
2021
NATIONAL EMERGENCY MEDICAL SERVICES
EDUCATION STANDARDS
This publication is distributed by the U.S. Department of
Transportation (DOT), National Highway Trafc Safety
Administration (NHTSA), in the interest of information exchange.
The contents of this document do not have the force and effect of
law and are not meant to bind the public in any way. This document
is intended only to provide clarity to the public regarding existing
requirements under the law or agency policies.
The United States Government assumes no liability for its content
or use thereof. If trade or manufacturers’ names or products are
mentioned, it is because they are considered essential to the object
of the publication and should not be construed as an endorsement.
The United States Government does not endorse products or
manufacturers.
National EMS Education Standards 2021. Washington, DC:
National Highway Trafc Safety Administration.

Technical Report Documentation Page

2
Table of Contents
Executive Summary ................................................................................................................................................... 3
Introduction and the Evolution of EMS in the United States .................................................................................. 5
About the Revised EMS Education Standards ......................................................................................................... 15
Summary of Signicant Changes to the EMS Education Standards ...................................................................... 23
National EMS Education Standards .......................................................................................................................... 28
Preparatory ........................................................................................................................................................... 28
Anatomy and Physiology ....................................................................................................................................... 31
Medical Terminology .............................................................................................................................................. 31
Pathophysiology .................................................................................................................................................... 31
Life Span Development ......................................................................................................................................... 31
Public Health .......................................................................................................................................................... 32
Pharmacology ........................................................................................................................................................ 33
Airway Management, Respiration and Articial Ventilation ................................................................................... 35
Assessment ........................................................................................................................................................... 36
Medicine ................................................................................................................................................................. 38
Shock and Resuscitation ....................................................................................................................................... 45
Trauma .................................................................................................................................................................. 46
Special Patient Populations ................................................................................................................................... 50
EMS Operations ..................................................................................................................................................... 52
Clinical Behavior/Judgment ................................................................................................................................... 54
Educational Infrastructure ...................................................................................................................................... 56
Glossary ....................................................................................................................................................................... 59
References ................................................................................................................................................................... 62
Acknowledgements and Stakeholder Input .............................................................................................................. 63
Appendix A: Resources for EMS .............................................................................................................................. 65

3
Back to Table of Contents >
In 2009, the EMS community came together to create the
original National EMS Education Standards (the Standards).
This represented a major step toward realizing the vision put
forth in the 1996 EMS Agenda for the Future and was further
outlined in the EMS Education Agenda for the Future: A Systems
Approach four years later. This new version of the Standards
builds on the foundation created by those landmark documents
and other achievements of the last quarter-century, including
EMS Agenda 2050 and the National Scope of Practice Model.
The National EMS Education Standards outline the minimal
competencies for entry-level EMS clinicians to perform their
roles as outlined in the 2019 and 2021* updated National
EMS Scope of Practice Model. The Standards, while a
national effort, were intentionally created in a way that allows
for diverse implementation methods to meet local needs
and evolving educational practices. This less prescriptive
format of the Standards allows for ongoing revision of EMS
educational content consistent with scientic evidence,
educational practices, and community standards of care.
Noteworthy revisions found in the 2021 edition of the Standards
are based upon input and considerations obtained from
numerous sources. These include stakeholder and public
comments, national guidance documents (the original 2009
National EMS Education Standards, EMS Agenda 2050, and
the 2019 and 2021* updated National Scope of Practice Model),
the National Registry of EMT’s practice analysis, technological
advances, known and evolving best practices, and evidence-
based medicine.
The following areas within the Standards had notable revisions:
public health; pediatrics; geriatrics, behavioral/psychiatric; cultural
humility; EMS operations; pharmacology; and EMS safety,
wellness and resilience. Input was provided and every suggestion
or recommendation was considered. Revision and adjustments
were based on a team discussion, with expert consultation when
needed.
When applying the Standards to individual programs and
classes, EMS educators have the freedom to develop their own
curricula or use any of the wide variety of lesson plans and
instructional resources that are available. This ensures that
each program can specically address individual and community
needs.
The Standards are not intended to stand as a comprehensive
document guiding the entire development of EMS clinicians,
but rather one part of a comprehensive system. EMS education
programs will incorporate each element of the education system
proposed in the Education Agenda.
These elements include:
• National EMS Core Content
• National EMS Scope of Practice Model
• National EMS Education Standards
• National EMS Certication
• National EMS Program Accreditation
This integrated system approach to EMS education is essential
to achieving the goal of developing EMS clinicians across the
country who are competent in the appropriate knowledge, skills,
and abilities for their licensure level.
Executive Summary
* As a result of the 2020-21 public health emergency, several changes were made under the
urgent update process to the 2019 National EMS Scope of Practice Model which are reected in
these education standards.

4
Back to Table of Contents >
January 2019
Project Commencement
Stakeholder Comments
Public Comments
Technological Advances
Related Government Resource Documents
NREMT Practice Analysis
Evidence-Based Medicine
Known/Evolving Best Practices
March 2021
Project Completion
Inputs
Team
Evaluation &
Expert
Consensus
Revision/
Adjustment
Distributed to
Stakeholders &
Public for Additional
Comment and
Transparency
Revision Process

5
Back to Table of Contents >
Introduction and the Evolution of EMS in the United States
EMS has evolved and grown signicantly since the rst organized,
national effort to develop EMS systems began in the 1960s.
Compared to colleagues in health care and public safety,
EMS remains a young profession and continues to advance
as we further dene and enhance our structure, oversight and
organization.
As EMS system operations have developed, so has EMS
education. In the early 1970s, registered nurses and physicians
taught most EMS programs. Few student and instructor
resources related directly to prehospital emergency care. No
standards existed to dene what EMS clinicians should know
and what they should be able to do. By the early 2000s, most
of this original framework was being replaced, and national
education standards and a scope of practice were dened
for the rst time. Today, the profession has become more
sophisticated, and community expectations have increased.
With health care, technology and science evolving faster than
ever, it is also important to revisit these topics and update these
guidelines more frequently.
EMS Agenda for the Future
In August 1996, the EMS Agenda for the Future (the Agenda)
was published. Developed with funding from the National
Highway Trafc Safety Administration and the Health Resources
and Services Administration, and led by the National Association
of EMS Physicians and the National Association of State EMS
Directors, the Agenda brought together stakeholders from
throughout EMS to create a unifying vision for emergency
medical services in the United States.
The Agenda was designed to guide government and private
organizations in EMS planning, development, and policymaking
at the national, state and local levels. It addressed 14 attributes of
EMS, including the EMS education system, and dened a vision for
EMS education “based on research” and “conducted by qualied
instructors” while employing “sound educational principles.”
EMS Education Conference
Soon after publication of the Agenda, representatives of
30 EMS-related organizations met at an EMS Education
Conference sponsored by NHTSA to identify the necessary
steps for implementing that vision.
The EMS Education Conference resulted in several
recommendations, including:
• The National EMS Education and Practice Blueprint (the
Blueprint) is a valuable component of the EMS education
system. A multidisciplinary panel, led by NHTSA, to
identify core educational content more explicitly for each
licensure level, should revise it.
• National EMS Education Standards are necessary
but need not include specic declarative material or
lesson plans. NHTSA should support and facilitate the
development of national EMS Education Standards.
• The Blueprint and national EMS Education Standards
should be revised periodically, with major revisions
occurring every 5 to 7 years, and minor updates made
every 2 to 3 years.

6
Back to Table of Contents >
EMS Education Agenda for the Future: A Systems Approach
Figure 1: Model EMS System
Periodic updates
of these three
documents
The Universe of EMS
Knowledge and Skills
Delineation of provider
practice levels
A single agency for each function – Standard exam, minimum competence, consumer protection
Delineation of provider
educational competencies
National EMS Certification National EMS Education Program Accreditation
National EMS Core Content
National EMS Scope of Practice
National EMS Education Standards
EMS Education Agenda for the Future
In 1998, NHTSA convened a group of educators who developed
a document titled EMS Education Agenda for the Future: A
Systems Approach (the Education Agenda). The EMS education
system envisioned in the EMS Agenda for the Future was
further dened and articulated in the Education Agenda (see
Figure 1). The Education Agenda’s authors also stated that,
to be most effective, each component in the EMS education
system should be structured, coordinated and interdependent.
National EMS Core Content
The National EMS Core Content was published in 2005. Core
Content denes the entire domain of out-of-hospital practice and
identies the universal body of knowledge and skills for EMS
clinicians who do not function as independent practitioners.
Funded by NHTSA and HRSA, this project was led by the
National Association of EMS Physicians and the American
College of Emergency Physicians.

7
Back to Table of Contents >
National EMS Scope of Practice
The National EMS Scope of Practice Model (the Scope of
Practice) is a consensus document that was published in
2007 and revised in 2019. This document denes four levels
of EMS licensure—emergency medical responder (EMR),
emergency medical technician (EMT), advanced emergency
medical technician (AEMT) and paramedic—and delineates the
practices and minimum competencies for each level. The Scope
of Practice does not have regulatory authority but provides
guidance to states. Adherence to the Scope of Practice would
increase uniformity in EMS practice throughout the U.S. and
facilitate reciprocity between states. Leadership for this project
was delegated to the National Association of State EMS Ofcials
and funded by NHTSA and HRSA.
The Scope of Practice further denes practice, suggests
minimum educational preparation, and designates appropriate
psychomotor skills at each level of licensure. Further, the
document describes each level of licensure as distinct
and distinguished by unique “skills, practice environment,
knowledge, qualications, services provided, risk, level of
supervisory responsibility, and amount of autonomy and
judgment/critical thinking/decision-making.”
National EMS Education Standards
The National EMS Education Standards replaced the NHTSA
National Standard Curricula at all licensure levels when rst
published in 2009. The Standards dene the competencies, clinical
behaviors, and judgments that should be met by entry-level EMS
clinicians to meet practice guidelines dened in the Scope of
Practice. Content and concepts dened in the National EMS Core
Content are also integrated within the Standards. Leadership for
this project was delegated to the RedFlash Group and National
Association of EMS Educators, and funded by NHTSA and HRSA.
With input from a large number of stakeholders, the team chose
not to update the separate Instructional Guidelines for each
clinician level originally published as companion documents to the
2009 Standards. Instead, the Instructional Guidelines have been
incorporated within the Standards, replacing the need for those
supplemental materials.
National EMS certication and national EMS education
program accreditation are the “bookends” that support the
other key elements of the system. The Education Agenda
recommended an individual should graduate from a nationally
accredited EMS education program to be eligible for National
EMS Certication. Essential components of the EMS
Agenda include a single National EMS Accreditation Agency
and a single National EMS Certication Agency to ensure
consistency and quality of EMS personnel.

8
Back to Table of Contents >
1970s
Robert Wood
Johnson Foundation
and Federal
Government
Funded regional EMS
systems and
demonstration projects
1950s
1960
1966
1966
American College
of Surgeons
Developed the first
training program for
ambulance attendants
President’s Committee
for Trac Safety
Recognized the need
to address emergency
care in reducing traffic
fatalities
National Academy of
Science published
Accidental Death and
Disability: The Neglected
Disease of Modern Society
Quantified the scope of
traffic-related death in the U.S.,
including the deficiencies in
prehospital care
Highway Safety
Act of 1966
Required each State
to adopt highway
safety programs to
comply with federal
standards, including
“emergency services”
1970s
1973
Crash Injury
Management for the
Law Enforcement Ocer
published by NHTSA
40-hour program that
evolved into First
Responder: NSC in 1979
Emergency Medical Services Act of
1973 enacted by Congress as Title XII
of the Public Health Services Act
Provided more than $300 million in
EMS funding over 8 years that allowed
for EMS system planning and
implementation, mandated states to
focus on EMS personnel and training,
and resulted in legislation and
regulation of EMS personnel levels
A Brief History of EMS Education in the United States
This timeline outlines key events in the development of EMS education in the United States
from the 1950s to the present.
1970
National Registry
of EMTs (NREMT)
Held first board
meeting, with goal to
provide uniform
standards for
credentialing
ambulance
attendants
1971
Emergency Care and
Transportation of the
Sick and Injured
published by the
American Academy of
Orthopedic Surgeons (AAOS)
One of the first EMS
textbooks

9
Back to Table of Contents >
1975
American Medical
Association (AMA)
Recognized EMT-Paramedic
as an allied health occupation
1977
1978
1985
1990
NHTSA hosts EMS
Training Workshop
Facilitated the development
of the 1990s curricula and
introduced the
assessment-based
education concept
National Standard
Curriculum (NSC) for
EMT-Paramedic
published by NHTSA
The original NSC
consisted of 15
instructional modules
The Essentials for
Paramedic Program
Accreditation
developed by AMA
Joint Review Committee
on Education Programs
for the EMT-Paramedic
(JRCEMT-P) adopted
The Essentials as the
standard for accreditation
First Responder,
EMT-Ambulance (EMT-A),
EMT-Intermediate (EMT-I),
and EMT-Paramedic
(EMT-P): NSC revised by
NHTSA
EMT-Paramedic reformatted
into six divisions
1994
1994
1995
First Responder:
NSC is revised
1992
EMS Education and
Practice Blueprint
Document served as a template
for the revised format of the
1990s NSC revision projects
1996
EMS Agenda for the
Future is created
Vision statement
created by NAEMSP
and NASEMSO for
integration of EMS
into the health care
system; funded by
NHTSA and HRSA
NREMT Practice Analysis
Determined frequency
and criticality of EMS
interventions, and
provided the foundation
for NREMT test blueprint
1998
PEW Health Professions
Commission Taskforce on Health
Care Workforce Regulation
published Strengthening Consumer
Protection: Priorities for Health
Care Workforce Regulation
Recommended a National Policy
Advisory Board to establish
standards and model legislative
language for uniform scope of
practice authority for health
professions
EMT-A revised and
renamed EMT-Basic
(EMT-B): NSC

10
Back to Table of Contents >
2019
2019
2021
National EMS Scope of Practice
Model revised and published
by NHTSA
The document adjusted for
changes in EMS delivery and
made revisions between the
first edition (2007) and current
times (2019)
EMS Agenda
2050
A people-centered,
community-driven
vision document
describing EMS
in the future
National EMS Education Standards
revised and published by NHTSA
National guideline to define the entry-level
education requirement for each level of EMS
clinician. The document contains revised education
standards reflecting the EMS Agenda 2050,
National EMS Scope of Practice Model (as
updated), advances in technology, evidence-based
medicine and evolving known best practices.
2006
2007
2009
2019
2019
Practice
Analysis
conducted
by NREMT
1998
EMT-P:
NSC revised
1999
EMT-I:
NSC revised
2000
Education Agenda for
the Future: A Systems
Approach published
by NHTSA
Funded by NHTSA and
HRSA, developed an
integrated system of EMS
regulation, certification
and licensure
2004
2004 National EMS Practice
Analysis published by NREMT
Updated the 1994 Practice
Analysis
2005
2005
The State of EMS Education EMS
Research Project: Characteristics of
EMS Educators by Ruple et al. in
Prehospital Emergency Care
Research related to identifying
characteristics of EMS instructors,
describing infrastructure available
to instructors, and identifying
instructor attributes necessary for
implementing education standards
National EMS Core Content
published by NHTSA and HRSA
Defines the EMS personnel
domain of knowledge described
in the National Scope of Practice,
and the universal knowledge and
skills of EMS personnel
EMS at the Crossroads Institute
of Medicine Report
Among other recommendations, required
national accreditation of paramedic
programs, adopting a common scope of
practice for EMS personnel with state
licensing reciprocity and national certification
as a prerequisite for state licensure and local
credentialing of EMS providers
National EMS Scope of Practice
Model published by NHTSA
National guidelines based
on the National EMS Core
Content that defined levels
of EMS licensure and their
scopes of practice
National EMS Education
Standards published by NHTSA
National set of guidelines that
defined the entry-level education
requirement for each level of
EMS clinician, and contained four
companion Instructional Guideline
documents to assist educators in
transitioning from the NSC

11
Back to Table of Contents >
1. Competency (yellow) – This statement
represents the minimum competency required for
entry-level clinicians at each licensure level.
2. Knowledge (blue) – This represents an
elaboration of the knowledge within each
competency (when appropriate) that entry-level
clinicians would need to master to achieve
competency.
3. Clinical Behaviors/Judgments (green) – This
section describes the clinical behaviors and
judgments essential for entry-level EMS clinicians
at each licensure level.
4. Educational Infrastructure (gray) – This section
describes the support standards necessary
for conducting EMS training programs at each
licensure level.
The National EMS Education Standards
The National EMS Education Standards is comprised of four components (Table 1):
Table 1: Format of National EMS Education Standards
EMR EMT AEMT Paramedic
Content Area
Competency Competency Competency Competency
Elaboration of
Knowledge
Additional knowledge
related to the competency
Additional knowledge
related to the competency
Additional knowledge
related to the competency
Additional knowledge
related to the competency
Clinical behaviors and
judgments
Clinical behaviors and
judgments
Clinical behaviors and
judgments
Clinical behaviors and
judgments
Educational Infrastructure Educational Infrastructure Educational Infrastructure Educational Infrastructure
Each statement in the
Standards presumes that
the expected knowledge
and behaviors are within
the scope of practice for
that EMS licensure level, as
dened by the National EMS
Scope of Practice Model.
Each competency applies to
patients of all ages.
The Standards also assume
there is a progression in
practice from the emergency
medical responder level to
the paramedic level. That is,
licensed personnel at each
level are responsible for all
knowledge, judgments, and
behaviors at their level and at
all levels preceding their level.
For example, a paramedic is
responsible for the knowledge
and tasks described for the
paramedic as well as the
other three levels of licensure.

