
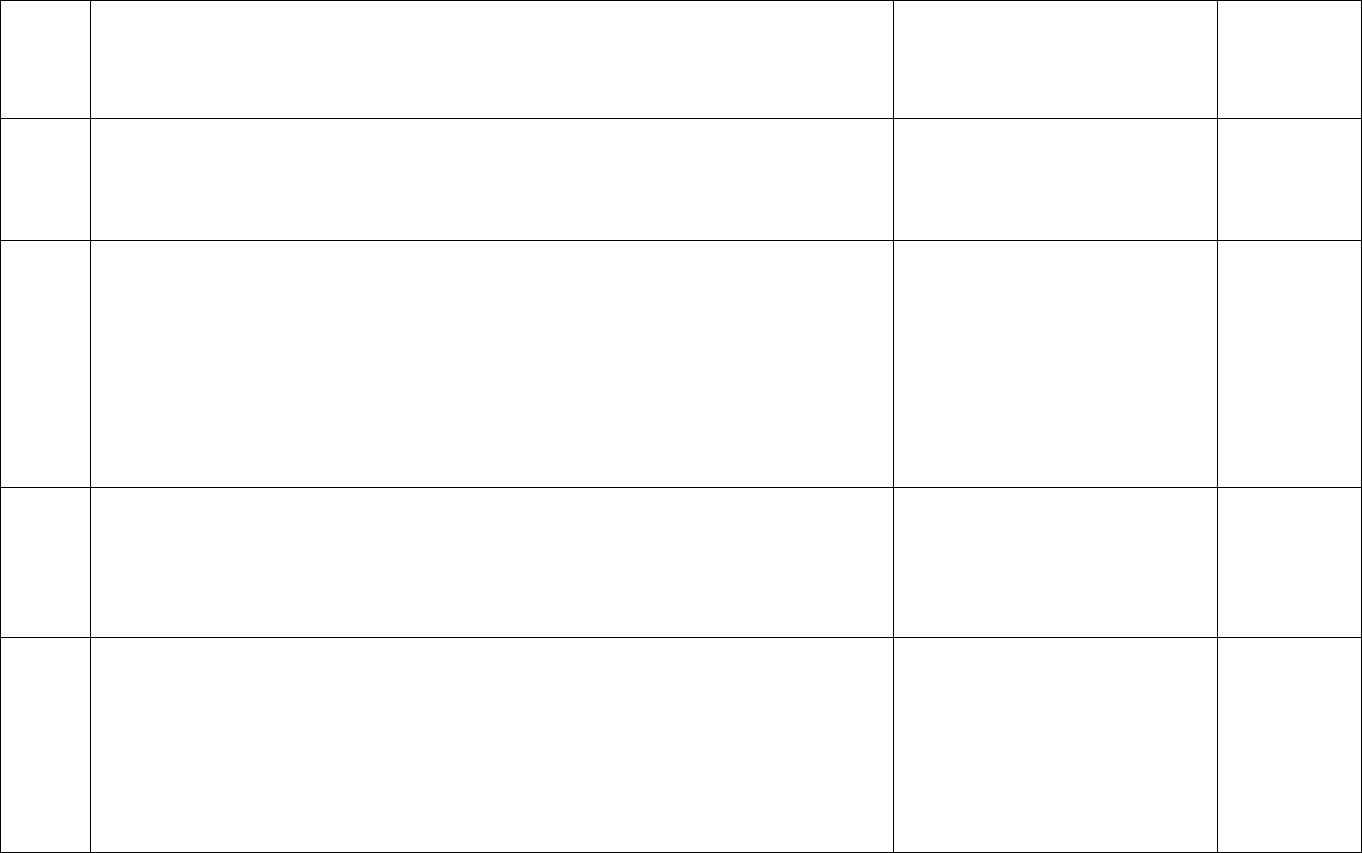
All CMS Provisions -- As of December 10, 2010
1
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
1001
(1of9)
Amendments to the Public Health Service Act -- 2711 -- No lifetime or annual limits –
Prohibits all loans from establishing lifetime or unreasonable annual limits on the
dollar value of benefits.
With respect to plan years beginning prior to January 1, 2014, a group health plan and
a health insurance issuer offering group or individual health insurance coverage may
only establish a restricted annual limit on the dollar value of benefits for any
participant or beneficiary with respect to the scope of benefits that are essential health
benefits as determined by the Secretary.
Requires plans to provide a summary of coverage to applicants and policyholders or
certificate holders, as well as to enrollees.
RB -- 2301 -- Insurance Reforms -- Extends the prohibition of lifetime limits and a
requirement to provide coverage for non‐dependent children up to age 26 to all
existing health insurance plans starting six months after enactment. For group health
plans, prohibits pre‐existing condition exclusions in 2014, restricts annual limits
beginning six months after enactment, and prohibits them starting in 2014.
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Preventive Services)
Guidance
6-22-10
5-10-10

All CMS Provisions -- As of December 10, 2010
2
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
1001
(2of9)
Amendments to the Public Health Service Act – 2712 --Prohibition on rescissions --
Prohibits all plans from rescinding coverage except in instances of fraud or
misrepresentation.
RB -- 2301 -- Insurance Reforms -- Extends the prohibition on rescissions and a
requirement to provide coverage for non‐dependent children up to age 26 to all
existing health insurance plans starting six months after enactment.
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Preventive Services)
Guidance
6-22-10
5-10-10
1001
(3of9)
Amendments to the Public Health Service Act -- 2713 -- Coverage of preventive health
services -- Requires all plans to cover preventive services and immunizations
recommended by the U.S. Preventive Services Task Force and the CDC, and certain
child preventive services recommended by the Health Resources and Services
Administration, without any cost-sharing.
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Preventive Services)
Guidance
7-14-10
5-10-10
1001
(4of9)
Amendments to the Public Health Service Act -- 2714 -- Extension of dependent
coverage -- Requires all plans offering dependent coverage to allow unmarried
individuals until age 26 to remain on their parents’ health insurance.
RB -- 1004 -- Income definitions -- Extends the exclusion from gross income for
employer provided health coverage for adult children up to age 26.
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Coverage Up to Age 26)
Guidance
5-10-10
5-10-10
1001
(5of9)
Amendments to the Public Health Service Act -- 2715 --Development and
utilization of uniform explanation of coverage documents and standardized
definitions -- Requires the Secretary to develop standards for use by health
insurers in compiling and providing an accurate summary of benefits and
explanation of coverage. The standards must be in a uniform format, using
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Coverage Up to Age 26)
5-10-10
5-10-10

