
1
Allergen Immunotherapy
Extract Preparation
Instructional Guide
Revised October 2019
AUTHORS
Peter Mustillo, MD
Bryan L. Martin, DO, FACAAI
John Oppenheimer, MD, FACAAI
Michael R. Nelson, MD, PhD, FACAAI

2
Table of Contents
I. Introduction .......................................................................................3
II. Allergen Extracts.................................................................................... 4
III. Allergen Extract Mixing Standards Qualifications, and Competencies ......................................5
IV. Allergy Immunotherapy Prescriptions..................................................................7
V. Color Coding, Labels and Beyond Use Dates (BUD) ..................................................... 9
VI. Mixing Individual Patient Allergen Extract Treatment Sets................................................10
VII. Stinging Insect Allergen Extract Preparation ...........................................................15
VIII. Allergen Extract Stability and Storage.................................................................16
IX. Summary .........................................................................................17
X. Acknowledgments .................................................................................18
XI. References ........................................................................................18
XII. Appendices
Appendix 1. Effective Dose Range for Allergen Extracts, US Standardized Units ............................20
Appendix 2. Initial and Ongoing Competency Assessment: Allergen Extract Mixing ........................21
Appendix 3. Extract Volumes Needed for 5.0 ml Maintenance Vials.......................................22
Appendix 4. Recommended Documentation for Allergen Immunotherapy Extract Prescription Forms
and Allergen Immunology Extract Prescription Form ........................................23
Appendix 5. USP Section 21 — Compounding Allergenic Extracts ........................................25
Appendix 6. Forms
Competency Assessment — Initial Personnel Training: Allergen Extract Mixing............................30
Competency Assessment — Annual Personnel Training: Allergen Extract Mixing ..........................32
Competency Assessment — Aseptic Technique and Related Practices of Mixing Personnel .................34
Competency Assessment — Hand Hygiene and Garbing Procedures ....................................36
Competency Assessment — Cleaning and Disinfecting Procedures......................................38
Complaints/Adverse Effects .......................................................................40
Gloved Fingertip and Thumb Sampling .............................................................41
Media-fill Testing Checklist ........................................................................42
Primary Engineering Control (PEC) Hood............................................................43
Refrigerator Temperature Log......................................................................44
©2019 ACAAI

3
I. INTRODUCTION
Origins of Allergy Immunotherapy
Allergen immunotherapy was first introduced
by Leonard Noon in 1911.
1
Dr. Noon originally
hypothesized that patients suffering from “hay fever”
were sensitive to a “toxin” contained in grass pollen. He
proposed that patients would benefit by stimulating the
immune system against the toxin by use of inoculations
of pollen extract. These inoculations involve giving
increasing amounts of allergen extracts to reduce
symptoms on re-exposure to those particular allergens.
The procedure has been widely used since its inception
to treat immediate hypersensitivity disorders mediated
by allergen-specific IgE antibodies. These same basic
principles hold true today, more than 100 years later, for
current allergen immunotherapy.
Efficacy of Allergy Immunotherapy
Multiple studies have demonstrated the effectiveness of
allergen immunotherapy for the following conditions for
both children and adults:
2-25
• Allergic rhinitis
• Allergic conjunctivitis
• Allergic asthma
• Atopic dermatitis
• Insect allergy (Hymenoptera)
Each patient’s immunotherapy prescription is customized
and tailored to their particular allergic triggers, and
the administration schedule (buildup or maintenance)
may vary. The degree of effectiveness may vary for the
individual patient and is in part determined by whether
causative symptoms are predominantly allergic vs non-
allergic — patients may be more likely to have a limited
response if other causes are contributing to impairment.
Other symptomatic causes may include vasomotor
rhinitis, chronic infectious sinusitis, or anatomical
obstruction such as severe adenoidal hypertrophy.
In those whose symptoms are predominantly allergic
in nature, clinical improvement should occur within or
soon after the first year of treatment, and this benefit
may improve with continued treatment. The Allergen
Immunotherapy Practice Parameter third update
26
suggests that, “If clinical improvement is not apparent
after one year of maintenance therapy, possible
reasons for lack of efficacy should be evaluated. If
none are found, discontinuation of immunotherapy
should be considered, and other treatment options
should be pursued.” It has been observed that some
patients may experience a worsening of their asthma,
atopic dermatitis and allergic rhinitis or conjunctivitis
symptoms during treatment, especially during the first
few months of therapy.
Duration of Therapy
There is no consensus on when to discontinue
aeroallergen immunotherapy, but benefits are often
maintained for years after stopping therapy in some
individuals, and indefinitely in others. In grass-
pollen allergy, a three-year course of subcutaneous
immunotherapy gave prolonged relief of symptoms.
25
For many patients with stinging insect allergy, 3-5
years of treatment may be sufficient for sustained
effectiveness. However, patients who have experienced
life-threatening hymenoptera venom reactions should
be considered for life-long treatment.
Adverse Reactions
Allergen immunotherapy is usually well tolerated;
however, adverse reactions do occur, ranging in severity
from mild to severe. Allergen immunotherapy carries a
small but significant risk for life-threatening anaphylaxis
and has very rarely been associated with death.
Systemic reactions associated with immunotherapy may
have numerous causes. Risk factors include asthma and
injections administered during periods of symptom
exacerbations. Human error, due to administering
an incorrect dose or the wrong extract to a patient
is another risk factor. Delays in the administration of
epinephrine during a systemic reaction may increase
the risk of fatalities, which highlights the importance of
having trained personnel capable of identifying and
managing reactions.
Each patient should be evaluated prior to the
immunotherapy administration visit to determine
whether any recent health changes such as illness, acute
asthma symptoms, or new medication - which might
require modifying or withholding the immunotherapy
treatment. Clinical judgment is required when altering
the dose or schedule of administration. While allergen
immunotherapy extracts are relatively easy to prepare
and administer, initial and ongoing training will improve
the expertise of health care workers responsible for
mixing and administering immunotherapy and improve
the safety of the patients.
Subcutaneous allergen immunotherapy is not
indicated for patients with food allergies. Although
studies have demonstrated an increased tolerance to
peanut in patients who received subcutaneous peanut
immunotherapy,
27, 28
there was an unacceptably high
rate of systemic reactions (e.g., anaphylaxis) in most of
the patients during treatment.
28

4
II. ALLERGEN EXTRACTS
Allergen extracts used for immunotherapy are
manufactured following collection of raw material.
They consist of liquid solutions containing dissolved
allergenic proteins derived from pollens, dust mites,
animal dander and epithelia, molds, cockroach, and/or
venom. Extracts chosen for the treatment vials should be
clinically relevant for patients receiving treatment, based
on perennial and seasonal symptoms, the regional
presence of pollens and molds, and causative allergens
based on exposure.
The manufacturing process typically involves crushing
raw materials and “extracting” allergenic proteins by
addition of solvents capable of isolating the protein
from the solid raw material. This is followed by a
purification process, resulting in a liquid solution that is
stable under normal storage condition (approximately
4 degrees C or 39 degrees F), consisting of a mixture
of the diluents or solvents, additives, stabilizer /
preservative, allergenic proteins and other components
of the raw material.
Stock allergen extracts are licensed by the Center for
Biologics Evaluation and Research (CBER) within the
Food and Drug Administration (FDA) in the United
States. Commercially available stock extracts, supplied
by a handful of manufacturers, are used to mix
individual treatment sets and to prepare test panels.
Concentrated stock extracts are available in multiple
forms:
• Aqueous
• Glycerinated
• Lyophilized (freeze dried)
• Acetone precipitated
• Alum precipitated
Glycerinated stock extracts contain 50% glycerin by
definition. Other liquid-based extracts (i.e., saline,
buffers, liquid diluents) are referred to as aqueous
extracts.
Lyophilized extracts are aqueous extracts that
have been freeze-dried to increase stability during
storage and shipping. When they are reconstituted in
accordance with package insert instructions with an
appropriate diluent just prior to use, they form aqueous
extracts. Hymenoptera venom extracts are typically
available in lyophilized form.
Acetone-precipitated extracts are liquid extracts that
include a processing step of acetone precipitation to
create a high concentration stock solution. The acetone
is used to precipitate proteins from liquid into a solid
form, which is then re-dissolved in a diluent to make the
final highly concentrated stock solution.
Alum-precipitated extracts are liquid extracts that
include a processing step involving the addition of
aluminum hydroxide, or alum. Allergenic proteins attach
to the alum and form complexes that serve as depot
when injected into skin, slowing the release of allergens
on injection. The slow-release alum-allergen complexes
may allow for larger doses of extract to be given at less-
frequent intervals and a more rapid buildup to higher
maintenance doses with reduced incidence of systemic
reactions. Local reactions at the site of alum-precipitated
extract injection may be immediate or delayed. Delayed
reactions may start several hours later, with local edema,
erythema (redness), itching and pain.
The cloudy appearance of the extract, which may
contain visible precipitate, is normal and different
than typical aqueous extracts. These extracts require
shaking before use. Furthermore, only certain diluents
can be used to dilute these extracts. The package
insert from stock antigens may be referenced to
identify the appropriate diluents for use with alum-
precipitated extracts. For example, one manufacturer
requires the use of phenol saline diluent for all 10-
fold dilution vials. Ten percent glycerol-saline and
human serum albumin (HSA) diluent usually cannot
be used for alum-precipitated prescriptions because
of interference with the aluminum hydroxide-antigen
absorbed complex. The slow release described above
makes these less effective in skin testing and are thus
used for treatment only.
Diluents are solutions used to keep the allergens in
suspension. They are used to reconstitute lyophilized
extracts, to dilute extracts for diagnostic use, to dilute
vials in treatment sets and to fill maintenance vials to
final volume after addition of stock allergen quantities.
Commonly used diluents:
• Glycerin (e.g., 50% glycerin ± phenol)
• Phenol saline (e.g., 0.4% phenol, saline)
• HSA (e.g., 0.03% HSA, 0.4% phenol, saline)
Each diluent has advantages and disadvantages related
to preservation of extract potency and sterility. These
additives are discussed in further detail in this chapter’s
discussion of extract stability.
Standardized Subcutaneous Allergen Extracts
Standardized subcutaneous allergen extracts in the
United States include:

5
• Cat hair and pelt (BAU/mL potency labeling based
on Fel d 1 content)
• Dust mite (Dermatophagoides pteronyssinus and D.
farinae; potency in AU/ML)
• Short ragweed (potency in AU/mL or wt/vol with
lot-specific Amb a 1 concentration)
• Grass (Bermuda, Kentucky bluegrass, perennial
rye, orchard, timothy, meadow fescue, red top and
sweet vernal; potency in BAU/mL)
• Hymenoptera venoms (yellow jacket, honey bee,
wasp, yellow hornet, white-faced hornet, and mixed
vespids; potency in µg/mL)
These extracts have been standardized with the intent
of ensuring consistency of allergy content and potency
between manufacturers and lots made from the same
manufacturer. Standardization is based on intradermal
skin test responses in allergic individuals. Specifically,
reference standards from the FDA CBER are obtained
for standardized allergen extracts by identifying
concentrations that reproducibly produce erythema
with a sum of perpendicular long axes of 50 mm, or
ID
50
EAL.
29
These reference standards are then used by
manufacturers to ensure that the allergen content of
each new lot falls within specified ranges for potency
labeling. Blood tests (immunoassays) have been
developed that correlate allergenic protein content to
skin test reactions and, in some cases, treatment results.
These include measurement of major allergen content
(cat hair Fel d 1 and ragweed Amb a1), total protein/
hyaluronidase/phospholipase content (Hymenoptera
venom) and other assays (pooled sera immunoassay
inhibition activity).
Units of potency applied to standardized extracts vary
and include bioequivalent allergy unit/mL (BAU/mL),
allergy unit/mL (AU/mL), and microgram protein/mL
(µg/mL). Some allergen extract labels also include the
concentration of major allergenic proteins in µg/mL.
Since the standardization is based on allergen content
falling within a specified range, it still remains possible
for actual allergenic protein content to vary several-fold
for the same potency label. Only a few allergen extracts
have been standardized to date (see Appendix 1 for
effective dosing ranges).
III. ALLERGEN EXTRACT MIXING STANDARDS, QUALIFICATIONS, AND COMPETENCIES
While it would be ideal for allergen mixing personnel
to have a single guideline to refer to, there are
currently two documents that all personnel who mix
allergen extracts must utilize. The most widely adopted
recommendations in the United States for all aspects
of allergen immunotherapy are contained in the 2011
publication, “Allergen immunotherapy: A practice
parameter third update.”
26
This joint effort by experts
from the College and AAAAI and focuses on evidence-
based recommendations to optimize immunotherapy
efficacy and safety. All health care providers involved
in immunotherapy preparation and administration
should be oriented to the contents of this practice
parameter, which contains practical clinical information
and sample forms. In this document, TABLE VII. Allergen
Immunotherapy extract preparation guidelines may be
found on page S36.
The second publication, USP Chapter <797>, focuses
on maintaining sterility in the compounding of
allergen extracts, including requirements for training
and testing of personnel. USP 797 sets standards for
preparing sterile preparations, including allergen extract
preparation. The requirements for compounding of
allergenic extracts are laid out in USP 797 Section 21.
Required qualifications of mixing personnel may be
found in Section 21 on pages 30 — 31, and facilities
requirements found on page 31. These standards,
though extensive and more rigorous than earlier USP
797 requirements, remain less rigorous than standards
required for typical sterile drug compounding in
pharmacies.
Practitioner Qualifications
There are many positions within the allergy immunology
office that have an impact on the safety of allergen
immunotherapy. These include:
1. Supervising physician: responsible for overseeing
and ensuring the competency of staff preparing and
administering allergen immunotherapy.
2. Designated supervisor: person with training
and expertise in allergen immunotherapy who is
responsible for ensuring that personnel who will
be preparing allergen immunotherapy are trained,
evaluated and supervised.
3. Compounding personnel: those who mix allergenic
extracts. Before beginning to independently prepare