12
Back to Table of Contents >
• Minimal Knowledge
• Minimal Range of Skills or Tasks
• Elemental Knowledge
• Increased Range of Skills or Tasks
• Deep Level of Knowledge
• Wide-Ranging, Broad and Extensive Skills or Tasks
• Lifelong Learning
P
s
y
c
h
o
-
S
o
c
i
a
l
E
x
t
e
n
s
i
v
e
H
i
s
t
o
r
y
E
p
i
d
e
m
i
o
l
o
g
y
E
x
t
e
n
s
i
v
e
A
n
a
t
o
m
y
I
n
-
d
e
p
t
h
D
i
f
f
e
r
e
n
t
i
a
l
D
i
a
g
n
o
s
i
s
A
l
t
e
r
n
a
t
i
v
e
C
o
n
d
i
t
i
o
n
s
E
x
t
e
n
s
i
v
e
P
a
t
h
o
p
h
y
s
i
o
l
o
g
y
P
r
e
d
i
c
t
i
o
n
s
o
f
M
a
n
a
g
e
m
e
n
t
A
s
p
e
c
t
s
G
a
t
h
e
r
i
n
g
ActionReassess
Recognize
Recognizes
Signs & Symptoms
Recall
Protocol | Theory
Management
Adjust Therapy
Based on
Recall
S
A
M
P
L
E
O
P
Q
R
S
T
L
i
m
i
t
e
d
P
a
t
h
o
p
h
y
s
i
o
l
o
g
y
L
i
m
i
t
e
d
D
i
f
f
e
r
e
n
t
i
a
l
D
i
a
g
n
o
s
i
s
L
i
m
i
t
e
d
A
u
t
o
n
o
m
y
ActionReassess
Recognize
Recognizes
Signs & Symptoms
S
A
M
P
L
E
O
P
Q
R
S
T
L
i
m
i
t
e
d
P
a
t
h
o
p
h
y
s
i
o
l
o
g
y
L
i
m
i
t
e
d
D
i
f
f
e
r
e
n
t
i
a
l
D
i
a
g
n
o
s
i
s
L
i
m
i
t
e
d
A
u
t
o
n
o
m
y
ActionReassess
Recognize
Recognizes
Signs & Symptoms
Recall
Protocol | Theory
Management
Adjust Therapy
Based on
Recall
Recall
Protocol | Theory
Management
Adjust Therapy
Based on
Recall
The descriptors used to illustrate the increasing complexity of
knowledge and behaviors through the progression of licensure
levels originate, in part, from the National EMS Scope of Practice
Model. These terms reect the differences in the breadth, depth
and actions required at each licensure level (Figures 2 and 2.1).
The depth of knowledge is the amount of detail a student needs
to know about a particular topic. The breadth of knowledge refers
to the number of topics or issues a student needs to learn in
a particular competency. For example, EMS instructors need
to ensure the emergency medical responder has a thorough
understanding of how to use the bag valve mask (BVM) safely
and effectively. The amount of detail the instructor provides about
how to use that BVM represents the depth of knowledge. Some
instructors might adjust their specic curriculum to provide slightly
more information about the BVM compared to other instructors,
but every graduating EMR will know how to use the device.
Simple Breadth/
Simple Depth
Foundational Breadth/
Fundamental Depth
Comprehensive Breadth/
Complex Depth
Figure 2: Depth/Breadth Terminology

13
Back to Table of Contents >
Because of the limited scope of practice for the EMR (fewer
tools in the airway box), the instructor may supplement BVM
education with a few additional concepts (breadth) surrounding
management of a patient’s airway, such as airway anatomy
and assessment. Supplementing the education with additional
concepts adds to the breadth of the material, with each concept
having its own level of detail (depth) limited only by the amount
of the time the instructor has to teach the material. As more
airway management tools are added to the toolbox for each
licensure level (EMT, AEMT, paramedic), the level of detail
will also change, and curriculum length will need to reect this
increased depth.
To describe the intended depth of knowledge of a particular
concept within a provider level, the revision team uses the
terms simple, fundamental and complex. These terms can
seem ambiguous and confusing when used in isolation (e.g.,
learning to correctly use a BVM is not a “simple” task). Instead,
the meaning of each term is relative to the other terms. For
example, knowledge that is categorized as “simple” is only
simple relative to another curriculum that provides more detail,
such as when comparing EMT to AEMT. EMT students may
need a greater level of airway anatomy detail because the
scope of practice is different. Scope of practice is even more
different for the AEMT and paramedic student, who will need
increasingly greater levels of airway anatomy detail (complex).
Course directors, instructors, medical directors and local
stakeholders can decide the precise level of detail based on
community and student needs rather than establishing a single
prescriptive curriculum for the entire nation.
Similarly, the intended breadth of knowledge surrounding a
concept is reected in the terms simple, foundational and
comprehensive. As curricula include an increasing level of
detail about the use of the BVM, airway assessment and airway
anatomy, the increasing size of the toolbox reected by the
increased scope of practice necessitates a broader list of related
subjects. For example, the addition of CPAP, nasopharyngeal
airway and oxygen delivery devices at the EMT level broadens
the curriculum for the EMT instructor. For instructors teaching
paramedic students, the increased scope of practice broadens
the knowledge base even more. Clearly, the use of CPAP
requires the EMT to have an increased depth and more complex
breadth of knowledge than the EMR, but not nearly as much as
the paramedic.
Expansive & Detailed
Lifelong Learning
Professional-Level
Knowledge
Technician-Level
Knowledge
Rudimentary
Integrates
Lifelong
Learning
Lifelong
Learning
Applies
Complex
Fundamental
Simple Foundational
Comprehensive
Uses
Simple
Breadth (How much material?)
Depth (How much detail?)
Figure 2.1: Depth/Breadth Terminology

14
Back to Table of Contents >
Emergency Medical
Responder
Emergency Medical
Technician
Advanced Emergency
Medical Technician
Paramedic
The emergency medical responder
(EMR) is an out-of-hospital practitioner
whose primary focus is to initiate
immediate lifesaving care to patients
while ensuring patient access to the
emergency medical services system.
EMRs possess the basic knowledge and
skills necessary to provide lifesaving
interventions while awaiting additional
EMS response and rely on an EMS or
public safety agency or larger scene
response that includes other higher-level
medical personnel. When practicing in
less populated areas, EMRs may have
a low call volume coupled with being the
only care personnel for prolonged periods
awaiting arrival of higher levels of care.
EMRs may assist, but should not be the
highest-level person caring for a patient
during ambulance transport. EMRs are
often the rst to arrive on scene. They
must quickly assess patient needs,
initiate treatment and request additional
resources.
An emergency medical technician (EMT)
is a health professional whose primary
focus is to respond to, assess and triage
emergent, urgent and non-urgent requests
for medical care, and to apply basic
knowledge and skills necessary to provide
patient care and medical transportation to/
from an emergency or health care facility.
Depending on a patient’s needs and/or
system resources, EMTs are sometimes
the highest level of care a patient will
receive during an ambulance transport.
EMTs often are paired with higher levels
of personnel as part of an ambulance
crew or other responding group. With
proper supervision, EMTs may serve as
a patient care team member in a hospital
or health care setting to the full extent of
their education, certication, licensure
and credentialing. In a community setting,
an EMT might visit patients at home and
make observations that are reported to
a higher-level authority to help manage
a patient’s care. When practicing in less
populated areas, EMTs may have low call
volume coupled with being the only care
personnel during prolonged transports.
EMTs may provide minimal supervision of
lower-level personnel. EMTs can be the
rst to arrive on scene; they are expected
to quickly assess patient conditions,
provide stabilizing measures and request
additional resources as needed.
The advanced emergency medical
technician (AEMT) is a health professional
whose primary focus is to respond to,
assess and triage non-urgent, urgent and
emergent requests for medical care; apply
basic and focused advanced knowledge
and skills necessary to provide patient
care and/or medical transportation; and
facilitate access to a higher level of care
when the needs of the patient exceed the
capability level of the AEMT. The additional
preparation beyond EMT prepares
an AEMT to improve patient care in
common emergency conditions for which
reasonably safe, targeted and evidence-
based interventions exist. Interventions
within the AEMT scope of practice may
carry more risk if not performed properly
than interventions authorized for the EMR/
EMT levels. With proper supervision,
AEMTs may serve as a patient care
team member in a hospital or health care
setting to the full extent of their education,
certication, licensure and credentialing. In
a community setting, an AEMT might visit
patients at home and make observations
that are reported to a higher-level authority
to help manage a patient’s care.
The paramedic is a health professional
whose primary focus is to respond to,
assess and triage emergent, urgent and
non-urgent requests for medical care;
apply basic and advanced knowledge
and skills necessary to determine
patient physiologic, psychological,
and psychosocial needs; administer
medications, interpret and use diagnostic
ndings to implement treatment; provide
complex patient care; and facilitate
referrals and/or access to a higher
level of care when the needs of the
patient exceed the capability level of the
paramedic. Paramedics often serve as a
patient care team member in a hospital
or other health care setting to the full
extent of their education, certication,
licensure and credentialing. Paramedics
may work in community settings where
they take on additional responsibilities
monitoring and evaluating the needs of
at-risk patients, as well as intervening
to mitigate conditions that could lead to
poor outcomes. Paramedics help educate
patients and the public in the prevention
and/or management of medical, health,
psychological and safety issues.
EMS Personnel Licensure Levels
These licensure levels are from the National EMS Scope of Practice Model. Each educational level assumes mastery of previously
stated competencies. Every clinician must demonstrate each competency within their scope of practice and for patients of all ages.

15
Back to Table of Contents >
About the Revised EMS Education Standards
2019 National EMS Scope of Practice Model Relationship
The recently released 2019 National EMS Scope of Practice
Model, funded by NHTSA and HRSA, assembled experts to
evaluate the scope of EMS practice for each of the four national
practitioner levels (EMR, EMT, AEMT and paramedic). The
2019 Scope of Practice Model is the launching pad and guide
for this revision of the National EMS Education Standards. The
Education Standards reect the 2019 and 2021 updated Scope
of Practice Model and ensure practitioners receive the education
and training they need to perform within their scopes and best
serve their patients and communities.
The revision of the National EMS Scope of Practice Model and
National EMS Education Standards are naturally interrelated,
as one informs the other. As such, the team brought together
to lead the revision of the National EMS Education Standards
was funded by NHTSA and HRSA, and included 10 proven and
renowned EMS educators. The National EMS Scope of Practice
Model, recommendations from EMS Agenda 2050, known best
practices, emerging technology, evidence-based medicine,
information from the National EMS Database and societal issues
were all considered. EMS stakeholder input and public comment
were solicited and received multiple times throughout the revision
process. The National Registry of EMTs also provided its Practice
Analysis ndings.
NREMT Practice Analysis
Several members of the EMS Education Standards Revision
Team were involved in the NREMT’s practice analysis working
group. This process has informed the team regarding the most
encountered EMS emergencies, according to the National EMS
Database, made possible by the National EMS Information
System (NEMSIS). In addition, the project revision team has
reached out to NREMT throughout the revision project to obtain
input and feedback. NREMT’s practice analysis has been one of
many critical resources consulted by the revision team.
Domains of EMS: Learning, Competency, Authorization and
Operational/Local Qualification
The 2019 National EMS Scope of Practice Model identies four
domains within the “Professional Scope of Practice” and provides
a structure for the differences between education, certication,
licensure and credentialing (see denitions below). The EMS
Education Standards Revision Team focused on education, or
the learning domain.
• Education, the learning domain – This domain includes
all didactic, psychomotor, and affective learning that an
EMS learner should be taught during an EMS course to
become an entry-level apprentice.
• Certication, the competency verication domain –
This domain includes all external evaluation and verication
processes that are led by an outside entity to ensure that a
learner has achieved competency to be safe and effective
when conducting duties as an entry-level EMS clinician. In
most states, National Registry certication is used to verify
competency.
• Licensure, the legal authorization domain – Licensure
refers to the legal authority, granted by a state, to an
individual to perform certain dened and restricted duties.
The clinical duties usually vary from one state to the
next. The term is not to be confused or referred to as
“certication.” As dened in the 2019 Scope of Practice

16
Back to Table of Contents >
Model, certication and licensure are independent yet
related processes. When state requirements are met, a
state license is issued along with the legal authority to
perform a role at the appropriate level of licensure.
• Credentialing, the operational/local qualication
domain – Credentialing is the responsibility of the
individual EMS organization and, in most cases, the
medical director. Being that a learner has been educated,
certied and licensed, the duty falls to the organization
and local community to ensure that the EMS clinician is
able to operate safely by following appropriate clinical and
operational guidelines and philosophies set forth by the
physician EMS medical director. Typically, this involves
orientation courses with an evaluation and structured
operational and clinical training programs. Credentialed
providers have been taught and assessed on skills and
actions that are beyond the entry-level education and
training of an EMS school. For instance, if allowed by the
state, ultrasound may be a role performed after proper
credentialing by the local EMS medical director and
jurisdiction, even though ultrasound is not included in the
National EMS Scope of Practice Model or the National
EMS Education Standards.
Because most EMS education programs teach students who will
not all practice in the same organization, communities or even
states, a one-size-ts-all education is not possible. The writing of
a detailed national curricula for each of the four levels would be
problematic. No educational institution can teach a learner every
possible clinical or operational guideline or associated philosophy,
nor can an educational entity train an individual about every clinical
device used by EMS services across the nation. As a result, the
credentialing process is a critical piece of preparing EMS clinicians
to practice in their respective organizations after the completion of
initial education and certication.
When a learner successfully concludes coursework and has
satised a program’s identied terminal requirements (Education
Domain), the apprentice can then sit for an evaluation that
provides verication of competency (Certication Domain). After
successfully navigating the Licensure Domain with a state, a
learner is deemed “entry-level.” Finally, the entry-level clinician
is ready for the Credentialing Domain of an employer, after
which the learner is “job-ready.” The term “entry-level” indicates
that a learner has completed the education, certication, and
licensure domains. “Job-ready” indicates that a learner has been
credentialed by an employer and the local medical director, and
is competent in the system’s operational and clinical guidelines,
policies and philosophies.
Common comments and recommendations that were received
by the revision team addressed content areas that clearly did
not apply to the entry-level education of an apprentice EMS
clinician. Many suggestions t within the credentialing domain
and are not appropriate for national adoption at this time. The
team worked hard to stay within the education domain for entry-
level EMS clinicians.
Education Standards vs. Instructional Guidelines
vs. Curriculum
The National EMS Education Standards outline the minimal
competencies for entry-level EMS clinicians to achieve within
the parameters outlined in the 2019 and 2021 updated Scope
of Practice Model. Education programs should contemplate the
Standards when developing curricula for national consistency.
The Standards’ format will allow diverse implementation methods
to meet local needs and evolving education practices. The less
prescriptive format of the Standards will also allow for ongoing
revision of content consistent with scientic evidence, advances in
technology, known “best practices” and community standards of
care.

17
Back to Table of Contents >
In general, the content of education standards can range from
largely non-prescriptive to detailed and very prescriptive.
Non-Prescriptive Education Standards:
• increase teacher autonomy
• increase instructional exibility
• increase responsiveness to student learning needs
• increase responsiveness to local needs and situations
• increase responsiveness to national trends
Prescriptive Education Standards:
• improve education consistency
• protect from societal harm that may result from low
education expectations and/or low-quality instruction
• have been labeled as “burdensome checklists” by some
educators and are problematic in medicine due to rapid
changes in technology, scientic evidence and best
practices
The National EMS Education Standards are not meant to stand
as a comprehensive document guiding all of the development of
EMS clinicians, but rather one part of a comprehensive system
(Figure 3). EMS education programs will incorporate each
element of the education system proposed in the Education
Agenda. These elements include:
• National EMS Core Content
• National EMS Scope of Practice
• National EMS Education Standards
• National EMS Certication
• National EMS Program Accreditation
This integrated system is essential to achieving the goals of
program efciency, consistency of instructional quality and
student competence as outlined in the Education Agenda.
While the Education Standards are developed at the national
level, each state retains the right to wholly adopt the Standards
or adopt and modify the Education Standards to t a state’s
unique needs. The National EMS Education Standards have
been created to provide states with a vetted, consensus-driven
foundation for EMS education. They also benet clinicians by
paving the way for national certication and easier transition
from one locality or state to another.
Individual EMS educators and local communities select or
create curricula based on a multitude of curriculum inuencers.
These inuencers can also be strong mechanisms for education
program accountability. Regional needs, accreditation standards
and state and local policies and regulations are a few examples.
Curricula design, implementation and adjustment are complex
processes. Specic curricular content, instructional strategies
and competency evaluation processes should be resolved at the
education program level through implementation and feedback.
Regulatory rules must be adhered to as well. Decisions on
curriculum implementation are based on local situations,
students’ needs and available resources. Figure 3 illustrates
numerous inputs and points for accountability when curricula
are designed, implemented and adjusted. Program directors,
faculty and education institutions would be wise to consider
each inuence.

18
Back to Table of Contents >
Where are the Instructional Guidelines?
The 2009 instructional guidelines (IGs) were originally designed
to help educators transition from the National Standard Curricula
developed in the 1990s to the 2009 Education Standards.
When the revision team met, a discussion ensued regarding
the ongoing usefulness of the IGs in their current form. It was
agreed that the addition of the existing four IGs (EMR, EMT,
AEMT and paramedic) to the Education Standards made the
documents too cumbersome to be easily useful.
It was also evident that, while much of the IGs remained
relevant, several sections had become outdated because
of changes in evidence-based medicine, best practices or
technology. Simultaneously, it was felt that it would be useful to
have a level of specicity within the Education Standards rather
than require educators to look in multiple places when seeking
guidance to create curricula.
The resulting document combined elements of the IGs with
the overarching principles of the Education Standards. A level
of knowledge depth and breadth is provided for each section
Figure 3: Influences on EMS Education Curriculum Development
Program
and
Course
Curriculum
I
m
p
l
e
m
e
n
t
a
t
i
o
n
F
e
e
d
b
a
c
k
Federal
• EMS Education Agenda for the Future:
A Systems Approach
• National EMS Core Content
• National EMS Scope of Practice Model
• National EMS Education Standards
• EMS Agenda 2050
• Stakeholder interests
Accrediting & Certifying
Organizations
• CAAHEP/CoAEMSP
1
• National Registry of EMTs
- Practice analysis
• Stakeholder interests
1 CAAHEP: Commission on Accreditation of Allied Health Education Programs, CoAEMSP: Committee
on Accreditation of Educational Programs for the Emergency Medical Services Professions
Advances in EMS
• Evidence-based medicine
• Technology
• Known and evolving best practices
Local
• Resources
• Student needs
• Community needs
• Medical direction
State & Regional
• State laws and regulations
• Regional requirements
• Stakeholder interests
• Local advisory committees
• Stakeholder interests
• Employers

19
Back to Table of Contents >
of the Standards. At a glance, trained educators will be able
to determine the extent of information to be provided to their
students. The result is an enriched blueprint of the education
and training of today’s EMS clinicians.
Beyond the Scope of the Project
There are four areas that were frequently brought up by
stakeholders but not part of the project. Specialty certication
education (critical care paramedic, community paramedic,
tactical medic); degree requirements at any clinician level;
nomenclature of the EMS profession and clinicians; and
continuing education requirements were beyond the scope
of this effort. Instead, the focus was to align the Education
Standards with the newly released 2019 Scope of Practice
Model.
Degree Requirements
The revision team heard numerous comments regarding
degree requirements. Clearly, some parties strongly desire
degree requirements for paramedics. Others strongly
oppose them. Currently, there is not an industry consensus
for degree requirements for EMS personnel. In many cases,
several signicant EMS stakeholders and the “larger” EMS
community take a more neutral position. Time will allow
for further discussion and debate on the topic. Early in the
process, the team was advised that the debate for or against
degrees was beyond the scope of the project as the 2021
National EMS Education Standards do not address degree
requirements.
The team also received recommendations for education
related to deeper clinical subject matter, leadership and
management, public health, education, social work,
research, and other areas related to EMS systems. One
national stakeholder called for courses in health systems
science and value-based care. Suggested courses included:
• Health care system structure and processes
• Health care policy, economics, and management
• Clinical informatics and health information technology
• Public/population health
• Health system improvement and person-centered care
• Structure and processes beyond EMS
• Health care reimbursement and nance
• Health care quality and safety
AEMT Accreditation
The 2019 National EMS Scope of Practice Model subject
matter expert panel recommended requiring AEMT program
accreditation by January 1, 2025. The panel deliberated and
came to a consensus on the matter with the involvement of 13
stakeholders and various independent contributors. Despite this
understanding in 2019, the topic continues to be passionately
debated. The Education Standards revision team supports this
recommendation. The revision team deliberated the topic and
concluded that accreditation is an original and identied goal of
the 2000 EMS Education Agenda. Through the use of collegial
evaluation practices and the identication of recognized routines
for establishing sound EMS education programs, program
accreditation is expected to promote clinical and educational
excellence by ensuring the availability of adequate resources
and services for educators and their students.
Portable Technologies
During the public comment periods, many participants identied
the need for education standards that covered new and

20
Back to Table of Contents >
emerging technologies. There were specic and repeated
recommendations for Point-of-Care Ultrasound (POCUS);
the 2019 Scope of Practice Model subject matter experts
directly addressed this skill and have determined that “portable
technology” (which includes POCUS) has been left to the
“credentialing” process of the EMS organization and medical
director. The Standards revision team believes that the ideal
time for use of these technologies is when a person has been
educated, deemed competent, licensed and credentialed with
knowledge and skill. The local EMS medical director should be
involved in the selection of technologies. Widespread education
based on specic technologies should be decided at the local
or state level. Only after national adoption and inclusion in
a practice analysis should technologies be included in the
National EMS Education Standards and National EMS Scope of
Practice Model.
Instructional Practices: Simulation, Shadowing &
Interprofessional Education
Because education standards are not intended to be a
curriculum, the instructional strategies of simulation, shadowing
and interprofessional education are addressed here but not
in the Standards themselves. The team does believe that an
education program should implement numerous instructional
techniques to accommodate the diversity of student learning
needs inside and outside the EMS classroom. Using numerous
instructional strategies will help reach every learner. A heavy
reliance on the traditional lecture is not ideal and is not
equitable, as some students learn better in different settings
and every student benets from experiencing other methods of
instruction. Three types of instructional practices were identied
by the public and various stakeholders: simulation, shadowing
and interprofessional education. The team believes that each
practice has merit and should be considered as an additional
instructional strategy.
Simulation
EMS simulation begins in the classroom with educators
creating realistic scenarios to train all levels of EMS
personnel. The practice of allowing students to memorize
and verbalize a check sheet is no longer acceptable and
should be changed. Simulation has proven to increase
critical thinking skills and reduce medical errors in our health
care system. Simple to complex simulation comes in many
forms, from table-top exercises and practicing intramuscular
injections on an orange to standardized live patients and
high-delity manikins. Cost will vary, but simulation does not
have to be expensive to be successful. Simulation in EMS
can achieve:
• The creation of a “safe-to-fail” environment in which
students can make mistakes without dire consequences
and learn from those mistakes
• Higher success rates on the NREMT psychomotor
exams
• Enhanced understanding and more robust
therapeutic communication
• Increased understanding and demonstration of
affective domain competencies
• Improvement in critical thinking skills of entry-level
personnel
• Improved safety, effectiveness and efciency of
services
• Substitution for infrequent or unattainable clinical
scenarios
Shadowing
Shadowing a practicing clinician offers students experiential,
hands-on learning opportunities, and many learners have a
special afnity for it. Shadowing affords a prospective EMS