All CMS Provisions -- As of December 10, 2010
3
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
language that is easily understood by the average enrollee, and must include
uniform definitions of standard insurance and medical terms. The explanation must
also describe any cost-sharing, exceptions, reductions, and limitations on coverage,
and examples to illustrate common benefits scenarios.
Guidance
1001
(6of9)
Amendments to the Public Health Service Act – 2716 -- Prohibition on discrimination
in favor of highly compensated individuals -- Employers that provide health coverage
will be prohibited from limiting eligibility for coverage based on the wages or salaries
of full-time employees. Also, prohibits the required collection of data from employees
(specifically gun ownership).
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Coverage Up to Age 26)
Guidance
5-10-10
5-10-10
1001
(7of9)
Amendments to the Public Health Service Act -- 2717 -- Ensuring quality of care --
Requires the Secretary to develop guidelines for use by health insurers to report
information on initiatives and programs that improve health outcomes through the
use of care coordination and chronic disease management, prevent hospital
readmissions and improve patient safety, and promote wellness and health.
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Preventive Services)
Guidance
7-14-10
5-10-10
1001
(8of9)
Amendments to the Public Health Service Act -- 2718 -- Bringing down the cost of
health care coverage -- Requires the Secretary promulgate regulations for
enforcing the provisions under this section. Health insurance companies will be
required to report publicly the ratio of the incurred loss (or incurred claims) plus
the loss adjustment expense (or change in contract reserves) to earned premiums
including the percentage of total premium revenue that is expended on clinical
services, and quality rather than administrative costs. Health insurance companies
will be required to refund each enrollee by the amount by which premium revenue
expended by the health insurer for non-claims costs exceeds 20 percent in the
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Coverage Up to Age 26)
Notice--Request for Information
on Medical Loss Ratio
5-10-10
4-12-10

All CMS Provisions -- As of December 10, 2010
4
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
group market and 25 percent in the individual market. The requirement to provide
a refund expires on December 31, 2013, but the requirement to report percentages
continues.
Require the Secretary make reports received under this section available to the
public on the HHS website.
1101
Immediate access to insurance for people with a preexisting condition -- Enacts a
temporary insurance program with financial assistance for those who have been
uninsured for several months and have a pre-existing condition. Ensures premium rate
limits for the newly insured population. Provides up to $5 billion for this program,
which terminates when the American Health Benefit Exchanges are operational in
2014. Also establishes a transition to the Exchanges for eligible individuals.
High Risk Pools; Interim Final
Rule
Guidance -- Letter to States
5-10-10
4-30-10
1102
Reinsurance for early retirees -- Establishes a temporary reinsurance program to
provide reimbursement to participating employment-based plans for part of the cost
of providing health benefits to retirees (age 55-64) and their families. The program
reimburses participating employment-based plans for 80 percent of the cost of
benefits provided per enrollee in excess of $15,000 and below $90,000. The plans are
required to use the funds to lower costs borne directly by participants and
beneficiaries, and the program incentivizes plans to implement programs and
procedures to better manage chronic conditions. The act appropriates $5 billion for
this fund and funds are available until expended.
Regulation -- Reinsurance
Program for Retirees Interim
Final Rule
05-04-10

All CMS Provisions -- As of December 10, 2010
5
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
1003
Ensuring that consumers get value for their dollars -- For plan years beginning in 2010,
the Secretary and States will establish a process for the annual review of increases in
premiums for health insurance coverage. Requires States to make recommendations to
their Exchanges about whether health insurance issuers should be excluded from
participation in the Exchanges based on unjustified premium increases. Provides $250
million in funding to States from 2010 until 2014 to assist States in reviewing and, if
appropriate under State law, approving premium increases for health insurance
coverage and in providing information and recommendations to the Secretary.
Regulation -- Omnibus Health
Insurance Market Interim Final
Rule(Part 1)
Notice--Request for Information
on Premium Rate Review
Guidance
5-10-10
4-30-10
4-30-10
1103
Immediate information that allows consumers to identify affordable coverage
options -- Establishes an Internet portal for beneficiaries to easily access affordable
and comprehensive coverage options. This information will include eligibility,
availability, premium rates, cost sharing, and the percentage of total premium
revenues spent on health care, rather than administrative expenses, by the issuer
[(including Medicaid) in the State shall be available to small businesses and shall
contain information on coverage options.]
Clarifies that reinsurance for early retirees applies to plans sponsored by State and
local governments for their employees.
Creation of Website
Regulation -- Web Portal for
Private Plan and Medicaid/CHIP
Data Interim Final Rule with
Comment
7-1-10
4-30-10
1201
(4of8)
Amendment to the Public Health Service Act -- Sec. 2704 -- Prohibition of preexisting
condition exclusions or other discrimination based on health status -- No group health
plan or insurer offering group or individual coverage may impose any pre-existing
condition exclusion or discriminate against those who have been sick in the past.
Regulation- Omnibus Health
Insurance Market Interim Final
Rule (Part1)
Guidance
5-10-10
5-10-10

All CMS Provisions -- As of December 10, 2010
6
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
1201
(5of8)
Amendment to the Public Health Service Act -- Sec. 2705 -- Prohibiting discrimination
against individual participants and beneficiaries based on health status -- No group
health plan or insurer offering group or individual coverage may set eligibility rules
based on health status, medical condition, claims experience, receipt of health care,
medical history, genetic information, evidence of insurability – including acts of
domestic violence or disability. Permits employers to vary insurance premiums by as
much as 30 percent for employee participation in certain health promotion and disease
prevention programs. Authorizes a 10-State demonstration to apply such a program in
the individual market.
Regulation- Omnibus Health
Insurance Market Interim Final
Rule (Part 1)
Guidance
5-10-10
5-10-10
1251
Preservation of right to maintain existing coverage -- Allows any individual enrolled in
any form of health insurance to maintain their coverage as it existed on the date of
enactment.
Regulation- Omnibus Health
Insurance Market Interim Final
Rule (Part 2)
6-14-10
1303
Special rules -- Voluntary Choice of Coverage of Abortion Services -- 10104 -- Affirms that
States may prohibit abortion coverage in qualified health plans offered through an Exchange in
such State if such State enacts a law to provide for such prohibition.
Allows plans to elect whether or not to cover abortion. Requires a segregation of funds for
subsidy-eligible individuals in plans that cover abortions for which the expenditure of Federal
funds appropriated for HHS is not permitted. Subsidy-eligible individuals would make two
payments, with one going to an allocation account to be used exclusively for payment of such
services. Requires State insurance commissioners to ensure compliance with the requirement
to segregate federal funds in accordance with generally accepted accounting requirements and
guidance from OMB and GAO. Plans would be required to include in their benefit descriptions
whether or not they cover abortion, as they will do for all other benefits. Replaces provider
conscience protections with new conscience language that would prohibit qualified health plans
Regulation-Omnibus Health
Insurance Market Interim Final
Rule (Part1)
Guidance
5-10-10
5-10-10