6
allergenic extracts, all compounding personnel must
complete training and demonstrate knowledge of
principles and skills for sterile compounding.
4. Shot personnel: those who administer allergy
immunotherapy injections. State laws may differ with
regard to approved personnel. Knowledge of how to
appropriately administer immunotherapy extracts is
critical for patient safety, making personnel training
a requirement. Recognizing the signs and symptoms
of anaphylaxis are also critical for any facility involved
in the delivery of allergen immunotherapy. Efforts
at standardization, including color coding vials,
standardizing labeling and documentation are
intended to decrease the risk of dosing errors for any
facility administering immunotherapy.
Training, Competency Assessment and Documentation
Training of personnel involved in the mixing of
allergen extracts and/or administration of allergen
immunotherapy is a critical requirement for safety
and efficacy. Content of the training should include
core cognitive knowledge as well as demonstration of
procedure performance competency.
There are a variety of ways to receive training in allergen
immunotherapy preparation and administration.
Formats may vary from lectures to hands-on training to
meet the needs of each learner and include:
• On-the-job training from a qualified co-worker or
supervisor.
• Workshops and seminars offered at the College’s
Annual Meeting.
• Educational offerings via the College Learning
Connection, including the Allergen Extract
Preparation Quiz.
• Manuals from allergen extract manufacturers.
• Allergen Immunotherapy: A Practice Parameter
Third Update and other journal articles.
• Allergen Extract Mixing Toolkit.
Suggested qualifications of extract preparation
personnel based on the Practice Parameter on Allergen
Immunotherapy and applicable USP Chapter <797>
standards include ability to:
• Demonstrate understanding of appropriate hand
hygiene, garbing, surface disinfection, aseptic
technique, achieving and/or maintaining sterility,
calculating/measuring/mixing, use of equipment
and documentation.
• Pass a written test on aseptic technique and extract
preparation.
• Annually pass a media-fill or equivalent test
verifying use of aseptic technique.
• Annually pass a gloved fingertip-thumb sampling
test verifying hand sterility after passing three initial
tests.
• Be reinstructed and reevaluated if failing the written
test, media-fill test or gloved fingertip-thumb
sampling test.
To be compliant with USP Chapter 797 Section 21
requirements, allergist offices must keep records
of training, assessment results, evaluations and
qualifications for all compounding personnel, including
any corrective actions following assessments and
evaluations. Appendix 2 contains a sample document
for assessing and documenting competency of
personnel in the preparation of allergen immunotherapy
treatment sets. It is adapted from competency elements
for allergy technicians / nursing personnel at the U.S.
Army Centralized Allergen Extract Laboratory. These
competency elements are based on recommendations
of the Joint Commission on Accreditation of Hospital
Organizations, or JCAHO, requirements. As with all
sample forms, this serves as an example — each mixing
center should develop site-specific standard operating
procedures and competency standards, with forms that
meet the needs of their specific practice.

7
IV. ALLERGEN IMMUNOTHERAPY PRESCRIPTIONS
Allergen immunotherapy prescriptions specify the
precise contents of individual treatment sets for
patients receiving immunotherapy. They may be written
or electronic but should contain several essential
elements. Standardization of content will promote
proper preparation, minimize risk for errors in allergy
shot administration and facilitate patient transfers of
care. Employing the prescribing principles that follow
will result in a product that is safe and effective, and can
ensure maintenance of expected potency through the
expiration date. Each prescription / immunotherapy
record should contain:
• Two patient identifiers (i.e., Name and Date of Birth
or Medical Record Number)
• Patient contact information
• Name of prescriber
• Date of prescription
• Name, concentration and volume for each allergen
• Name and volume of diluents
• Schedule for administration (including adjustments
for interruptions and reactions)
All prescriptions should be reviewed for accuracy prior
to preparation.
Optimal mixing of allergens to create an individual
patient treatment set should be based on:
• Use of relevant allergens for each patient
• Dosing of allergen extracts within minimum
effective dose ranges (Appendix 1)
• Avoiding combining extracts that may adversely
affect overall potency
° Separate high protease extracts (mold, cockroach)
from pollens
32
° Avoid mixing venom extracts with aeroallergen
extracts.
26
Selection and adjustment of doses
using knowledge of cross-reactivity
Mixing high-protease extracts with most other
aeroallergens will result in a loss of potency that can
affect immunotherapy efficacy. Aeroallergens with
known high cross-reactivity allow prescribers to treat
with fewer allergens while providing coverage for
a large number of related allergens. For example,
treatment with one or two northern pasture grass
allergen extracts should be sufficient to provide benefit
for the more than 10 cross-reactive northern grass
species.
34
Figure 1 is an example of a completed allergen
immunotherapy prescription. In this example, the
desired maintenance dose for cat was 2000 BAU for a
0.5-mL injected dose from a 5-mL maintenance vial (a
blank form is available in the Appendix).
2 mL of standardized cat extract (10,000 BAU/
mL) is needed to achieve a final maintenance vial
concentration of 4000 BAU/mL and an injection dose of
2000 BAU. To do this use the step-by-step calculations
below.
Step-by-step calculations are as follows:
• Maintenance vial concentration of cat = injection
dose/injection volume = 2000 BAU/0.5 mL = 4000
BAU/mL
• V1 x C1 = V2 x C2 (maintenance vial volume x
maintenance vial concentration = stock volume x
stock concentration)
• 5mL x 4000 BAU/mL = V2 x 10,000 BAU/mL [V2 =
stock volume = (5 x 4K)/10K = 2 mL]
• Repeat for each antigen in vial
• Total antigen volume = cat 2 mL + D. farinae 0.5 mL
+ D. pteronyssinus 0.5 mL + timothy 0.4 mL + short
ragweed 0.2 mL
• Diluent volume = (maintenance vial volume) – (sum
antigen volumes) = 5 mL – 3.6 mL = 1.4 mL
• Final maintenance vial contents:
Antigen Concentration Dose
Cat 4000 BAU/ml 2000 BAU
Ragweed 17.5 microgram/mL 8.75 microgram/
mL Amb A 1
D. farina 1000 AU/mL 500 AU
D. pteronyssinus 1000 AU/mL 500 AU

8
FIGURE 1. EXAMPLE — ALLERGEN IMMUNOTHERAPY EXTRACT PRESCRIPTION (blank form available in Appendix)
Patient Name: Mary Wheeze Prescribing Physician: Dr. Allergist
Patient Number: Address:
Birth Date: Telephone:
Telephone: Fax:
Antigen
Number
Extract Name
Allergen or Diluent
(Common name of
Genus/species)**
Concentration and Type
Manufacturer’s Extract
(AU, BAU, W/V, PNU)/
(50%, G, Aq, Ly, AP)
Volume of
Manufacturer’s
Extract to Add
Extract
Manufacturer
Lot
Number
Expiration
Date
1
Short Ragweed 1:10 w/v G
(350 mcg Amb a1
0.25 ml Greer 11111 12/25/2021
2
D. farina 10,000 AU/ml G 0.5 ml Allermed 22222 12/26/2021
3
D. Pteronyssinus 10,000 AU/ml G 0.5 ml Antigen labs 33333 2/7/2022
4
Cat 10,000 BAU/ml G 2 ml Hollister-Stier 44444 12/5/2021
5
Timothy Grass 100,000 BAU/ml G 0.4 ml ALK 55555 12/3/2021
6
7
8
9
10
Diluent
HAS 1.35 ml ALK 66666 12/5/2021
Total
Volume
**Components of mixes listed on a separate sheet.
By Use Date ____________________________________________________________________________________________________________
Storage Requirements ___________________________________________________________________________________________________
Results of Quality Control (e.g. visual inspections, second verification of questions) _____________________________________________
Allergen Extract Name:
R, Dm, C, G
Bottle Name Abbreviations
Tree: T Mold: M
Grass: G Cat: C
Weed: W Dog: D
Ragweed: R Cockroach: CR
Mixture: Mx Dust Mite: Dm
Specific Instructions:
Prescribing Physician’s Signature Date
Volume to add = Maintenance Concentration x Total Volume
Conc. of Manufacturer’s Extract
Maintenance concentration and subsequent dilutions
reported as volume/volume (v/v) dilutions with maintenance
concentrations=1:1 v/v
BAU=Bioequivalent Allergy Unit, AU=Allergy Unit
PNY=Protein Nitrogen Unit
W/V=Weight per Volume Ratio
G=50% Glycerinated
Aq=Aqueous, Ly=Lyophilized
AP=Alum precipitated, AcP=Acetone precipitated
Maintenance Concentrate Prescription Form
Prepared by: Great Nurse Date Prepared: 11/01/2019 Time: 10 a.m.
Dates of subsequent dilutions from maintenance concentration with expirations dates:
Vial __________ From Vial __________ on ____/____/____ Expiration date: ____/____/____
Vial __________ From Vial __________ on ____/____/____ Expiration date: ____/____/____
Vial __________ From Vial __________ on ____/____/____ Expiration date: ____/____/____
Vial __________ From Vial __________ on ____/____/____ Expiration date: ____/____/____
*Adapted from Allergen immunotherapy: A practice parameter second update. J Allergy Clin Immunol 2007;120: S77.

9
V. COLOR CODING, LABELS AND BEYOND USE DATES
The Allergen Immunotherapy Practice Parameters
and Joint Commission National Patient Safety goals
emphasize the need for clear and consistent labeling.
Standardization of allergen immunotherapy label
contents and vial coding helps improve communication
between care providers and patients, and likely prevent
errors in extract administration.
Each patient’s treatment vial label should contain at
minimum:
• Patient name, plus a second identifier (e.g., date of
birth)
• Concentration in vol/vol
• Color code and vial number, per the Practice
Parameters
26
• Expiration or beyond use date (BUD)
• Storage conditions
Immunotherapy treatment vial concentrations are
now labeled in vol/vol, with 1:1 vol/vol representing
the maintenance concentrate. Alternatively, the vial
concentration can be labeled in actual units (e.g., 1000
BAU, 100 BAU), but this system may be complicated
if allergens with different potency units are used (e.g.,
wt/vol, BAU, AU or PNU) and these differences make
it difficult to interpret the vial label. All vials in the
treatment set should be numbered and/or color coded
in the following manner as outlined in the most recent
practice parameters (Figure 2, page S44):
26
RED Maintenance 1:1 vol/vol #1
concentrate
YELLOW 10-fold dilution 1:10 vol/vol #2
BLUE 100-fold dilution 1:100 vol/vol #3
GREEN 1000-fold dilution 1:1000 vol/vol #4
SILVER 10,000-fold dilution 1:10,000 vol/vol #5
The highest concentration should be labeled #1 and
the next 10-fold dilution (i.e., yellow vial) would be
labeled #2, and so forth. This system was designed to
eliminate variation from patient to patient that occurs
when labeling vials of higher concentrations with larger
numbers. This practice resulted in patients often having
a different number on their maintenance vial that was
based on the total number of dilutions prepared.
Vial expiration dates should follow the manufacturer’s
recommendations. The expiration date for a treatment
vial should be no later than the earliest expiration
date recommended for any stock allergen or diluent
contained in each prescription vial. Less-concentrated
extracts are more sensitive to temperature and might
not maintain potency until the listed expiration date;
1:10 to 1:200 dilutions of stock extracts are generally
stable for at least 12 months. This usually includes at
least the patient’s red maintenance treatment vial and
the 1:10 vol/vol, or yellow, vial. Expiration dates for
venom extracts may be shorter; perhaps this is due
to the use of diluents with low levels of glycerin. The
venom extract package inserts provide guidelines for
expiration dates for the different dilutions.
Expiration dating periods for allergen extract products
are regulated by the FDA. Even under ideal refrigerated
conditions, some loss of potency occurs over time.
The potency and stability of these products are not
guaranteed beyond their labeled expiration date.
Nonstandard extract products are assigned expiration
dates in accordance with FDA regulations (21 CFR,
Section 610.53) with regard to whether products are
glycerinated or non-glycerinated. A total of six years
from the time of extraction is allotted to 50% glycerin
bulk extracts. This six-year period is divided into a
maximum of three years for manufacturer storage
and three years for shipped vial expiration dating.
Non-glycerinated products are allowed only a total of
three years or half the expiration the time allotted for
glycerinated extracts —18 months for manufacturer
storage and 18 months for shipped expiration dating.
Following is an example of expiration dates for
diagnostic and treatment sets prepared by the
U.S. Army Centralized Allergen Extract Laboratory,
which are based on stock concentrate manufacturer
recommendations from its suppliers.