21
Back to Table of Contents >
professional the chance to be immersed in the actual job
environment, making it possible to see an experienced
worker apply the skills and traits needed to accomplish
the work.
Interprofessional Education
Health care is best when delivered in a cooperative
team environment; collaboration can result in improved
communications, thus reducing medical errors, reducing
costs for patients and improving patient outcomes.
Interprofessional Education is a proven instructional method
that results in positive outcomes in clinical preparation,
health care profession education and public safety.
Interprofessional Education helps a learner realize how
EMS ts into the larger “continuum of care” and plays a
role in critical “systems of care.” Learning how patients
move through the health care system, from dispatch to
discharge to follow-up care, plays a critical role in patient
safety. Interaction with other health care providers and rst
responders during initial education will mutually enhance an
understanding of everyone’s roles in the system.
Out-of-hospital care is becoming more diverse and complex.
As a result, individual EMS instructors may not possess
the expertise or knowledge to teach all subjects within the
revised Standards. When this occurs, a subject matter
expert should be enlisted for the given topic. For instance,
the public health section has been expanded and it would
be a “best practice” to bring in a qualied content expert to
cover the topic. Many areas related to EMS operations would
also require a qualied content expert. Rescue operations
have become extremely broad and specialized. Bodies of
knowledge such as incident command, hazardous materials
and other unique topics require experience and specialized
knowledge for quality instruction. The instructor should have
a proper background, relevant knowledge and a degree
or a recognized and credible credential in the topic. It is
recommended that the EMS educator work with the subject
matter experts to ensure relevance of the content to the
practice of prehospital medicine.
Eminence of the Aective Domain
Competence in the affective domain of learning is critical to the
success of EMRs, EMTs, AEMTs and Paramedics. The National
EMS Education Standards focus on the knowledge and skills
that an entry-level practitioner needs to treat sick or injured
patients. The third dimension needed for any skilled EMS
clinician is related to values, attitude, professional behavior,
compassion and a willingness to serve. Values provide the
foundation for decisions, and attitudes reect values and
inuence interpersonal dynamics. Professional behavior is a key
component of medical practice, and compassion is a required
characteristic of medical professionals supporting clinical
knowledge and skill. A willingness to serve underlies all that a
health care provider does.
The importance of affective domain competence cannot be
overstated. Every EMS education program director and faculty
member should consider this aspect of medical practice.
Modeling and setting professional-level expectations for
affective domains are part of the educational duty of an educator
within career and technical school. From the very rst day of
class until course conclusion, the importance of teaching and
evaluating affective domain competency to ensure graduates
are fully prepared for professional practice should be identied
as a high priority and a universal goal.
Sequence of Instruction
The order of the National EMS Education Standards does not
imply any particular sequence of instruction. For example,
some topics, such as public health, could be taught early on or
later in a course, despite appearing early in these Standards.
Other topics, such as basic assessment skills, would likely

22
Back to Table of Contents >
come early in the clinician’s education and precede concepts
that build upon them. Curricular ow should be determined by
the education program director, with input from faculty, medical
direction and advisory committees.
Locally Identified Topics
The revision team recognized and heard numerous comments
regarding clinical content that is of great local need and yet may
not be essential as an item for the entire nation. As a result,
the team believed it would be best to include a statement that
some content should be locally determined and developed at
the simple depth, simple breadth level (or higher when desired).
This content should be identied, developed and implemented
using a program medical director, advisory boards, the larger
medical community or faculty judgement.
Implicit Expectations
For a given illness, condition, or traumatic injury, the implicit
expectation is that an educational program will include instruction
of the relevant anatomy, physiology, pathophysiology, assessments
and accepted treatments. The team determined that this
expectation is known by educators and repeating the statement in
each section of the document is not required or desired.
Additional Resources
It is impossible for EMS instructors to know everything about
the profession, and trying to stay up to date on the latest
evidence-based guidelines, best practices, industry standards
and research is a very difcult task. The resources found in
Appendix A are intended as tools for educators to use as
needed to remain current on changes in the eld.
Two critical sources that educators should consider referencing
as they create learning content are the National Model EMS
Clinical Guidelines, maintained by the National Association of
State EMS Ofcials (NASEMSO), and pre-hospital evidence-
based guidelines, many of which are produced through the
efforts of The Prehospital Guidelines Consortium, maintained
by the National Association of EMS Physicians (NAEMSP). The
guidance provided by these sources is a result of collaboration
among many national EMS stakeholders intent on promoting
consensus and evidence to inform a general standard of
prehospital care.

23
Back to Table of Contents >
Summary of Significant Changes to the EMS Education Standards
Behavioral/Psychiatric
Many, if not most EMS systems have seen a steady rise in
behavioral emergencies and patients experiencing acute and
chronic manifestations of psychiatric illnesses. Moreover, a
lack of available in-patient beds at mental health facilities has
resulted in EMS clinicians needing to manage these patients for
longer periods of time and over longer distances.
As a result, the behavioral/psychiatric section of the Education
Standards was revised to include more information regarding
acute behavioral crisis and mental health disorders. Greater
depth and breadth of knowledge were recommended for
areas involving potential safety hazards to patients and EMS
clinicians. Conversely, certain psychiatric disease and syndrome
areas were revised and simplied.
Cultural Humility
Throughout health care and related elds, there has been a
recognition of the importance of maintaining an awareness of the
assumptions and biases related to cultural issues and how they
may affect our patients, co-workers and students. Cultural humility
is a lifelong, ongoing process of self-reection and self-critique in
which one learns about others’ cultural identities and looks at how
one’s own background and social environment have shaped the
individual. Cultural humility in EMS should address:
• Education: Are our EMS educators diverse? Does
our student population reect the community? Are our
classrooms free of stereotypes? Do we understand our own
biases and the differences between all of our students?
• EMS workforce: Are we creating a diversied and
equitable workforce reective of our population?
Promoting cultural humility can help strengthen
relationships among staff, leadership, patients and
families and other health care personnel we interact with
on a daily basis.
• Patient care: Are we teaching cultural competency and
humility to our EMS students? After graduation, can our
students provide culturally competent, equitable and
medically appropriate prehospital care to each and every
patient no matter their background? Cultural humility leads
to higher-quality care and better communication and trust
between patients and clinicians.
EMS Operations
EMS operations, while extremely important, are determined by a
variety of factors, including the setting, the clinician’s role and the
EMS system design. Therefore, it is not possible to provide strict
and straightforward training requirements that would be appropriate
across these diverse settings. Next is a summary of the intent of
each section of the EMS operations education standards. EMS
educators and EMS institutions need to be able to work with local
and state agencies to determine the appropriate level of knowledge
that providers need to perform their duties safely and efciently.

24
Back to Table of Contents >
• Principles of Safely Operating EMS Emergency
Response Vehicles
The intent of this section is to give an overview of
emergency response to ensure the safety of EMS
personnel, patients and others during EMS response
vehicle operations. This does not prepare the entry-level
student to be an experienced and competent driver.
Appropriate driver training designed for the entry-level
provider must be completed as required by state and local
regulations and is not intended to be part of a requirement
to achieve national certication as an emergency medical
responder. Information related to the clinical management
of the patient during emergency response is found in the
clinical sections of the National EMS Education Standards
for each personnel level.
• Incident Management
Information related to the clinical management of the
patient within components of the Incident Management
System is found in the clinical sections of the National
EMS Education Standards for each licensure level. The
material presented in this section should be delivered by
an individual who has been trained and has the proper
credentials to educate students in these areas. The
material may be obtained in-person or through distance
learning as determined by state and local requirements.
• Mass Casualty Incidents
The intent of this section is to give an overview of
operating during a mass casualty incident when a multiple
casualty incident plan is activated. Information related to
the clinical management of the patients during a multiple
casualty incident is found in the clinical sections of the
National EMS Education Standards for each licensure
level. The depth and breadth of training that must be
achieved by clinicians at each level should be determined
by state and local requirements.
• Landing Zone Operations
The intent of this section is to give an overview of
operating safely in and around a landing zone during
air medical operations and transport. The safety
considerations of setting up and operating in a landing
zone should be taught by properly trained experts who
have the proper knowledge and experience in the area
of air medical transportation. The depth and breadth of
information that is needed by each level of clinician should
be determined by state and local regulations. Information
related to the clinical management of the patient being
cared for during air medical operations is found in the
clinical sections of the National EMS Education Standards
for each licensure level.
• Rescue Operations
The intent of this section is to provide an overview of
rescue operations including, but not limited to, vehicle
extrication, low/high angle, water, trench and conned
space to ensure the safety of EMS personnel and patients
during these events. This does not prepare the entry-level
student to become competent or qualied to work in these
rescue environments. Information related to the clinical
management of the patient being cared for during rescue
incidents is found in the clinical sections of the National
EMS Education Standards for each personnel level.
• Hazardous Materials
Information related to the clinical management of the
patient exposed to hazardous materials is found in the
clinical sections of the National EMS Education Standards
for each personnel level. This information may be done as
a corequisite or prerequisite, or as part of the entry-level
course as determined by state and local requirements.

25
Back to Table of Contents >
Training in this area should only be done by those properly
trained and credentialed to provide the required training.
Federal regulations require that, at a minimum, EMS
personnel must be trained at the Hazardous Materials
Awareness level. State and local regulations may have
additional requirements that are above and beyond federal
regulations. EMS educators should work in collaboration with
local re or emergency management authorities to determine
the proper training level required and assuring that properly
credentialed instructors are providing the training. The
information contained in the hazardous materials awareness
programs are above and beyond the scope of national EMS
programs for the entry-level provider.
• Mass Casualty Incidents Due to Active Threats
and Disaster
The intent of this section is to give an overview of
operating during a terrorist event or during a natural or
man-made disaster. Instruction in this area should be
done by properly trained and knowledgeable individuals in
this area. State and local regulations may have additional
requirements that are above and beyond federal
regulations. Information related to the clinical management
of patients exposed to a terrorist event or involved in a
disaster is found in the clinical sections of the National EMS
Education Standards for each personnel level.
Public Health
Since the release of the original National EMS Education
Standards in 2009, EMS has made substantial progress from
being viewed as simply a provider of medical transport to a true
out-of-hospital health care resource. The changes to the public
health section of the Standards reect this evolution in EMS.
Public health prevention and pandemic preparedness efforts are
essential functions in the future as EMS continues to be at the
crossroads between health care, public health and public safety.
The EMS clinician of the future will be expected to integrate into
pandemic plans, assist in vaccinations and act as the initial point
of entry into robust community health programs.
The new standards are intended to prepare the entry-level
provider to work alongside and collaboratively with specially
trained community paramedics, social workers, public health
organizations, health care entities, emergency management
agencies and non-governmental organizations in their day-
to-day duties, and lay the foundation for advancement into
specialized roles.
Pharmacology
An EMS culture of safety is a universal goal within the industry.
A key area for safety is the administration of medications in
the prehospital setting. The lack of desired pharmacology
competency among EMS program graduates was identied
by the EMS Scope of Practice subject matter experts, in EMS
evidenced-based literature and numerous other sources. When
it comes to pediatric populations, EMS for Children identied
a signicant need for additional training in this area and called
for specic teaching for pediatric dosing and troubleshooting
abnormal situations. As a result, the pharmacology section has
been expanded for EMR, EMT, AEMT and paramedics. It is not
enough to solely teach pharmacology in a traditional didactic
manner. This skill should include didactic, psychomotor and
affective instruction. There should be signicant opportunities
to practice the skill before leaving the education program.
Simulation and, ideally, actual patient encounters should
be offered to students. Emphasis and specic focus should be
given to psychomotor practice of adult, pediatric and geriatric
medication administration due to the complexity of drug dosing
and the chance of error.

26
Back to Table of Contents >
EMS Safety, Wellness and Resilience
Workforce safety and wellness has been expanded to reect
principles of stress management, responder mental health,
resilience and suicide prevention across all levels. With greater
number of responders reporting thoughts of suicide, and suicide
rates among rst responders signicantly exceeding those of
the general population, a foundational level of knowledge is
crucial to addressing this professional and occupational crisis.
An overall greater emphasis on mental health resources is also
recommended.
Standard safety precautions, use of personal protective
equipment, illness and injury prevention, and lifting and moving
patients continue to be emphasized at all levels of emergency
responders. Other areas that have been added include
crew resource management across all levels and disease
transmission in the EMT, AEMT and paramedic curricula.
Pediatric and Geriatric Content Competencies
Individual sections for pediatrics and geriatrics have been
removed, with education content addressing these special
populations now incorporated throughout the education
standards. This change is based on recommendations from
pediatric-focused stakeholders, scientic evidence and
consensus among clinical partners.
Concepts related to geriatric and pediatric patients deserve
equitable attention and should be taught repeatedly throughout
every section of a course resulting in an earlier assimilation
of the content. Pediatric stakeholders reported that anxiety,
unfamiliarity with pediatric patients and equipment, and
discomfort on the part of rescuers calls for aggressive remedies.
These ndings may be associated with the low frequency and
high acuity of pediatric encounters.
The need for better EMS assessment, diagnosis, treatment,
safe medication administration, airway management and
appropriate pain management has been identied. In every
aspect of education, troubleshooting and critical thinking are
required when clinical situations are confusing or problematic.
As students acquire knowledge, skills and abilities, opportunities
to compare and contrast pediatric, adult and geriatric
populations will enhance and deepen learning.
During each section of the Standards, relevant pediatric and
geriatric content should be discussed in detail as they aren’t
covered in a separate section. Incorporation of this special
population information into the general content should improve
the comfort level of students by making the care of these
patients part of everyday operations.
EMS education should include knowledge from the cradle to
the grave. Pediatric and geriatric topics should no longer be
minimized, in comparison to “adult” topics, or relegated to an
isolated component of an EMS course, which can create a
perception that the content is somehow less important.
EMS education and care should be family-centered. Family-
centered care is a clinical methodology for the planning,
delivery and evaluation of health care which is established in
an afrming partnership that collaboratively involves patients,
families and the health care providers. Family-centered care
represents a signicant transition away from paternalistic
medicine to that which is founded on pillars of respect,
collaboration, information sharing and shared decision-making.
While family-centered care is often taught as an area of focus
for children with special needs, it should be integrated into
the care of all patients. In the case of children with special
health care needs, the family’s knowledge of a child’s condition
can be immensely valuable. Yet, even among children with

27
Back to Table of Contents >
simple, acute medical emergencies, families and children
often experience high levels of stress. Family-centered care
seeks to help patients and families retain a sense of control.
This includes providing opportunities for family members to
be present during medical transport and invasive procedures.
The approach recognizes that each family is unique, integral
and essential for health care safety and quality. The values of
collaboration, responsiveness and united decision-making are at
the forefront of treatment. The beliefs, desires, and values from
cultural backgrounds of the family and patient are considered
and respected. Health care workers communicate with complete
information and in an unbiased and respectful manner. When
choices are made, decision-making involves all parties as
coequal parts and decision-makers are known and informed,
and health care clinicians listen to and honor patient and family
choices. When family-centered care is optimal, there is high-
quality care with safety, and family and patient satisfaction are
achieved.
The reader will nd phrases such as “include age-related
variations in pediatric and geriatric patients” and “include
psychosocial aspects of age-related assessment and
treatment modications for the major or common diseases
and/or emergencies associated with pediatric and geriatric
patients.” These phrases are intended to remind and direct EMS
educators to elevate the importance of geriatric and pediatric
education within each section.

28
Back to Table of Contents >
EMR EMT AEMT Paramedic
Preparatory
Uses knowledge of the EMS
system, safety/well-being of
the EMR, medical/legal issues
and ethical issues at the scene
of an emergency while awaiting
a higher level of care.
Applies knowledge of the EMS
system, safety/well-being of
the EMT, medical/legal and
ethical issues to the provision
of emergency care.
Applies knowledge of the EMS
system, safety/well-being of
the AEMT, medical/legal and
ethical issues to the provision
of emergency care.
Integrates knowledge of EMS
systems, the safety/well-being
of the paramedic, and medical/
legal and ethical issues intended
to improve the health of EMS
personnel, patients and the
community.
EMS Systems
• EMS systems (S,S)
• Roles, responsibilities and
professionalism of EMS
personnel (S,S)
• Quality improvement vs. quality
assurance (S,S)
• Role of medical oversight (S,S)
• Culture of safety / patient safety
(S,S)
• Continuum of care (S,S)
• EMS systems (S,F)
• Roles, responsibilities and
professionalism of EMS
personnel (F,F)
• Quality improvement vs. quality
assurance (S,F)
• Role of medical oversight (S,S)
• Culture of safety / patient safety
(S,F)
• Continuum of care (S,F)
• History of EMS (S,F)
• Systems of care, e.g., Stroke,
STEMI, Trauma, Pediatrics
(S,F)
• MIH/CP and other EMS-related
specialty roles (S,S)
• EMS systems (S,F)
• Roles, responsibilities and
professionalism of EMS
personnel (F,F)
• Quality improvement vs. quality
assurance (F,F)
• Role of medical oversight (F,F)
• Culture of safety / patient
safety (F,F)
• Continuum of care (F,F)
• History of EMS (S,F)
• Systems of care, e.g., Stroke,
STEMI, Trauma, Pediatrics
(F,F)
• MIH/CP and other EMS-related
specialty roles (F,F)
• EMS systems (C,C)
• Roles, responsibilities, and
professionalism of EMS
personnel (C,C)
• Quality improvement vs. quality
assurance (C,C)
• Role of medical oversight (C,C)
• Culture or safety / patient
safety (C,C)
• Continuum of care (F,F)
• History of EMS (F,F)
• Systems of care, e.g., Stroke,
STEMI, Trauma, Pediatrics
(C,C)
• MIH/CP and other EMS-related
specialty roles (F,F)
National EMS Education Standards
Preparatory
LEGEND
The rst letter refers to Breadth, which can be:
• Simple (S)
• Foundational (F)
• Comprehensive (C)
The second letter refers to Depth, which can be:
• Simple (S)
• Fundamental (F)
• Complex (C)
For more information refer to Fig. 2 and Fig. 2.1 (Depth/Breadth
Terminology) on p.11-12.