All CMS Provisions -- As of December 10, 2010
7
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
from discriminating against any individual health care provider or health care facility because of
its unwillingness to provide, pay for, provide coverage of, or refer for abortions. Federal and
State laws regarding abortion are not preempted.
2001
(2of3)
Medicaid coverage for the lowest income populations -- Eligibility --Eligible
individuals include: all non-elderly, non-pregnant individuals who are not entitled to
Medicare (e.g., childless adults and certain parents). Creates a new mandatory
Medicaid eligibility category for all such “newly-eligible” individuals with income at or
below 133 percent of the Federal Poverty Level (FPL) beginning January 1, 2014. Also,
as of January 1, 2014, the mandatory Medicaid income eligibility level for children ages
six to 19 changes from 100 percent FPL to 133 percent FPL. States have the option to
provide Medicaid coverage to all non-elderly individuals above 133 percent of FPL
through a State plan amendment.
SMD Letter
SMD Letter
Enhanced Funding Proposed Rule
(CMS-2346-P)
04/09/2010
7/2/2010
11/18/10
2302
Concurrent care for children -- Allows children who are enrolled in either Medicaid
or CHIP to receive hospice services without foregoing curative treatment related to
a terminal illness.
SMD Letter
09/09/2010
2303
(1of2)
State eligibility option for family planning services -- Adds a new optional
categorically-needy eligibility group to Medicaid comprised of (1) non-pregnant
individuals with income up to the highest level applicable to pregnant women
covered under Medicaid or CHIP, and (2) individuals eligible under the standards
and processes of existing section 1115 waivers that provide family planning
services and supplies. Benefits would be limited to family planning services and
supplies, including related medical diagnostic and treatment services.
SMD Letter
SMD Letter
07/2/2010
7/2/2010

All CMS Provisions -- As of December 10, 2010
8
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
2402
(2of2)
Removal of barriers to providing home and community-based services -- Removes
barriers to providing HCBS by giving States the option to provide more types of
HCBS through a State plan amendment to individuals with higher levels of need,
rather than through a waiver, and to extend full Medicaid benefits to individuals
receiving HCBS under a State plan amendment.
SMD Letter
08/6/2010
2403
Money Follows the Person Rebalancing Demonstration -- Extends the Money
Follows the Person Rebalancing Demonstration through September 30, 2016 and
changes the eligibility rules for individuals to participate in the demonstration
project by requiring that individuals reside in an inpatient facility for not less than
90 consecutive days.
SMD Letter
Issue Grant Solicitations
Award Planning Grant
6/22/2010
7/26/2010
9/28/2010
2501
(1of2)
Prescription drug rebates -- The flat rebate for single source and innovator
multiple source outpatient prescription drugs would increase from 15.1 percent to
23.1 percent, except the rebate for clotting factors and outpatient drugs approved
by the Food and Drug Administration exclusively for pediatric indications would
increase to 17.1 percent. The basic rebate percentage for multi-source, non-
innovator drugs would increase from 11 percent to 13 percent. Drug
manufacturers would also be required to pay rebates for drugs dispensed to
Medicaid beneficiaries who receive care from a Medicaid managed care
organization (MCO). Total rebate liability would be limited to 100 percent of the
average manufacturer price (AMP). Additional revenue generated by these
increases will be remitted to the federal government.
SMD Letter
04/22/2010
2501
Prescription drug rebates -- RB -- 1206 -- Drug rebates for new formulations of
existing drugs -- For purposes of applying the additional rebate, narrows the
SMD Letter
04/22/2010

All CMS Provisions -- As of December 10, 2010
9
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
(2of2)
definition of a new formulation of a drug to a line extension of a single source or
innovator multiple source drug that is an oral solid dosage form of the drug.
2902
Elimination of sunset for reimbursement for all Medicare Part B services
furnished by certain Indian hospitals and clinics -- Removes the sunset provision,
allowing IHS and I/T/U services to continue to be reimbursed by Medicare Part B.
Guidance -- JSM
Federal Register Notice --
Updates to the OPPS and ASC
Payment system Resulting from
2010 HCR provisions
3/29/2010
7/2/2010
3002
(1of4)
Improvements to the physician quality reporting initiative -- Extends through
2014 payments under the PQRI program, which provide incentives to physicians
who report quality data to Medicare. Creates appeals and feedback processes for
participating professionals in PQRI. Establishes a participation pathway for
physicians completing a qualified Maintenance of Certification program with their
specialty board of medicine.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
Guidance – Change Request
06/25/2010
11/2/2010
11/2/2010
3002
(3of4)
Improvements to the physician quality reporting initiative -- Requires the
Secretary establish and have in place an informal process for eligible professionals
to seek a review of the determination that an eligible professional did not
satisfactorily submit data on quality measures.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
Guidance – Change Request
06/25/2010
11/2/2010
11/2/2010

All CMS Provisions -- As of December 10, 2010
10
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3003
Improvements to the physician feedback program – 1. Expands Medicare’s
physician resource use feedback program to provide for development of
individualized reports by 2012. Reports will compare utilization of physicians (or
groups of physicians) to other physicians who see similar patients. Reports will be
risk-adjusted and standardized to take into account local health care costs.
2. Develop a public domain episode grouper NLT 1/1/2012
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
3027
Extension of gainsharing demonstration -- The Deficit Reduction Act of 2005
authorized a demonstration to evaluate arrangements between hospitals and
physicians designed to improve the quality and efficiency of care provided to
beneficiaries. This provision would extend the demonstration through September
30, 2011 and extend the date for the final report to Congress on the
demonstration to September 30, 2012. It would also authorize an additional $1.6
million in FY2010 for carrying out the demonstration.
Contract modification
05-01-10
3102
(1of3)
Extension of the work geographic index floor and revisions to the practice
expense geographic adjustment under the Medicare physician fee schedule --
Extends a floor on geographic adjustments to the work portion of the fee schedule
through the end of 2010, with the effect of increasing practitioner fees in rural
areas.
RB -- 1108 -- PE GPCI ADJUSTMENT FOR 2010 -- Requires that for services
furnished during 2010, the employee wage and rent portions of the practice
expense geographic index reflect 1/2 of the difference between the relative costs
Guidance – Change Request
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
5/10/010
06/25/2010
11/2/2010