10
Diagnostic Products Expiration Date*
Prick Test Materials 1 Year
ID Test Materials 6 Months
Immunotherapy Treatment Sets
1:10 W/V-1:5000 W/V 1 Year
1:50,000 W/V and weaker 3-6 Months**
1000 PNU/ml — 20,000 PNU/ml 1 Year
<1000 PNU/ml 3-6 Months**
500 AU/ml and Stronger 1 Year
< 500 AU/ml 3-6 months**
1000 BAU/ml and Stronger 1 Year
< 1000 BAU/ml 3-6 months**
*Use earliest of stock extract label expiration date or date
below
**The stability of lower extract concentrations (e.g.,
1:1000 and 1:10,000 vol/vol) has not been extensively
studied. Loss of potency in these lower concentrations
may be due to absorption of the allergenic proteins to
the glass wall. Human serum albumin may have a more
protective effect against this cause of loss of potency
than other diluents such as normal saline.
Reconstituted Venom Freeze Dried Preparations
100mcg/ml 6 or 12 months*
1-10mcg/ml 1 month
0.1mcg/ml 14 days
<0.1mcg/ml 24 hours
*Varies with company. Guidelines for dilution expiration
dating are in the extract package insert
VI. MIXING INDIVIDUAL PATIENT ALLERGEN EXTRACT TREATMENT SETS
General Principles
Every clinic should develop a specific standard
operating procedure (SOP) document or manual to
ensure standardization and safe practices of allergen
extract mixing. Responsible providers developing the
procedures should consult stock extract manufacturer
recommendations and the most recent Allergen
Immunotherapy Practice Parameter Update to
incorporate the most up-to-date recommendations. USP
797 requirements must also be reviewed and followed.
The mixing of antigens in a syringe is not recommended
because of the potential for cross-contamination of
extracts.
Initial Preparation
1) Designate a dedicated allergenic extracts
compounding area (AECA) with a visible perimeter
that establishes the boundaries of the AECA, and
meets the following conditions (as required by USP
797):
• Access restricted to authorized personnel.
• No other activity permitted during compounding.
• All surfaces are cleanable and kept clean.
• Carpet is not allowed.
• Surfaces must be impervious to cleaning and
sanitizing agents; must be smooth, non-shedding,
and free of cracks or crevices.
• Overhangs should be avoided or must be easily
cleaned.
• Work areas must be well lit, temperature and
humidity controlled for comfort of compounding
personnel.
• Work surface must be cleaned and disinfected
before and after each compounding session;
disinfected between each new set, as well as at the
time of any spill or contamination.
• During compounding, at that time.
2) Before beginning compounding, ensure your
personnel performs hand hygiene and garbing
procedures (that should include the minimum
requirements noted below) and according to your
clinic’s SOPs.
• Low-lint garment with sleeves that fit snugly around
the wrists and that is enclosed at the neck (e.g.,
gowns or coveralls);
• Low-lint, disposable covers for head that cover the
hair and ears and, if applicable, disposable cover
for facial hair;
• Face mask; and
• Sterile powder-free gloves.
3) Ensure compounding personnel rub sterile 70% IPA
onto all surfaces of the gloves and allow them to dry

11
thoroughly throughout the compounding process.
4) Clearly identify expiration dating standards for your
clinic.
5) Become familiar with stock allergen ordering and
storage procedures.
6) Orient personnel to stock allergen extracts,
refrigerator storage designated mixing location,
mixing equipment, prescriptions, documentation and
packaging.
7) Ensure appropriate personnel are trained on SOP and
safety measures and have the required competencies
to independently mix allergen extracts.
Pre-mixing Preparation
1) Verify that a supervising physician is present in the
same building as the mixing location(s).
2) Cleanse and maintain an aseptic work environment
using 70% isopropanol as recommended in USP 797
Allergen Extract Preparation
3) Prepare vial labels in accordance with prescription
and verify accuracy of:
• Name and second identifier
• Concentration
• By use date (BUD) is consistent with clinic
procedures and source antigens.
4) Verify color-coded vials with designated
concentration
Labels may be applied after mixing. For example, the
label for the empty maintenance concentrate (red) vial
(or all vials) can be left off until all contents are injected
into the vial to improve visibility during checks for
impurities, final volume, color comparison of dilution
series, and better aseptic technique.
Example Allergen Extract Mixing Step-By-Step
Procedures
This sample set of procedures provides general guide-
lines that can be used as a starting point to develop
procedures that best fit a specific clinic/facility needs.
Mixing the Maintenance (Red) Vial (see Appendix 3)
1) Select new empty sterile vials (usually 5, 8 or 10 mL)
for each vial in patient’s treatment set, using color
codes to line up strongest (maintenance/red) to most
dilute.
2) Select stock extract for each antigen contained in the
prescription, and stock diluents.
• Check stock antigens for turbidity/particulate
matter. If present, consult package insert or
manufacturer guidelines including possible
recommendations for resuspension or filtering.
• For prolonged mixing sessions, return unused
stock extracts to refrigerator or cooling tray (2º-8ºC)
between prescriptions or during extended breaks.
3) Place a new syringe by each stock antigen vial and
the diluent.
• A separate syringe is used for each antigen and
diluent.
• Label each syringe (i.e. abbreviation for antigen or
diluents)
• Avoid storing stock extracts in a syringe for
extended periods due to risk of potency loss and
misidentification.
4) Document lot number and manufacturer for each
antigen
5) Ensure that label expiration date does not exceed
earliest stock vial extract or diluent expiration date.
6) Perform Hand Hygiene per USP 797 standards.
• Remove visible debris from underneath fingernails
under warm running water using a disposable nail
cleaner
• Wash hands and forearms up to the elbows with
soap and water for at least 30 seconds
• Dry hands and forearms to the elbows completely
with low-lint disposable towels or wipers.
7) Personnel garbing requirements
• Don hair and facial hair covers, gowns and face
masks
• Use alcohol- based surgical hand scrub prior to
gloving.
• Don powder-free sterile gloves compatible with
70% isopropyl alcohol.
8) Disinfect gloves with isopropyl alcohol and allow
them to dry before mixing (and intermittently for
lengthy mixing).
9) Wipe vials and/or ampules with 70% isopropyl
alcohol and allow to dry.
10) Maintain aseptic technique by minimizing contact
with secretions, skin, glove fingertips and other
potential sources of contamination during the
mixing process.

12
11) Draw the correct amount of each antigen and the
diluent into the syringe, and place each syringe by
the respective stock antigen vial.
12) Verify drawn doses are correct volume and antigen.
(Quality checkpoint opportunity: have a co-worker
verify, if available. This is a best practice, but this is
not required by USP 797.)
13) Sequentially inject contents of antigens into the
maintenance concentrate (red) vial.
• Empty syringes should be discarded immediately
into an appropriate sharps disposal container
• If the sterile maintenance vial is not a vacuum vial,
an equal volume of air may need to be withdrawn
prior to injecting stock extract volumes
14) After mixing is complete, conduct final quality
assurance check (best practice would include mixer
and trained co-worker), including:
• Solution color check.
• Label check.
• Vial color-code check.
• Liquid turbidity, precipitate and consistency check.
• Vial physical integrity (leaks, cracks and so on)
check.
15) If applicable, package treatment set for transport or
shipping.
16) Document preparation details according to clinic-
specific procedures on prescription or preparation
form and in mixing log as follows:
• Name of preparer and date prepared.
• Stock allergen extract manufacturer, lot number
and beyond-use or expiration date.
• Mixing log, to be maintained in the unlikely event
of a stock allergen recall or for extract or adverse-
event troubleshooting.
Notes Regarding Alum-Precipitated Extracts
• Diluent: Alum-precipitated extracts generally
require phenol saline diluent for all 10-fold dilution
vials. Ten percent glycerol-saline or HSA diluent
cannot be used for alum- precipitated prescriptions
as it interferes with the aluminum hydroxide-
antigen absorbed complex.
• For alum-precipitated extract treatment vials,
consider applying a small “shake well” label, as
the alum-precipitated antigens are very viscous
in nature. Precipitated alum- antigen complex will
settle to the bottom of the vial.
• Unlike aqueous and glycerinated extracts that
generally do not lose potency with filtering, large
antigen-alum complexes may be lost during the
filtering process, with the result being a result
in loss of potency. Therefore, do not filter alum-
precipitated extracts.
Preparing Serial 10-Fold Dilutions
• Serial 10-fold dilutions are prepared to complete a
patient’s initial allergen immunotherapy treatment
vial set. Dilutions are made by serial dilution
(taking from a parent vial and placing into a new
vial prefilled with diluent to create a 10-fold dilution
1/10 the amount of allergen contained in the
parent vial). This newly diluted vial then becomes
the “new” parent vial, and dilutions are repeated
until the desired number of 10-fold dilutions is
achieved.
• The volume used to make serial dilutions from
parent vials depends on both the desired dilution
(10-fold in this case) and the final volume.
Typical treatment set vials are 2, 5, 8 or 10 mL.
Treatment set vials are available with original or
snap-on colored caps to create sets according to
the recommended color scheme. Vials also are
available empty or prefilled with diluents suitable
for intradermal or subcutaneous administration.
Prefilled volumes correspond to the amount of
diluent needed to make a 10-fold dilution.
• To determine how much should be taken from the
parent vial for a 10-fold dilution for final volume
X, divide X by ten (i.e., for a 10 ml vial: 10ml/10
= 1 ml). Then calculate the amount of diluent
needed by subtracting this X/10 volume from the
final volume X (i.e. 10 ml – 1 ml = 9 ml). The final
concentration of the diluted vial is 1/10th that of the
parent vial.
Sample preparation of a 5-mL SERIAL 10-Fold Dilution
Verify that the labeling and order (color coded, label
concentration) for vials are correct.
1) Ensure the maintenance vial is mixed by inverting or
rolling.
2) Using a fresh syringe and aseptic technique, remove
0.5 mL from the mixed 5-mL maintenance concentrate
red or 1:1 vol/vol vial.
3) Using aseptic technique, inject this 0.5 mL form
the maintenance vial into the 4.5-mL prefilled (10%
glycerol-saline or HSA) yellow or 1:10 vol/vol vial.
This vial will consist of 5mL of a 10-fold dilution of the
maintenance concentration vial.
4) Ensure the newly made 10-fold diluted (yellow) vial is
mixed by inverting or rolling.
13
5) Subsequent 10-fold dilutions are done in the same
manner for the remainder of the vials in the treatment
set (0.5 mL into 4.5 mL of the 10-fold, labeled 10%
glycerol-saline prefilled vial):
1. 0.5 mL from yellow 1:10 vol/vol into a 4.5 mL
diluent-filled blue 1:100 vol/vol vial
2. 0.5 mL from blue 1:100 vol/vol into 4.5 mL diluent-
filled green 1:1000 vol/vol vial
3. 0.5 mL from green 1:1000 vol/vol into 4.5 mL
diluent-filled silver 1:10,000 vol/vol vial
4. And so on for additional more dilute (silver) vials
5. Whereas using a fresh syringe for each dilution
transfer is often preferred, use of the same syringe
for serial dilution transfers is an alternative if a
“mix/rinse” step is included. A mix/rinse step
consists of pulling up a syringe volume (1mL for
a 1-mL syringe) from the vial just injected and re-
injected into the same vial without removing the
syringe. This is often repeated (i.e., for a total of
three times) prior to pulling up the final volume for
the transfer to the next dilute vial. (Reminder: This
is for making dilutions only. Do not reuse syringes
or mix/rinse between different stock solutions
when mixing the initial maintenance vial.)
Table 1. Calculations for making Extract Dilutions
Table II. Calculations for making Extract Dilutions* (from Practice Parameters page S10)
All dilutions can be calculated by using the following formula:
V1 X C1 = V2 X C2,
where
V1 = Final volume you want to prepare
C1 = Concentration (wt/vol or PNU) of extract you want to prepare
V2 = Volume of extract you will need for dilution
C2 = Concentration of extract you will use.
Example: Solve for V2; (V1 X C1)/C2 = V2.
To determine the concentration of an item in a mixture:
1. determine which formula you need to use;
2. choose the numbers/fractions that will be inserted into the formula for V1, C1, V2, and C2;
3. change all wt/vol fractions to a decimal number and insert into the formula (see below); and
4. multiply first and then divide to get the answer.
To express concentration as a percentage:
1:10 wt/vol 1/10 = 0.1 X 100 = 10% solution
1:20 wt/vol 1/20 = 0.05 X 100 = 5% solution
1:40 wt/vol 1/40 = 0.025 X 100 = 2.5% solution
Example:
V1 = 5 mL Final volume you want to prepare
C1 = 1:200 Concentration you want to prepare
V2 = Unknown Volume of extract you will need for dilution
C2 = 1:10 Concentration of extract you will use
Add values into formula:
V1 X C1 = V2 X C2 5 X (1/200) = V2 X (1/10)
5 X (0.005) = V2 X (0.1)
V2 = (V1 X C1)/C2 V2 = 0.025/0.1 = 0.25
To determine amount of diluent needed:
V1 — V2 5 – 0.25 = 4.75 mL
Adapted from the Greer Allergy Compendium. Lenoir (NC): Greer Laboratories: 2005. p. 71. Permission provided by Robert Esch, PhD.