29
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Workforce
Safety and
Wellness
• Standard safety precautions
(S,S)
• Personal protective equipment
(S,S)
• Lifting and moving patients
(S,S)
• Crew resource management
(S,S)
• Stress management (F,F)
• Prevention of work-related
injuries and illnesses (F,F)
• Responder mental health,
resilience and suicide
prevention (F,F)
• Wellness principles (F,F)
• Disease transmission (S,S)
• Standard safety precautions
(F,F)
• Personal protective equipment
(F,F)
• Lifting and moving patients (F,F)
• Crew resource management
(F,F)
• Stress management (F,F)
• Prevention of work-related
injuries and illnesses (F,F)
• Responder mental health,
resilience and suicide
prevention (F,F)
• Wellness principles (F,F)
• Disease transmission (F,F)
• Standard safety precautions
(F,F)
• Personal protective equipment
(F,F)
• Lifting and moving patients (F,F)
• Crew resource management
(F,F)
• Stress management (F,F)
• Prevention of work-related
injuries and illnesses (F,F)
• Responder mental health,
resilience and suicide
prevention (F,F)
• Wellness principles (F,F)
• Disease transmission (F,F)
• Standard safety precautions
(C,C)
• Personal protective equipment
(C,C)
• Lifting and moving patients (C,C)
• Crew resource management
(F,F)
• Stress management (C,C)
• Prevention of work-related
injuries and illnesses (C,C)
• Responder mental health,
resilience and suicide prevention
(C,C)
• Wellness principles (C,C)
• Disease transmission (C,C)
Research
• Impact of research on EMR
care (S,S)
• Data collection (S,S)
• Impact of research on EMT care
(S,S)
• Data collection (S,S)
• Evidence-based decision
making (S,S)
• Impact of research on AEMT
care (S,S)
• Data collection (S,S)
• Evidence-based decision
making (S,S)
• Impact of research on
Paramedic care (S,S)
• Data collection (S,S)
• Evidence-based decision making
(S,S)
• Research principles to interpret
literature and advocate
evidence-based practice (F,F)
Documentation
• Recording patient ndings (S,S) • Recording patient ndings (S,S)
• Principles of medical
documentation and report writing
(F,F)
• Supporting medical necessity (S,S)
• Recording patient ndings (S,S)
• Principles of medical
documentation and report writing
(C,F)
• Supporting medical necessity (S,S)
• Recording patient ndings (S,S)
• Principles of medical documentation
and report writing (C,C)
• Supporting medical necessity (S,S)
EMS System
Communication
• Call for resources (S,S)
• Transfer care of the patient
(S,S)
• Interact within the team
structure (S,S)
• EMS communication system
(S,S)
• Communication with other
health care professionals to
include cohesive and organized
patient handoff (S,S)
• Team communication and
dynamics (S,S)
• Telemetric monitoring devices
and transmission of clinical
data, including video data (S,S)
• EMS communication system
(F,F)
• Communication with other
health care professionals to
include cohesive and organized
patient handoff (F,F)
• Team communication and
dynamics (F,F)
• Telemetric monitoring devices
and transmission of clinical
data, including video data (S,S)
• EMS communication system
(C,C)
• Communication with other health
care professionals to include
cohesive and organized patient
handoff (C,C)
• Team communication and
dynamics (C,C)
• Telemetric monitoring devices
and transmission of clinical data,
including video data (S,S)
Preparatory

30
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Therapeutic
Communication
• Health care literacy (S,S)
• Interviewing techniques (S,S)
• Verbal defusing strategies (S,S)
• Managing communication
challenges (S,S)
• Family centered care (S,S)
• Health care literacy (S,S)
• Interviewing techniques (F,F)
• Verbal defusing strategies (F,F)
• Managing communication
challenges (F,F)
• Family centered care (F,F)
• Adjusting communication
strategies for age, stage of
development, patients with
special needs (S,S)
• Non-discriminatory
communication that addresses
inherent or unconscious bias, is
culturally aware and sensitive,
and intended to improve patient
outcome (S,S)
• Health care literacy (F,F)
• Interviewing techniques (F,F)
• Verbal defusing strategies (F,F)
• Managing communication
challenges (F,F)
• Family centered care (F,F)
• Adjusting communication
strategies for age, stage of
development, patients with
special needs (S,S)
• Non-discriminatory
communication that addresses
inherent or unconscious bias, is
culturally aware and sensitive,
and intended to improve patient
outcome (S,S)
• Health care literacy (C,C)
• Interviewing techniques
(C,C)
• Verbal defusing strategies
(F,F)
• Managing communication
challenges (C,C)
• Family centered care (F,F)
• Adjusting communication
strategies for age, stage of
development, patients with
special needs (C,C)
• Non-discriminatory
communication that
addresses inherent or
unconscious bias, is culturally
aware and sensitive, and
intended to improve patient
outcome (C,C)
Medical/Legal
and Ethics
• Consent/refusal of care (S,S)
• Condentiality (S,S)
• Advanced directives (S,S)
• Tort and criminal actions (S,S)
• Evidence preservation (S,S)
• Statutory responsibilities (S,S)
• Mandatory reporting (S,S)
• Ethical principles/moral
obligations (S,S)
• End-of-life issues (S,S)
• Consent/involuntary consent/
refusal of care (F,F)
• Condentiality (F,F)
• Advanced directives (F,F)
• Tort and criminal actions (F,F)
• Evidence preservation (F,F)
• Statutory responsibilities (F,F)
• Mandatory reporting (F,F)
• Ethical principles/moral
obligations (F,F)
• End-of-life issues (S,S)
• Patient rights/advocacy (S,S)
• Consent/involuntary consent/
refusal of care (F,F)
• Condentiality (F,F)
• Advanced directives (F,F)
• Tort and criminal actions (F,F)
• Evidence preservation (F,F)
• Statutory responsibilities (F,F)
• Mandatory reporting (F,F)
• Ethical principles/moral
obligations (F,F)
• End-of-life issues (S,S)
• Patient rights/advocacy (S,S)
• Consent/involuntary
consent/ refusal of care
(C,C)
• Condentiality (C,C)
• Advanced directives (C,C)
• Tort and criminal actions
(C,C)
• Evidence preservation (F,F)
• Statutory responsibilities
(C,C)
• Mandatory reporting (C,C)
• Ethical principles/moral
obligations (C,C)
• End-of-life issues (C,C)
• Health care regulation (C,C)
• Patient rights/advocacy
(C,C)
• Ethical tests and decision
making (C,C)
Preparatory

31
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Medical
Terminology
Uses medical and anatomical
terms.
Uses anatomical and medical
terms and abbreviations in
written and oral communication
with colleagues and other health
care professionals.
Same as EMT Level Integrates anatomical and
medical terminology and
abbreviations into written
and oral communication with
colleagues and other health care
professionals.
EMR EMT AEMT Paramedic
Pathophysiology
Uses knowledge of shock and
respiratory compromise to
respond to life threats.
Applies knowledge of the
pathophysiology of respiration
and perfusion to patient
assessment and management.
Applies knowledge of the
pathophysiology of respiration
and perfusion to patient
assessment and management.
Integrates knowledge of
pathophysiology of major human
systems.
EMR EMT AEMT Paramedic
Life Span
Development
Uses knowledge of age-related
differences to assess and care
for patients.
Applies knowledge of life
span development to patient
assessment and management.
Same as EMT Level Integrates knowledge of life span
development.
EMR EMT AEMT Paramedic
Anatomy and
Physiology
Uses knowledge of the anatomy
and function of the upper airway,
heart, vessels, blood, lungs,
skin, muscles and bones as the
foundation of emergency care.
Applies knowledge of the
anatomy and function of all
human systems to the practice of
EMS.
Integrates knowledge of the
anatomy and physiology of
the airway, respiratory and
circulatory systems to the
practice of EMS.
Integrates knowledge of the
anatomy and physiology of all
human systems

32
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Public
Health
Has an awareness of local
public health resources and
their role in public health.
Applies knowledge of the
principles of public health
epidemiology including public
health emergencies, public
health monitoring, health
promotion and illness and
injury prevention.
Same as EMT level Applies knowledge of
principles of public health and
epidemiology including public
health emergencies, health
promotion and illness and
injury prevention.
Public
Health
Overview
• EMS roles in public health
(S,S)
• Infection prevention and
control (S,S)
• Human trafcking (S,S)
• EMS roles in public health
(S,S)
• Infection prevention and
control (S,S)
• Human trafcking (S,S)
• EMS EHR reporting and data
collection (S,S)
• Governmental/
nongovernmental roles &
resources (S,S)
• Public health mission and
goals (S,S)
• Social, geographic, economic,
demographic determinants of
health (S,S)
• Patient and community
education (S,S)
• Injury prevention and wellness
(S,S)
• Unique pediatric, geriatric and
special populations public
health concerns (S,S)
• Screenings and vaccinations/
immunizations (S,S)
• EMS roles in public health
(S,S)
• Infection prevention and
control (S,S)
• Human trafcking (S,S)
• EMS EHR reporting and data
collection (S,S)
• Governmental/
nongovernmental roles &
resources (S,S)
• Public health mission and
goals (S,S)
• Social, geographic, economic,
demographic determinants of
health (S,S)
• Patient and community
education (S,S)
• Injury prevention and wellness
(S,S)
• Unique pediatric, geriatric and
special populations public
health concerns (S,S)
• Screenings and vaccinations/
immunizations (F,F)
• Impacts of political, social and
economic issues (F,F)
• Infectious disease (F,F)
• EMS roles in public health
(C,F)
• Infection prevention and
control (F,F)
• Human trafcking (S,S)
• EMS EHR reporting and data
collection (S,S)
• Governmental/
nongovernmental roles &
resources (S,S)
• Public health mission and
goals (S,S)
• Social, geographic, economic,
demographic determinants of
health (S,S)
• Patient and community
education (S,S)
• Injury prevention and wellness
(S,S)
• Unique pediatric, geriatric and
special populations public
health concerns (S,S)
• Screenings and vaccinations/
immunizations (C,F)
• Impacts of political, social and
economic issues (F,F)
• Infectious disease (C,F)
• Patient disposition, selecting
destination, ambulance
transport (C,F)
• Bioinformatics (C,F)
Public Health

33
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Pharmacology
Uses knowledge of the
medications that the EMR may
administer in an emergency.
Applies knowledge of the
medications the EMT may
administer to a patient during
an emergency and chronic or
maintenance medications the
patient may be taking.
Applies (to patient assessment
and management) knowledge
of the medications carried
by AEMTs that may be
administered to a patient
during an emergency and
chronic or maintenance
medications the patient may
be taking.
Integrates knowledge of
pharmacology to formulate
a treatment plan intended to
mitigate emergencies and
improve the overall health of
the patient.
Principles of
Pharmacology
• Medication safety (S,S)
• Kinds of medications used
during an emergency (S,S)
• Medication safety (F,F)
• Medication legislation (F,F)
• Naming (F,F)
• Classications (F,F)
• Storage and security (F,F)
• Medication interactions (S,S)
• Adverse drug reactions (S,S)
• Metabolism and excretion (F,F)
• Mechanism of action (F,F)
• Medication response
relationships (F,F)
• Medication safety (C,C)
• Medication legislation (C,C)
• Naming (C,C)
• Classications (C,C)
• Storage and security (C,C)
• Medication interactions (C,C)
• Adverse drug reactions (C,C)
• Pharmacokinetics (C,C)
• Pharmacodynamics (C,C)
• Schedules (C,C)
• Medication safety (C,C)
• Medication legislation (C,C)
• Naming (C,C)
• Classications (C,C)
• Storage and security (C,C)
• Medication interactions (C,C)
• Adverse drug reactions (C,C)
• Pharmacokinetics (C,C)
• Pharmacodynamics (C,C)
• Schedules (C,C)
Medication
Administration
• Use a Medication Cross Check
procedure (S,S)
• Use an autoinjector (S,S)
• Use a unit-dose, premeasured
intranasal device (S,S)
• Use of tools/resources to
facilitate safe administration of
weight-based dosing.
• Use a Medication Cross Check
procedure (F,F)
• Use an autoinjector (S,S)
• Use a unit-dose, premeasured
intranasal device (S,S)
• Administer medications to a
patient (F,F)
• Provide pain management,
including ethical and safety
considerations (F,F)
• Routes of administration (S,S)
• Use a Medication Cross Check
procedure (F,F)
• Use an autoinjector (S,S)
• Use a unit-dose, premeasured
intranasal device (S,S)
• Administer medications to a
patient (C,C)
• Provide pain management,
including ethical and safety
considerations (C,C)
• Routes of administration (C,C)
• Resources for safe
administration of weight-based
dosing (F,F)
• Use a Medication Cross
Check procedure (F,F)
• Use an autoinjector (S,S)
• Use a unit-dose, premeasured
intranasal device (S,S)
• Administer medications to a
patient (C,C)
• Provide pain management,
including ethical and safety
considerations (C,C)
• Routes of administration
(C,C)
• Resources for safe
administration of weight-
based dosing (F,F)
Pharmacology

34
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Acute
Medications
• Names (S,S)
• Effects (S,S)
• Indications (S,S)
• Contraindications (S,S)
• Side effects (S,S)
• Routes of administration (S,S)
• Dosages (S,S)
• Names (F,S)
• Effects (S,S)
• Indications (F,S)
• Contraindications (F,S)
• Side effects (F,S)
• Routes of administration (F,S)
• Dosages (F,S)
• Actions (F,S)
• Complications (F,S)
• Interactions (F,S)
• Names (C,C)
• Effects (C,C)
• Indications (C,C)
• Contraindications (C,C)
• Side effects (C,C)
• Routes of administration (C,C)
• Dosages (C,C)
• Actions (C,C)
• Complications (C,C)
• Interactions (C,C)
• Names (C,C)
• Effects (C,C)
• Indications (C,C)
• Contraindications (C,C)
• Side effects (C,C)
• Routes of administration (C,C)
• Dosages (C,C)
• Actions (C,C)
• Complications (C,C)
• Interactions (C,C)
Chronic or
Maintenance
Medications
No knowledge related to this
competency is applicable at
this level.
Specic medication classes to be
determined locally
• Class names (S,S)
• Class indications (S,S)
• Class complications (S,S)
• Class side effects (S,S)
• Polypharmacy (S,S)
Specic medication classes to be
determined locally
• Class names (S,S)
• Class indications (S,S)
• Class complications (S,S)
• Class side effects (S,S)
• Polypharmacy (S,S)
Specic medication classes
and examples to be determined
locally
• Class names (F,S)
• Class indications (F,S)
• Class complications (F,S)
• Class side effects (F,S)
• Polypharmacy (F,S)
Pharmacology

35
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Airway
Management,
Respiration
and
Ventilation
Applies knowledge of anatomy
and physiology to assure
a patent airway, adequate
mechanical ventilation and
respiration while awaiting
additional EMS response for
patients of all ages.
Applies knowledge of anatomy
and physiology to patient
assessment and management in
order to assure a patent airway,
adequate mechanical ventilation
and respiration for patients of
all ages.
Applies knowledge of upper
airway anatomy and physiology
to patient assessment and
management in order to assure
a patent airway, adequate
mechanical ventilation and
respiration for patients of all
ages.
Integrates knowledge of anatomy,
physiology and pathophysiology
into the assessment to develop
and implement a treatment plan
with the goal of assuring a patent
airway, adequate mechanical
ventilation and respiration for
patients of all ages.
Airway
Management
(Include age-
related variations
in pediatric and
geriatric patients)
• Airway anatomy (F,S)
• Airway assessment (F,S)
• Techniques of assuring a patent
airway (F,S)
• Airway anatomy (F,F)
• Airway assessment (F,F)
• Techniques of assuring a patent
airway (F,F)
• Airway anatomy (F,F)
• Airway assessment (F,F)
• Techniques of assuring a patent
airway (F,F)
• Airway anatomy (C,C)
• Airway assessment (C,C)
• Techniques of assuring a patent
airway (C,C)
Respiration
(Include age-
related variations
in pediatric and
geriatric patients)
• Anatomy of the respiratory
system (F,S)
• Physiology and pathophysiology
of respiration (F,S)
- Pulmonary ventilation
- Oxygenation
- Respiration
• External
• Internal
• Cellular
• Assessment and management
of adequate and inadequate
respiration (F,S)
• Supplemental oxygen therapy
(F,S)
• Anatomy of the respiratory
system (F,F)
• Physiology and pathophysiology
of respiration (F,C)
- Pulmonary ventilation
- Oxygenation
- Respiration
• External
• Internal
• Cellular
• Assessment and management
of adequate and inadequate
respiration (F,C)
• Supplemental oxygen therapy
(F,C)
• Anatomy of the respiratory
system (C,F)
• Physiology and pathophysiology
of respiration (F,C)
- Pulmonary ventilation
- Oxygenation
- Respiration
• External
• Internal
• Cellular
• Assessment and management
of adequate and inadequate
respiration (F,C)
• Supplemental oxygen therapy
(F,C)
• Anatomy of the respiratory
system (C,C)
• Physiology and pathophysiology
of respiration (C,C)
- Pulmonary ventilation
- Oxygenation
- Respiration
• External
• Internal
• Cellular
• Assessment and management
of adequate and inadequate
respiration (C,C)
• Supplemental oxygen therapy
(C,C)
Ventilation
(Include age-
related variations
in pediatric and
geriatric patients)
• Assessment and management
of adequate and inadequate
ventilation (F,S)
• Effect of ventilation on cardiac
output (F,S)
• Assessment and management
of adequate and inadequate
ventilation (F,F)
• Effect of ventilation on cardiac
output (F,F)
• Assessment and management
of adequate and inadequate
ventilation (C,F)
• Effect of ventilation on cardiac
output (C,F)
• Assessment and management
of adequate and inadequate
ventilation (C,C)
• Effect of ventilation on cardiac
output (C,C)
Airway Management, Respiration and Ventilation

36
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Assessment
Use scene information and
patient assessment ndings
to identify and manage
immediate life threats and
injuries within the scope of
practice of the EMR.
Applies scene information and
patient assessment ndings
(scene size up, primary and
secondary assessment, patient
history and reassessment) to
guide emergency management.
Same as EMT Level Integrate scene and patient
assessment ndings with
knowledge of epidemiology
and pathophysiology to
form a eld impression. This
includes developing a list of
differential diagnoses through
clinical reasoning to modify the
assessment and formulate a
treatment plan.
Scene
Assessment
• Scene safety/situational
awareness (C,C)
• Scene management (F,F)
• Impact of the environment on
patient care (F,F)
• Addressing hazards (F,F)
• Violence (F,F)
• Need for additional or
specialized resources (F,F)
• Standard precautions (F,F)
• Multiple patient situations (F,F)
• Scene safety/situational
awareness (C,C)
• Scene management (F,F)
• Impact of the environment on
patient care (F,F)
• Addressing hazards (F,F)
• Violence (F,F)
• Need for additional or
specialized resources (F,F)
• Standard precautions (F,F)
• Multiple patient situations (F,F)
• Scene safety/situational
awareness (C,C)
• Scene management (F,F)
• Impact of the environment on
patient care (F,F)
• Addressing hazards (F,F)
• Violence (F,F)
• Need for additional or
specialized resources (F,F)
• Standard precautions (F,F)
• Multiple patient situations (F,F)
• Scene safety/situational
awareness (C,C)
• Scene management (C,C)
• Impact of the environment on
patient care (C,C)
• Addressing hazards (C,C)
• Violence (C,C)
• Need for additional or
specialized resources (F,F)
• Standard precautions (F,F)
• Multiple patient situations (C,C)
Primary
Assessment
(Include
age-related
variations
in pediatric
and geriatric
patients)
• Primary assessment (S,S)
• Begin interventions needed to
preserve life (S,S)
• Primary assessment (F,S)
• Integration of treatment/
procedures needed to preserve
life (F,S)
• Primary assessment (F,F)
• Integration of treatment/
procedures needed to preserve
life (F,F)
• Primary assessment (C,C)
• Integration of treatment/
procedures needed to preserve
life (C,C)
Assessment