All CMS Provisions -- As of December 10, 2010
11
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
of employee wages and rents in each of the different fee schedule areas and the
national average of such employee wages and rents.
3102
(2of3)
Extension of the work geographic index floor and revisions to the practice
expense geographic adjustment under the Medicare physician fee schedule --
Provides immediate relief to areas negatively impacted by the geographic
adjustment for practice expenses, and requires the Secretary of HHS to improve
the methodology for calculating practice expense adjustments beginning in 2012.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
3102
(3of3)
Extension of the work geographic index floor and revisions to the practice
expense geographic adjustment under the Medicare physician fee schedule --
10324 -- Protections for frontier states – Provides that for purposes of payment for
services furnished in a frontier State on or after January 1, 2011, after calculating
the practice expense index the Secretary is required to increase any such index to
1.00 if such index would otherwise be less that 1.00.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
3103
Extension of exceptions process for Medicare therapy caps -- Extends the process
allowing exceptions to limitations on medically necessary therapy until December
31, 2010.
Guidance – Change Request /JSM
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
03/29/2010
06/25/2010
11/2/2010

All CMS Provisions -- As of December 10, 2010
12
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3104
Extension of payment for technical component of certain physician pathology
services -- Extends a provision that directly reimburses qualified rural hospitals for
certain clinical laboratory services through the end of 2010.
Guidance -- JSM
Guidance -- Change request
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
03/29/2010
4/9/2010
06/25/2010
11/2/2010
3105
Extension of ambulance add-ons -- Extends bonus payments made by Medicare for
ground and air ambulance services in rural and other areas 1-1-11.
Guidance -- JSM
Guidance -- Change request
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
03/29/2010
4/9/2010
06/25/2010
11/2/2010
3106
Extension of certain payment rules for long-term care hospital services and of
moratorium on the establishment of certain hospitals and facilities -- Extends
Sections 114 (c) and (d) of the Medicare, Medicaid and SCHIP Extension Act of 2007
by two years.
Federal Register Notice --
Changes to the IPPS Resulting
from 2010 HCR Provisions
Regulation – IPPS Final Rule
05/21/10
07/30/2010

All CMS Provisions -- As of December 10, 2010
13
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
10312-- amd'd
3107
Extension of physician fee schedule mental health add-on -- Increases the
payment rate for psychiatric services by 5 percent for two years, through the end
of 2010.
Guidance -- Change request
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
5/10/2010
6/25/2010
11/2/2010
3108
Permitting physician assistants to order post-hospital extended care services --
Authorizes clinical nurses or physician assistants to order skilled nursing care
services in the Medicare program beginning in 2011.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
6/25/2010
11/2/2010
3109
Exemption of certain pharmacies from accreditation requirements -- Allows
pharmacies which meet certain criteria, including having less than 5 percent of
revenues from Medicare DMEPOS billings for the past 3 years, to be exempt from
accreditation requirements until the Secretary of HHS develops pharmacy-specific
standards.
Fact Sheet
Guidance -- Change Request
7/7/2010
6/25/2010

All CMS Provisions -- As of December 10, 2010
14
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3111
(1of2)
Payment for bone density tests -- Restores payment for dual-energy x-ray
absorptiometry (DXA) services furnished during 2010 and 2011 to 70 percent of the
Medicare rate paid in 2006.
Guidance -- Change Request
Guidance -- Change Request
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
5/10/2010
5/28/10
06/25/2010
11/2/2010
3112
Revision to the Medicare Improvement Fund-- Eliminates the remaining funds in
the Medicare Improvement Fund.
Self-Implementing
N/A
3114
Improved access for certified nurse-midwife services -- Increases the payment
rate for certified nurse midwives for covered services from 65 percent of the rate
that would be paid were a physician performing a service to the full rate.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
3121
Extension of outpatient hold harmless provision -- Extends the existing outpatient
hold harmless provision through the end of FY2010 and would allow Sole
Community Hospitals with more than 100 beds to also be eligible to receive this
adjustment through the end of FY2010.
Guidance – JSM
Regulation – OPPS Proposed Rule
Regulation – OPPS Final Rule
03/31/2010
07/2/2010
11/2/2010

All CMS Provisions -- As of December 10, 2010
15
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3122
Extension of Reasonable Cost Payment for Clinical Lab Tests Furnished to
Hospitals Patients in Certain Rural Areas -- Re-institutes reasonable cost payment
for clinical lab tests performed by hospitals with fewer than 50 beds in qualified
rural areas as part of their outpatient services for cost reporting periods beginning
on or after July 1, 2010, through June 30, 2011. This could affect services
performed as late as June 30, 2012.
Guidance – JSM
Guidance – Change Request
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
03/29/2010
4/2/2010
06/25/2010
11/2/2010
3123
Extension of the Rural Community Hospital Demonstration Program -- Extends
the program for five years and expands eligible sites to additional States and
additional rural hospitals.
Sec. 10313 -- Revisions to the extension for the Rural Community Hospital
demonstration program -- Makes adjustments to payment levels provided within
the demonstration program.
Regulation –Changes to the IPPS
Resulting from 2011 HCR Proposed
Rule
Regulation – IPPS Final Rule
05/21/2010
07/30/2010
3124
Extension of the Medicare-dependent hospital (MDH) program -- Extends the
Medicare-dependent hospital program by one year through October 1, 2012. It
would also require HHS to study whether certain urban hospitals should qualify for
the MDH program.
Regulation –Changes to the IPPS
Resulting from 2011 HCR Proposed
Rule
Regulation – IPPS Final Rule
05/21/2010
07/30/2010