14
Allergen Extract Treatment Set Preparation Hints
1) Do not mix prescriptions for more than one patient at
a time.
2) Train multiple qualified personnel in allergen extract
preparation in case of absences and for participation
in quality checks.
3) Avoid putting hand lotion on before the
compounding of allergen extract and skin test
antigens. Lotion tends to harbor bacteria.
4) Regularly review operating procedures for opportunities
to make the process safer and more efficient.
5) Establish a regular inventory check.
• Identify stock allergen extracts, diluents and mixing
supplies in need of reordering
• Check for expiring stock allergen extracts, diluents
and mixing supplies
6) Return antigen stock trays to the refrigerator when
away from the compounding area for an extended
period of time.
7) Minimize distractions during extract preparation.
8) Stock refrigerators are not to be used for food or
drink storage.
9) Particulates and precipitates suspended in an extract
solution are not uncommon.
• These particulates and precipitates often do not
cause any significant loss in potency. Consult
manufacturer recommendations in package insert
or bulletins for additional information.
• Attempted re-suspension by agitation (shaking
or rolling) may be indicated in accordance with
the package insert and your clinic operating
procedures.
10) Diluted allergen immunotherapy vials (yellow,
blue, green, and silver) should not made by pulling
directly from a manufacturer’s concentrated stock
vial extract.
• The primary reason for this is the potential for error
that is increased progressively with each dilution. For
dilute vials, a very small amount of allergen would
need to be pulled from the stock extract vial, and it is
virtually impossible to achieve the precision needed
for the most dilute vials.
• Thus, a dilution vial prepared by this method
may contain inaccurate amounts of extract and
potentially increase the risk of adverse events
during vial transitions within the buildup phase.
Additional Quality Assurance Checks
Additional quality assurance checks before allergen
extract shipping and use ideally are confirmed by a co-
worker. Vials should be inspected for:
• Vial serial color dilution that matches label
concentration and vial color coding
• Vial integrity (no cracks, leaks, and so on)
• Vial content (particulate matter, fill volume, and so
on)
• Label accuracy – “five rights” as described below
Verify that the label contains the 5 rights
• Right name,
• Right content (allergens),
• Right concentration, right alphanumeric number
in the right order with most concentrated = 1 (if
numbers used),
• Right expiration date (dilute vials may have earlier
expiration dates than more concentrated vials).
• Right color, a solution color check for each vial
should be conducted.
The solution in the maintenance concentrate vial should
be the darkest in color, and vials should be lighter in
color with each 10-fold dilution. The weakest strength
vial should contain the lightest-colored solution. When
using color-coded vials, a vial color code check should
be performed. Vials in the treatment set should be
arranged in order (red/maintenance, yellow, blue,
green and silver). For each color-coded vial, label
concentration, in vol/vol, or number should match what
is recommended in the Practice Parameters for the color
code (see Tables XI and XII from Practice Parameters
26
).
All vials should also undergo a content check. Vials
should be filled to the expected volume. Solutions
within each vial should be inspected for the presence of
particulate or solid materials and cloudiness. If found,
vials may be contaminated or contain precipitated
raw allergen extract contents. Contamination may
be bacterial or other microbial source, but may
also be a result of introduced solid materials like
the rare occurrence of vial stopper fragments from
manufacturing or repeated puncturing. Any abnormal
finding during any of these checks should be followed
by an investigation for the cause and, in most instances,
starting over and remixing that patient’s vial set.

15
Table 2. Preparing Allergen Extract Treatment Sets (2 antigens, 0.5 ml stock of each)
Dilution label/
color
Label Conc
vol/vol
Extract
added
Diluent
added
Ragweed
w/v
Grass
BAU/ml
stock extract 1:10 100,000
1 (red/maint) 1:1 0.5 mL of each stock 4.0 mL 1:100 10,000
2 (yellow) 1:10 0.5 mL red (1) vial 4.5 mL 1:1,000 1,000
3 (blue) 1:100 0.5 mL yellow (2) vial 4.5 mL 1:10.000 100
4 (green) 1:1,000 0.5 mL blue (3) vial 4.5 mL 1:100,000 10
5 (silver) 1:10,000 0.5 mL green (4) vial 4.5 mL 1:1,000,000 1
*Treatment set for maintenance concentrate with 0.5 ml stock conc. grass (100,000 BAU/ml) & ragweed (1:10 w/v) in 5ml
VII. STINGING INSECT ALLERGEN EXTRACT PREPARATION
Extracts are available for five winged Hymenoptera
species at a concentration of 100 µg/mL: honey bee,
wasp, yellow jacket, yellow hornet and white-faced
hornet. The last three (yellow jacket, yellow hornet
and white-faced hornet) are closely related members
of the Vespidae family and have also been combined
in a single “mixed vespid” extract at a reconstituted
concentration of 300 µg/mL. Lyophilized or freeze-
dried stinging insect venom extracts are available
commercially for diagnostic testing and patient
treatment. These extracts are composed of venom
isolated directly from dissected venom sacs.
Previously manufactured extracts using whole insect
body as opposed to concentrated venom proved
not to be as effective as extracts made from venom.
35
Accordingly, handling of these extracts is limited to
reconstitution and dilution. The same principles and
requirements for labeling apply with the exception of
number/color coding and use of vol/vol concentration.
The concentration of these extracts and all dilutions is
expressed in µg/mL. Reconstitution and dilution of all
insect venom extracts is most commonly performed with
HSA (HSA/phenol) diluent.
Extracts are also available for imported fire ant
Hymenoptera species. Two fire ant species, Solenopsis
richteri and S. invicta, are commercially available as
individual extracts for testing or treatment, or as a
fire ant mix containing both species. Fire ant extracts
are made from whole fire ant bodies. Fire ant venom
extracts are being investigated for clinical use but
require a significant amount of time and resources for
mass production. Fire ant stock concentrate extracts
typically are available as non-standardized glycerinated
extracts in wt/vol concentrations (i.e., 1:20 wt/vol). The
Practice Parameters for Insect Allergy contains survey
data on common fire ant maintenance doses ranging
from 0.5 mL of 1:100 wt/vol to 0.5 mL of 1:10 wt/vol
maintenance concentrate, with most using 0.5 mL of a
1:100 wt/vol maintenance concentrate.
36
Insect venom (and fire ant) extracts generally should
not be mixed with other venom or aeroallergen extracts
for either testing or treatment because of the lack of
sufficient stability, safety and efficacy studies to support
mixing. The only FDA-approved mixture is commercially
available mixed vespid extract containing 100 µg/mL of
each of the three common vespids.

16
VIII. ALLERGEN EXTRACT STABILITY AND STORAGE
The stability and potency of allergen extracts can be
compromised by elevated temperatures, contamination
and protease degradation of key allergenic proteins
responsible for the efficacy of immunotherapy.
31-34,37
Several measures are taken by stock extract manufacturers
and healthcare personnel to minimize the risk of loss of
potency of extracts during normal storage and use.
Dilution of extracts alone can affect the long-term
potency of extracts. For example, diluted extracts have
lower concentrations of important preservatives and
stabilizers. Furthermore, lower concentrations of proteins
decrease three-dimensional protein structure stabilization
achieved through protein-interactions present at higher
protein concentrations. Finally, dilutions may also magnify
the effect of allergenic protein loss as a result of binding
to sites on glass vials that is essentially insignificant at
higher protein concentrations.
There are several “routine” operating procedures that
when performed consistently should promote extract
stability and reduce errors associated with the use of
outdated materials:
• Routinely check expiration dates on all products.
• Ensure that the stock inventory in refrigerators is
routinely rotated such that expiring products are
placed in the front and used first.
• Verify that the expiration dates on labels for
treatment and diagnostic sets are no later than the
stock extract used with the earliest expiration date.
• Discard or separate products that have expired.
• Ensure that personal allergen extract storage trays
are stored at recommended temperatures.
• Ensure that extracts are kept cool during extended
periods of mixing.
Manufacturer processing steps include additives that
stabilize the allergenic proteins and preservatives
that prevent contamination of the stock extract and
individual patient treatment sets derived from them.
Preservatives are added to allergen extract solutions
to prevent microbial growth in the event that bacteria
or fungi are introduced into the solution during the
preparation process or when needles are inserted
into vials for administration of immunotherapy. All
allergen extracts must contain preservatives that are
bacteriostatic. Bacteriostatic agents prevent the growth
of microbial contaminants like bacteria, but do not
necessarily kill microorganisms.
Sterilization and pasteurization processes that kill
microorganisms are less commonly used.
Phenol is a common bacteriostatic preservative added
to allergen extracts and is used at a final concentration
of approximately 0.4%. One possible ill effect of using
phenol is that it may denature (unfold or breakdown)
allergenic proteins even if in a 50% glycerin.
31,33
HSA
may protect against phenol’s adverse effects on
allergenic proteins.
31
Other recognized preservatives
such as thimerosal and methylparaben are not generally
used in allergen extract preparation.
Stabilizers are added to diluents to maintain the
structure of allergens in solution and prevent sticking or
adherence to the glass vials in which they are contained.
Common stabilizers include glycerin and HSA. Fifty
percent glycerin is often considered the best stabilizer
alternative and is also considered a preservative,
whereas HSA is not a preservative. Glycerin potently
stabilizes proteins in solution and inhibits proteases
found in some allergen extracts, and is bacteriostatic at
concentrations ≥20%.
37
Preservative and stabilizing properties decrease as the
concentration of glycerin is decreased. Glycerin, when
injected subcutaneously, can cause local irritation and
result is a burning sensation.
Allergen extracts are stored in refrigerators at a
temperature of 4ºC or in accordance with manufacturer
recommendations. A temperature range of 2˚- 8ºC is
considered acceptable by most experts. Given the
expense and temperature sensitivity of stock allergen
extract concentrates and mixed patient treatment
sets, it is also reasonable to conduct some form of
temperature monitoring to ensure that extracts are not
exposed to temperature extremes. For example, a log
of daily temperatures (See Refrigerator Temperature
Log Form) can be maintained or an automated
continuous temperature monitoring device can be
installed. Facilities might also consider installing
temperature alarms.
Many allergen extracts are heat sensitive. The loss in
potency when allergen extracts are exposed to high
temperatures (i.e., over 78ºF or 26ºC) may be due to the
heat-labile (-sensitive) proteins that unfold or degrade
at these temperatures. Loss of potency can also occur at
lower temperatures, including room temperature (i.e.,
68ºF – 72ºF and 22ºC). This is possibly due to proteases
in the extract that are activated at these temperatures
and degrade relevant allergen proteins in the extract.
Allergen extracts exposed to room temperature over
time may thus lose potency, such as extracts frequently
left out of the refrigerator for long periods during
testing or treatment. For example, skin testing trays

17
with extracts that are taken out of the refrigerator in
the morning every day and not replaced until the clinic
closes in the evening may suffer from reductions in
potency unless the trays are cooled while out of the
refrigerator. Short intervals for testing or treatment rarely
result in clinically significant losses of potency. Fifty
percent glycerin may help protect against the effects
of prolonged exposure to room temperature, possibly
due to its effect on proteolytic enzymes. Less is known
about the effects of freezing (<0ºC) on allergen extract
potency, but at least one study found a moderate loss of
potency when an extract was stored frozen and thawed
for use.
15
An increase in the number of multiple freeze-
thaw cycles increases the observed loss in potency
of extracts. Thus, extracts that are accidentally frozen
should be replaced with new extract prior to use.
Some extracts contain proteolytic enzymes or proteases
that can degrade proteins needed for allergen extract
effectiveness. Tree, grass and weed pollens and some
pet danders are particularly susceptible to these
proteases. For this reason, the most recent Practice
Parameters recommend the separation of extracts
with high proteolytic enzyme activities, such as mold
and cockroach, from other extracts, such as pollens.
Dust mite extracts do not appear to cause significant
degradation of pollen or animal dander extracts and
thus can be mixed together.
Investigations have shown that extracts stored in vials
only partially filled with solution are less stable. In
other words, 1 mL of extract in a 10-mL vial will lose
potency more rapidly than 10 mL of extract in a 10-
mL vial. This volume effect is more pronounced with
higher dilutions. For this reason, it is reasonable to
consider reordering and preparing treatment and
diagnostic materials as the extract volume in current
vials diminishes.
IX. SUMMARY
The preparation of allergen immunotherapy extracts is
a technical skill that requires training and a high level
of attention to detail. Errors may cause life-threatening
allergic reactions in patients receiving immunotherapy.
Using a team approach to develop clinic/facility-
specific policies and procedures and verify ongoing
competency will ultimately improve the quality and
precision of allergen immunotherapy preparation.
Ongoing review of these procedures will lead to
increased knowledge of and adherence by individuals
preparing allergen extracts. These steps will ensure
the end product is appropriately prepared according
to the most recent standards and manufacturer
recommendations. Thorough knowledge and training will
promote the safety of the patients entrusted to our care
and of those performing allergen extract preparation.
There are several major themes that new personnel
assigned to prepare allergen extracts should become
familiar with. These include, but are not limited to:
• Contamination is prevented by adequate training
and the use of using aseptic technique
• Accurate labels and color coding are highly
recommended to prevent errors
• Use of quality assurance checks throughout the
mixing process is highly recommended
• Initial treatment sets consist of a maintenance vial
and a series of 10-fold dilutions
• Stinging insect and aeroallergen extracts should
not be mixed
All personnel involved in allergen extract preparation
should be familiar with the contents of the most recent
Immunotherapy Practice Parameter and 2019 Updated
USP 797 Standards for allergen extract mixing. A
companion examination has been developed based on
this training document to assist in satisfying competency
assessment and documentation requirements. It is
currently available via the College Learning Connection.