37
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
History Taking
(Include
age-related
variations
in pediatric
and geriatric
patients)
• Determining the chief
complaint (S,S)
• Mechanism of injury/
nature of illness (S,S)
• Associated signs and
symptoms (S,S)
• Investigation of the chief
complaint (F,F)
• Mechanism of injury/nature of
illness (F,F)
• Associated signs and
symptoms (F,F)
• Past medical history (F,F)
• Pertinent negatives (F,F)
• Investigation of the chief
complaint (F,F)
• Mechanism of injury/nature of
illness (F,F)
• Associated signs and
symptoms (F,F)
• Past medical history (F,F)
• Pertinent negatives (F,F)
• Investigation of the chief complaint
(C,C)
• Mechanism of injury/nature of illness
(C,C)
• Associated signs and symptoms
(C,C)
• Past medical history (C,C)
• Pertinent negatives (C,C)
• Interviewing techniques (C,C)
• Therapeutic communication and
adaptive interview techniques (C,C)
Secondary
Assessment
(Include
age-related
variations
in pediatric
and geriatric
patients)
• Assessment of vital
signs (S,S)
• Assessment of pain
(S,S)
• Performing a rapid full
body scan (S,S)
• Assessment of vital signs (F,F)
• Assessment of pain (F,F)
• Techniques of physical
examination (F,F)
- Respiratory system
including breath sound
quality
- Cardiovascular system
- Neurological system
- Musculoskeletal system
- Major anatomical regions
• Assessment of vital signs (C,F)
• Assessment of pain (C,F)
• Techniques of physical
examination (C,F)
- Respiratory system
including breath sound
quality
- Cardiovascular system
- Neurological system
- Musculoskeletal system
- Major anatomical regions
• Assessment of vital signs (C,C)
• Assessment of pain (C,C)
• Techniques of physical examination
(C,C)
- Respiratory system including
breath sound quality
- Cardiovascular system
- Neurological system
- Musculoskeletal system
- Major anatomical regions
Monitoring
Devices
No knowledge related
to this competency is
applicable at this level.
• Pulse oximetry (S,S)
• Non-invasive blood pressure
(S,S)
• Cardiac monitoring – 12
lead ECG acquisition and
transmission (S,S)
• Blood glucose determination
(S,S)
• Pulse oximetry (S,S)
• Non-invasive blood pressure
(S,S)
• Cardiac monitoring – 12
lead ECG acquisition and
transmission (S,S)
• Blood glucose determination
(S,S)
• End tidal CO
2
monitoring and
interpretation of waveform
capnography (S,S)
• Venous blood sampling (S,S)
• Pulse oximetry (S,S)
• Non-invasive blood pressure (S,S)
• Cardiac monitoring – 12 lead ECG
acquisition and transmission (F,F)
• Blood glucose determination (S,S)
• End tidal CO
2
monitoring and
interpretation of waveform
capnography (F,F)
• Venous blood sampling (S,S)
• 12-lead ECG interpretation (F,F)
• Blood chemistry analysis (F,F)
Reassessment
(Include age-
related variations
in pediatric and
geriatric patients)
• How and when to
reassess patients (S,S)
• How and when to reassess
patients (F,F)
• How and when to reassess
patients (F,F)
• How and when to reassess patients
(C,C)
Assessment

38
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Medicine
Recognizes and manages life
threats based on assessment
ndings of a patient with a
medical emergency while
awaiting additional emergency
response.
Applies knowledge to provide
basic emergency care and
transportation based on
assessment ndings for an
acutely ill patient.
Applies knowledge to
provide basic and selected
advanced emergency care
and transportation based on
assessment ndings for an
acutely ill patient.
Integrates assessment ndings
with principles of epidemiology
and pathophysiology to
formulate a eld impression
and implement a treatment/
disposition plan for a patient
with a medical complaint.
Medical Overview
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Assessment and management
of a medical complaint (S,S)
• Pathophysiology, assessment,
and management of a medical
complaints to include (S,F)
- Transport mode
- Destination decisions
• Pathophysiology, assessment,
and management of a medical
complaints to include (F,F)
- Transport mode
- Destination decisions
• Pathophysiology, assessment,
and management of a medical
complaints to include (C,C)
- Transport mode
- Destination decisions
Abdominal and
Gastrointestinal
Disorders
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Anatomy, presentations
and management of shock
associated with gastrointestinal
bleeding (S,S)
• Acute and chronic
gastrointestinal hemorrhage (F,F)
• Other gastrointestinal disorders
to be determined locally (S,S)
• Acute and chronic
gastrointestinal hemorrhage (F,F)
• Other gastrointestinal disorders
to be determined locally (S,S)
• Acute and chronic
gastrointestinal hemorrhage
(C,C)
• Bowel obstruction (C,C)
• Liver and biliary tract disorders
(F,F)
• Pancreatitis (S,S)
• Inammatory disorders (S,S)
• Peritonitis (S,S)
• Other gastrointestinal disorders
to be determined locally (S,S)
Medicine

39
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Cardiovascular
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Chest pain (S,S) • Acute coronary syndrome
(F,F)
• Hypertensive emergencies
(S,S)
• Aortic aneurysm/dissection
(F,F)
• Thromboembolism (F,F)
• Heart failure (F,F)
• Other cardiovascular disorders
to be determined locally (S,S)
• Acute coronary syndrome
(C,F)
• Hypertensive emergencies
(F,S)
• Aortic aneurysm/dissection
(F,F)
• Thromboembolism (F,F)
• Heart failure (F,F)
• Other cardiovascular disorders
to be determined locally (S,S)
• Acute coronary syndrome (C,C)
• Hypertensive emergencies (C,C)
• Aortic aneurysm/dissection (F,F)
• Thromboembolism (F,F)
• Heart failure (C,C)
• Non-traumatic cardiac
tamponade (C,C)
• Cardiogenic shock (C,C)
• Vascular disorders (C,C)
• Cardiac rhythms (C,C)
• Conditions that predispose
patients to cardiac rhythm
disturbances including WPW,
Brugada, long QT syndrome
and others (C,C)
• Infectious diseases of the
heart: endocarditis, myocarditis,
pericarditis (F,F)
• Congenital heart disease (F,F)
• Hypertrophic cardiomyopathy
(F,F)
• Other cardiovascular disorders
to be determined locally (S,S)
Disorders of the
Eyes, Ears, Nose,
and Throat
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Epistaxis (S,S) • Epistaxis (S,S)
• Other eye, ear, nose and
throat disorders to be
determined locally (S,S)
• Epistaxis (F,F)
• Post-surgical oropharyngeal
hemorrhage (F,F)
• Other eye, ear, nose and
throat disorders to be
determined locally (S,S)
• Epistaxis (F,F)
• Post-surgical oropharyngeal
hemorrhage (F,F)
• Common or major diseases of
the eyes, ears, nose and throat
(F,F)
• Other eye, ear, nose and throat
disorders to be determined
locally (S,S)
Medicine

40
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Endocrine Disorders
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or
common diseases
and/or emergencies
associated with
pediatric and geriatric
patients)
• Awareness that diabetic
emergencies cause altered
mental status (S,S)
• Diabetic emergencies (F,F)
• Other endocrine disorders to be
determined locally (S,S)
• Diabetic emergencies (C,F)
• Other endocrine disorders to be
determined locally (S,S)
• Diabetic emergencies (C,C)
• Chronic diabetes (C,C)
• Adrenal disease (S,S)
• Pituitary and thyroid disorders
(S,S)
• Inborn errors of metabolism
(S,S)
• Other endocrine disorders to
be determined locally (S,S)
Genitourinary/Renal
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or
common diseases
and/or emergencies
associated with
pediatric and geriatric
patients)
• Blood pressure assessment in
hemodialysis patients (S,S)
• Complications related to renal
dialysis (S,S)
• Complications related to urinary
catheter management (not
insertion) (S,S)
• Kidney stones (S,S)
• Sexual assault (Female and
Male) (F,F)
• Other GI/Renal to be
determined locally (S,S)
• Complications related to renal
dialysis (F,S)
• Complications related to urinary
catheter management (not
insertion) (S,S)
• Kidney stones (F,S)
• Sexual assault (Female and
Male) (F,F)
• Other GI/Renal to be
determined locally (S,S)
• Complications of dialysis (C,C)
• Complications related to urinary
catheter management (not
insertion) (S,S)
• Renal calculi (C,C)
• Sexual assault (Female and
Male) (C,C)
• Acute/chronic renal failure (C,C)
• Acid base disturbances (C,C)
• Fluid and electrolytes (C,C)
• Infection (F,F)
• Male genital tract conditions
(F,F)
• Other GI/Renal to be
determined locally (S,S)
Hematology
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or
common diseases
and/or emergencies
associated with
pediatric and geriatric
patients)
No knowledge related to this
competency is applicable at this
level.
• Sickle cell crisis (S,S)
• Clotting disorders (S,S)
• Other hematologic disorders to
be determined locally (S,S)
• Sickle cell crisis (F,F)
• Clotting disorders (S,S)
• Other hematologic disorders to
be determined locally (S,S)
• Sickle cell disease (C,C)
• Coagulopathies (F,F)
• Blood transfusion complications
(F,F)
• Hemostatic disorders (F,F)
• Red blood cell disorders (F,F)
• White blood cell disorders (F,F)
• Other hematologic disorders to
be determined locally (S,S)
Medicine

41
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Immunology
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Anaphylactic reactions (S,S) • Allergic and anaphylactic
reactions (F,F)
• Other immunological
disorders to be determined
locally (S,S)
• Allergic and anaphylactic
reactions (C,C)
• Systemic Inammatory
Response Syndrome (SIRS)
(C,C)
• Other immunological
disorders to be determined
locally (S,S)
• Allergic and anaphylactic
reactions (C,C)
• Systemic Inammatory
Response Syndrome (SIRS)
(C,C)
• Hypersensitivity (C,C)
• Anaphylactoid reactions (C,C)
• Collagen vascular disease
(F,F)
• Transplant-related problems
(F,F)
• Immunodeciency syndromes
(acquired or congenital) (F,F)
• Other immunological disorders
to be determined locally (S,S)
Infectious
Diseases
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Awareness of patient who
may have an infectious
disease (S,S)
• How to disinfect and
decontaminate equipment
after treating a patient (S,S)
• Assessment and
management of a patient
who may have an infectious
disease (S,S)
• How to decontaminate the
ambulance and equipment
after treating a patient (S,S)
• Sepsis and septic shock (S,S)
• Other infectious diseases to
be determined locally (S,S)
• Assessment and
management of a patient
who may have an infectious
disease (S,S)
• How to decontaminate the
ambulance and equipment
after treating a patient (S,S)
• Sepsis and septic shock (F,F)
• HIV (F,F)
• Hepatitis B (F,F)
• Antibiotic resistance (F,F)
• Current infectious diseases
prevalent in the community
(F,F)
• Vaccine-preventable diseases
(F,F)
• Other infectious diseases to
be determined locally (S,S)
• Assessment and management
of a patient who may have an
infectious disease (S,S)
• How to decontaminate the
ambulance and equipment
after treating a patient (S,S)
• Sepsis and septic shock (C,C)
• HIV-related disease (C,C)
• Hepatitis (C,C)
• Meningitis (C,C)
• Antibiotic resistance (F,F)
• Current infectious diseases
prevalent in the community
(F,F)
• Vaccine-preventable diseases
(C,C)
• Viral diseases: RSV, Herpes
zoster (F,F)
• Sexually transmitted infections
(F,F)
• Tetanus (S,S)
• Vector-borne diseases (S,S)
• Tuberculosis (S,S)
• Emerging infectious disease
(S,S)
• Other infectious diseases to be
determined locally (S,S)
Medicine

42
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Neurology
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Decreased level of
responsiveness (S,S)
• Seizure (S,S)
• Stroke (S,S)
• Decreased level of
responsiveness (S,S)
• Seizure (F,F)
• Stroke (F,F)
• Dementia vs. delirium (S,S)
• Alzheimer’s disease (S,S)
• Headache (F,F)
• Brief Resolved Unexplained
Event (BRUE) (F,F)
• Other neurological disorders
to be determined locally (S,S)
• Decreased level of
responsiveness (F,F)
• Seizure (C,F)
• Stroke (F,F)
• Dementia vs. delirium (S,S)
• Alzheimer’s disease (S,S)
• Headache (F,F)
• Brief Resolved Unexplained
Event (BRUE) (F,F)
• Parkinson’s disease (S,S)
• Other neurological disorders
to be determined locally (S,S)
• Decreased level of
responsiveness (C,C)
• Seizure (C,C)
• Stroke (C,C)
• Dementia vs. delirium (S,S)
• Alzheimer’s disease (S,S)
• Headache (C,C)
• Brief Resolved Unexplained
Event (BRUE) (F,F)
• Parkinson’s disease (S,S)
• Hydrocephalus – CSF
diversion devices or shunts
(F,F)
• Other neurological disorders
to be determined locally (S,S)
Non-Traumatic
Musculoskeletal
Disorders
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Non-traumatic fractures (S,S) • Non-traumatic fractures (F,F)
• Other non-traumatic
musculoskeletal disorders to
be determined locally (S,S)
• Non-traumatic fractures (F,F)
• Other non-traumatic
musculoskeletal disorders to
be determined locally (S,S)
• Non-traumatic fractures (F,F)
• Disorders of the spine (F,F)
• Joint abnormalities (F,F)
• Muscle abnormalities (F,F)
• Overuse syndromes (F,F)
• Rhabdomyolysis (F,F)
• Other non-traumatic
musculoskeletal disorders to
be determined locally (S,S)
Medicine
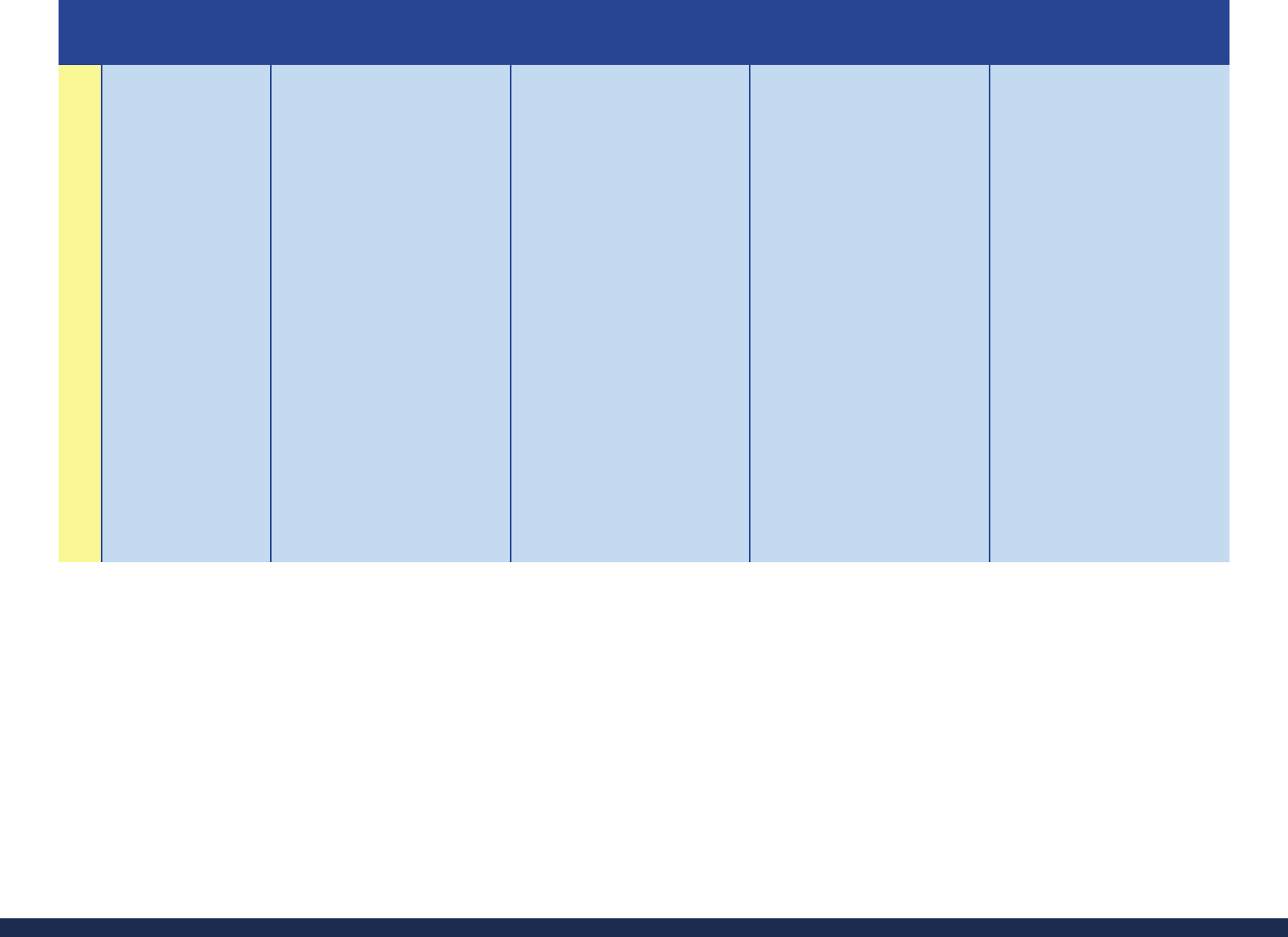
43
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Psychiatric or
Behavioral
Emergencies
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Recognition of behaviors
that pose a risk to the EMR,
patient or others
• Recognition of suicide risk
• Basic principles of the mental
health system (S,S)
• Patterns of violence, abuse
and neglect (S,S)
• Acute psychosis (F,F)
• Suicide ideation (F,F)
• Excited delirium (F,F)
• Anxiety (F,F)
• Depression (F,F)
• Medical fear (F,F)
• Substance use disorder (F,F)
• PTSD (F,F)
• Other psychiatric/behavioral
disorders to be determined
locally (S,S)
• Basic principles of the mental
health system (S,S)
• Patterns of violence, abuse
and neglect (F,F)
• Acute psychosis (F,F)
• Suicide ideation (C,C)
• Excited delirium (F,F)
• Anxiety (F,F)
• Depression (F,F)
• Medical fear (F,F)
• Substance use disorder/
addictive behavior (C,C)
• PTSD (F,F)
• Other psychiatric/behavioral
disorders to be determined
locally (S,S)
• Basic principles of the mental
health system (S,S)
• Patterns of violence, abuse
and neglect (C,C)
• Suicide ideation (C,C)
• Excited delirium (C,C)
• Anxiety (C,C)
• Depression (C,C)
• Medical fear (F,F)
• Substance use disorder/
addictive behavior (C,C)
• PTSD (C,C)
• Acute psychosis (C,C)
• Cognitive disorders (F,F)
• Thought disorders (F,F)
• Mood disorders (F,F)
• Neurotic disorders (F,F)
• Somatoform disorders (F,F)
• Factitious disorders (F,F)
• Personality disorders (F,F)
• Other psychiatric/behavior
disorders to be determined
locally (S,S)
Medicine

44
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Respiratory
(Include psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Respiratory
distress/failure/
arrest (F,F)
• Upper airway
obstruction (S,S)
• Lower airway
disease: Asthma,
bronchiolitis,
pneumonia,
chronic obstructive
pulmonary disease
(COPD) (S,S)
• Respiratory distress/failure/
arrest (F,F)
• Upper airway obstruction (F,F)
• Lower airway disease: Asthma,
bronchiolitis, pneumonia,
chronic obstructive pulmonary
disease (COPD) (F,F)
• Spontaneous pneumothorax
(F,F)
• Pulmonary edema (F,F)
• Other respiratory disorders to
be determined locally (S,S)
• Respiratory distress/failure/
arrest (F,F)
• Upper airway diseases: foreign
body, croup, epiglottitis (C,F)
• Lower airway disease: Asthma,
bronchiolitis, pneumonia,
chronic obstructive pulmonary
disease (COPD) (C,F)
• Spontaneous pneumothorax
(F,F)
• Pulmonary edema (C,F)
• Other respiratory disorders to
be determined locally (S,S)
• Respiratory distress/failure/arrest
(F,F)
• Upper airway diseases: foreign body,
croup, epiglottitis (C,C)
• Lower airway disease: Asthma,
bronchiolitis, pneumonia, chronic
obstructive pulmonary disease
(COPD), bronchopulmonary
dysplasia (C,C)
• Spontaneous pneumothorax (C,C)
• Pulmonary edema (C,C)
• Other respiratory disorders to be
determined locally (S,S)
Toxicology
(Include psychosocial
aspects of age-
related assessment
and treatment
modications for the
major or common
diseases and/
or emergencies
associated with
pediatric and
geriatric patients)
• Carbon monoxide
poisoning (S,S)
• Nerve agent
poisoning (S,S)
• Opioid toxicity (S,S)
• How and when to
contact a poison
control center (S,S)
• Carbon monoxide poisoning
(S,S)
• Nerve agent poisoning (S,S)
• Opioid toxicity (S,S)
• How and when to contact a
poison control center (S,S)
• Poisons (inhaled, ingested,
injected, absorbed) (F,F)
• Alcohol intoxication and
withdrawal (F,F)
• Other toxicological disorders to
be determined locally (S,S)
• Carbon monoxide poisoning
(S,S)
• Nerve agent poisoning (S,S)
• Opioid toxicity (F,F)
• How and when to contact a
poison control center (S,S)
• Poisons (inhaled, ingested,
injected, absorbed) (F,F)
• Alcohol intoxication and
withdrawal (F,F)
• Other toxicological disorders to
be determined locally (S,S)
• Carbon monoxide poisoning (C,C)
• Nerve agent poisoning (S,S)
• Opioid toxicity (F,F)
• How and when to contact a poison
control center (S,S)
• Poisons (inhaled, ingested, injected,
absorbed) (F,F)
• Alcohol intoxication and withdrawal
(C,C)
• Toxidromes (C,C)
- Cholinergic
- Anticholinergic
- Sympathomimetic
- Sedative/hypnotics
- Opioid
- Corrosive
- Knockdown
• Chronic or maintenance medications
(C,C)
• Drugs of abuse (C,C)
• Non-FDA approved medications and
supplements (C,C)
• Serotonin Syndrome (C,C)
• Malignant Hyperthermia (C,C)
• Other toxicological disorders to be
determined locally (S,S)
Medicine