All CMS Provisions -- As of December 10, 2010
16
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3124
Extension of the Medicare-dependent hospital (MDH) program -- Extends the
Medicare-dependent hospital program by one year through October 1, 2012. It
would also require HHS to study whether certain urban hospitals should qualify for
the MDH program.
Regulation –Changes to the IPPS
Resulting from 2011 HCR Proposed
Rule
Regulation – IPPS Final Rule
05/21/2010
07/30/2010
3125
Temporary improvements to the Medicare inpatient hospital payment
adjustment for low-volume hospitals -- Expands the program providing a
temporary adjustment to inpatient hospital payments for certain low-volume
hospitals through FY2012 and would modify eligibility requirements regarding
distance from another facility and number of eligible discharges.
Sec. 10314 -- Adjustment to low-volume hospital provision -- Increases threshold
for eligible hospitals from 1,500 Medicare Part A discharges per year to 1,600 per
year.
Regulation –Changes to the IPPS
Resulting from 2011 HCR Proposed
Rule
Regulation – IPPS Final Rule
05/21/2010
07/30/2010
3128
Technical correction related to critical access hospital services -- Clarifies that
CAHs can continue to be eligible to receive 101 percent of reasonable costs for
providing outpatient care regardless of eligible billing method the facility uses and
for providing qualifying ambulance services. (as if included in MMA of 2003)
Regulation –Changes to the IPPS
Resulting from 2011 HCR Proposed
Rule
Regulation – IPPS Final Rule
05/21/2010
07/30/2010

All CMS Provisions -- As of December 10, 2010
17
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3131
(2of7)
Payment adjustments for home health care -- Establishes a 10 percent cap on the
amount of reimbursement a home health provider can receive from outlier
payments and would reinstate an add-on payment for rural home health providers
from April 1, 2010 through 2015.
Guidance – Change Request
Regulation – HHA Proposed Rule
Regulation – HHA Final Rule
03/31/2010
7/16/2010
11/2/2010
3131
(7of7)
Payment adjustments for home health care -- Reinstate an add-on payment for
rural home health providers from April 1, 2010 through 2015
Guidance -- JSM
Guidance -- Change Request
04/08/2010
04/23/2010
3132
(3of3)
Hospice reform - Requires a hospice physician or nurse practitioner to have a face-
to-face encounter with the individual to determine continued eligibility for
hospice care prior to the 180th day recertification and each subsequent
recertification and attests that such visit took place as established by the Secretary.
Regulation – Home Health PPS
Proposed Rule
Regulation – HHA Final Rule
7/16/2010
11/2/2010
3134
Misvalued codes under the physician fee schedule -- Directs the Secretary to
regularly review fee schedule rates for physician services paid for by Medicare,
including services that have experienced high growth rates. Strengthens the
Secretary’s authority to adjust fee schedule rates that are found to be misvalued or
inaccurate.
Eliminates the Practicing Physicians Advisory Council (PPAC).
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010

All CMS Provisions -- As of December 10, 2010
18
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3135
(1of3)
Modification of equipment utilization factor for advanced imaging services -- RB -
- 1107 -- Payment for Imaging Services -- Sets the assumed utilization rate at 75
percent for the practice expense portion of advanced diagnostic imaging services.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
3135
(2of3)
Modification of equipment utilization factor for advanced imaging services --
Adjusts the technical component discount on single session imaging studies on
contiguous body parts from 25 percent to 50 percent.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
3136
Revision of payment for power-driven wheelchairs -- Eliminates the option for
Medicare to purchase power-driven wheelchairs with a lump-sum payment at the
time the chair is supplied. Medicare would continue to make the same payments
for power-driven chairs over a 13-month period. Purchase option for complex
rehabilitative power wheelchairs would be maintained.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
3137
(1of3)
Hospital wage index improvement -- Extends reclassifications under section 508 of
the Medicare Modernization Act (P.L 108-173) through the end of FY2011. Also
directs the Secretary to restore the average hourly wage comparison thresholds
used to determine hospital reclassifications to the percentages used as of
September 30, 2008.
Guidance -- JSM
Guidance – Change Request
Regulation –Changes to the IPPS
Resulting from 2011 HCR
Proposed Rule
Regulation – IPPS Final Rule
4/22/2010
7/10/2010
05/21/2010
07/30/2010

All CMS Provisions -- As of December 10, 2010
19
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3137
(2of3)
Hospital wage index improvement -- Sec. 10317-- Revisions to extension of
Section 508 hospital provisions -- Clarifies the Secretary may only use wage data of
certain eligible hospitals in carrying out this provision if doing so does not result in
lower wage index adjustments for affected facilities.
Guidance – JSM
Regulation – IPPS Proposed Rule
Regulation – IPPS Final Rule
4/22/2010
04/19/2010
07/30/2010
3138
Treatment of certain cancer hospitals -- Directs the Secretary to study whether
existing cancer hospitals that are exempt from the inpatient prospective payment
system have costs under the outpatient prospective payment system (OPPS) that
exceed costs of other hospitals, and to make an appropriate payment adjustment
under OPPS based on that analysis.
10324 -- Protections for frontier states -- With respect to covered OPD services
furnished on or after January 1, 2011, the area wage adjustment factor applicable
under the payment system established under this subsection to any hospital
outpatient department which is located in a frontier State may not be less than
1.00.
Regulation – OPPS Proposed
Rule
Regulation – OPPS Final Rule
07/2/2010
11/2/2010
3139
Payment for biosimilar biological products -- Sets the add-on payment rate for
biosimilar products reimbursement under Medicare Part B at 6 percent of the
average sales price of the brand biological product.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
3141
Application of budget neutrality on a national basis in the calculation of the
Federal Register Notice --
Changes to the IPPS Resulting
05/21/2010

All CMS Provisions -- As of December 10, 2010
20
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
Medicare hospital wage index floor -- Starting on October 1, 2010, the provision
would require application of budget neutrality associated with the effect of the
imputed rural and rural floor to be applied on a national, rather than State-specific
basis through a uniform, national adjustment to the area wage index.
from 2010 HCR Provisions
Regulation – IPPS Final Rule
07/30/2010
3201
(1of2)
Medicare Advantage payment -- RB -- 1102 -- Medicare Advantage payments --
Freezes Medicare Advantage payments in 2011. Benchmarks will vary from 95% of
Medicare spending in high‐ cost areas to 115% of Medicare spending in low‐cost
areas. The changes will be phased‐in over 3, 5 or 7 years, depending on the level of
payment reductions.
2011 Call Letter
Regulation – Revisions to the
Parts C & D Contract Years
2012 Proposed Rule
04-05-10
11-10-10
3301
(1of3)
Medicare coverage gap discount program -- Requires drug manufacturers to
provide a 50 percent discount to Part D beneficiaries for brand-name drugs and
biologics purchased during the coverage gap beginning January 1, 2011.
Guidance -- HPMS
Federal Register Notice
Regulation – Revisions to the
Parts C & D Contract Years
2012 Proposed Rule
4/30/2010
05/21/2010
11-10-10
3301
(2of3)
Medicare coverage gap discount program -- Requires the Secretary establish a
model agreement for use under the program in consultation with manufacturers
and allow for comment on such model agreement.
Federal Register Notice
05-21-10