18
XI. REFERENCES
1. Noon, L. (1911). Prophylactic inoculation against hay
fever. Lancet, 1, 1572-73.
2. Ross, R. N., Nelson, H.S., Finegold, I. (2000). Effec-
tiveness of specific immunotherapy in the treatment
of asthma: A meta-analysis of prospective, random-
ized, double-blind, placebo- controlled studies. Clin
Ther, 22, 329-41.
3. Ross, R. N., Nelson, H.S., Finegold, (2000). Effective-
ness of specific immunotherapy in the treatment of
allergic rhinitis: An analysis of randomized, prospec-
tive, single- or double-blind, placebo-controlled
studies. Clin Ther, 22, 342-350.
4. Ross, R. N., H.S., Finegold, I. (2000). Effectiveness of
specific immunotherapy in the treatment of hyme-
noptera venom hypersensitivity: A meta-analysis.
Clin Ther, 22, 351-8.
5. Calderon, M. A., Alves, B., Jacobson, M., Hurwitz,
B., Sheikh, A., Durham, S. (2007). Allergen injection
immunotherapy for seasonal allergic rhinitis. The Co-
chrane Database of Systematic Reviews, Jan 24(1).
CD001936.
6. Abramson, M. J., Puy, R. M., Weiner, J. M. (2003).
Allergen immunotherapy for asthma. The Cochrane
Database of Systematic Reviews. (4). $%001186.
7. Lockey, R., Bukantz, S., Bousquet, J. (Eds.) (2004).
Allergens and allergen immunotherapy. (3rd Ed).
8. Ewan, P. W., Alexander, M. M., Snape, C., Ind, P. W.,
Agrell, B., Drebord, S. (1988). Effective hyposensi-
tization in allergic rhinitis using a potent partially
purified extract of house dust mite. Clin Allergy, 18,
501-8.
9. Olsen, O. T., Larsen, K. R., Jacobsan, L., Svendsen, U.
G. (1997). A 1-year placebo-controlled, double-blind
house dust-mite immunotherapy study in asthmatic
adults. Allergy, 52, 853-859.
10. Haugaard, L., Dahl, R., Jacobsen, L. (1993). A con-
trolled dose-response study of immunotherapy with
standardized, partially purified extract of house dust
mite: Clinical efficacy and side effects. J Allergy Clin
Immunol, 91, 709-22.
11. Ohman, J. L., Jr., Sundin, B. (1987). Standardized
allergenic extracts derived from mammals. Clin Rev
Allergy, 5, 37-47.
12. Lombardero, M., Carreira, J., Duffort, O. (1988).
Monoclonal antibody based radioimmunoassay for
the quantitation of the main cat allergen (Fel d I or
Cat-1). J Immunol Methods, 108, 71-76.
13. American Academy of Allergy, Asthma and Immu-
nology (AAAAI) (1977). The use of standardized
allergen extracts. J Allergy Clin Immunol, 99, 583-6.
X. ACKNOWLEDGMENTS
ORIGINAL DOCUMENT CREATED IN 2007
Authored by:
Michael R. Nelson, MD, PhD, FAAAAI, FACAAI
Edited by:
Linda Cox, MD, FAAAAI
Tao T. Le, MD, MHS, FACAAI, FAAAAI
With Acknowledgments to:
Ms. Susan Kosisky, Ms. Anita Bienlein, Dr. Ceclia Mikita,
Mr. Eric Riddock, TSgt Adam Hughlett, TSgt Debra Horne
of the US Army Centralized Allergen Extract Laboratory at
Walter Reed Army Medical Center. Dr. Bryan Martin and
Dr. Renata Engler of the Walter Reed Vaccine Healthcare
Centers Network. Dr. Gary Gross and Dr. Don Aaronson,
MD of Advocacy Council of ACAAI; Dr. Linda Cox and
colleagues of the AAAAI Immunotherapy and Allergy
Diagnostics Committee and ACAAI Immunotherapy and
Diagnostics Committee and the members of ACAAI/
AAAAI Task Force on Practice Parameters.
DOCUMENT REVISED IN 2017
ACAAI Immunotherapy & Diagnostics Committee
John J. Oppenheimer, MD — Chair
Mike Tankersley, MD
Trever Burnett, MD
David B. Engler, MD
Warren V. Filley, MD
Desiree E. Larenas-Linnemann, MD
Alnoor A. Malick, MD
Anil Nanda, MD
Michael R. Nelson, MD, PhD
Ruby Pawankar MD, PhD, FRCP
Jorge A. Quel, MD
Noel Rodriguez, MD
Millard Tierce, IV, DO
Kevin M. White, MD
Ira Finegold, MD
Cheryl Bernstein, RN

19
14. Van Metre, T. E., Jr., Marsh, D. G., Adkinson, N. F.,
Jr., et al. (1989). Immunotherapy decreases skin
sensitivity to cat extract. J Allergy Clin Immunol, 83,
888-899.
15. Van Metre, T. T., Jr., Marsh, D. G., Adkinson, N. G., Jr.,
et al. (1988). Immunotherapy for cat asthma.
J Allergy Clin Immunol, 82, 1055-1068.
16. Ewbank, P. A., Murray, J., Sanders, K., Curran-Eberett,
D., Dreskin, S., Nelson, H. S. (2003). A double-blind,
placebo-controlled immunotherapy dose-response
study with standardized cat extract. J Allergy Clin
Immunol, 111, 155-161.
17. Dolz, I., Martinez-Cocera, C., Bartolome, J. M., Cimar-
ra, M. (1996). A double-blind, placebo-controlled
study of immunotherapy with grass-pollen extract
Alutard SQ During a 3-year period with initial rush
immunotherapy. Allergy, 51, 489-500.
18. Walker, S. M., Pajno, G. B., Lima, M. T., Wilson, D. R.,
Durham, S. R. (2001). Grass pollen immunotherapy
for seasonal rhinitis and asthma: A randomized,
controlled trial. J Allergy Clin Immunol, 107, 87-93.
19. Frew, A. J., Powell, R. J., Corrigan C. J., Durham, S. R.
(2006). Efficacy and safety of specific immunother-
apy with SQ allergen extract in treatment-resistant
seasonal allergic rhinoconjunctivitis. J Allergy Clin
Immunol, 117, 319-325.
20. Leynadier, F., Banoun, L., Dollois, B., et al. (2001). Im-
munotherapy with a calcium phosphate-adsorbed
five-grass pollen extract in Seasonal rhinoconjuncti-
vitis: A double-blind, placebo-controlled study. Clin
Exp Allergy, 31, 988-996.
21. Lockey, R., Slater, J., Esch, E. Preparation of standard-
ization of allergen extracts. In F. Adkinson, J. Yungin-
ger, W. Busse, B. Bochner, S. Holgate, & E. Simmons
(Eds.0. (2003). Middelton’s allergy principles and
practice (6th ed.). St. Louis: Mosby.
22. Creticos, P., Adkinson, N. F., Jr., Kagey-Sabotka, A.,
et al. (1985). Nasal challenge with ragweed pollen in
hay fever patients: Effect of immunotherapy. J Clin
Invest, 76, 2247-2253.
23. Creticos, P. S., Marsh, D. G., Proud, D., et al. (1989).
Responses to ragweed-pollen nasal challenge be-
fore and after immunotherapy.
J Allergy Clin Immunol, 84, 197-205.
24. Lent, A. M., Harbekc, R., Strand, M., et al. (2006). Im-
munologic response to administration of standard-
ized dog allergen extract at differing doses. J Allergy
Clin Immunol, 118, 1249-1256.
25. Durham, S. R., Walker, S. M., Varga, E. M., et al.
(1999). Long-term clinical efficacy of grass-pollen
immunotherapy. N Engl J Med, 341, 468- 475.
26. Cox, L., Nelson, H., Lockey, R., et al. (2011). Allergen
immunotherapy: A practice parameter third update.
J Allergy Clin Immunol, 127 (1 Suppl,) S1-S55. Erra-
tum. (2011). J Allergy Clin Immunol, 127, 840.
27. Oppenheimer, J. J., Nelson, H. S., Bock, S. A., Chris-
tensen, F., Leung, D. Y. (1992). Treatment of peanut
allergy with rush immunotherapy.
J Allergy Clin Immunol, 90, 256-262.
28. Nelson, H. S., Lahr, J., Rule, R., Bock, A., Leung, D.
(1997). Treatment of anaphylactic sensitivity to pea-
nuts by immunotherapy with injections of aqueous
peanut extract. J Allergy Clin Immunol, 99, 744-751.
29. Turkeltaub, P. Allergenic extracts. II. In vivo standard-
ization. In E. Middleton, JR., E. F. Ellis, N. F. Adkinson,
Jr., & J. W. Yunginger (Eds.). (1988). Allergy: Princi-
ples and practice (3rd ed.). St. Louis: Mosby.
30. USP Sterile Compounding Committee (2008, 2019).
USP <797> Guidebook to Pharmaceutical Com-
pounding — Sterile Preparations. U.S. Pharmacopeia
31. Vijay, H. M., Young, N. M., Bernstein, I. L. (1987).
Studies on Alternaria tenuis extracts under a variety
of storage conditions. Int Arch Allergy Appl Immu-
nol, 83, 325-328.
32. Grier, T. J., LeFevre, D. M., Duncan, E. A., Esch, R. E.
(2007). Stability of standardized grass, dust mite, cat,
and short ragweed allergens after mixing with mold
or cockroach extracts. Ann Allergy Asthma Immunol,
99, 151-160.
33. Niemeijer, N. R., Kauffman, H. F., van Hove, W., Du-
bois, A. E., de Monchy, J. G. (1996). Effect of dilution,
temperature, and preservatives on the long-term
stability of standardized inhalant allergen extracts.
Ann Allergy Asthma Immunol, 76, 535-540.
34. Weber, R. W. (2008). Guidelines for using pollen
cross-reactivity in formulating allergen immunother-
apy. J Allergy Clin Immunol, 122, 219-221.
35. Hunt, K. J., Valentine, M. D., Sobotka, A. K., et al.
(1978, July 27). A controlled trial of immunotherapy
in insect hypersensitivity. N Engl J Med, 299(4), 157-
161.
36. Golden, B. K., Moffitt, J., Nicklas, R. A., et al. (2011).
Stinging insect hypersensitivity: A practice parame-
ter update 2011. J Allergy Clin Immunol, 127, 852-
854.
37. Soldatova, L. N., Paupore, E. J., Burk, S. H., Pastor,
R. W., Slater, J. E. (2000). The stability of house dust
mite allergens in glycerinated extracts. J Allergy Clin
Immunol, 105, 482-488.
38. Grier, TJ. How’s my dosing? A one-step, math-free
guide for comparing your clinic’s maintenance
immunotherapy doses to current practice parameter
recommendations. Ann Allergy Asthma Immunol
108 (2012) 201-205

20
XII. APPENDICES
Appendix 1. Effective Dose Range for Allergen Extracts, US Standardized Units
Table IX. Probable effective dose range for standardized and non-standardized US-licensed allergen extracts
Allergenic extract
Labeled potency
or concentration
Probable effective
dose range
Range of estimated major allergen
content in US-licensed extracts
Dust mites: D farinae and
D pteronyssinus
3,000, 5,000, 10,000, and
30,000 AU/mL
500-2,000 AU 10,000 AU/mL
20-160 µg/Ml Der p 1, Der f 1*
2-180 µg/mL Der p 2, Der f 2*
78-206 µg./mL Der p 1, Der f 1†
13-147 µg/mL Der p 2, Der f 2†
Cat hair 5,000 and 10,000
BAU/mL
1,000-4,000 BAU 10,000 AU/mL
20-50 µg/mL Fel d 1*‡
30-100 µg/mL cat albumin§
Cat pelt 5,000-10,000 BAU/mL 1,000-4,000 BAU 10,000 BAU/mL
20-50 µg/mL Fel d 1 *‡
400-2,000 µg/mL cat albumin§
Grass, standardized 100,000 BAU/mL 1,000-4,000 BAU 100,000 BAU/mL
425-1,100 µg/mL Phl p 5*
506-2,346 µg/mL group 1||
Bermuda 10,000 BAU/mL 300-1,500 BAU 10,000 BAU/mL
141-422 Cyn d 1 µg/mL*
Short ragweed 1:10, 1:20 wt/vol,
100,000 AU/mL
6-12 µg of Amb a 1 or 1,000-
4,000 AU
1:10 wt/vol
300 µg/mL Amb a 1‡
Concentration of Amb a 1 is
on the label of wt/vol extracts
Nonstandardized
AP Dog
1:100 wt/vol 15 µg of Can f 1 80-400 µg/mL Can f 1†
10-20 µg/mL dog albumin¶
Nonstandardized extract,
dog
1:10 and 1:20 wt/vol 15 µg of Can f 1 0.5 to 10 µg/mL Can f 1†
<12-1,500 µg/mL dog albumin¶
Nonstandardized
extracts: pollen
1:10 to 1:40 wt/vol or
10,000-40,000 PNU/mL
0.5 mL of 1:100 or 1:200 wt/vol NA
Nonstandardized
extracts: mold/fungi,
cockroach
1:10 to 1:40 wt/vol or
10,000-40,000 PNU/mL
Highest tolerated dose NA
Hymenoptera venom 100 µg/mL single venom
300 µg/mL in mixed
vespid extract
50-200 µg of each venom 100-300 µg/mL of venom protein
Imported fire ant 1:10 to 1:20 wt/vol
whole-body extract
0.5 mL of a 1:100 wt/vol to 0.5
mL of a 1:10 wt/vol extract
NA
NA, Information not available.
ALK-Abelló ELISA.
†Indoor Biotechnology ELISA.
‡FDA radial immunodiffusion assay.
§Greer Radial Immunodiffusion assay.
||Greer ELISA.
¶Hollister-Stier ELISA using Innovative Research, Inc, reagents.