45
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Shock and
Resuscitation
Uses assessment information
to recognize shock,
respiratory failure or arrest,
and cardiac arrest based on
assessment ndings and
manages the emergency
while awaiting additional
emergency response.
Applies knowledge of the
causes, pathophysiology
and management of shock,
respiratory failure or arrest,
cardiac failure or arrest,
termination of resuscitative
efforts and post resuscitation
management.
Applies knowledge to
provide basic and selected
advanced emergency care
and transportation based on
assessment ndings for a
patient in shock, respiratory
failure or arrest, cardiac
failure or arrest, termination
of resuscitative efforts
and post resuscitation
management.
Integrates knowledge of
causes and pathophysiology
into the management of
cardiac arrest and peri-arrest
states.
Shock
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications
for pediatric and
geriatric patients)
• Denition (S,S)
• Physiologic response (S,S)
• Essential components in
normal perfusion (F,S)
• Physiologic response (S,S)
• Types of shock (S,S)
• Treatment of shock (S,S)
• Essential components in
normal perfusion (F,F)
• Physiologic response (F,F)
• Types of shock (F,F)
• Treatment of shock,
hypoperfusion and
dehydration (C,C)
• Complications of shock (F,F)
• Circulatory assist devices
(F,F)
• Essential components in
normal perfusion (C,C)
• Physiologic response (C,C)
• Types of shock (C,C)
• Treatment of shock,
hypoperfusion and
dehydration (C,C)
• Complications of shock (C,C)
• Circulatory assist devices
(C,C)
Resuscitation
from Cardiac
Arrest
(Include
psychosocial
aspects of age-
related assessment
and treatment
modications
for pediatric and
geriatric patients)
• Ethical issues in resuscitation
(S,S)
• CPR physiology (S,S)
• Resuscitation system
components (S,S)
• Special arrest and peri-arrest
situations (S,S)
• Ethical issues in resuscitation
(C,C)
• CPR physiology (F,F)
• Resuscitation system
components (F,F)
• Special arrest and peri-arrest
situations (F,F)
• Postresuscitation support
(F,F)
• Termination of resuscitation
(F,F)
• Ethical issues in resuscitation
(C,C)
• CPR physiology (F,F)
• Resuscitation system
components (F,F)
• Special arrest and peri-arrest
situations (F,F)
• Postresuscitation support (C,C)
• Termination of resuscitation
(C,C)
• Ethical issues in resuscitation
(C,C)
• CPR physiology (C,C)
• Resuscitation system
components (C,C)
• Special arrest and peri-arrest
situations (C,C)
• Postresuscitation support (C,C)
• Termination of resuscitation
(C,C)
• Premorbid conditions (C,C)
Shock and Resuscitation

46
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Trauma
Uses knowledge to recognize
and manage life threats based
on assessment ndings for an
acutely injured patient while
awaiting additional emergency
medical response.
Applies knowledge to provide
basic emergency care and
transportation based on
assessment ndings for an
acutely injured patient.
Applies knowledge to
provide basic and selected
advanced emergency care
and transportation based on
assessment ndings for an
acutely injured patient.
Integrates assessment ndings
with principles of epidemiology
and pathophysiology to
formulate a eld impression
to implement a treatment/
disposition plan for an acutely
injured patient.
Trauma Overview
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or common
diseases and/or
emergencies associated
with pediatric and
geriatric patients)
No knowledge related to this
competency is applicable at
this level.
• Trauma scoring (F,F)
• Transport and destination
issues (F,F)
• Transport mode (F,F)
• Trauma scoring (F,F)
• Transport and destination
issues (F,F)
• Transport mode (F,F)
• Trauma scoring (C,C)
• Transport and destination
issues (C,C)
• Transport mode (F,F)
Abdominal and
Genitourinary Trauma
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or common
diseases and/or
emergencies associated
with pediatric and
geriatric patients)
• Blunt versus penetrating
mechanisms (S,S)
• Evisceration (S,S)
• Impaled object (S,S)
• Blunt versus penetrating
mechanisms (F,S)
• Evisceration (S,S)
• Impaled object (S,S)
• Solid and hollow organ injuries
(F,S)
• Injuries to the internal or
external genitalia (F,S)
• Blunt versus penetrating
mechanisms (F,F)
• Evisceration (S,S)
• Impaled object (S,S)
• Solid and hollow organ injuries
(F,F)
• Injuries to the internal or
external genitalia (F,F)
• Vascular injury (F,F)
• Retroperitoneal injuries (F,F)
• Blunt versus penetrating
mechanisms (F,F)
• Evisceration (S,S)
• Impaled object (S,S)
• Solid and hollow organ injuries
(F,F)
• Injuries to the internal or
external genitalia (F,F)
• Vascular injury (F,F)
• Retroperitoneal injuries (F,F)
Bleeding
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or common
diseases and/or
emergencies associated
with pediatric and
geriatric patients)
• Bleeding (S,S) • Bleeding (F,F) • Bleeding (F,F)
• Fluid resuscitation (C,C)
• Bleeding (F,F)
• Fluid resuscitation (C,C)
Trauma

47
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Chest Trauma
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or
common diseases
and/or emergencies
associated with
pediatric and geriatric
patients)
• Blunt versus penetrating
mechanisms (S,S)
• Open chest wound (S,S)
• Impaled object (S,S)
• Blunt versus penetrating
mechanisms (F,S)
• Open chest wound (S,S)
• Impaled object (S,S)
• Hemothorax (F,S)
• Pneumothorax (F,S)
• Cardiac tamponade (F,S)
• Rib fractures (F,S)
• Flail chest (F,S)
• Commotio cordis (F,S)
• Blunt versus penetrating
mechanisms (F,S)
• Open chest wound (S,S)
• Impaled object (S,S)
• Hemothorax (F,F)
• Pneumothorax (F,F)
• Cardiac tamponade (F,F)
• Rib fractures (F,F)
• Flail chest (F,F)
• Commotio cordis (F,S)
• Traumatic aortic disruption
(F,F)
• Pulmonary contusion (F,F)
• Blunt cardiac injury (F,F)
• Traumatic asphyxia (F,F)
• Blunt versus penetrating
mechanisms (F,S)
• Open chest wound (S,S)
• Impaled object (S,S)
• Hemothorax (C,C)
• Pneumothorax (C,C)
• Cardiac tamponade (C,C)
• Rib fractures (C,C)
• Flail chest (C,C)
• Commotio cordis (F,S)
• Traumatic aortic disruption
(C,C)
• Pulmonary contusion (C,C)
• Blunt cardiac injury (C,C)
• Traumatic asphyxia (C,C)
• Tracheobronchial disruption
(C,C)
• Diaphragmatic rupture (C,C)
Environmental
Emergencies
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or
common diseases
and/or emergencies
associated with
pediatric and geriatric
patients)
• Drowning (S,S)
• Temperature-related illness
(S,S)
• Bites and envenomations
(S,S)
• Lightning injury (S,S)
• Other environmental
emergencies to be determined
locally (S,S)
• Drowning (F,F)
• Temperature-related illness
(F,F)
• Bites and envenomations (F,F)
• Lightning injury (F,F)
• Other environmental
emergencies to be determined
locally (S,S)
• Drowning (F,F)
• Temperature-related illness
(F,F)
• Bites and envenomations (F,F)
• Lightning injury (F,F)
• Other environmental
emergencies to be determined
locally (S,S)
• Drowning (C,C)
• Temperature-related illness
(C,C)
• Bites and envenomations
(C,C)
• Lightning injury (C,C)
• Other environmental
emergencies to be determined
locally (S,S)
Trauma
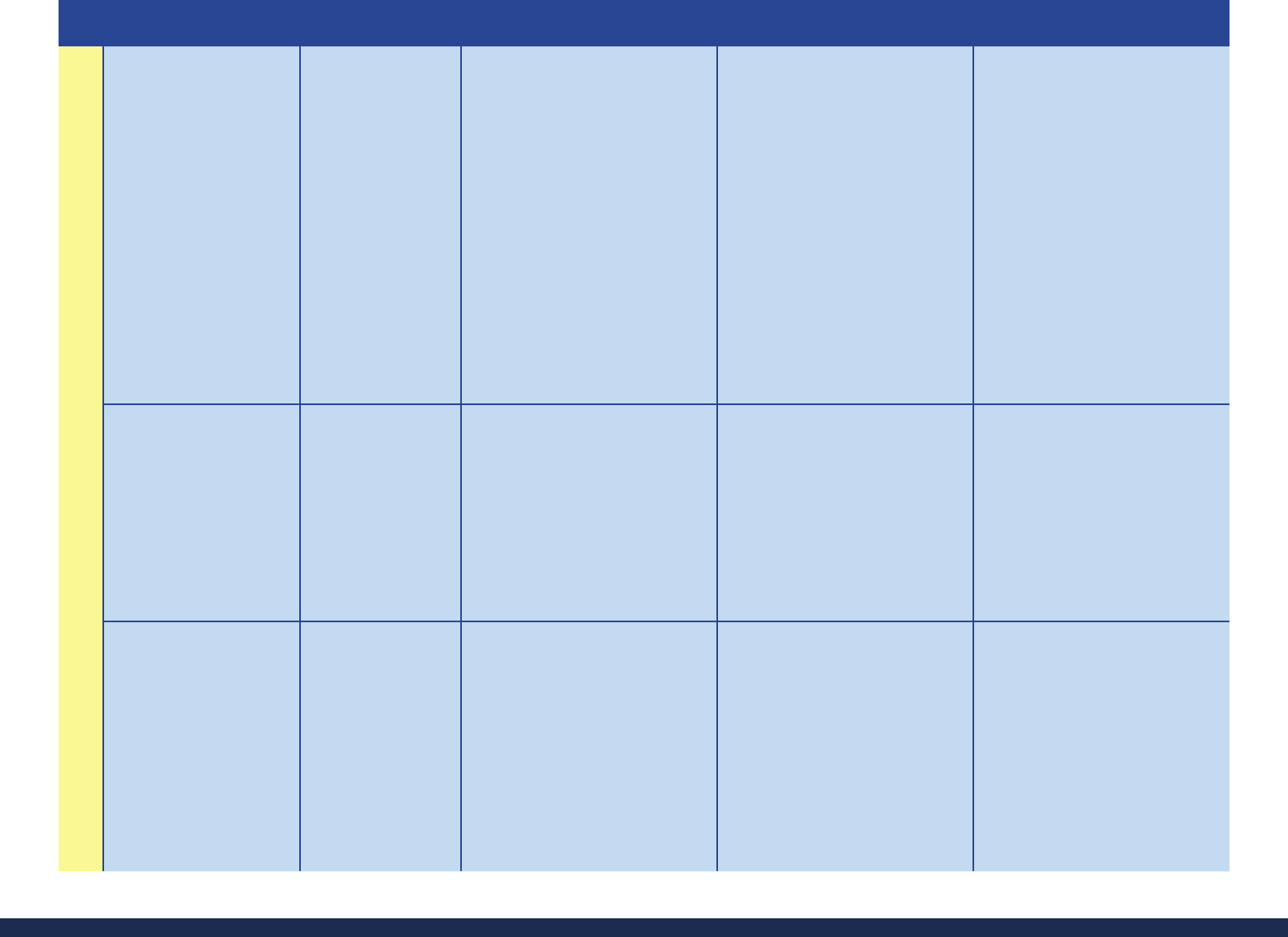
48
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Head, Facial, Neck,
and Spine Trauma
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or common
diseases and/or
emergencies associated
with pediatric and
geriatric patients)
• Life threats (S,S)
• Spine trauma (S,S)
• Life threats (S,S)
• Spine trauma (F,F)
• Penetrating neck trauma (F,F)
• Laryngotracheal injuries (F,F)
• Shaken Baby Syndrome (F,F)
• Facial fractures (S,S)
• Skull fractures (S,S)
• Foreign bodies in the eyes (S,S)
• Globe rupture (S,S)
• Dental trauma (S,S)
• Severe epistaxis (S,S)
• Life threats (S,S)
• Spine trauma (F,F)
• Penetrating neck trauma (F,F)
• Laryngotracheal injuries (C,F)
• Shaken Baby Syndrome (F,F)
• Facial fractures (C,F)
• Skull fractures (S,S)
• Foreign bodies in the eyes (S,S)
• Globe rupture (S,S)
• Dental trauma (S,S)
• Severe epistaxis (S,S)
• Life threats (S,S)
• Spine trauma (C,C)
• Penetrating neck trauma (C,C)
• Laryngotracheal injuries (C,C)
• Shaken Baby Syndrome (F,F)
• Facial fractures (C,F)
• Skull fractures (C,C)
• Foreign bodies in the eyes (S,S)
• Globe rupture (S,S)
• Dental trauma (S,S)
• Severe epistaxis (S,S)
• Unstable facial fractures (F,F)
• Orbital fractures (F,F)
• Perforated tympanic membrane
(F,F)
• Mandibular fractures (C,C)
Multi-System Trauma
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or common
diseases and/or
emergencies associated
with pediatric and
geriatric patients)
• Multi-system
trauma (S,S)
• Multi-system trauma (F,F)
• Blast injuries (F,F)
• Multi-system trauma (C,F)
• Blast injuries (F,F)
• Multi-system trauma (C,C)
• Blast injuries (C,C)
Nervous System
Trauma
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or common
diseases and/or
emergencies associated
with pediatric and
geriatric patients)
• Traumatic brain
injury (S,S)
• Traumatic brain injury (F,F)
• Spinal cord injury (F,F)
• Traumatic brain injury (C,F)
• Spinal cord injury (F,F)
• Traumatic brain injury (C,C)
• Spinal cord injury (C,C)
• Spinal shock (C,C)
• Cauda equina syndrome (F,F)
• Nerve root injury (F,F)
• Peripheral nerve injury (F,F)
Trauma

49
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Orthopedic Trauma
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or common
diseases and/or
emergencies associated
with pediatric and
geriatric patients)
• Open fractures (S,S)
• Closed fractures (S,S)
• Dislocations (S,S)
• Amputations (S,S)
• Open fractures (F,F)
• Closed fractures (F,F)
• Dislocations (F,F)
• Amputations/replantation (F,F)
• Upper and lower extremity
orthopedic trauma (F,F)
• Sprains/strains (F,F)
• Pelvic fractures (F,F)
• Open fractures (F,F)
• Closed fractures (F,F)
• Dislocations (F,F)
• Amputations/replantation
(C,F)
• Upper and lower extremity
orthopedic trauma (F,F)
• Sprains/strains (F,F)
• Pelvic fractures (C,F)
• Open fractures (C,C)
• Closed fractures (C,C)
• Dislocations (C,C)
• Amputations/replantation
(C,F)
• Upper and lower extremity
orthopedic trauma (C,C)
• Sprains/strains (F,F)
• Pelvic fractures (C,F)
• Pediatric fractures (F,F)
• Tendon laceration/
transection/ rupture (Achilles
and patellar) (F,F)
Soft Tissue Trauma
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or common
diseases and/or
emergencies associated
with pediatric and
geriatric patients)
• Wounds (avulsion, bite,
laceration, puncture, incision)
(S,S)
• Burns (electrical, chemical,
thermal) including inhalation
injury (S,S)
• Chemicals in the eye and on
the skin (S,S)
• Wounds (avulsion, bite,
laceration, puncture, incision)
(F,F)
• Burns (electrical, chemical,
thermal, radiation) including
inhalation injury (F,F)
• Chemicals in the eye and on
the skin (S,S)
• Crush/compartment syndrome
(S,S)
• High-pressure injection injury
(S,S)
• Wounds (avulsion, bite,
laceration, puncture, incision)
(F,F)
• Burns (electrical, chemical,
thermal, radiation) including
inhalation injury (F,F)
• Chemicals in the eye and on
the skin (S,S)
• Crush/compartment syndrome
(F,S)
• High-pressure injection injury
(S,S)
• Wounds (avulsion, bite,
laceration, puncture, incision)
(C,C)
• Burns (electrical, chemical,
thermal, radiation) including
inhalation injury (C,C)
• Chemicals in the eye and on
the skin (S,S)
• Crush/compartment syndrome
(C,C)
• High-pressure injection injury
(S,S)
Special Considerations
in Trauma
• Pregnant patient (S,S)
• Pediatric patient (S,S)
• Geriatric patient (S,S)
• Pregnant patient (F,F)
• Pediatric patient (F,F)
• Geriatric patient (F,F)
• Cognitively impaired patient
(F,F)
• Pregnant patient (C,F)
• Pediatric patient (C,F)
• Geriatric patient (C,F)
• Cognitively impaired patient
(C,F)
• Pregnant patient (C,C)
• Pediatric patient (C,C)
• Geriatric patient (C,C)
• Cognitively impaired patient
(C,C)
Trauma

