs/nhis/nhpi.html
. Accessed March 25, 2014.
32
Appendix A: Glossary of Acronyms
ACA Patient Protection and Affordable Care Act of 2010
ACF Administration for Children and Families
ACL Administration for Community Living
AHRQ Agency for Healthcare Research and Quality
AI/AN American Indian and Alaska Native
ASA Assistant Secretary for Administration
ASPE Assistant Secretary for Planning and Evaluation
ASPR Office of Assistant Secretary for Preparedness and Response
CDC Centers for Disease Control and Prevention
CLAS Culturally and Linguistically Appropriate Services
CMS Centers for Medicare & Medicaid Services
FDA Food and Drug Administration
FIHET Federal Interagency Health Equity Team
FPL Federal Poverty Level
FQHC Federally Qualified Health Center
FY Fiscal Year
HBCUs Historically Black Colleges and Universities
HHS U.S. Department of Health and Human Services
HRSA Health Resources and Services Administration
IHS Indian Health Service
NCHS National Center for Health Statistics
NCI National Cancer Institute
NDMS National Disaster Medical System
NHDR National Healthcare Disparities Report
NHPI Native Hawaiian and Pacific Islander
NHSC National Health Service Corps
NIH National Institutes of Health
NIMHD National Institute on Minority Health and Health Disparities
NPA National Partnership for Action to End Health Disparities
NVPO National Vaccine Program Office
OASH Office of the Assistant Secretary of Health
OCR Office for Civil Rights
OMH U.S. Department of Health and Human Services Office of Minority Health
ONC Office of the National Coordinator of Health Information Technology
A.1
SAMHSA Substance Abuse and Mental Health Services Administration
A.2
Appendix B: Overview of HHS Action Plan to
Reduce Racial and Ethnic Health Disparities
SEE APPENDIX B in PDF for formatted version.
B.1