21
Appendix 2. Initial and Ongoing Competency Assessment: Allergen Extract Mixing
Extract Preparation Task Date Validated
by:
Comments, Notes, Additional Testing
Personnel Training documented
Passed initial and annual written test on aseptic
technique & extract preparation
Passed initial and annual Media-fill test verifying
aseptic technique
Successfully completed initial gloved fingertip
and thumb sampling 3 separate times and then
at least annually thereafter
Understands & demonstrates appropriate hand
hygiene
Understands and appropriately dons required
garb
Reviews prescriptions for accuracy
Checks expiration dating of antigens and diluents
Cleans mixing surface appropriately
Checks stocks & mixed extracts for turbidity/
particulate matter
Swabs vial stoppers with 70% IPA
Draws up appropriate amounts of extract
Disposes of syringes in an appropriate manner
Documents lot # and preparation details per
clinic SOP
Creates appropriate labels
Stores extracts at appropriate temperatures
Packages materials and supplies in a neat and
efficient manner.
I understand that of all the topics listed, I will be allowed to perform only those for my skill level/scope of practice and only after I
have demonstrated competency.
Employee Signature _____________________________________________ Date _________________________________

22
Appendix 3. Extract Volumes Needed for 5.0 ml Maintenance Vials with 0.5 ml injection volume (From Grier TJ. “How’s
my dosing? A one-step, math free guide for comparing your clinic’s maintenance immunotherapy doses to current
practice parameter recommendations” Ann Allergy Asthma Immunol 108 (2012) 201-205.
Extract/concentrate strength Volume of concentrate needed per vial (mL)
Category Concentrate Min Mid Max
Pollens, fungi, insects 1:10 w/v 0.25 0.375 0.50
1:20 w/v 0.50 0.75 1.00
1:40 w/v 1.00 1.50 2.00
Short ragweed
a
200 AgE U/mL 0.30 0.45 0.60
Cat 10,000 BAU/mL 1.00 2.50 4.00
Dog AP 1:100 w/v NA NA 1.00
Dog epithelia 1:10 w/v 0.25 0.375 0.50
1:20 w/v 0.50 0.75 1.00
Dust mites
b
30,000 AU/mL 0.17 0.42 0.67
10,000 AU/mL 0.50 1.25 2.00
Pasture grasses
b
100,000 BAU/mL 0.10 0.25 0.40
10,000 BAU/mL 1.00 2.50 4.00
Bermuda grass 10,000 BAU/mL 0.30 0.90 1.50
Abbreviations: w/v, weight-to-volume ratio; AgE. Antigen E or Amb a 1; U Unit; AU, Allergy Unit; BAU. Bioequivalent Allergy Unit;
NA. Not applicable.
Minimum recommended dose was not specified for this extract category.
ªAlso applies to ragweed mix (short + giant) products at 1:20 w/v and approx. 100AgE U/mL.
b
Also applies to dust mite mix and pasture grass mix (eg, KORT,7 grass) products at the same AU/mL or BAU/mL strengths.

23
Appendix 4. Recommended Documentation for Allergen Immunotherapy Extract Prescription Forms
The purpose of the allergen immunotherapy
prescription form is to define the contents of the
allergen immunotherapy extract in enough detail that it
could be precisely duplicated. The following information
should be on an immunotherapy prescription form:
Patient information:
• Patient name, patient number (if applicable), birth
date, telephone number, and picture (if available)
should be included.
Preparation information:
• Name of person and signature preparing the
allergen immunotherapy extract should be
included.
• Date of preparation should be recorded.
• Bottle name should be included (eg, trees and
grass). If abbreviations are used, a legend should
be included to describe the meaning of the
abbreviations.
Allergen immunotherapy extract content information:
The following information for each allergen should be
included on the form in a separate column:
• Content of the allergen immunotherapy extract,
including common name or genus and species of
individual antigens and detail of all mixes, should
be included..
• Concentration of available manufacturer’s extract.
• Volume of manufacturer’s extract add added to
achieve the projected effective concentration.
This can be calculated by dividing the projected
effective concentration by the concentration of
available manufacturer’s extract times the total
volume.
• The type of diluent (if used).
• Extract manufacturer.
• Lot number should be included.
• Expiration date should be recorded and not
exceed the expiration date of any of the individual
components.

24
Appendix 4. Allergen Immunology Extract Prescription Form*
Patient Name: Prescribing Physician:
Patient Number: Address:
Birth Date: Telephone:
Telephone: Fax:
Antigen
Number
Extract Name
Allergen or Diluent
(Common name of
Genus/species)**
Concentration and Type
Manufacturer’s Extract
(AU, BAU, W/V, PNU)/
(50%, G, Aq, Ly, AP)
Volume of
Manufacturer’s
Extract to Add
Extract
Manufacturer
Lot
Number
Expiration
Date
1
2
3
4
5
6
7
8
9
10
Diluent
Total
Volume
**Components of mixes listed on a separate sheet.
By Use Date ____________________________________________________________________________________________________________
Storage Requirements ___________________________________________________________________________________________________
Results of Quality Control (e.g. visual inspections, second verification of questions) _____________________________________________
Allergen Extract Name:
Bottle Name Abbreviations
Tree: T Mold: M
Grass: G Cat: C
Weed: W Dog: D
Ragweed: R Cockroach: CR
Mixture: Mx Dust Mite: Dm
Specific Instructions:
Prescribing Physician’s Signature Date
Volume to add = Maintenance Concentration x Total Volume
Conc. of Manufacturer’s Extract
Maintenance concentration and subsequent dilutions
reported as volume/volume (v/v) dilutions with maintenance
concentrations=1:1 v/v
BAU=Bioequivalent Allergy Unit, AU=Allergy Unit
PNY=Protein Nitrogen Unit
W/V=Weight per Volume Ratio
G=50% Glycerinated
Aq=Aqueous, Ly=Lyophilized
AP=Alum precipitated, AcP=Acetone precipitated
Maintenance Concentrate Prescription Form
Prepared by: ____________________________ Date Prepared: ___/___/___ Time: __________
Dates of subsequent dilutions from maintenance concentration with expirations dates:
Vial __________ From Vial __________ on ____/____/____ Expiration date: ____/____/____
Vial __________ From Vial __________ on ____/____/____ Expiration date: ____/____/____
Vial __________ From Vial __________ on ____/____/____ Expiration date: ____/____/____
Vial __________ From Vial __________ on ____/____/____ Expiration date: ____/____/____

25
USP Section 21 – Compounding Allergenic Extracts
*Final 2019 standards for allergen extract compounding under USP Chapter 797.
Allergenic extract prescription sets must follow
standards at least as stringent as those in this section:
Personnel Qualifications
• A designated person with training and expertise
in allergen immunotherapy is responsible for
ensuring that personnel who will be preparing
allergen immunotherapy are trained, evaluated and
supervised.
• Before beginning to independently prepare
allergenic extracts, all compounding personnel
must complete training and be able to
demonstrate knowledge of principles and skills for
sterile compounding.
• Annual personnel training and competency must
be documented. Personnel must demonstrate
proficiency in these procedures by passing written
or electronic testing before they can be allowed to
compound allergenic extract prescription sets.
• Before being allowed to independently compound,
all compounders must successfully complete
gloved fingertip and thumb sampling on both
hands (see USP Chapter <797>; Box 2-1 and Table
1), no fewer than 3 separate times. Each fingertip
and thumb evaluation must occur after performing
separate and complete hand hygiene and garbing
procedure. After the initial competency evaluation,
compounding personnel must successfully
complete gloved fingertip and thumb sampling at
least every 12 months thereafter.
• Compounding personnel must have their sterile
technique and related practices evaluated every 12
months as demonstrated by successful completion
of a media-fill test (see USP Chapter <797>; Box
2-2).
• Personnel who fail competency evaluations must
successfully pass reevaluations in the deficient
area(s) before they can resume compounding of
allergenic extract prescription sets. The designated
person(s) must identify the cause of failure and
determine appropriate retraining requirements.
• Personnel who have not compounded an
allergenic extract prescription set in more than 6
months must be evaluated in all core competencies
before resuming compounding duties.
Personnel Hygiene and Garbing
• Before beginning compounding of allergen
immunotherapy prescription sets, personnel must
perform hand hygiene (see USP Chapter <797>;
Box 3-1 and garbing procedure according to
facility SOPs.
• The Minimum garb requirements include:
° Low-lint garment with sleeves that fit snugly
around the wrists and that is enclosed at the neck
(e.g., gowns or coveralls).
° Low-lint, disposable covers for head that cover
the hair and ears and, if applicable, disposable
cover for facial hair.
° Face mask.
° Sterile powder-free gloves.
• Compounding personnel must rub sterile 70%
IPA onto all surfaces of the gloves and allow them
to dry thoroughly throughout the compounding
process.
Facilities
• The compounding process must occur in an ISO
Class 5 PEC or in a dedicated allergenic extract
compounding area (AECA). The PEC or AECA used
to compound prescription sets must be located
away from unsealed windows, doors that connect
to the outdoors, and traffic flow, all of which may
adversely affect the air quality. Neither a PEC nor
an AECA may be located where environmental
control challenges (e.g., restrooms, warehouses,
or food preparation areas) could negatively affect
the air quality. The PEC or the work surfaces in the
AECA must be located at least 1 meter away from a
sink. The impact of activities that will be conducted
around or adjacent to the PEC or AECA must be
considered carefully when designing such an area.
° If used, the PEC must be certified every 6 months
(see 5. Certification and Recertification).
° If used, a visible perimeter must establish the
boundaries of the AECA.
› Access to the AECA during compounding must
be restricted to authorized personnel.
› During compounding activities, no other activity
is permitted in the AECA.
Appendix 5. USP Section 21 — Compounding Allergenic Extracts