50
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Special Patient
Populations
Recognizes and
manages life threats
based on simple
assessment ndings for
a patient with special
needs while awaiting
additional emergency
response.
Applies knowledge of
growth, development and
aging and assessment
ndings to provide basic
emergency care and
transportation for a patient
with special needs.
Applies knowledge of growth,
development and aging and
assessment ndings to provide
basic and selected advanced
emergency care and transportation
for a patient with special needs.
Integrates assessment ndings with
principles of pathophysiology and
knowledge of psychosocial needs
to formulate a eld impression and
implement a treatment/disposition plan
for patients with special needs.
Gynecology
(Include psychosocial
aspects of age-related
assessment and
treatment modications
for the major or
common diseases
and/or emergencies
associated with
pediatric and geriatric
patients)
• Shock associated with
vaginal bleeding (S,S)
• Vaginal bleeding (F,F)
• Infections (S,S)
• Other gynecological
disorders to be determined
locally (S,S)
• Vaginal bleeding (F,F)
• Infections (S,S)
• Other gynecological disorders to
be determined locally (S,S)
• Vaginal bleeding (C,C)
• Infections (F,F)
• Ovarian emergencies (F,F)
• Vaginal foreign body (F,F)
• Other gynecological disorders to be
determined locally (S,S)
Obstetrics
• Normal delivery (S,S)
• Vaginal bleeding in the
pregnant patient (S,S)
• Normal delivery (F,F)
• Vaginal bleeding in the
pregnant patient (S,S)
• Normal pregnancy (anatomy
and physiology) (F,F)
• Pathophysiology of
complications of pregnancy
(F,F)
• Assessment of the pregnant
patient (F,F)
• Abnormal delivery (nuchal
cord, prolapsed cord,
breech, shoulder dystocia,
prematurity, multiparity) (F,F)
• Third trimester and
antepartum bleeding
(placenta previa. placental
abruption) (F,F)
• Spontaneous abortion/
miscarriage (F,F)
• Ectopic pregnancy (F,F)
• Preeclampsia/eclampsia
(F,F)
• Postpartum complications
(S,S)
• Normal delivery (F,F)
• Vaginal bleeding in the pregnant
patient (S,S)
• Normal pregnancy (anatomy and
physiology) (F,F)
• Pathophysiology of complications
of pregnancy (F,F)
• Assessment of the pregnant patient
(F,F)
• Abnormal delivery (nuchal cord,
prolapsed cord, breech, shoulder
dystocia, prematurity, multiparity)
(F,F)
• Third trimester and antepartum
bleeding (placenta previa. placental
abruption) (F,F)
• Spontaneous abortion/miscarriage
(F,F)
• Ectopic pregnancy (F,F)
• Preeclampsia/eclampsia (F,F)
• Postpartum complications (C,C)
• Normal delivery (C,C)
• Vaginal bleeding in the pregnant patient (S,S)
• Normal pregnancy (anatomy and physiology)
(C,C)
• Pathophysiology of complications of
pregnancy (C,C)
• Assessment of the pregnant patient (C,C)
• Abnormal delivery (nuchal cord, prolapsed
cord, breech, shoulder dystocia, prematurity,
multiparity) (C,C)
• Third trimester and antepartum bleeding
(placenta previa. placental abruption) (F,F)
• Spontaneous abortion/miscarriage (C,C)
• Ectopic pregnancy (C,C)
• Preeclampsia/eclampsia (C,C)
• Postpartum complications (C,C)
• High-risk pregnancy (C,C)
• Complications of labor (fetal distress,
premature rupture of membranes, rupture of
uterus) (C,C)
• Hyperemesis gravidarum (S,S)
• Postpartum depression (S,S)
Special Patient Populations
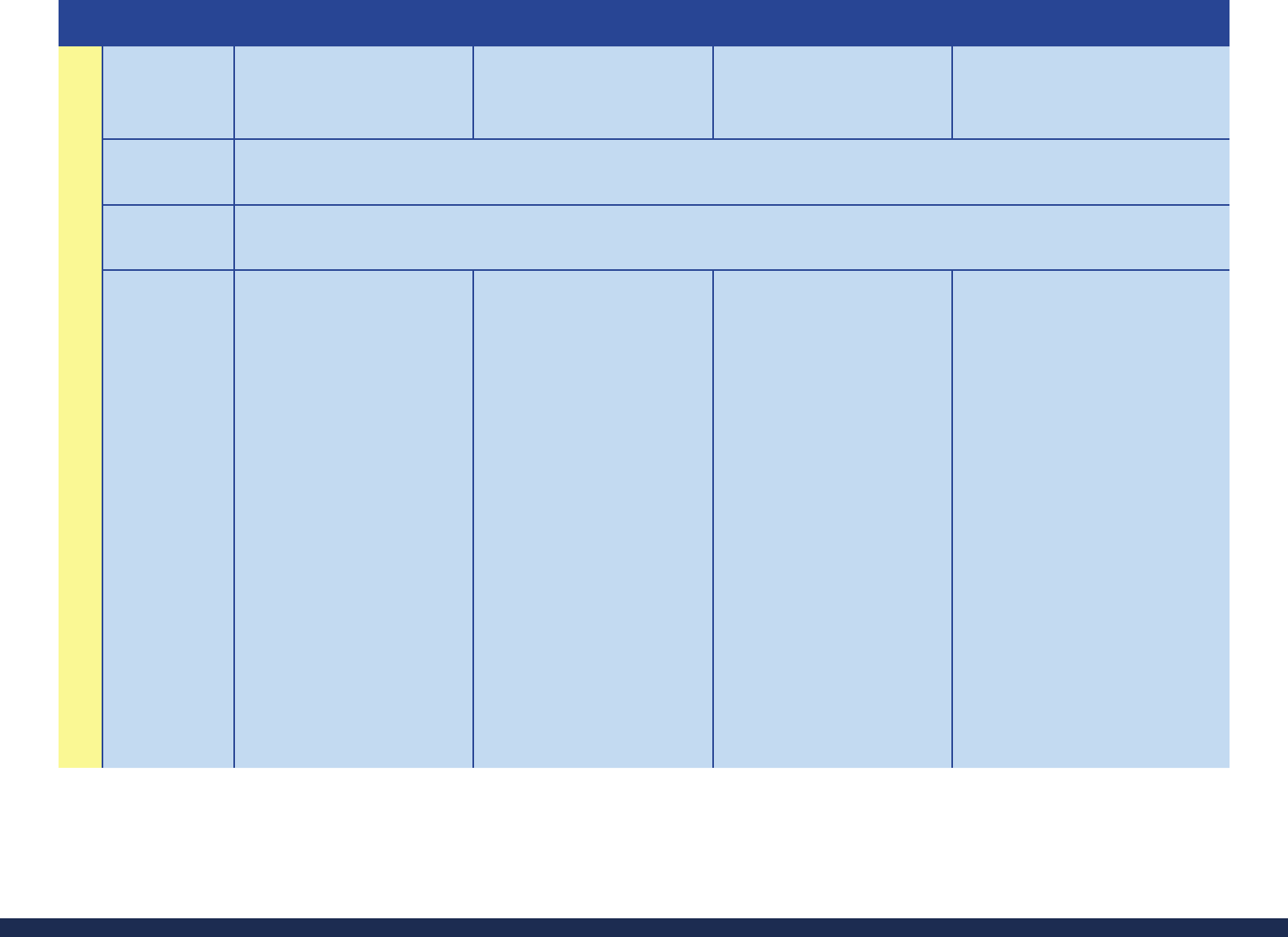
51
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Neonatal
Care
• Newborn stabilization (S,S)
• Neonatal resuscitation (S,S)
• Newborn stabilization (F,F)
• Neonatal resuscitation (F,F)
• Newborn stabilization (F,F)
• Neonatal resuscitation (F,F)
• Newborn stabilization (C,C)
• Neonatal resuscitation (C,C)
• Anatomy and physiology of neonatal
circulation (C,C)
Pediatrics
The Education Standards now integrate assessment, diagnostic, treatment and disposition modications for pediatric-specic diseases and
emergencies into each section of the document.
Geriatrics
The Education Standards now integrate assessment, diagnostic, treatment and disposition modications for geriatric-specic diseases and
emergencies into each section of the document
Patients
with Special
Challenges
• Recognizing and reporting
abuse and neglect (S,S)
• Recognizing and reporting
abuse and neglect (S,S)
• Abuse/Intimate partner
violence (S,S)
• Neglect (S,S)
• Child/dependent adult
maltreatment (S,S)
• Homelessness (S,S)
• Poverty (S,S)
• Bariatrics (S,S)
• Technology dependent (locally
determined) (S,S)
• Hospice/ terminally ill (S,S)
• Tracheostomy care/dysfunction
(S,S)
• Homecare (S,S)
• Sensory decit/loss (S,S)
• Developmental disability (S,S)
• Autism Spectrum Disorder
(S,S)
• Orthotics/prosthetics (S,S)
• Recognizing and reporting
abuse and neglect (S,S)
• Abuse/Intimate partner
violence (F,F)
• Neglect (F,F)
• Child/dependent adult
maltreatment (F,F)
• Homelessness (F,F)
• Poverty (F,F)
• Bariatrics (F,F)
• Technology dependent (locally
determined) (F,F)
• Hospice/ terminally ill (F,F)
• Tracheostomy care/dysfunction
(F,F)
• Homecare (F,F)
• Sensory decit/loss (F,F)
• Developmental disability (F,F)
• Autism Spectrum Disorder
(F,F)
• Orthotics/prosthetics (S,S)
• Recognizing and reporting abuse
and neglect (S,S)
• Abuse/Intimate partner violence
(C,C)
• Neglect (C,C)
• Child/dependent adult maltreatment
(C,C)
• Homelessness (F,F)
• Poverty (C,C)
• Bariatrics (C,C)
• Technology dependent (vagal nerve
stimulators, CSF diversion devices
or shunts, VAD, pacemakers, gastric
tubes and others to be locally
determined) (C,C)
• Hospice/ terminally ill (C,C)
• Tracheostomy care/dysfunction
(C,C)
• Homecare (F,F)
• Sensory decit/loss (F,F)
• Developmental disability (F,F)
• Autism Spectrum Disorder (F,F)
• Orthotics/prosthetics (S,S)
Special Patient Populations

52
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
EMS
Operations
Knowledge of operational roles
and responsibilities to ensure
patient, public and personnel
safety
Same as EMR Level Same as EMR Level Same as EMR Level
Emergency
Response
Vehicles
• Risks and responsibilities of
emergency response and radio
communications (S,S)
• Risks and responsibilities of
operating emergency vehicles
(S,S)
• Risks and responsibilities of
emergency response and radio
communications (S,S)
• Risks and responsibilities of
operating emergency vehicles
(S,S)
• Pediatric transport
considerations (F,F)
• Risks and responsibilities of
transport (F,F)
• Risks and responsibilities of
emergency response and radio
communications (S,S)
• Risks and responsibilities of
operating emergency vehicles
(S,S)
• Pediatric transport
considerations (F,F)
• Risks and responsibilities of
transport (F,F)
• Risks and responsibilities of
emergency response and radio
communications (S,S)
• Risks and responsibilities of operating
emergency vehicles (S,S)
• Pediatric transport considerations
(F,F)
• Risks and responsibilities of transport
(F,F)
Incident
Management
(The extent
of information
presented in this
area will vary at
the regional and
local level.)
• Establish and work within the
incident management system
(S,S)
• Establish and work within the
incident management system
(F,F)
• Understand the principles of Crew
Resource Management (F,F)
• Establish and work within the
incident management system
(F,F)
• Understand the principles of
Crew Resource Management
(F,F)
• Establish and work within the incident
management system (F,F)
• Understand the principles of Crew
Resource Management (F,F)
Multiple
Casualty
Incidents
(The extent
of information
presented in this
area will vary at
the regional and
local level.)
• Operational goals (F,F)
• Field triage (F,F)
• Operational goals (F,F)
• Field triage (F,F)
• Destination determination (F,F)
• Treatment principles (F,F)
• Operational goals (F,F)
• Field triage (F,F)
• Destination determination (F,F)
• Treatment principles (F,F)
• Operational goals (F,F)
• Field triage (F,F)
• Destination determination (F,F)
• Treatment principles (F,F)
Air Medical
(The extent
of information
presented in this
area will vary at
the regional and
local level.)
• Safe air medical operations (S,S)
• Criteria for utilizing air medical
response (S,S)
• Medical risks/needs/advantages
(S,S)
• Safe air medical operations (S,S)
• Criteria for utilizing air medical
response (S,S)
• Medical risks/needs/advantages
(F,F)
• Safe air medical operations (S,S)
• Criteria for utilizing air medical
response (S,S)
• Medical risks/needs/advantages
(F,F)
• Safe air medical operations (S,S)
• Criteria for utilizing air medical
response (S,S)
• Medical risks/needs/advantages (F,F)
EMS Operations

53
National EMS Education Standards
Back to Table of Contents >
EMR EMT AEMT Paramedic
Rescue Operations
(The extent of information
presented in this area will
vary at the regional and
local level.)
• Safety principles of rescue
operations (S,S)
• Safety principles of rescue
operations (S,S)
• Safety principles of rescue
operations (S,S)
• Safety principles of
rescue operations (S,S)
Hazardous Materials
(The extent of information
presented in this area will
vary at the regional and
local level.)
• Risks and responsibilities of
operating on the scene of a
hazardous materials incident
(S,S)
• Risks and responsibilities of
operating on the scene of a
hazardous materials incident
(S,S)
• Risks and responsibilities of
operating on the scene of a
hazardous materials incident
(S,S)
• Risks and
responsibilities of
operating on the
scene of a hazardous
materials incident (S,S)
Mass Casualty Incidents
due to Terrorism and
Disaster
(The extent of information
presented in this area will
vary at the regional and
local level.)
• Risks and responsibilities of
operating on the scene of a
natural or man-made disaster
(F,F)
• Risks and responsibilities of
operating on the scene of a
natural or man-made disaster
(F,F)
• Risks and responsibilities of
operating on the scene of a
natural or man-made disaster
(F,F)
• Risks and
responsibilities of
operating on the scene
of a natural or man-
made disaster (F,F)
EMS Operations

54
National EMS Education Standards
Back to Table of Contents >
Clinical Behavior/Judgment
EMR EMT AEMT Paramedic
Assessment
• Perform a simple assessment
to identify life threats, identify
injuries requiring spinal motion
restriction and conditions
requiring treatment within the
scope of practice of the EMR:
• Perform a basic history and
physical examination to identify
acute complaints and monitor
changes.
• Formulate a eld diagnosis
based upon an actual and/or
potential illness or injury.
• Perform a basic history and
physical examination to identify
acute complaints and monitor
changes.
• Formulate a eld diagnosis
based upon an actual and/or
potential illness or injury.
• Perform a comprehensive
history and physical
examination to identify factors
affecting the health and health
needs of a patient.
• Relate assessment ndings
to underlying pathological and
physiological changes in the
patient’s condition.
• Integrate and synthesize the
multiple determinants of health
and clinical care.
• Formulate a eld diagnosis
based on an analysis of
comprehensive assessment
ndings, anatomy, physiology,
pathophysiology and
epidemiology.
• Perform health screening and
referrals.
Therapeutic
Communication and
Cultural Humility
• Effectively communicates in a non-discriminatory manner that addresses inherent or unconscious bias, is culturally aware and sensitive,
and intended to improve patient outcome.
Psychomotor Skills
• Safely and effectively perform all psychomotor skills within the National EMS Scope of Practice Model AND state Scope of Practice at this level.

55
National EMS Education Standards
Back to Table of Contents >
Clinical Behavior/Judgment
EMR EMT AEMT Paramedic
Professionalism
Demonstrate professional affective domain behaviors including but not limited to:
• Integrity
• Empathy/compassion
• Self-motivation
• Appearance/personal hygiene
• Self-condence
• Communications
• Time management
• Teamwork/diplomacy
• Respect
• Patient advocacy
• Careful delivery of service
• Lifelong learning
Is a role model of exemplary
professional affective domain
behaviors including but not limited
to:
• Integrity
• Empathy/compassion
• Self-motivation
• Appearance/personal hygiene
• Self-condence
• Communications
• Time management
• Teamwork/diplomacy
• Respect
• Patient advocacy
• Careful delivery of service
• Lifelong learning
Decision Making
• Initiates simple interventions
based on assessment
ndings.
• Initiates interventions based on assessment ndings intended
to provide symptom relief (within the provider’s scope of
practice) while providing access to denitive care
• Evaluates the effectiveness of interventions and modies
treatment plan accordingly.
• Performs interventions as part
of a treatment plan intended
to provide symptom relief and
improve the overall health of the
patient.
• Evaluates the effectiveness
of interventions and modies
treatment plan accordingly.
• Evaluates decision making
strategy for cognitive errors to
enhance future critical thinking
skills (metacognition)
Record Keeping
• Report and document
assessment ndings and
interventions performed.
• Report and document assessment ndings, interventions performed, and clinical decision making
Team Dynamics
• Manage the scene until care
is transferred to an EMS
team member licensed at a
higher level arrives.
• The entry-level clinician serves as a team member, while gaining the experience necessary to
function as the team leader.
Safety
• Ensure the safety of the rescuer, other public safety personnel, civilians and the patient.

56
National EMS Education Standards
Back to Table of Contents >
Educational Infrastructure
EMR EMT AEMT
2
Paramedic
Educational
Facilities
• Facility sponsored or approved by sponsoring agency
• Sponsoring agency commitment to diversity, equity and inclusion
• ADA compliant facility
• Sufcient space for class size
• Controlled environment
Reference
Committee on
Accreditation
for EMS
Professions
(CoAEMSP)
Standards and
Guidelines
(www.coaemsp.
org)
1
Student Space
• Provide space sufcient for students to attend classroom sessions, take notes, and participate in classroom activities
• Provide space for students to participate in kinematic learning and practice activities
Instructional
Resources
• Provide basic instructional support material
• Provide audio, visual, and kinematic aids to support and supplement didactic instruction
Instructor
Preparation
Resources
• Provide space for instructor preparation
• Provide support equipment for instructor preparation
Storage Space
• Provide adequate and secure storage space for instructional materials
1
The National EMS Education Agenda for the Future: A Systems Approach (2000) calls for national accreditation of Paramedic programs. The Commission on Accreditation of Allied Health Education
Programs (CAAHEP) accredits programs upon the recommendation of the Committee on Accreditation of Educational Programs for the Emergency Medical Services Professions (CoAEMSP). CAAHEP
is the only national agency that offers Paramedic educational programmatic accreditation and is used or recognized by most states. Recognition of national accreditation remains the responsibility of
each state.
2
The 2019 and 2021 updated National Scope of Practice Model call for national accreditation of AEMT programs. The target for full implementation of AEMT program accreditation is January 1, 2025.
Until that date, AEMT programs should reference the existing infrastructure suggestions within this document. The Commission on Accreditation of Allied Health Education Programs (CAAHEP) accredits
programs upon the recommendation of the Committee on Accreditation of Educational Programs for the Emergency Medical Services Professions (CoAEMSP).CAAHEP is the only national agency that
offers EMS programmatic accreditation and is used or recognized by most states. Recognition of national accreditation remains the responsibility of each state.

57
National EMS Education Standards
Back to Table of Contents >
Educational Infrastructure
EMR EMT AEMT Paramedic
Sponsorship
Sponsoring organizations shall be one of the following:
• Accredited educational institution
• Public safety organization
• Accredited hospital, clinic or medical center, or
• Other state approved institution or organization
Reference
Committee on
Accreditation
for EMS
Professions
(CoAEMSP)
Standards and
Guidelines
(www.
coaemsp.org)
1
Programmatic
Approval
• Sponsoring organization shall have programmatic approval by authority having jurisdiction for program approval (state)
Faculty
Course primary instructors should:
• Be educated at a level higher than they are teaching; however, as a minimum, they must be educated at the level they are
teaching
• Have completed an approved instructor training program or equivalent
Medical Director
Oversight
• Provide medical oversight for all medical aspects of instruction
Hospital/Clinical
Experience
• None required at this level • The student must demonstrate
the ability to perform an adequate
assessment and implement an
adequate treatment plan.
- These can be performed in an
emergency department, ambulance,
clinic, nursing home, doctor’s ofce,
on a standardized patient or in an
alternative clinical environment when
clinical access is not available.
• The student must demonstrate
the ability to perform an adequate
assessment and implement an
adequate treatment plan.