All CMS Provisions -- As of December 10, 2010
21
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
3401
(1of3)
Revision of certain market basket updates and incorporation of productivity
improvements into market basket updates that do not include such improvements --
Incorporates a productivity adjustment into the market basket update for inpatient
hospitals, home health providers, skilled nursing facilities, hospice providers, inpatient
psychiatric facilities, long-term care hospitals and inpatient rehabilitation facilities
beginning in various years and implements additional market basket reductions for certain
providers. It would also incorporate a productivity adjustment into payment updates for
Part B providers who do not already have such an adjustment.
Sec. 10319 -- Revisions to market basket adjustments -- Modifies market adjustments for
inpatient hospitals, inpatient rehabilitation facilities, inpatient psychiatric hospitals and
outpatient hospitals in 2012 and 2013 and for long-term care hospitals in 2011, 2012 and
2013. Also, modifies market basket adjustments for home health providers in 2013 and
hospice providers in 2013 through 2019.
RB -- 1105 -- Market basket updates-- Revises the hospital market basket reduction that is
in addition to the productivity adjustment as follows: ‐0.3 in FY14 and ‐0.75 in FY17, FY18
and FY19. Removes Senate provision that eliminates the additional market basket for
hospitals based on coverage levels. Providers affected are inpatient hospitals, long‐term
care hospitals, inpatient rehabilitation facilities, psychiatric hospitals and outpatient
hospitals.
Guidance -- JSM (IRF,SNF,IPPS,
LTCH, OPPS, HH,)
Guidance -- JSM (IPPS, LTCH)
Regulation – IPPS Proposed Rules
Regulation – PFS and OPPS
Proposed Rule
Federal Register Notice –
Changes to the OPPS/ASC
Resulting from 2010 HCR
Provisions
Regulation – HH Proposed Rule
Regulation – IPPS Final Rules
Psych PPS Notice
Regulation – PFS and OPPS Final
Rule
Regulation – HH Final Rule
4/1/2010
4/14/2010
04/19/2010
6/25/2010
7/2/2010
7/16/2010
07/30/2010
5/1/2010
11/2/2010
11/2/10
4103
(1of4)
Medicare coverage of annual wellness visit providing a personalized prevention
plan -- Provides coverage under Medicare, with no co-payment or deductible, for
Regulation -- Physician Fee
Schedule Proposed Rule
06/25/2010

All CMS Provisions -- As of December 10, 2010
22
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
an annual wellness visit and personalized prevention plan services. Such services
would include a comprehensive health risk assessment. The personalized
prevention plan would take into account the findings of the health risk assessment
and include elements such as: a five- to ten-year screening schedule; a list of
identified risk factors and conditions and a strategy to address them; health advice
and referral to education and preventive counseling community-based
interventions to address modifiable risk factors such as physical activity, smoking,
and nutrition.
Regulation – Physician Fee
Schedule Final Rule
11/2/2010
4103
(2of4)
Medicare coverage of annual wellness visit providing a personalized prevention
plan -- Requires the Secretary establish publicly available guidelines for health risk
assessments.
Requires the Secretary establish standards for interactive telephonic or webbased
programs used to furnish health risk assessments.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
4104
Removal of barriers to preventive services in Medicare -- This section would waive
beneficiary coinsurance requirements for most preventive services, requiring
Medicare to cover 100 percent of the costs. Services for which no coinsurance or
deductible would be required are the personalized prevention plan services and
any covered preventive service if it is recommended with a grade of A or B by the
U.S. Preventive Services Task Force.
Sec. 10406 -- Amendment relating to waiving coinsurance for preventive services
– Clarifies that Medicare beneficiaries do not have to pay coinsurance (including
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
Guidance – Change Request
Regulation – Revisions to the
Parts C & D Contract Year
06/25/2010
11/2/2010
11/2/2010
11/10/10

All CMS Provisions -- As of December 10, 2010
23
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
co-pays and deductibles) for preventive services delivered in all settings.
2012 Proposed Rule
4105
(2of3)
Evidence-based coverage of preventive services in Medicare -- 10501 - (3)(A) --
Directs the Secretary to require FQHCs to submit to the Secretary such information
require in order to develop and implement the FQHC prospective payment system.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
5104
(2of2)
Sec. 10501 -- Amendments to Title V -- Interagency task force to assess and
improve access to health care in the State of Alaska – requires the Task force
submit a report to Congress.
RTC
9/17/10
5501
Expanding access to primary care services and general surgery service -- Beginning
in 2011, provides primary care practitioners, as well as general surgeons practicing
in health professional shortage areas, with a 10 percent Medicare payment bonus
for five years. Half of the cost of the bonuses would be offset through an across-
the-board reduction in all other services.
Guidance – Change Request
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
6-4-10
06/25/2010
11-2-10
5503
Distribution of additional residency positions -- Beginning July 1, 2011, directs the
Secretary to redistribute residency positions that have been unfilled for the prior
three cost reports and directs those slots for training of primary care physicians. In
distributing the residency slots under this section, special preference will be given
to programs located in States with a low physician resident to general population
ratio and to programs located in States with the highest ratio of population living in
Regulation -- OPPS Proposed Rule
Regulation – OPPS Final Rule
7-2-10
11-2-10

All CMS Provisions -- As of December 10, 2010
24
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
a health professional shortage area (HPSA) relative to the general population.
5504
Counting resident time in outpatient settings and allowing flexibility for jointly
operated residency training programs -- Modifies rules governing when hospitals
can receive indirect medical education (IME) and direct graduate medical
education (DGME) funding for residents who train in a non-provider setting so that
any time spent by the resident in a non-provider setting shall be counted toward
DGME and IME if the hospital incurs the costs of the stipends and fringe benefits.
Regulation -- OPPS Proposed Rule
Regulation – OPPS Final Rule
7-2-10
11-2-10
5505
Rules for counting resident time for didactic and scholarly activities and other
activities -- Modifies current law to allow hospitals to count resident time spent in
didactic conferences toward IME costs in the provider (i.e., hospital) setting and
toward DGME in the non-provider (i.e., non-hospital) setting.
Sec. 10501 -- Amendments to Title V – (j) Technical corrections to the rules for
counting resident time for didactic and scholarly activities and other activities --
Clarifies that the Secretary is not required to reopen certain settled cost reports in
applying changes to Medicare graduate medical education payment rules related
to didactic training.
Regulation -- OPPS Proposed Rule
Regulation – OPPS Final Rule
7-2-10
11-2-10
5506
Preservation of resident cap positions from closed hospitals -- Directs the
Secretary to redistribute medical residency slots from a hospital that closes on or
after the date that is two years before enactment of this legislation based on
certain criteria.
Regulation -- OPPS Proposed Rule
Regulation – OPPS Final Rule
7-2-10
11-2-10