26
› The surfaces of walls, floors, fixtures, shelving,
counters, and cabinets in the AECA must be
cleanable.
› Carpet is not allowed in the AECA.
› Surfaces should be resistant to damage by
cleaning and sanitizing agents.
› The surfaces in the AECA upon which the
allergenic extract prescription sets are prepared
must be smooth, impervious, free from cracks
and crevices, and non-shedding to allow for
easy cleaning and disinfecting.
› Dust-collecting overhangs such as utility pipes,
ledges, and windowsills should be minimized. If
overhangs or ledges are present, they must be
easily cleanable.
› The AECA must be designed and controlled
to provide a well-lit working environment, with
temperature and humidity controls for the
comfort of compounding personnel wearing the
required garb.
Cleaning and Disinfecting
• In a PEC, all interior surfaces of the PEC must be
cleaned and disinfected daily and when surface
contamination is known or suspected. Apply sterile
70% IPA to the horizontal work surface between
each prescription set.
• In an AECA, all work surfaces in the AECA where
direct compounding is occurring must be
cleaned and disinfected daily and when surface
contamination is known or suspected. Apply sterile
70% IPA to the horizontal work surface between
each prescription set.
° If present, walls, doors, and door frames within
the perimeter of the AECA must be cleaned
and disinfected monthly and when surface
contamination is known or suspected.
° Ceilings within the perimeter of the AECA must
be cleaned and disinfected when visibly soiled
and when surface contamination is known or
suspected.
• Vial stoppers on packages of conventionally
manufactured sterile ingredients must be wiped
with sterile 70% IPA to ensure that the critical sites
are wet and allowed to dry before they are used to
compound allergenic extracts prescription sets.
Establishing BUDs
• The by-use-date (BUD) for the prescription set must
be no later than the earliest expiration date of any
allergenic extract or any diluent that is part of the
prescription set, and the BUD must not exceed 1
year from the date the prescription set is mixed or
diluted.
Labeling
• The label of each vial of an allergenic extract
prescription set must display the following
prominently and understandably:
° Patient name.
° Type and fractional dilution of each vial, with a
corresponding vial number.
° BUD.
° Storage conditions.
Shipping and Transport
• If shipping or transporting allergenic extract
prescriptions sets, compounding personnel must
select modes of transport that are expected to
deliver properly packed prescription sets in an
undamaged, sterile, and stable condition.
• When shipping or transporting allergen extract
prescriptions sets that require special handling,
personnel must include specific handling
instructions on the exterior of the container.
Documentation
• All facilities where allergenic extract prescription
sets are prepared must have and maintain written
or electronic documentation to include, but not
limited to the following:
° SOPs describing all aspects of the compounding
process.
° Personnel training records, competency
assessments, and qualification records including
corrective actions for any failures.
° Certification reports of the PEC, if used, including
corrective actions for any failures.
° Temperature logs for the refrigerator(s).
° Compounding records for individual allergenic
extract prescription sets (see USP Chapter
<797>; Box 21-1).
° Information related to complaints and adverse
events.
° Investigations and corrective actions.
*Adapted from USP General Chapter <797> Pharmaceutical
Compounding-Sterile Preparations; Section 21. Compounding
Allergenic Extracts
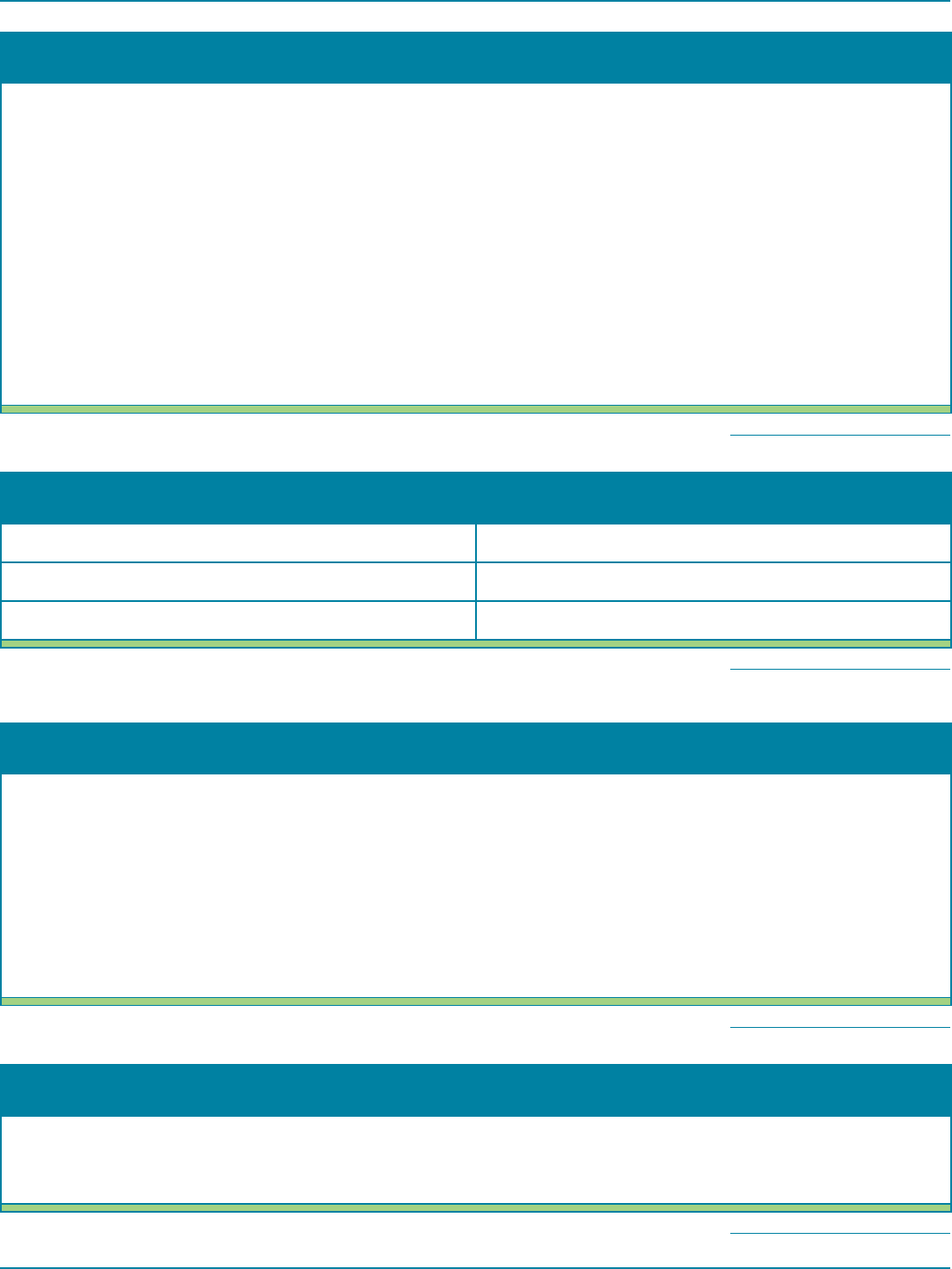
27
Box 2-1. Gloved Fingertip and Thumb Sampling Procedures
• Use one sampling device per hand (e.g., plates, paddles, or slides) containing general microbial growth agar [e.g.,
trypticase soy agar (TSA)] supplemented with neutralizing additives (e.g., lecithin and polysorbate 80) as the agar
supports both bacterial and fungal growth.
• Label each sampling device with a personnel identifier, whether it was from the right or left hand, and the date
and time of sampling.
• Do not apply sterile 70% isopropyl alcohol (IPA) to gloves immediately before touching the sampling device
because this could cause a false-negative result.
• Using a separate sampling device for each hand, collect samples from all gloved fingers and thumbs from both
hands by rolling finger pads and thumb pad over the agar surface.
• Incubate the sampling device at a temperature of 30°- 35°for no less than 48 hours and then at 20°- 25° for no
less than 5 additional days. Store media devices during incubation to prevent condensate from dropping onto the
agar and affecting the accuracy of the cfu reading (e.g., invert plates).
• Record the number of cfu per hand (left hand, right hand).
• Determine whether the cfu action level is exceeded by counting the total number of cfu from both hands.
Return to Allergy Standards
Table 1. Action Levels for Gloved Fingertip and Thumb Sampling
a
Gloved Fingertip and Thumb Sampling Action Levels (total number of cfu from both hands)
Initial sampling after garbing >0
Subsequent sampling after media-fill testing >3
a
Action levels are based on the total cfu count from both hands. Return to Allergy Standards
Box 2-2. Media-Fill Testing Procedures
• If all of the starting components are sterile to begin with, manipulate them in a manner that simulates sterile-to-
sterile compounding activities, and transfer the sterile soybean – Casein digest medium in non-bacteriostatic water
to make a 3% nonsterile solution. Manipulate it in a manner that simulates nonsterile-to-sterile compounding
activities. Prepare at least 1 container as the positive control to demonstrate growth promotion, which is indicated
by visible turbidity upon incubation.
• Once the compounding simulation is completed and the final containers are filled with the test media, incubate
them in an incubator for 7 days at 20°- 25° followed by 7 days at 30°- 35° to detect a broad spectrum of
microorganisms.
• Failure is indicated by visible turbidity or other visual manifestations of growth in the media in one or more
container-closure unit(s) on or before 14 days.
Return to Allergy Standards
Box 3-1. Hand Washing Procedures
• Remove visible debris from underneath fingernails under warm running water using a disposable nail cleaner.
• Wash hands and forearms up to the elbows with soap and water for at least 30 seconds.
• Dry hands and forearms to the elbows completely with low-lint disposable towels or wipers.
Return to Allergy Standards

28
Box 3-2. Hand Sanitizing Procedures
• Apply an alcohol-based hand rub to dry skin following the manufacturer’s instructions for the volume of product
to use.
• Apply product to one hand and rub hands together, covering all surfaces of hands and fingers, until hands are dry.
• Allow hands to dry thoroughly before conning sterile gloves.
Return to Allergy Standards
Box 21-1. Compounding Records for individual Allergenic Extract Prescription Sets
Compounding Records must include at least the following information:
• Name, concentration, volume, vendor or manufacturer, lot number, and expiration date for each component.
• Date and time of preparation of the allergenic extract.
• Assigned internal identification number.
• A method to identify the individuals involved in the compounding process and verifying the final CSP.
• Total quantity compounded.
• Assigned BUD and storage requirements.
• Results of QC procedures (e.g., visual inspection, second verification of quantities).
Return to Allergy Standards

29
Appendix 6. Forms
Competency Assessment — Initial Personnel Training: Allergen Extract Mixing..............................30
Competency Assessment — Annual Personnel Training: Allergen Extract Mixing ............................32
Competency Assessment — Aseptic Technique and Related Practices of Mixing Personnel ...................34
Competency Assessment — Hand Hygiene and Garbing Procedures ......................................36
Competency Assessment — Cleaning and Disinfecting Procedures .......................................38
Complaints/Adverse Effects . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40
Gloved Fingertip and Thumb Sampling ...............................................................41
Media-fill Testing Checklist ..........................................................................42
Primary Engineering Control (PEC) Hood .............................................................43
Refrigerator Temperature Log .......................................................................44

Competency Assessment –
Initial
Personnel Training: Allergen Extract Mixing
Name: Job Title:
Extract Preparation Task Date Validated by Comments, Notes, Additional Testing
1. Passed initial written test on aseptic technique and extract preparation. See Form A1.
2. Passed initial Media-fill test verifying aseptic technique. Attach lab report.
3. Successfully completed initial gloved fingertip and thumb sampling three separate
times. Attach lab report. TOTAL R cfu + L cfu = 0.
Test 1: R cfu + L cfu =
Test 2: R cfu + L cfu =
Test 3: R cfu + L cfu =
4. Understands & demonstrates appropriate hand hygiene. See Form A2.
5. Understands and appropriately dons required garb. See Form A2.
6. Reviews prescriptions for accuracy.
7. Checks expiration dates of antigens and diluents.
8. Cleans mixing surface appropriately. See Form A3.
9. Checks stocks & mixed extracts for turbidity/particulate matter.
10. Swabs vial stoppers with 70% IPA.
11. Draws up appropriate amounts of extract.
12. Disposes of syringes in an appropriate manner.
13. Documents lot # and preparation details per clinic SOP.
14. Creates appropriate labels.
15. Stores extracts at appropriate temperatures.
16. Packages materials and supplies in a neat and efficient manner.
I understand that of all the topics listed, I will be allowed to perform only those for my skill level/scope of practice and only after I have demonstrated
competency. Furthermore, I must successfully pass reevaluations in *deficient area(s) before I can resume compounding allergenic extract.
_______________________________________
Employee signature
_______________________________________
Date
college.acaai.org/extract ©2019 ACAAI
Self-Assessment: Evaluation/Validation Methodologies:
1 = Experienced T = Tests
2 = Needs practice/assistance D = Demonstration
3 = Never done V = Verbal
NA = Not applicable I = Interactive Class
*Corrective actions on separate page.

Competency Assessment – Corrective Action
Name: Job Title:
Extract Preparation Task Date Validated by Actions Taken
1. Passed written test on aseptic technique and extract preparation.
2. Passed Media-fill test verifying aseptic technique.
3. Successfully completed gloved fingertip and thumb sampling three separate times.
4. Understands & demonstrates appropriate hand hygiene.
5. Understands and appropriately dons required garb.*
6. Reviews prescriptions for accuracy.
7. Checks expiration dates of antigens and diluents.
8. Cleans mixing surface appropriately.
9. Checks stocks & mixed extracts for turbidity/particulate matter.
10. Swabs vial stoppers with 70% IPA.
11. Draws up appropriate amounts of extract.
12. Disposes of syringes in an appropriate manner.
13. Documents lot # and preparation details per clinic SOP.
14. Creates appropriate labels.
15. Stores extracts at appropriate temperatures.
16. Packages materials and supplies in a neat and efficient manner.
college.acaai.org/extract ©2019 ACAAI

Competency Assessment –
Annual
Personnel Training: Allergen Extract Mixing
Name: Job Title:
Extract Preparation Task Date Validated by Comments, Notes, Additional Testing
1. Passed annual written test on aseptic technique and extract preparation. See Form A1.
2. Passed annual Media-fill test verifying aseptic technique. Attach lab report.
3. Successfully completed annual gloved fingertip and thumb sampling three
separate times. Attach lab report. TOTAL R cfu + L cfu = 0.
Test 1: R cfu + L cfu =
4. Understands & demonstrates appropriate hand hygiene. See Form A2.
5. Understands and appropriately dons required garb. See Form A2.
6. Reviews prescriptions for accuracy.
7. Checks expiration dates of antigens and diluents.
8. Cleans mixing surface appropriately. See Form A3.
9. Checks stocks & mixed extracts for turbidity/particulate matter.
10. Swabs vial stoppers with 70% IPA.
11. Draws up appropriate amounts of extract.
12. Disposes of syringes in an appropriate manner.
13. Documents lot # and preparation details per clinic SOP.
14. Creates appropriate labels.
15. Stores extracts at appropriate temperatures.
16. Packages materials and supplies in a neat and efficient manner.
I understand that of all the topics listed, I will be allowed to perform only those for my skill level/scope of practice and only after I have demonstrated
competency. Furthermore, I must successfully pass reevaluations in *deficient area(s) before I can resume compounding allergenic extract.
_______________________________________
Employee signature
_______________________________________
Date
Self-Assessment: Evaluation/Validation Methodologies:
1 = Experienced T = Tests
2 = Needs practice/assistance D = Demonstration
3 = Never done V = Verbal
NA = Not applicable I = Interactive Class
*Corrective actions on separate page.
college.acaai.org/extract ©2019 ACAAI

Competency Assessment – Corrective Action
Name: Job Title:
Task Date Validated by Actions Taken
1. Passed annual written test on aseptic technique and extract preparation. See Form A1.
2. Passed annual Media-fill test verifying aseptic technique. Attach lab report.
3. Successfully completed annual gloved fingertip and thumb sampling three
separate times. Attach lab report. TOTAL R cfu + L cfu = 0.
4. Understands & demonstrates appropriate hand hygiene. See Form A2.
5. Understands and appropriately dons required garb. See Form A2.
6. Reviews prescriptions for accuracy.
7. Checks expiration dates of antigens and diluents.
8. Cleans mixing surface appropriately. See Form A3.
9. Checks stocks & mixed extracts for turbidity/particulate matter.
10. Swabs vial stoppers with 70% IPA.
11. Draws up appropriate amounts of extract.
12. Disposes of syringes in an appropriate manner.
13. Documents lot # and preparation details per clinic SOP.
14. Creates appropriate labels.
15. Stores extracts at appropriate temperatures.
16. Packages materials and supplies in a neat and efficient manner.
college.acaai.org/extract ©2019 ACAAI