58
National EMS Education Standards
Back to Table of Contents >
Educational Infrastructure
EMR EMT AEMT Paramedic
Field Experience
• None required at this level • The student should participate in and document
patient contacts in a eld experience in an
ambulance, mobile health care experience,
or simulated environment when ambulance
experience is not available as approved by the
medical director and program director. This may
occur in an ambulance, ambulance experience,
or simulated environment when ambulance
experiences are not available.
• The student must participate in and
document both patient contacts and team
leadership roles in a eld experience
approved by the medical director and
program director.
Reference
Committee on
Accreditation for
EMS Professions
(CoAEMSP)
Standards and
Guidelines (www.
coaemsp.org)
1
Course Length
• Instructors may use a variety of formats to
deliver content including but not limited to:
- Independent student preparation
- Synchronous or asynchronous
instruction
- Face-to-face instruction
- Pre- or co-requisites
• Course length should be based on
competency, not hours
- Consensus opinion is that students
should need a minimum of 48 didactic
and laboratory clock hours to cover the
material.
• Instructors may use a variety of formats to
deliver content including but not limited to:
- Independent student preparation
- Synchronous or asynchronous instruction
- Face-to-face instruction
- Pre- or co-requisites
• Course length should be based on
competency, not hours
- Consensus opinion is that students should
need a minimum of 150 clock hours including
the four integrated phases of education
(didactic, laboratory, clinical and eld) to cover
the material
• Instructors may use a variety of formats
to deliver content including but not
limited to:
- Independent student preparation
- Synchronous or asynchronous
instruction
- Face-to-face instruction
- Pre- or co-requisites
• Course length should be based on
competency, not hours
- Consensus opinion is that
students should need a minimum
of 200 clock hours beyond EMT
requirements including the four
integrated phases of education
(didactic, laboratory, clinical and
eld) to cover the material
Course Design
• Provide the following components of
instruction:
- Didactic instruction
- Skills laboratories
• Provide the following components of instruction:
- Didactic instruction
- Skills laboratories
- Hospital/clinical experience
- Field experience
Student
Assessment
• Perform knowledge, skill and professional behavior evaluation based on educational standards and program objectives
• Provide several methods of assessing achievement
• Provide assessment that measures, as a minimum, entry-level competency in all domains
Program
Evaluation
• Provide evaluation of program instructional effectiveness
• Provide evaluation of organizational and administrative effectiveness of program

59
Back to Table of Contents >
Academic institution – Body or establishment instituted for
an educational purpose that provides college credit or awards
degrees.
Accreditation – The granting of approval by an ofcial review
board after meeting specic requirements. Typical requisites may
cover areas such as program structure, processes, resources
and student evaluation. The review board is nongovernmental
and the review is collegial and based on self-assessment,
peer assessment and judgment. The purpose of accreditation
is student protection and public accountability. Additionally,
accreditation can provide consistent quality education evaluation
for a program’s continual improvement and provides for a more
consistent and uniform graduate competency.
Advanced-level care – Care that has greater potential benet
to the patient, but also greater potential risk to the patient if
improperly or inappropriately performed. It is more difcult to
attain and maintain competency in and requires signicant
background knowledge in basic and applied sciences. This level
of care includes invasive and pharmacological interventions.
Affective domain – Describes learning in terms of feelings/
emotions, attitudes and values. Additionally, the affective domain
covers many professional behaviors that are required by an
EMS clinician to perform his or her role as a health care provider.
(NAEMSE, 2020)
Asynchronous instruction/learning – An instructional method
that allows the learner to use a self-directed and self-paced
learning format to move through the content of the course. In this
type of instruction, learner-to-learner and learner-to-instructor
interactions are independent of time and place. Communications
and submission of work typically follow a schedule while learners
and instructors do not interact at the same time.
Certication – The issuing of a certicate by a private agency
based upon deemed competency established through standards
adopted by that agency and met by the individual.
Cognitive domain – Describes learning that takes place through
the process of thinking—it deals with facts and knowledge.
(NAEMSE, 2020)
Competency – Expected behavior or knowledge to be achieved
within a dened area of practice.
Credential – Generic term referring to all forms of professional
qualication.
Credentialing – The umbrella term that includes the concepts
of accreditation, licensure, registration and professional
certication. Credentialing can establish criteria for fairness,
quality, competence, and/or safety for professional services
provided by authorized individuals, for products or for educational
endeavors. Credentialing is the process by which an entity,
authorized and qualied to do so, grants formal recognition to
or records the recognition status of individuals, organizations,
institutions, programs, processes, services or products that meet
predetermined and standardized criteria. (NOCA, 2006)
Credentialing agency – An organization that certies an
institution’s or individual’s authority or claim of competence in a
course of study or completion of objectives.
Curriculum – A particular course of study, often in a specialized
eld. For EMS education, it has traditionally included instructional
techniques, detailed lesson plans with identied objectives and
Glossary

60
Back to Table of Contents >
numerous forms of learner evaluation. Curriculum is developed
and adopted at the education program based upon National EMS
Education Standards and state and local regulatory requirements.
The use of local advisory groups can help tailor education to a
local community’s needs.
Didactic – The instructional theory, the lesson content.
(NAEMSE, 2020)
Distributive education – A generic term used to describe a
variety of learning delivery methods that attempt to accommodate
a geographical separation (at least for some of the time) of the
instructor and learners. Distributed education includes computer
and web-based instruction, distance learning through television
or video, web-based seminars, video conferencing and electronic
and traditional educational models.
Domains – A category of learning. (See Affective domain,
Cognitive domain, and Psychomotor domain.) (NAEMSE, 2020)
Entry-level competence – The level of competence expected
of an individual who is about to begin a career. The minimum
competence necessary to practice safely and effectively.
Health screening – A test or exam performed to nd a condition
before symptoms begin. Screening tests may help nd diseases
or conditions early when they may be easier to treat. (Medline
Plus denition)
Instructional Guidelines – An emeritus resource document that
provided crossover guidance for instructional content within the
2009 National EMS Education Standards.
Licensure – The act of granting an entity permission to do
something that the entity could not legally do without such
permission. Licensing is generally viewed by legislative bodies
as a regulatory effort to protect the public from potential harm.
In the health care delivery system, an individual who is licensed
tends to enjoy a certain amount of autonomy in delivering health
care services. Conversely, the licensed individual must satisfy
ongoing requirements that ensure certain minimum levels of
expertise. A license is generally considered a privilege, not a right.
Medical oversight – Physician review and approval of clinical
content and matters relevant to medical authority.
National EMS Core Content – The document that denes the
domain of out-of-hospital care.
National EMS Education Program Accreditation – The
accreditation process for institutions that sponsor EMS
educational programs.
National EMS Education Standards – The document that
denes the entry-level terminal knowledge content (depth
and breadth), clinical behavior/judgement, and educational
infrastructure for each licensure level.
National EMS Scope of Practice Model – The document
that denes the scope of practice of the various levels of EMS
licensure.
Patient simulation – An alternative to a human patient to help
students improve patient assessment and management skills;
a high-delity patient simulator provides realistic simulation that
responds physiologically to student therapies. These simulators have
realistic features such as chests that rise and fall with respirations,
pupils that react to light, pulses that can be palpated, etc.
Post-graduate internship and/or experience – Experience gained
after the student has completed and graduated from school.

61
Back to Table of Contents >
Practice analysis – A study conducted to determine the
frequency and criticality of the tasks performed in practice.
Preceptor – A clinical teacher or instructor who is responsible for
evaluating and ensuring student progress during hospital and eld
experiences. This individual typically has training to be able to
function effectively in the role.
Primary instructor – A person who possesses the appropriate
academic and/or allied health credentials and understanding
of the principles and theories of education, and the required
instructional experience necessary to provide quality instruction to
students. (NAEMSE, 2020)
Program director – The individual responsible for an educational
program or programs.
Psychomotor domain – Describes learning that takes place
through the attainment of skills and bodily or kinesthetic
movements. (NAEMSE, 2020)
Registration agency – An agency that is traditionally responsible
for providing a product used to evaluate a chosen area. States
may voluntarily adopt this product as part of their licensing
process. The registration agency is also responsible for gathering
and housing data to support the validity and reliability of its product.
Regulation – A rule or a statue that prescribes the management,
governance or operation parameters for a given group; tends to
be a function of administrative agencies to which a legislative
body has delegated authority to promulgate rules and regulations
to “regulate a given industry or profession.” Most regulations are
intended to protect public health, safety and welfare.
Scope of practice – The description of what a licensed individual
legally can and cannot perform.
Standardized patient – An individual who has been thoroughly
trained to accurately simulate a real patient with a medical
condition; a standardized patient plays the role of a patient
for students learning patient assessment, history taking skills,
communication skills and other skills.
Standard of care – The domain of acceptable practice,
as dened by scope of practice, current evidence, industry
consensus and experts. Standard of care can vary depending on
the independent variables of each situation.
Synchronous instruction – Instructional method whereby
learners and instructors interact at the same time, either in
the classroom or via a computer-driven course. This method
allows for more immediate learner guidance and feedback using
face-to-face, instant text-based messaging or real-time voice
communications.
Team leader – Someone who leads the call and provides
guidance and direction for setting priorities, scene and patient
assessment and management. The team leader may not actually
perform all the interventions but may assign others to do so.

62
Back to Table of Contents >
References
National Association of EMS Physicians, (Kuehl, A. E., Ed.),
Prehospital Systems and Medical Oversight, Third Edition. 2002.
Dubuque, IA: Kendall/Hunt Publishing Company.
National Association of EMS Educators. (2020). Foundations
of Education, An EMS Approach, Third Edition. Burlington, MA:
Jones and Bartlett Learning.
National Organization for Competency Assurance. (2006).
NOCA’s Basic Guide to Credentialing Terminology. Washington,
DC: National Organization for Competency Assurance.
Ruple, J. A., et al. (2004). State of EMS Education Research
Project. Prehospital Emergency Care, 9, 203-212.
Ruple, J. A., et al. (2006). Commonalities of the EMS Education
Workforce (2004) in the United States. Prehospital Emergency
Care, 10, 229-238.
NHTSA. (1996). Emergency Medical Services, Agenda for
the Future. Washington, DC: National Highway Trafc Safety
Administration. http://www.nhtsa.dot.gov/people/injury/ems/
agenda/emsman.html
NHTSA. (2019). Emergency Medical Services Agenda 2050.
Washington, DC: National Highway Trafc Safety Administration.
https://www.ems.gov/pdf/EMS-Agenda-2050.pdf
NHTSA. (2005). Emergency Medical Services Core Content.
Washington, DC: National Highway Trafc Safety Administration.
http://www.nhtsa.dot.gov/people/injury/ems/EMSCoreContent/
images/EMSCoreContent.pdf
NHTSA and Health Resources and Services Administration.
(2000). Emergency Medical Services Education Agenda for the
Future: A Systems Approach. Washington, DC: National Highway
Trafc Safety Administration. https://www.ems.gov/pdf/education/
EMS-Education-for-the-Future-A-Systems-Approach/EMS_
Education_Agenda.pdf
NHTSA and Health Resources and Services Administration.
(2007). National EMS Scope of Practice Model. Washington, DC:
National Highway Trafc Safety Administration.
https://www.ems.gov/education/EMSScope.pdf
NHTSA and Health Resources and Services Administration.
(2019). National EMS Scope of Practice Model. Washington,
DC, US Department of Transportation. https://www.ems.gov/pdf/
National_EMS_Scope_of_Practice_Model_2019.pdf
NHTSA and Health Resources and Services Administration.
(2021). National EMS Scope of Practice Model. Washington,
DC, US Department of Transportation. https://www.ems.gov/
pdf/National_EMS_Scope_of_Practice_Model_2019_Change_
Notices_1_and%20_2_August_2021.pdf

63
Back to Table of Contents >
Acknowledgements and Stakeholder Input
Education Standards Revision Team Leadership:
Director: Bryan Ericson, MEd, RN, NRP, Hurst, TX
Co-Chair: Paul Rosenberger, BS, MPA, EdD, NRP, Dallas, TX
Co-Chair: Art Hsieh, MA, NRP, Santa Rosa, CA
Coordinator: Kenneth Navarro, PhD(c), Dallas, TX
Medical Director: Katherine Remick, MD, FAAP, FACEP,
FAEMS, Austin, TX
Medical Director: Joshua Stilley, MD, FACEP, FAAEM, FAEMS,
Columbia, MO
Education Standards Revision Team Members*:
Deborah Akers, NRP, Glen Allen, VA
Steve Cole, MEd, NRP, Boise, ID (Paramedic Level Lead)
Lindi Holt, PhD, NRP, NCEE, Indianapolis, IN (AEMT Level Lead)
Mark Malonzo, EdD(c), NRP, Los Angeles, CA
Gina Riggs, MEd, NRP, Poteau, OK
Jose Salazar, BA, MPH, NRP, Leesburg, VA
Karla Short, BBA, MEd, EdD, Columbus OH (EMR/EMT
Level Lead)
Bill Young, EdD, NRP, Richmond, KY
NAEMSE Leadership:
Linda Abrahamson, MA, RN, EMTP, NCEE, Oak Lawn, IL
Stephen Perdziola, BS, Pittsburgh, PA
Administrative Support:
Jamie Royster, BS, Dallas, TX
* The Revision Team was chosen by NAEMSE in consultation with NHTSA and HRSA, and
comprised educators whose backgrounds and experiences represented a diverse range of
communities, educational institutions and EMS systems.
Federal Partners:
National Highway Trac Safety Administration (NHTSA)
Oce of EMS
David Bryson, EMT, EMS Specialist, Washington, DC
Kate Elkins, MPH, CPH, NRP, EMS Specialist, Washington, DC
Jon Krohmer, MD, FACEP, FAEMS, OEMS Director, Washington, DC
Health Resources and Services Administration (HRSA),
Maternal and Child Health Bureau’s EMS for Children
(EMSC) Program
Sara Kinsman, MD, PhD, MCHB DCAFH Director, Washington, DC
Theresa Morrison-Quinata, DCAFH EMSC Branch Chief,
Washington, DC
Diane Pilkey, RN, MPH, DCAFH Senior Nurse Consultant,
Washington, DC
RedFlash Group:
Tricia Duva, BA, Encinitas, CA
Michael Gerber, MPH, NRP, Washington, DC
Keith Grifths, BA, Encinitas, CA
Wendy Martin, BS, MPC, Encinitas, CA

64
Back to Table of Contents >
Academy of International Mobile Health Integration
American Academy of Pediatrics – NRP Steering Committee
American Ambulance Association
American College of Emergency Physicians
American College of Surgeons Committee on Trauma
Association of Air Medical Services
Association of Critical Care Transport
Commission on Accreditation of Ambulance Services
Commission on Accreditation of Medical Transport Systems
Committee on Accreditation of Educational Programs for the EMS
Professions/Commission on Accreditation of Allied Health Education
Programs
Congress of Mobile Medical Professionals
EMS for Children (Health Resources and Services Administration,
Maternal Child and Health Bureau)
EMS for Children Innovation & Improvement Center
Emergency Nurses Association
Georgia Department of Public Health
International Association of EMS Chiefs
International Association of Fire Chiefs
International Association of Fire Fighters
International Association of Flight & Critical Care Paramedics
State of Minnesota EMS Regulatory Board
National Association of EMS Physicians
National Association of EMTs
National Association of State EMS Ofcials
National EMS Management Association
National Fire Protection Agency
National Registry of EMTs
National Volunteer Fire Council
New Hampshire Department of Safety, Division of Fire Standards and
Training and EMS
New Jersey State EMS Council, 17th District
North Carolina Ofce of EMS
US Army
US Air Force
Project Meetings
• First Development Meeting – May 2-3, 2019, Pittsburgh, PA
• Association Liaison/Stakeholder Call – July 15, 2019
• Second Development Meeting – October 3-4, 2019,
Washington, DC
• Instructional Guideline Revision Meeting –
January 30-February 1, 2020, Hurst, TX
• Association Liaison/Stakeholder Call – August 11, 2020
• Revision Meeting (virtual) – October 9, 2020
• Third Development Meeting (virtual) – January 28, 2021
Public Comment Periods
• August 16-September 20, 2019
• February 17-March 17, 2020
• November 13-December 14, 2020
Stakeholder Organizations Who Provided Input

65
Back to Table of Contents >
Appendix A: Resources for EMS
National Organizations:
American Academy of Emergency Medicine (AAEM): https://www.aaem.org/
American Academy of Pediatrics (AAP): https://www.aap.org/en-us/Pages/Default.aspx
American Academy of Orthopedic Surgeons (AAOS): https://www.aaos.org/
American Ambulance Association (AAA): https://ambulance.org
American College of Emergency Physicians (ACEP): https://www.acep.org/
American College of Surgeons Committee on Trauma (ACS COT): https://www.facs.org/Quality-Programs/Trauma
American Medical Association (AMA): https://www.ama-assn.org/
American Public Health Association (APHA): https://www.apha.org/
American Trauma Society (ATS): https://www.amtrauma.org/
Association of Air Medical Services (AAMS): https://aams.org/
Association of State and Territorial Health Ofcials (ASTHO): https://www.astho.org/
Center for Disease Control: https//www.cdc.gov/
Commission on Accreditation of Allied Health Education Programs (CAAHEP): https://www.caahep.org/
Commission on Accreditation of Ambulance Services (CAAS): https://www.caas.org/
Commission of Accreditation of Medical Transport Systems (CAMTS): https://www.camts.org/International

66
Back to Table of Contents >
National Organizations:
Commission of Accreditation of Medical Transport Systems (CAMTS): https://www.camts.org/International
Committee on Accreditation of Educational Programs for the Emergency Medical Services Professions (CoAEMSP):
https://coaemsp.org/
Emergency Nurses Association (ENA): https://www.ena.org/
International Academies of Emergency Dispatch (IAED): https://www.emergencydispatch.org/home
International Association of Emergency Managers (IAEM): https://www.iaem.org/
International Association of EMS Chiefs (IAEMSC): https://www.iaemsc.org/
International Association of EMTs and Paramedics (IAEP): https://www.iaep.org/
International Association of Fire Chiefs (IAFC): https://www.iafc.org/
International Association of Fireghters: https://www.iaff.org/
International Association of Flight & Critical Care Paramedics (IAFCCP): https://www.iafccp.org/
National Association of County & City Health Ofcials (NACCHO): https://www.naccho.org/about
National Association of EMS Educators (NAEMSE): https://naemse.org/
National Association of EMS Ofcials (NASEMSO): https://nasemso.org/
National Association of EMS Physicians (NAEMSP): https://naemsp.org/
National Association of Emergency Medical Technicians (NAEMT): https://naemt.org/
National EMS Advisory Council: https://www.ems.gov/memsac.html
National EMS Management Association (NEMSMA): https://www.nemsma.org/

67
Back to Table of Contents >
National Organizations:
National EMS Quality Alliance (NEMSQA): https://www.nemsqa.org/
National Fire Protection Association (NFPA): https://www.nfpa.org/
National Organization of State Ofces of Rural Health (NOSORH): https://nosorh.org/
National Registry of Emergency Medical Technicians (NREMT): https://www.nremt.org
National Volunteer Fire Council (NVFC): https://www.nvfc.org/about/
Safe States Alliance: https://www.safestates.org/
Society for Academic Emergency Medicine: https://www.saem.org/home
Federal Agencies:
Federal Interagency Committee on EMS (FICEMS): https://www.ems.gov/ficems.html
Department of Transportation: https://www.transportation.gov/
Federal Highway Administration (FHWA): https://ops.fhwa.dot.gov/eto_tim_pse/preparedness/tim/index.htm
National Highway Trafc Safety Administration (NHTSA): https://www.ems.gov/
Department of Homeland Security (DHS): https://www.dhs.gov/
U.S. Fire Administration (USFA): https://www.usfa.fema.gov/
Department of Health and Human Services (DHHS): https://www.hhs.gov/
Agency for Healthcare Research and Quality (AHRQ): https://www.ahrq.gov/
Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/
National Institute for Occupational Safety and Health (NIOSH): https://www.cdc.gov/niosh/index.htm

68
Back to Table of Contents >
Federal Agencies:
Centers for Medicare & Medicaid Services (CMS): https://www.cms.gov/
Health Resources & Services Administration (HRSA): https://www.hrsa.gov/
Indian Health Service (IHS): https://www.ihs.gov/
National Institutes of Health (NIH): https://www.nih.gov/
Ofce of the Assistant Secretary for Preparedness and Response (ASPR): https://www.phe.gov/about/aspr/Pages/default.aspx
Substance Abuse and Mental Health Services Administration (SAMHSA): https://www.samhsa.gov/
Federal Communications Commission (FCC): https://www.fcc.gov/
Department of Defense (DoD): https://dod.defense.gov/
Ofce of the Assistant Secretary of Defense for Health Affairs: https://www.health.mil/About-MHS/OASDHA
Department of the Interior (DOI): https://www.doi.gov/
National Park Service (NPS): https://www.nps.gov/index.htm
Department of Agriculture (USDA): https://www.usda.gov/
U.S. Forest Service (USFS): https://www.fs.usda.gov/
Department of Labor (DOL): https://www.dol.gov/

69
Back to Table of Contents >
Other Sources:
Occupational Safety and Health Administration (OSHA): https://www.osha.gov/
National Highway Trafc Safety Administration (NHTSA): www.EMS.gov
American Heart Association ECC: https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines
EMSC Innovation and Improvement Center (EIIC): https://emscimprovement.center/
National EMS Advisory Council (NEMSAC): https://www.ems.gov/nemsac.html
National EMS Information System (NEMSIS): https://nemsis.org/
Prehospital Care Research Forum: https://www.cpc.mednet.ucla.edu/pcrf
Prehospital Guidelines Consortium: http://prehospitalguidelines.org/

December 9, 2021