All CMS Provisions -- As of December 10, 2010
25
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
6001
(1of3)
Limitation on Medicare exception to the prohibition on certain physician referrals
for hospitals -- Prohibits physician-owned hospitals that do not have a Medicare
provider agreement in effect on December 31, 2010 from furnishing services
pursuant to referrals made by physician owners or investors (known as “self-
referral”). Hospitals that have physician owners or investors and a provider
agreement in effect on December 31, 2010 may continue to access exceptions to
the self-referral prohibition if certain requirements are met addressing conflicts of
interest, bona fide investments, and patient safety issues, as well as new disclosure
and reporting requirements.
Sec 10601 -- Revisions to limitation on Medicare exception to the prohibition on
certain physician referrals for hospitals -- changed dates that were then changed
by RB.
RB -- 1106 -- Physician ownership
‐
referral -- Changes to December 31, 2010 the
date after which physician ownership of hospitals to which they self refer is
prohibited and provides a limited exception to the growth restrictions for
grandfathered physician owned hospitals that treat the highest percentage of
Medicaid patients in their county (and are not the sole hospital in a county).
Regulation -- OPPS Proposed Rule
Regulation – OPPS Final Rule
7-2-10
11-2-10
6003
Disclosure requirements for in-office ancillary services exception to the
prohibition on physician self-referral for certain imaging services -- Adds an
additional requirement to the Medicare in-office ancillary exception that requires
the referring physician to inform the patient in writing that the individual may
obtain the specified service from a person other than the referring physician, a
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
06/25/2010
11-2-10

All CMS Provisions -- As of December 10, 2010
26
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
physician who is a member of the same group practice as the referring physician,
or an individual who is directly supervised by the physician or by another physician
in the group practice.
Schedule Final Rule
6111
Civil money penalties -- Provides the Secretary with authority to reduce civil
monetary penalties (CMPs) from the level that they would otherwise be by 50
percent for certain facilities that self-report and promptly correct deficiencies
within ten calendar days of imposition. For CMPs that are cited at the level of
actual harm and immediate jeopardy, the Secretary would be provided with the
authority to place CMPs in an escrow account following completion of the informal
dispute resolution process, or the date that is 90 days after the date of the
imposition of the CMP, whichever is earlier. If the facility’s appeal is successful, the
CMP, with interest, would be returned to the facility. If the appeal is unsuccessful,
some portion of the proceeds may be used to fund activities that benefit facility
residents.
Regulation -- CMP Reduction for
Self-Reporting Proposed Rule
State Medicaid informational
Bulletin
7/12/2010
6/12/2010
6201
(1of2)
Nationwide program for National and State background checks on direct patient
access employees of long-term care facilities and providers -- Requires the
Secretary to establish a nationwide program for national and State background
checks on direct patient access employees of certain long-term supports and
services facilities or providers. This program is based on the background check pilot
program in the Medicare Modernization Act.
Grant Solicitation 06/15/2010

All CMS Provisions -- As of December 10, 2010
27
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
6401
Provider screening and other enrollment requirements under Medicare, Medicaid, and CHIP -- Provider
Screening -- Requires that the Secretary, in consultation with the OIG, establish procedures for screening
providers and suppliers participating in Medicare, Medicaid, and CHIP. Requires the Secretary to
determine the level of screening according to the risk of fraud, waste, and abuse with respect to each
category of provider or supplier. At a minimum, all providers. The Secretary would have the authority to
impose additional screening measures based on risk, including fingerprinting, criminal background checks,
multi-State data base inquiries, and random or unannounced site visits.
Regulation – Program Integrity for
Provider-Supplier Proposed Rule
CPI -CMCS Informational Bulletin
09/17/2010
6/21/2010
6402
(1of3)
Enhanced Medicare and Medicaid program integrity provisions --
National Provider Identifier -- Requires the Secretary to issue a regulation mandating
that all Medicare, Medicaid, and CHIP providers include their NPI on enrollment
applications.
Regulation – Changes in Provider
and Supplier Enrollment, Ordering
and Referring, and Documentation
Requirements, etc. Interim Final Rule
(to address NPI)
Regulation – Program Integrity for
Provider-Supplier Proposed Rule
4-30-10
09/17/10
6404
Maximum period for submission of Medicare claims reduced to not more than 12
months -- Beginning January 2010, the maximum period for submission of
Medicare claims would be reduced to not more than 12 months.
Guidance -- JSM
Guidance -- Change Request
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
3-31-10
5-7-10
6-25-10
11-2-10
6405
Physicians who order items or services required to be Medicare enrolled
physicians or eligible professionals -- Requires durable medical equipment (DME)
Regulation – Changes in Provider
and Supplier Enrollment, Ordering
04/30/2010

All CMS Provisions -- As of December 10, 2010
28
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
or home health services to be ordered by a Medicare physician enrolled in the
Medicare program. The Secretary would have the authority to extend these
requirements to other Medicare items and services to reduce fraud, waste, and
abuse.
Sec 10604 -- Technical Corrections to Section 6405 -- Clarifies that this expansion of
DME requirements applies to those enrolled in Sec. 1866(j) of the SSA and not also
those referred to in Sec. 1848(k)(3)(B) of the SSA.
and Referring, and Documentation
Requirements, etc. Interim Final Rule
(to address NPI)
Guidance -- Press Release
Regulation – Program Integrity for
Provider-Supplier Proposed Rule
6/30/2010
09/17/10
6406
(1of2)
Requirement for physicians to provide documentation on referrals to programs at
high risk of waste and abuse -- Beginning January 1, 2010, the Secretary would
have the authority to disenroll, for no more than one year, a Medicare enrolled
physician or supplier that fails to maintain and provide access to written orders or
requests for payment for DME, certification for home health services, or referrals
for other items and services.
Regulation – Changes in Provider
and Supplier Enrollment, Ordering
and Referring, and Documentation
Requirements, etc. Interim Final Rule
(to address NPI)
04/30/2010
6407
(1of2)
Face-to-face encounter with patient required before physicians may certify
eligibility for home health services or durable medical equipment under Medicare
-- Requires physicians to have a face-to-face encounter with the individual prior to
issuing a certification for home health services. The Secretary would be authorized
to apply the face-to-face encounter requirement to other items and services based
upon a finding that doing so would reduce the risk of fraud, waste, and abuse. This
provision also applies to Medicaid.
Sec. 10605 -- Certain other providers permitted to conduct face-to-face encounter
Guidance -- Change Request
Regulation – Home Health Proposed
Rule
Regulation – Home Health Final Rule
11/2/2010
07/16/2010
11/02/2010