Form A1: Competency Assessment – Aseptic Technique and Related Practices of Mixing Personnel
Name: Job Title:
Facility: Location:
All mixing personnel must perform media-fill testing to assess their sterile technique and related practices initially and every 12 months thereafter.
TASK (X = acceptable practice; N/A = not applicable; N/O = not observed) X N/A N/O
1. Completed hand hygiene and garbing competency assessment.
2. Performs proper hand hygiene, garbing and gloving procedures according to SOPs.
3. Disinfects work surfaces with sterile 70% IPA.
4. Disinfects components/vials with sterile 70% IPA.
5. Only introduces essential materials in a proper arrangement in work area.
6. Ensures syringes and needles are only opened in work area.
7. Does not expose critical sites to contact contamination.
8. Disinfects stoppers, injection ports and ampul necks by wiping with sterile 70% IPA and allows time to dry.
9. Affixes needles to syringes without contact contamination.
10. Punctures vial stoppers and spikes infusion ports without contact contamination.
11. Correctly prepares labels.
12. Disinfects sterile gloves routinely by wiping with sterile 70% IPA during prolonged mixing.
13. Disposes of sharps and waste according to institutional policy.
The person assessed is immediately informed of all unacceptable activities and informed of corrective actions.
_______________________________________ ____________________________________ _________________________
Signature of person assessed Printed name Date
_______________________________________ ____________________________________ _________________________
Signature of Qualified Evaluator Printed name Date
college.acaai.org/extract ©2019 ACAAI

Form A1: Competency Assessment – Corrective Action
Name: Job Title:
Task Date Validated by Actions Taken
1. Completed hand hygiene and garbing competency assessment.
2. Performs proper hand hygiene, garbing and gloving procedures according to SOPs.
3. Disinfects work surfaces with sterile 70% IPA.
4. Disinfects components/vials with sterile 70% IPA.
5. Only introduces essential materials in a proper arrangement in work area.
6. Ensures syringes and needles are only opened in work area.
7. Does not expose critical sites to contact contamination.
8. Disinfects stoppers, injection ports and ampul necks by wiping with sterile 70% IPA
and allows time to dry.
9. Affixes needles to syringes without contact contamination.
10. Punctures vial stoppers and spikes infusion ports without contact contamination.
11. Correctly prepares labels.
12. Disinfects sterile gloves routinely by wiping with sterile 70% IPA during
prolonged mixing.
13. Disposes of sharps and waste according to institutional policy.
college.acaai.org/extract
©2019 ACAAI

Form A2: Competency Assessment – Hand Hygiene and Garbing Practices
Name: Job Title:
Facility: Location:
Individuals entering a compounding area must take appropriate steps to minimize microbial contamination of the environment and the SCPs, including hand hygiene, garbing and consideration of
needed materials brought into the compounding area. Before entering a compounding area, individuals must remove any items that are not easily cleanable or that are not necessary for compounding.
TASK (X = acceptable practice; N/A = not applicable; N/O = not observed) X N/A N/O
Remove debris from underneath fingernails under running water using a disposable nail cleaner.
Wash hands and forearms up to the elbows with soap and water for at least 30 seconds.
Dry hands and forearms to the elbows completely with low-lint disposable towels or wipers.
The order of hand washing and garbing depends on the placement of the sink. The order of garbing must be determined by the facility and documented in the facility’s SOP. Hands must be
sanitized with alcohol-based hand rub before donning sterile gloves. Sterile gloves must be donned in a classified room or SCA.
Apply an alcohol-based hand rub to dry skin following the manufacturer’s instructions for the volume of product to use.
Apply product to one hand and rub hands together, covering all surfaces of hands and fingers, until hands are dry.
Allow hands to dry thoroughly before donning sterile gloves.
Dons appropriate size gloves; inspects to ensure a tight fit and that there are no defects, holes or tears – apply sterile 70% IPA to gloves – allow to dry
before compounding.
While compounding, routinely disinfects gloves with sterile 70% IPS after touching items or surfaces that may contaminate gloves .
Any person entering a compounding area must be properly garbed in accordance with the facility’s SOPs. Garb must be replaced immediately if it becomes visibly soiled or if its integrity is compromised.
Low-lint garment with sleeves that fit snugly around the wrists and that is enclosed at the neck (e.g., gowns or coveralls).
Low-lint, disposable covers for head that cover the hair and ears, and if applicable, disposable cover for facial hair.
Face mask.
Sterile powder-free gloves.
Compounding personnel must rub sterile 70% IPA onto all surfaces of the gloves and allow them to dry thoroughly throughout the compounding process.
Removes PPE on the clean side of the AECA.
Removes gloves and performs hand hygiene.
Removes and discards gown, mask, head cover and beard cover (if used).
The person assessed is immediately informed of all unacceptable activities and informed of corrective actions.
_______________________________________ ____________________________________ _________________________
Signature of person assessed Printed name Date
_______________________________________ ____________________________________ _________________________
Signature of Qualified Evaluator Printed name Date
college.acaai.org/extract ©2019 ACAAI

Form A2: Competency Assessment – Corrective Action
Name: Job Title:
Task Date Validated by Actions Taken
Remove debris from underneath fingernails under running water using a disposable
nail cleaner.
Wash hands and forearms up to the elbows with soap and water for at least 30
seconds.
Dry hands and forearms to the elbows completely with low-lint disposable towels or
wipers.
Apply an alcohol-based hand rub to dry skin following the manufacturer’s
instructions for the volume of product to use.
Apply product to one hand and rub hands together, covering all surfaces of hands
and fingers, until hands are dry.
Allow hands to dry thoroughly before donning sterile gloves.
Dons appropriate size gloves; inspects to ensure a tight fit and that there are
no defects, holes or tears – apply sterile 70% IPA to gloves – allow to dry before
compounding.
While compounding, routinely disinfects gloves with sterile 70% IPS after touching
items or surfaces that may contaminate gloves .
Low-lint garment with sleeves that fit snugly around the wrists and that is enclosed at
the neck (e.g., gowns or coveralls).
Low-lint, disposable covers for head that cover the hair and ears, and if applicable,
disposable cover for facial hair.
Face mask.
Sterile powder-free gloves.
Removes PPE on the clean side of the AECA.
Removes gloves and performs hand hygiene.
Removes and discards gown, mask, head cover and beard cover (if used).
college.acaai.org/extract ©2019 ACAAI

Form A3: Competency Assessment – Cleaning and Disinfecting Procedures
Name: Job Title:
Facility: Location:
DAILY TASKS (X = acceptable practice; N/A = not applicable; N/O = not observed) X N/A N/O
Follows garbing procedures when performing any cleaning activities.
In a PEC, all interior surfaces of the PEC must be cleaned and disinfected daily and when surface contamination is known or suspected. Apply sterile
70% IPA to the horizontal work surface between each prescription set.
In an AECA, all work surfaces in the AECA where direct mixing is occurring must be cleaned and disinfected daily and when surface contamination is
known or suspected. Apply sterile 70% IPA to the horizontal work surface between each prescription set.
Mops floors, starting at wall opposite the entrance; moves carts as needed to clean entire floor surface. Use of a microfiber cleaning system is an
acceptable alternative to mops.
MONTHLY TASKS
Follows garbing procedures when performing any cleaning activities
Performs monthly cleaning on a designated day.
If present, walls, doors and door frames within the perimeter of the AECA must be cleaned and disinfected monthly and when surface contamination is
known or suspected
Ceilings within the perimeter of the AECA must be cleaned and disinfected when visibly soiled and when surface contamination is known or suspected.
Documents all cleaning activities as to who performed such activities with date and time noted.
The person assessed is immediately informed of all unacceptable activities and informed of corrective actions.
_______________________________________ ____________________________________ _________________________
Signature of person assessed Printed name Date
_______________________________________ ____________________________________ _________________________
Signature of Qualified Evaluator Printed name Date
college.acaai.org/extract ©2019 ACAAI

Form A3: Competency Assessment – Corrective Action
Name: Job Title:
Task Date Validated by Actions Taken
Follows garbing procedures when performing any cleaning activities.
In a PEC, all interior surfaces of the PEC must be cleaned and disinfected daily and
when surface contamination is known or suspected. Apply sterile 70% IPA to the
horizontal work surface between each prescription set.
In an AECA, all work surfaces in the AECA where direct mixing is occurring must
be cleaned and disinfected daily and when surface contamination is known or
suspected. Apply sterile 70% IPA to the horizontal work surface between each
prescription set.
Mops floors, starting at wall opposite the entrance; moves carts as needed to clean
entire floor surface. Use of a microfiber cleaning system is an acceptable alternative
to mops.
Follows garbing procedures when performing any cleaning activities
Performs monthly cleaning on a designated day.
If present, walls, doors and door frames within the perimeter of the AECA must
be cleaned and disinfected monthly and when surface contamination is known or
suspected
Ceilings within the perimeter of the AECA must be cleaned and disinfected when
visibly soiled and when surface contamination is known or suspected.
Documents all cleaning activities as to who performed such activities with date and
time noted.
college.acaai.org/extract ©2019 ACAAI

Complaints/Adverse Events
Complainant/Adverse Event: Date:
Complaint received: Orally Written (attach)
Describe complaint/adverse event and any additional information:
Describe action taken and results:
Describe action taken to avoid same issue in the future:
_______________________________________ ____________________________________ _________________________
Signature Printed name Date
college.acaai.org/extract ©2019 ACAAI

Gloved Fingertip and Thumb Sampling
Name: Job Title:
Date: Time: Check Notes
Gather and prepare sampling plates – one plate per hand.
Label each sampling plate with a personnel identifier (i.e., initials); Right or Left hand.
DO NOT APPLY STERILE 70% ISOPROPYL ALCOHOL TO GLOVES IMMEDIATELY BEFORE
TOUCHING THE SAMPLING DEVICE, WHICH COULD CAUSE A FALSE-NEGATIVE RESULT.
Wipe the work surface with sterile 70% isopropyl alcohol; allow to dry.
Don garbing, including sterile gloves.
Using a separate sampling plate per hand, roll all finger pads & thumb pad over agar surface.
Cover and invert plates to prevent condensation from forming on agar; incubate at 30-
35°C for no less than 48 hours and then at 20-25°C for no less than five additional days.
Thumb Index Middle Ring Pinky
Record the number of cfu per Right hand.
Record the number of cfu per Left hand.
Attach report. TOTAL cfu
Action Levels for Gloved Fingertip and Thumb Sampling
a
Gloved Fingertip & Thumb Sampling. Action Levels (total cfu count from both hands)
Initial sampling after garbing. 0
Subsequent sampling after media-fill testing (every 6 months). ≤3
Successful completion of initial gloved fingertip and thumb sampling is defined as zero colony-forming units (cfu). Successful completion of subsequent gloved fingertip and
thumb sampling after media-fill testing is defined as ≤3 cfu (total from both hands).
a
Action levels are based on the total cfu count from both hands.
_______________________________________ ____________________________________ _________________________
Signature Printed name Date
college.acaai.org/extract ©2019 ACAAI

Media-fill Testing Checklist
Name: Media:
Date: Time: Manufacturer: Exp. Date: Lot #:
TASK Check Notes
Don garbing, including sterile gloves.
Wipe the work surface with sterile 70% isopropyl alcohol; allow to dry.
For sterile components (i.e., commercially sold media-fill kits) do not dilute the media
further, unless directed by manufacturer. Obtain certificate of analysis (COA). Using a
sterile syringe, transfer media to vial to simulate sterile-to-sterile compounding activities.
If non-sterile components are used, dissolve nonsterile soybean-casein digest powder in
non-bacteriostatic water to make a 3% nonsterile solution. (prepare one vial as a control to
demonstrate growth promotion) Using a sterile syringe, transfer media to vial and simulate
nonsterile to sterile compounding activities.
Once the compounding simulation is completed, incubate vials.
First incubate at 20-25°C for 7 days. Next incubate at 30-35°C for 7 additional days.
Starting Temp.: Date: Starting Temp.: Date:
Failure is indicated by visible turbidity or other visual growth in the media in one or more vials on or before 14 days.
_______________________________________ ____________________________________ _________________________
Observer Signature Printed name Date
_______________________________________ ____________________________________ _________________________
Person who Reads/Documents Results Printed name Date
college.acaai.org/extract ©2019 ACAAI

Primary Engineering Control (PEC) Hood
Name of Practice:
Location of PEC:
Date
Initial Certification Report Attached
6-Month recertification Report Attached
6-Month recertification Report Attached
6-Month recertification Report Attached
6-Month recertification Report Attached
6-Month recertification Report Attached
6-Month recertification Report Attached
_______________________________________ ____________________________________ _________________________
Signature Printed name Date
college.acaai.org/extract ©2019 ACAAI

Refrigerator Temperature Log
Refrigerator Name/Location:
Acceptable Temperature Range: 2-8°C
Date Time Temperature Initials
_______________________________________ ____________________________________ _________________________
Signature Printed name Date
college.acaai.org/extract ©2019 ACAAI