All CMS Provisions -- As of December 10, 2010
29
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
for home health services -- Clarifies that the face-to-face encounter required prior
to certification for home health services may be performed by a physician, nurse
practitioner, clinical nurse specialist, certified nurse-midwife, or physician assistant.
6409
(1of2)
Medicare self-referral disclosure protocol -- Within six months of enactment, the
Secretary, in cooperation with the HHS OIG, would be required to establish a self-
referral disclosure protocol to enable health care providers and suppliers to
disclose actual or potential violations of the physician self-referral law.
Guidance – Web posting
09/23/2010
6410
(1of2)
Adjustments to the Medicare durable medical equipment, prosthetics, orthotics,
and supplies competitive acquisition program -- Requires the Secretary to expand
the number of areas to be included in round two of the competitive bidding
program from 79 of the largest metropolitan statistical areas (MSAs) to 100 of the
largest MSAs.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
6410
(2of2)
Adjustments to the Medicare durable medical equipment, prosthetics, orthotics,
and supplies competitive acquisition program -- Requires the Secretary to use
competitively bid prices in all areas by 2016.
Regulation -- Physician Fee
Schedule Proposed Rule
Regulation – Physician Fee
Schedule Final Rule
06/25/2010
11/2/2010
6501
Termination of provider participation under Medicaid if terminated under
Medicare or other State plan-- Requires States to terminate the participation of
individuals or entities from their Medicaid programs if the participation individuals
or entities were terminated from Medicare or another State's Medicaid program.
Regulation – Program Integrity for
Provider-Supplier Proposed Rule
09/17/2010

All CMS Provisions -- As of December 10, 2010
30
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
6506
Overpayments -- Extends the period for States to recover overpayments due to
fraud to one year after date of discovery of the overpayment, before an
adjustment is made to the federal payment. If the State has not recovered the
overpayment due to fraud within one year of discovery because there has not been
a final determination of the overpayment amount, no adjustment shall be made in
the Federal payment to such State on account of such overpayment (or portion
thereof) before the date that is 30 days after the date on which a final judgment
(including, if applicable, a final determination on an appeal) is made.
The Secretary shall promulgate regulations that require States to correct Federally
identified claims overpayments, of an ongoing or recurring nature, with new
Medicaid Management Information System (MMIS) edits, audits, or other
appropriate corrective action.
SMD Letter
7-13-2010
6507
(1of2)
Mandatory State use of national correct coding initiative -- Requires States to
make their MMIS methodologies compatible with Medicare’s national correct
coding initiative (NCCI) that promotes correct coding and controls improper coding.
SMD Letter
9/1/2010

All CMS Provisions -- As of December 10, 2010
31
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
6703
(1of9)
Elder Justice -- Requires the Secretary of HHS, in consultation with the
Departments of Justice and Labor, to award grants and carry out activities that
provide greater protection to those individuals seeking care in facilities that
provide long-term services and supports and provide greater incentives for
individuals to train and seek employment at such facilities. Owners, operators, and
certain employees of these facilities would be required to report suspected crimes
committed at a facility. Owners or operators of such facilities would also be
required to submit to the Secretary and to the State written notification of an
impending closure of a facility within 60 days prior to the closure. In the notice, the
owner or operator would be required to include a plan for transfer and adequate
relocation of all residents.
Grant Solicitation 07-15-10
10201
(1of2)
Amendments to the Social Security Act and Title II of this Act – Increases the
transparency of the Medicaid waiver development and approval processes, at the
State and federal levels by Requiring the Secretary to promulgate regulations
relating to the application and renewals of a demonstration project that provides
for a process for public hearings.
Regulation – Proposed Rule 09/17/2010
10324
Protections for frontier states -- Starting in fiscal year 2011, establishes hospital
wage index and geographic practice expense floors for hospitals and physicians
located in states in which at least 50 percent of the counties in the state are
frontier.
Regulation -- OPPS and Physician
Fee Schedule Proposed Rule
Federal Register Notice --
Changes to the IPPS Resulting
from 2010 HCR Provisions
7-2-10
5-21-10
All CMS Provisions -- As of December 10, 2010
32
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
Regulation – OPPS and
Physician Fee Schedule Final
Rule
11-2-10
10325
Revision to skilled nursing facility prospective payment system --Delays
implementation of certain skilled nursing facility “RUGs-IV” payment system
changes by one year to October 1, 2011. Beginning October 1, 2010, the Secretary
shall implement changes specific to therapy furnished on a concurrent basis that is
a component of RUG-IV and changes to the look-back period to ensure that only
those services furnished after admission to a SNF are used as factors in
determining a case-mix classification.
Federal Register Notice -- SNF
PPS
07-19-10
10327
Improvements to the Physician Quality Reporting System -- Provides an additional
0.5 percent Medicare payment bonus to physicians who successfully report quality
measures to CMS via a qualified Maintenance of Certification program. Eliminates
the MA Regional Plan Stabilization Fund.
Regulation – Revisions to the
Parts C & D Contract Years 2012
Proposed Rule
11-10-10
10328
Improvement in Part D medication therapy management (MTM) programs --
Requires Part D prescription drug plans to include a comprehensive review of
medications (either in person or through telehealth technology) and a written
summary of the review as part of their medication therapy management programs.
Plans must also enroll beneficiaries who qualify on a quarterly basis and allow for
opt out.
Regulation – Revisions to the
Parts C & D Contract Years 2012
Proposed Rule
11-10-10

All CMS Provisions -- As of December 10, 2010
33
RB = Reconciliation bill
The Patient Protection and Affordable Care Act
Section
of the
Law
Subject Implementing Document
Release
Date
10332
Availability of Medicare data for performance measurement -- Authorizes the
release and use of standardized extracts of Medicare claims data to measure the
performance of providers and suppliers in ways that protect patient privacy and in
accordance with other requirements.
Federal Register Notice -- Medicare
Program; Listening Session
Regarding the Availability of
Medicare Data for Performance
Measurement, September 20, 2010 -
- (CMS- 0031-N)
08/27/2010
